1. Introduction
Depression, clinically referred to as depressive disorders, constitutes a spectrum of mental disorders which significantly impair social functioning, occupational performance, and other critical aspects of daily life [1,2]. Currently, depression has become one of the leading public health issues with approximately 280,000,000 individuals living with depression worldwide in 2023 [3]. The main symptoms of depressive disorders are significant weight loss, insomnia, fatigue, and thoughts of dying or suicide [1]. In severe cases, depression may contribute to self-harm behaviors and fatal suicide attempts. Regarding to World Health Organization report, over 700,000 people die by suicide due to depression worldwide every year [3], positioning it a globally critical public health priority. The United States reflects this alarming trend, where data reported by National Institute of Mental Health in 2021 revealed that approximately 21,000,000 adults (8.3% of the adult population) who have experienced at least a significant depressive episode [4].
Sleep, a fundamental physiological process, serves as a dynamic regulator of multisystem homeostasis [5]. Emerging evidence suggests a reciprocal, complicated relationship linking sleep disturbances to depression [6,7]. Substantial studies have demonstrated that sleep problems are common symptoms and critical factors and elevate the likelihood of developing depression [8–10]. Consequently, investigating the interrelationship between sleep duration and depression risk is significant to early prevention, accurate diagnosis, and optimized treatment strategies, and offers a theoretical foundation for intervening in depression via regulating and improving sleep.
Existing research has identified an inverted U-shaped curve linking sleep duration to incidence of depression, which illustrates the risk of depression was found to be negatively correlated with sleep duration, reaching its lowest point at 8 hours, and once sleep duration extended beyond 8 hours, there was a substantial elevation in the risk of depression occurrence [11]. Nevertheless, preceding studies have been limited by inadequate adjustment for some confounding factors or restrictive age ranges [12,13]. To address these gaps, we aimed to conduct a cross-sectional analysis utilizing data from the National Health and Nutrition Examination Survey (NHANES) between 2021 and 2023, examining the association between sleep duration and likelihood of depression in a general adult population in the U.S. We hypothesized the prospect of depression is associated with sleep duration.
2. Methods
2.1. Research population
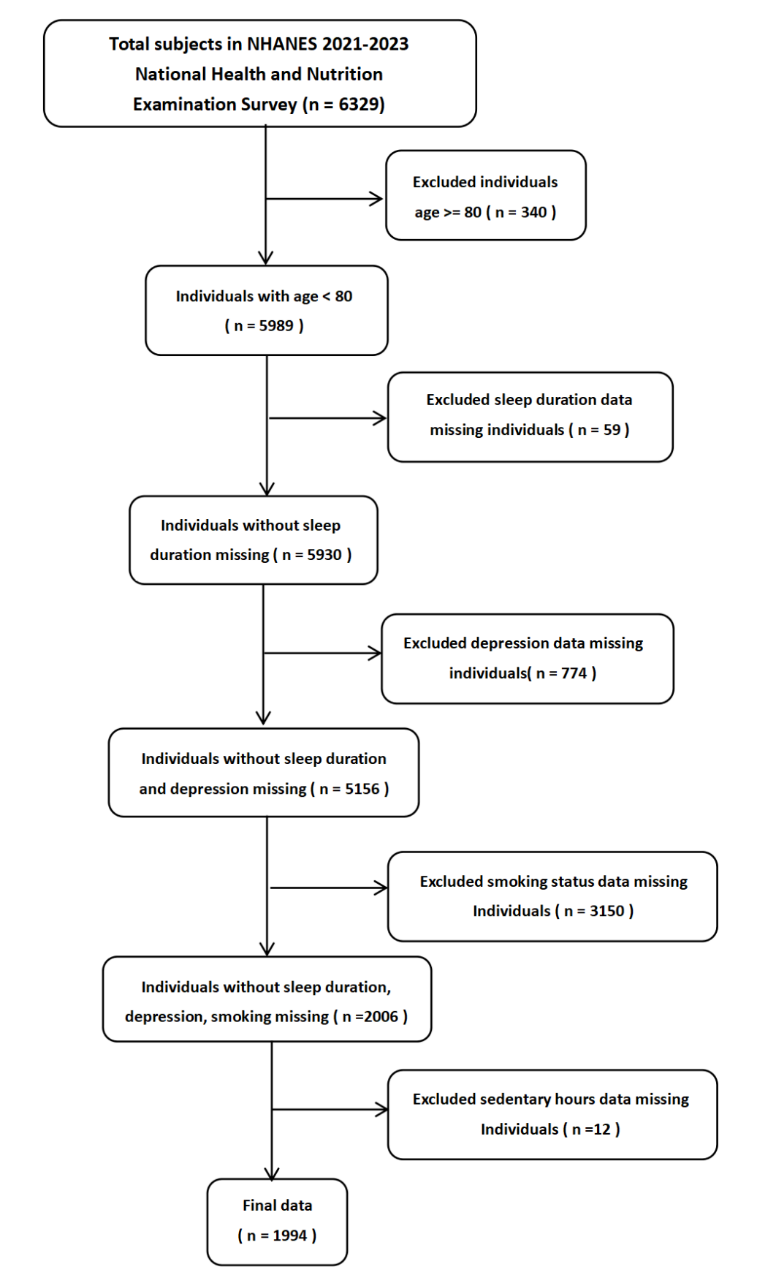
In this study, we scrutinized data procured from NHANES. The dataset comprised a two-year sample collected from 2021 to 2023 through a multi-year sampling design. This stratified, clustered four-stage sampling means included states, counties, households, and individuals from the U.S. civilian, non-institutionalized population. The initial dataset included 6,329 participants with identification numbers. After the inclusion of necessary covariates and exclusion of cases with missing values, our ultimate analytical sample encompassed 1994 samples (Fig. 1.).
2.2. Measurement
2.2.1. Sleep duration
Sleep Disorders (SLQ) is a module from the NHANES that asked respondents about their sleep and wake times, adapted from the Munich Chrono Type Questionnaire (2003). The variable "Weekdays sleep duration" was a continuous variable ranging from 2 to 14 hours, which was created from one of these questions: "Sleep hours - weekdays or workdays."
2.2.2. Depression
Mental Health - Depression Screener (DPQ) is an NHANES module which provides a nine-item scale for depression syndromes screening derived from the Patient Health Questionnaire (PHQ-9) to evaluate respondents’ depressive syndromes over the preceding two weeks. The PHQ-9 comprises 9 questions. We calculated the overall score (ranging from 0 to 27) of those who completed all nine questions of DPQ. Based on the scoring criteria, we classified respondents’ depression categories as follows: no depressive symptoms (with scores between 0 and 4), possible mild depression (with scores between 5 and 9), possible moderate depression (with scores between 10 and 14), possible moderately severe depression (with scores between 15 and 19), and possible severe depression (with scores between 20 and 27). Given that the data is heavily concentrated in the “no depressive symptoms” category while the sample sizes for the other categories are relatively small, the original depression categories were reclassified. Specifically, respondents with a score of 14 or lower were categorized as “unlikely depressed” and those with a score greater than 14 were classified as “likely depressed”.
2.3. Other factors
Sex assigned at birth was treated as a binary variable which include male and female. Race was categorized according to how participants responded to the survey questions on race and ethnicity and classified into 7 groups: Mexican American, Other Hispanic, Non-Hispanic White, Non-Hispanic Black, Non-Hispanic Asian and Other Race. Education level was categorized into 5 groups: less than 9th grade, 9-11th grade, high school graduate/GED or equivalent, some college or Associate of Arts, college graduate or above, according to the question: “What’s the highest school level you’ve finished up, or the highest degree you’ve obtained?” Marital status was grouped into 3 main categories: married/living with partner, widowed/divorced/separated and never married. Age was calculated as the years between participants' birth date and interview date. Smoking was grouped by the response to the query: “Do you now smoke cigarettes?” Based on responses to this question, smoking was divided into every day, some days and not at all and we separated them into smoker and non-smoker. Daily sedentary time was a value about how much time a participant usually spends sitting during a standard day and it was converted from minutes to hours to facilitate calculations.
2.4. Statistical analysis
Continuous variables, including weekday sleep duration and daily sedentary hours, were reflected as mean values along with standard deviation (SD). Categorical variables, such as smoking status, possibility of depression and age, were expressed as counts (weighted percentages). Logistic regression analysis was applied to appraisal the odds ratios (OR) with 95% confidence intervals (CI), aiming to appraise the association between the sleep hours and depression level. Hinged on previous research findings, we have noted that the statistical association between sleep hours and the probability of developing depression may not follow a linear pattern. Additionally, we adopted piecewise regression to study the potential nonlinear relationship between sleep hours and depression level. Hinged on the distribution of sleep duration in our data frame, we split sleep duration into two groups: less than 8 hours and 8 hours or more. Further exploration was conducted into the link between sleep hours and depression levels throughout each period. Statistical analyses were executed using R software, version 4.5.1, and p-value < 0.05 was established as the criterion for determining statistical significance.
3. Results
This study included 1994 individuals, of whom 1129 (56.6%) were male and 865 (43.4%) were female. The weighted total population number was 58,464,524, after accounting for survey weights. Within this group, the mean age of the participants stood at 55.4 years. Regarding depressive symptoms, an average DPQ score of the sample was 4.64, with 1888 (94.7%) classified as unlikely to be depressed and 106 (5.3%) as likely to be depressed. In terms of smoking habits, 1232 (61.8%) were non - smokers, while 762 (38.2%) were smokers. Additionally, the mean sedentary activity time was 6.2 hours. A summary of the participants' core idiosyncratic can be found in Table 1.
|
Characteristics |
Total |
|
N |
1994 |
|
Sex, n (%) |
|
|
Male |
1129(56.6%) |
|
Female |
865(43.4%) |
|
Education, n (%) |
|
|
Less than 11th grade |
207(10.4%) |
|
High school |
608(30.5%) |
|
Some college |
718(36.0%) |
|
College graduate or above |
461(23.1%) |
|
Race, n (%) |
|
|
Hispanic |
239(12.0%) |
|
White |
1372(68.8%) |
|
Black |
166(8.3%) |
|
Other Race |
215(10.8%) |
|
Marital stages, n (%) |
|
|
Marriage/living the partner |
1194(59.9%) |
|
Divorced/separated/widowed |
463(23.2%) |
|
Never married |
337(16.9%) |
|
Age(years), Mean (SD) |
55.4(15.6) |
|
DPQ score, Mean (SD) |
4.64(4.9) |
|
Severity level, n (%) |
|
|
Unlikely depress |
1888(94.7%) |
|
Likely depress |
106(5.3%) |
|
Smoking, n (%) |
|
|
Nonsmokers |
1232(61.8%) |
|
Smokers |
762(38.2%) |
|
Sedentary activity(hours), Mean (SD) |
6.2(3.6) |
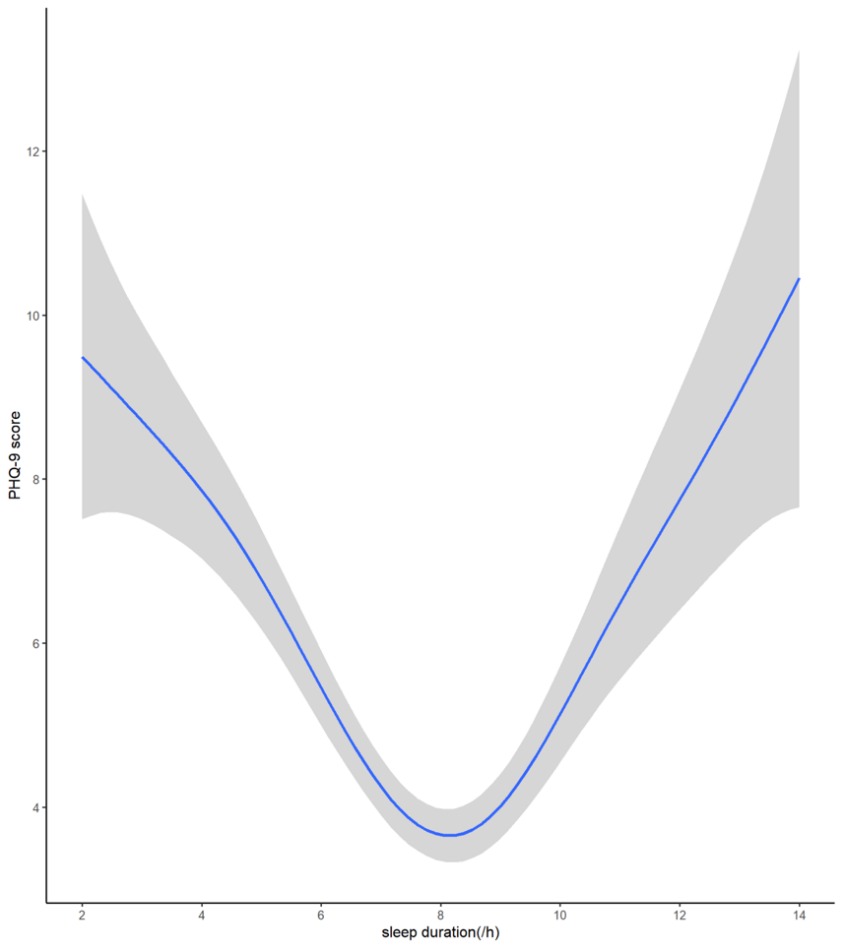
In this study, we provided qualitative assessment based on sample distribution map (Fig. 2.) and established 8 hours as the turning point for doing regression. To delve deeper into the nonlinear correlation between the length of sleep and the probability of depression, piecewise regression analysis was utilized. The fully adjusted model which is testified to a U-shaped connection between sleep time span and the PHQ-9 score (Fig. 2.). Through further threshold effect analysis (Table 2), we identified 8 hours as the critical threshold in the non-linear pattern between sleep time span and the likelihood of depression among adults. Among individuals sleeping less than 8 hours, each additional hour of sleep was followed with a 34.3% lower likelihood of depression (OR=0.657, 95% CI 0.558- 0.774, p<0.001). However, among individuals sleeping 8 hours or more, each additional hour of sleep was associated with a 60.7% higher likelihood of depression (OR=1.607, 95%CI 1.255, 2.059, p<0.001).
The solid blue line delineates the anticipated value, while the shaded region denotes the 95% CI. These results have been adjusted for factors including age, smoking status, and daily sedentary hours.
|
Threshold of sleep hours |
OR* |
95%CI* |
P value |
|
<8 |
0.657 |
0.558, 0.774 |
<0.001 |
|
≥8 |
1.607 |
1.255, 2.059 |
<0.001 |
4. Discussion
This study disclosed a U-shaped pattern concerning the relation between sleep duration and probability of depression by using 8 hours as the reference threshold. Individuals with a sleep duration under 8 hours exhibit a higher likelihood of depression, and each additional hour of sleeping reduce the likelihood of depression. Conversely, individuals whose sleep duration exceeded 8 hours are linked to a higher likelihood of depression. These outcomes imply that both meager(<8 hours) and exorbitant(>8hours) sleep, taking 8-hour as a reference, may elevate the probability of developing depression in U.S. adults.
Many previous studies have explored the relationship between sleep duration and depression. The study supervised by Liqing et al., which encompassed 34 prospective cohort studies, uncovered a notable link between insomnia and a heightened risk of depression [14]. Régis and his colleagues pointed out that hypersomnia exhibits a multifaceted relationship with depression [15]. Xin-Lin’s team, through a dose-response meta-analysis, revealed that not only insufficient but also excessive sleep duration are factors that precipitate a higher incidence of depression [16]. Additionally, previous cross-sectional studies utilizing data from NHANES have also advocated the presence of a U-shaped relationship between the length of sleep and the probability of developing depression [11,17,18]. These results align precisely with our research findings.
Short - term sleep deprivation may have a part to play in the initiation of depressive episodes through several mechanisms. The following are two possible mechanisms. First, insufficient sleep duration significantly diminishes the accessibility of dopamine D2/D3 receptors [19], subsequently leading to attenuated dopamine signal transmission [20], and ultimately resulting in depressive-like behaviors including anhedonia and a lack of motivation [21]. Second, short sleep duration weakens the activity of the right hippocampus in the brain, significantly impairing the human the brain’s capacity to hold back unwanted memories [22]. Over the long term, this can precipitate the accumulation of pessimistic emotions and potentially trigger depression. Conversely, excessive sleep duration may also elevate the peril of depression through several pathways. One possible explanation, sleeping for long periods of time may lead to a decline in cognitive ability, which can slash individuals’ abilities to cope with stress, forming a vicious cycle of “sleep disorder - cognitive decline - worsening depression” [23]. Additionally, long sleep duration may weaken the abilities of emotional regulation by inhibiting prefrontal cortex activity [24], potentially leading to manifestations such as irritability and excessive self-blame [25], thereby increasing the susceptibility to depression. Finally, long time sleeper may experience increased loneliness owing to reduced social activity, which in turn amplifies boredom and indirectly increases the tendency toward depression [26].The comorbidity of sleep disorders and major depressive disorder implies a potential bidirectional interaction between them, indicating that sleep problems can potentially exacerbate depressive symptoms, and conversely, depressive states can also impact sleep [27–29].
Several significant strengths are inherent in our study. First, our study population included adults aged from 18 to 79, which covered a relatively wide range of ages in adults’ population. Thus, the results of our study can have a broad generalizability among people of different ages. Second, we took both demographic and lifestyle factors (age , smoking status [30], and sedentary hours per day [31]) as our consideration to adjust our models. Moreover, we employed piecewise regression to flexibly capture the nonlinear linkage between the number of sleep hours and likelihood of depression. In this way, we captured complex U-shaped relationship within the data. However, we must point out that our study is accompanied by certain limitations. In the first place, we are incapable to obtain the provenance from the results due to the cross-sectional nature of the study. Long - term follow - up studies are imperative to infer causality between sleep hours and the likelihood of depression. Moreover, because our dependent and independent variables chosen from NHANES are both self-reported, potential misclassification biases are existing, such as subjective interpretation differences, social desirability bias, and recall bias. Furthermore, because of the relatively large number of missing data, we are incapable of adjusting all confounding factors, such as health condition [32], living condition [33], etc. Therefore, residual confounding factors are inevitable.
5. Conclusion
In conclusion, this study revealed that there is a U-shaped link between how long people sleep and their chance of having depression. When sleep hours less than 8, the likelihood of depressive disorder decreases as the sleep length increases. Meanwhile, when sleep duration exceeds or equal to 8, the likelihood of depressive disorder increases as the sleep length increases. As indicated by this finding, sleep duration may serve as a practical indicator for mental health assessment.
Acknowledgements
LU PENG, RUIYU YANG and GUANGXUAN MENG made equal contributions to this work and warrant recognition as co - first authors. All of us would like to declare sincere recognition to Professor Hui Zhang, whose proposed method provided critical guidance for the research direction. All of us also appreciate Teaching Assistant Cao Fang for her valuable assistance and professional guidance during the research process, which facilitated the smooth progress of this work.
References
[1]. American Psychiatric Association, editor. Desk reference to the diagnostic criteria from DSM-5. Washington, DC: American Psychiatric Publishing; 2013. 395 p.
[2]. Fazel BTR, Psy.D. Depression Definition and DSM-5 Diagnostic Criteria [Internet]. HealthCentral. 2022 [cited 2025 July 17]. Available from: https: //www.healthcentral.com/condition/depression/dsm-5-depression-criteria
[3]. Depressive disorder (depression) [Internet]. [cited 2025 July 17]. Available from: https: //www.who.int/news-room/fact-sheets/detail/depression
[4]. Major Depression - National Institute of Mental Health (NIMH) [Internet]. [cited 2025 July 21]. Available from: https: //www.nimh.nih.gov/health/statistics/major-depression
[5]. Postnova S, Sanz-Leon P. Sleep and circadian rhythms modeling: From hypothalamic regulatory networks to cortical dynamics and behavior. Handb Clin Neurol. 2025; 206: 37–58.
[6]. Sun Y, Shi L, Bao Y, Sun Y, Shi J, Lu L. The bidirectional relationship between sleep duration and depression in community-dwelling middle-aged and elderly individuals: evidence from a longitudinal study. Sleep Med. 2018 Dec; 52: 221–9.
[7]. Sculthorpe LD, Douglass AB. Sleep pathologies in depression and the clinical utility of polysomnography. Can J Psychiatry Rev Can Psychiatr. 2010 July; 55(7): 413–21.
[8]. Fang H, Tu S, Sheng J, Shao A. Depression in sleep disturbance: A review on a bidirectional relationship, mechanisms and treatment. J Cell Mol Med. 2019 Apr; 23(4): 2324–32.
[9]. Fink AM. Shift Work Sleep Disorder and Mental Health: An Integrative Review of Neurobiological, Sociological, and Psychological Perspectives With Public Policy Implications. Policy Polit Nurs Pract. 2024 May; 25(2): 94–102.
[10]. Roberts RE, Duong HT. The prospective association between sleep deprivation and depression among adolescents. Sleep. 2014 Feb 1; 37(2): 239–44.
[11]. Dong L, Xie Y, Zou X. Association between sleep duration and depression in US adults: A cross-sectional study. J Affect Disord. 2022 Jan 1; 296: 183–8.
[12]. Zhai L, Zhang H, Zhang D. SLEEP DURATION AND DEPRESSION AMONG ADULTS: A META-ANALYSIS OF PROSPECTIVE STUDIES. Depress Anxiety. 2015 Sept; 32(9): 664–70.
[13]. Li X lin, Wei J, Zhang X, Meng Z, Zhu W. Relationship between night-sleep duration and risk for depression among middle-aged and older people: A dose–response meta-analysis. Front Physiol. 2023 Mar 2; 14: 1085091.
[14]. Li L, Wu C, Gan Y, Qu X, Lu Z. Insomnia and the risk of depression: a meta-analysis of prospective cohort studies. BMC Psychiatry. 2016 Nov 5; 16(1): 375.
[15]. Lopez R, Barateau L, Evangelista E, Dauvilliers Y. Depression and Hypersomnia: A Complex Association. Sleep Med Clin. 2017 Sept; 12(3): 395–405.
[16]. Li XL, Wei J, Zhang X, Meng Z, Zhu W. Relationship between night-sleep duration and risk for depression among middle-aged and older people: A dose-response meta-analysis. Front Physiol. 2023; 14: 1085091.
[17]. Cai Z, Ye Y, Chen S, Cai H, Lin J, Peng H, et al. U-shaped association between average daily sleep duration and depression among individuals with hypertension: a cross-sectional study based on NHANES 2017-2020. BMC Psychiatry. 2025 July 1; 25(1): 608.
[18]. Chunnan L, Shaomei S, Wannian L. The association between sleep and depressive symptoms in US adults: data from the NHANES (2007-2014). Epidemiol Psychiatr Sci. 2022 Sept 8; 31: e63.
[19]. Volkow ND, Tomasi D, Wang GJ, Telang F, Fowler JS, Logan J, et al. Evidence that sleep deprivation downregulates dopamine D2R in ventral striatum in the human brain. J Neurosci Off J Soc Neurosci. 2012 May 9; 32(19): 6711–7.
[20]. Drevets WC. Functional anatomical abnormalities in limbic and prefrontal cortical structures in major depression. Prog Brain Res. 2000; 126: 413–31.
[21]. Wise RA. Dopamine, learning and motivation. Nat Rev Neurosci. 2004 June; 5(6): 483–94.
[22]. Harrington MO, Karapanagiotidis T, Phillips L, Smallwood J, Anderson MC, Cairney SA. Memory control deficits in the sleep-deprived human brain. Proc Natl Acad Sci U S A. 2025 Jan 7; 122(1): e2400743122.
[23]. Young VM, Bernal R, Baril AA, Zeynoun J, Wiedner C, Gaona C, et al. Long sleep duration, cognitive performance, and the moderating role of depression: A cross-sectional analysis in the Framingham Heart Study. Alzheimers Dement J Alzheimers Assoc. 2025 Apr; 21(4): e70160.
[24]. Aime M, Calcini N, Borsa M, Campelo T, Rusterholz T, Sattin A, et al. Paradoxical somatodendritic decoupling supports cortical plasticity during REM sleep. Science. 2022 May 13; 376(6594): 724–30.
[25]. Yiniu W, Yuejia L. Emotional Disorders in Patients with Prefrontal Cortex Lesions. Adv Psychol Sci. 2004 Mar 15; 12(02): 161.
[26]. Hager NM, Judah MR, Milam AL. Loneliness and Depression in College Students During the COVID-19 Pandemic: the Role of Boredom and Repetitive Negative Thinking. Int J Cogn Ther. 2022; 15(2): 134–52.
[27]. Sun Y, Shi L, Bao Y, Sun Y, Shi J, Lu L. The bidirectional relationship between sleep duration and depression in community-dwelling middle-aged and elderly individuals: evidence from a longitudinal study. Sleep Med. 2018 Dec; 52: 221–9.
[28]. Sun X, Zheng B, Lv J, Guo Y, Bian Z, Yang L, et al. Sleep behavior and depression: Findings from the China Kadoorie Biobank of 0.5 million Chinese adults. J Affect Disord. 2018 Mar 15; 229: 120–4.
[29]. Gao L, Yang J, Liu J, Xin T, Liu Y. Activities of Daily Living and Depression in Chinese Elderly of Nursing Homes: A Mediation Analysis. Psychol Res Behav Manag. 2023; 16: 29–38.
[30]. Fluharty M, Taylor AE, Grabski M, Munafò MR. The Association of Cigarette Smoking With Depression and Anxiety: A Systematic Review. Nicotine Tob Res Off J Soc Res Nicotine Tob. 2017 Jan; 19(1): 3–13.
[31]. Bo Li, Han SS, Ye YP, Li YX, Meng SQ, Feng S, et al. Cross sectional associations of physical activity and sleep with mental health among Chinese university students. Sci Rep. 2024 Dec 30; 14(1): 31614.
[32]. Beurel E, Toups M, Nemeroff CB. The Bidirectional Relationship of Depression and Inflammation: Double Trouble. Neuron. 2020 July 22; 107(2): 234–56.
[33]. Mykyta L. Living Alone and Feelings of Depression Among Adults Age 18 and Older. Natl Health Stat Rep. 2024 Feb; (199): 1–11.
Cite this article
Peng,L.;Yang,R.;Meng,G. (2025). The Association Between Sleep Duration and the Likelihood of Depression in US Adult Population. Theoretical and Natural Science,141,166-174.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of ICBioMed 2025 Symposium: AI for Healthcare: Advanced Medical Data Analytics and Smart Rehabilitation
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. American Psychiatric Association, editor. Desk reference to the diagnostic criteria from DSM-5. Washington, DC: American Psychiatric Publishing; 2013. 395 p.
[2]. Fazel BTR, Psy.D. Depression Definition and DSM-5 Diagnostic Criteria [Internet]. HealthCentral. 2022 [cited 2025 July 17]. Available from: https: //www.healthcentral.com/condition/depression/dsm-5-depression-criteria
[3]. Depressive disorder (depression) [Internet]. [cited 2025 July 17]. Available from: https: //www.who.int/news-room/fact-sheets/detail/depression
[4]. Major Depression - National Institute of Mental Health (NIMH) [Internet]. [cited 2025 July 21]. Available from: https: //www.nimh.nih.gov/health/statistics/major-depression
[5]. Postnova S, Sanz-Leon P. Sleep and circadian rhythms modeling: From hypothalamic regulatory networks to cortical dynamics and behavior. Handb Clin Neurol. 2025; 206: 37–58.
[6]. Sun Y, Shi L, Bao Y, Sun Y, Shi J, Lu L. The bidirectional relationship between sleep duration and depression in community-dwelling middle-aged and elderly individuals: evidence from a longitudinal study. Sleep Med. 2018 Dec; 52: 221–9.
[7]. Sculthorpe LD, Douglass AB. Sleep pathologies in depression and the clinical utility of polysomnography. Can J Psychiatry Rev Can Psychiatr. 2010 July; 55(7): 413–21.
[8]. Fang H, Tu S, Sheng J, Shao A. Depression in sleep disturbance: A review on a bidirectional relationship, mechanisms and treatment. J Cell Mol Med. 2019 Apr; 23(4): 2324–32.
[9]. Fink AM. Shift Work Sleep Disorder and Mental Health: An Integrative Review of Neurobiological, Sociological, and Psychological Perspectives With Public Policy Implications. Policy Polit Nurs Pract. 2024 May; 25(2): 94–102.
[10]. Roberts RE, Duong HT. The prospective association between sleep deprivation and depression among adolescents. Sleep. 2014 Feb 1; 37(2): 239–44.
[11]. Dong L, Xie Y, Zou X. Association between sleep duration and depression in US adults: A cross-sectional study. J Affect Disord. 2022 Jan 1; 296: 183–8.
[12]. Zhai L, Zhang H, Zhang D. SLEEP DURATION AND DEPRESSION AMONG ADULTS: A META-ANALYSIS OF PROSPECTIVE STUDIES. Depress Anxiety. 2015 Sept; 32(9): 664–70.
[13]. Li X lin, Wei J, Zhang X, Meng Z, Zhu W. Relationship between night-sleep duration and risk for depression among middle-aged and older people: A dose–response meta-analysis. Front Physiol. 2023 Mar 2; 14: 1085091.
[14]. Li L, Wu C, Gan Y, Qu X, Lu Z. Insomnia and the risk of depression: a meta-analysis of prospective cohort studies. BMC Psychiatry. 2016 Nov 5; 16(1): 375.
[15]. Lopez R, Barateau L, Evangelista E, Dauvilliers Y. Depression and Hypersomnia: A Complex Association. Sleep Med Clin. 2017 Sept; 12(3): 395–405.
[16]. Li XL, Wei J, Zhang X, Meng Z, Zhu W. Relationship between night-sleep duration and risk for depression among middle-aged and older people: A dose-response meta-analysis. Front Physiol. 2023; 14: 1085091.
[17]. Cai Z, Ye Y, Chen S, Cai H, Lin J, Peng H, et al. U-shaped association between average daily sleep duration and depression among individuals with hypertension: a cross-sectional study based on NHANES 2017-2020. BMC Psychiatry. 2025 July 1; 25(1): 608.
[18]. Chunnan L, Shaomei S, Wannian L. The association between sleep and depressive symptoms in US adults: data from the NHANES (2007-2014). Epidemiol Psychiatr Sci. 2022 Sept 8; 31: e63.
[19]. Volkow ND, Tomasi D, Wang GJ, Telang F, Fowler JS, Logan J, et al. Evidence that sleep deprivation downregulates dopamine D2R in ventral striatum in the human brain. J Neurosci Off J Soc Neurosci. 2012 May 9; 32(19): 6711–7.
[20]. Drevets WC. Functional anatomical abnormalities in limbic and prefrontal cortical structures in major depression. Prog Brain Res. 2000; 126: 413–31.
[21]. Wise RA. Dopamine, learning and motivation. Nat Rev Neurosci. 2004 June; 5(6): 483–94.
[22]. Harrington MO, Karapanagiotidis T, Phillips L, Smallwood J, Anderson MC, Cairney SA. Memory control deficits in the sleep-deprived human brain. Proc Natl Acad Sci U S A. 2025 Jan 7; 122(1): e2400743122.
[23]. Young VM, Bernal R, Baril AA, Zeynoun J, Wiedner C, Gaona C, et al. Long sleep duration, cognitive performance, and the moderating role of depression: A cross-sectional analysis in the Framingham Heart Study. Alzheimers Dement J Alzheimers Assoc. 2025 Apr; 21(4): e70160.
[24]. Aime M, Calcini N, Borsa M, Campelo T, Rusterholz T, Sattin A, et al. Paradoxical somatodendritic decoupling supports cortical plasticity during REM sleep. Science. 2022 May 13; 376(6594): 724–30.
[25]. Yiniu W, Yuejia L. Emotional Disorders in Patients with Prefrontal Cortex Lesions. Adv Psychol Sci. 2004 Mar 15; 12(02): 161.
[26]. Hager NM, Judah MR, Milam AL. Loneliness and Depression in College Students During the COVID-19 Pandemic: the Role of Boredom and Repetitive Negative Thinking. Int J Cogn Ther. 2022; 15(2): 134–52.
[27]. Sun Y, Shi L, Bao Y, Sun Y, Shi J, Lu L. The bidirectional relationship between sleep duration and depression in community-dwelling middle-aged and elderly individuals: evidence from a longitudinal study. Sleep Med. 2018 Dec; 52: 221–9.
[28]. Sun X, Zheng B, Lv J, Guo Y, Bian Z, Yang L, et al. Sleep behavior and depression: Findings from the China Kadoorie Biobank of 0.5 million Chinese adults. J Affect Disord. 2018 Mar 15; 229: 120–4.
[29]. Gao L, Yang J, Liu J, Xin T, Liu Y. Activities of Daily Living and Depression in Chinese Elderly of Nursing Homes: A Mediation Analysis. Psychol Res Behav Manag. 2023; 16: 29–38.
[30]. Fluharty M, Taylor AE, Grabski M, Munafò MR. The Association of Cigarette Smoking With Depression and Anxiety: A Systematic Review. Nicotine Tob Res Off J Soc Res Nicotine Tob. 2017 Jan; 19(1): 3–13.
[31]. Bo Li, Han SS, Ye YP, Li YX, Meng SQ, Feng S, et al. Cross sectional associations of physical activity and sleep with mental health among Chinese university students. Sci Rep. 2024 Dec 30; 14(1): 31614.
[32]. Beurel E, Toups M, Nemeroff CB. The Bidirectional Relationship of Depression and Inflammation: Double Trouble. Neuron. 2020 July 22; 107(2): 234–56.
[33]. Mykyta L. Living Alone and Feelings of Depression Among Adults Age 18 and Older. Natl Health Stat Rep. 2024 Feb; (199): 1–11.