1. Research Background
With the continuous increase in the global number of Type II diabetes patients, this chronic metabolic disease has become an increasingly serious public health issue. Due to the significant burden that diabetes imposes on individuals' health, quality of life, and socio-economic aspects, the development of efficient health management systems is crucial. Such systems can assist patients in better controlling blood sugar, preventing complications, and adopting a healthier lifestyle more proactively.
In this context, scholars in the field of service design are actively working to improve health management systems by optimizing service touchpoints. Service touchpoints refer to all points of contact during the interaction between service providers and users, including direct interactions, telephone communications, and online platforms. For health management services, these touchpoints not only constitute the steps through which patients experience medical services but also serve as crucial criteria for assessing service quality. Therefore, when designing services for the management of Type II diabetes, focusing on and optimizing these touchpoints is particularly important for enhancing patient experience and management effectiveness.
Traditional approaches to the treatment and management of Type II diabetes revolve around medication, lifestyle adjustments, self-blood glucose monitoring, and patient education. However, inadequate design or communication issues in patient touchpoints may lead to obstacles in utilizing related services, affecting patient compliance and self-management abilities. With technological advancements, especially the widespread adoption of mobile health applications and remote monitoring devices, health management systems now have new design possibilities. These innovative technologies provide more convenient and personalized services, extending touchpoints from medical environments into patients' daily lives, presenting new design opportunities and challenges.
This study aims to comprehensively analyze how service touchpoints operate within the Type II diabetes health management system, how they influence user experience, and explore ways to enhance health management effectiveness by improving these touchpoints. The research will not only focus on the design of traditional touchpoints but will also investigate how digital tools can be effectively utilized in health management services to offer more comprehensive and personalized solutions.
2. Overview of Service Touchpoints
2.1. Definition and Development of Service Touchpoints
2.1.1. Definition of Service Touchpoints
The theory of touchpoints refers to any points of communication and interaction between consumers and service providers during the interaction process. This includes physical, personnel, scene, process, and information aspects. In service design, the touchpoint theory helps designers better understand the consumer's interaction process with the service provider, thereby creating service value, enhancing consumer satisfaction, and loyalty.
The definition of "touchpoints" in the context of service design is as follows: Touchpoint theory refers to the key interactions (interactivity) that users can perceive at the physical, digital, or psychological levels during the service process. These interactions have continuity over time (temporality), and their sum constitutes a complete user experience, influencing the user's evaluation of service quality (experiential).
2.1.2. Development of Service Touchpoints
The concept of service touchpoints originated from Norman's definition of "moments of truth" in 1982, describing critical moments of interaction between customers and service providers that significantly influence customer perception. Carlzon further identified "key moments" in airline services, where interactions between customers and the company typically last only a brief 15 seconds. Additionally, in 1982, Shostack introduced the service blueprint as a tool for designing and managing service processes, including service processes, tangible evidence, service time, and cost-benefit, with tangible evidence being the element customers use to validate service effectiveness.
In the field of service marketing, scholars expanded the concept of service touchpoints, considering it a core measure of service quality and customer satisfaction. In 1987, Surprenant et al. defined service touchpoints as a binary process of interaction between customers and service providers. The term "touchpoints" began to appear frequently in discussions on customer relationship marketing in the late 1990s and was widely introduced into academic research after 2008, although the number of academic studies remains limited.
Kronqvist et al. categorized touchpoints into three types: interaction events between service providers and customers, interaction interfaces, and communication instances through different channels. This classification explains the interactivity and physicality of touchpoints.
Service touchpoints can be defined from four different perspectives: moments, elements, interactions, and experiential views, not only elucidating the multidimensionality of touchpoints but also providing a theoretical framework for researching and optimizing customer service experiences. See Figure 1.
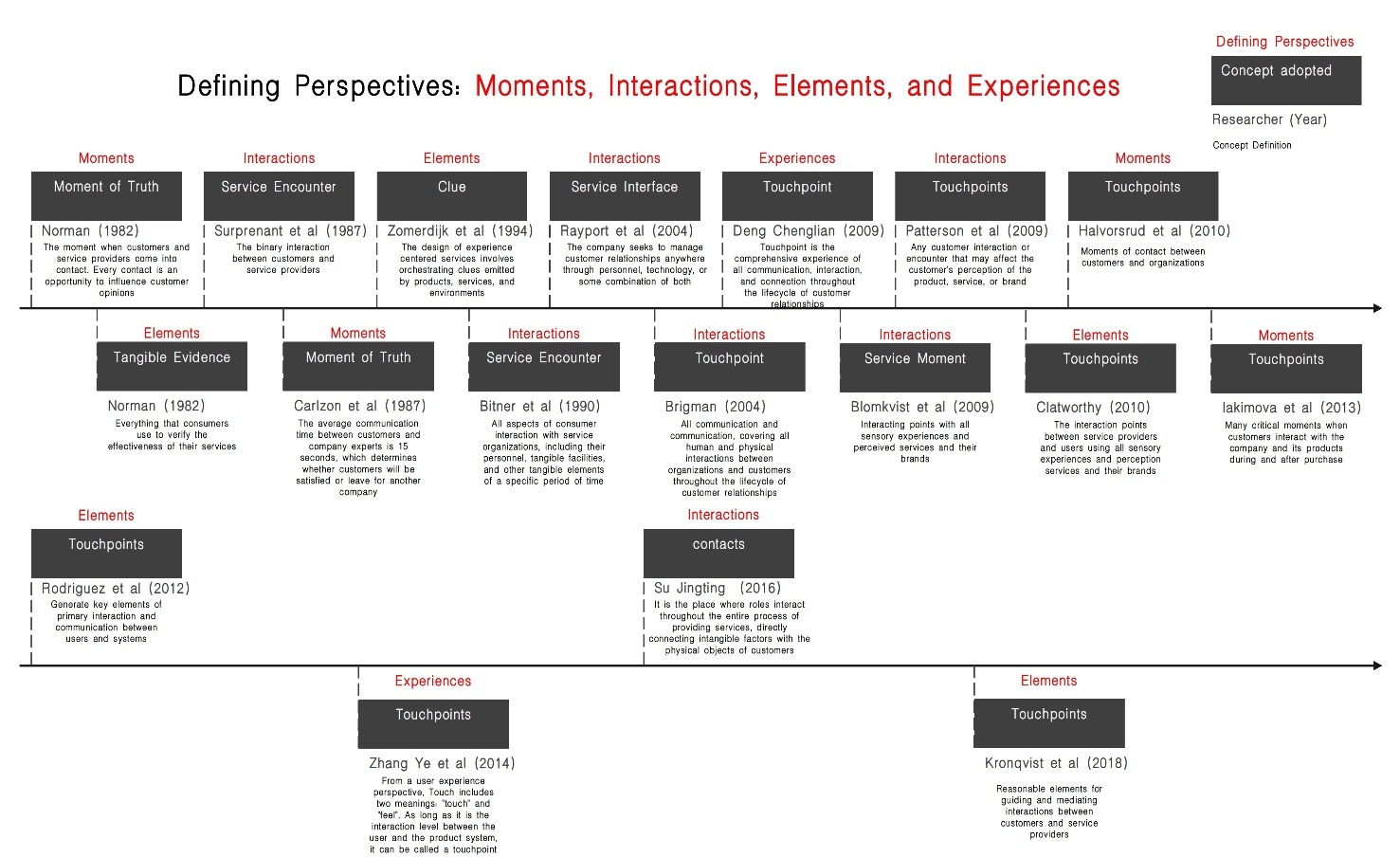
Figure 1: Development Process of Service Touchpoints
2.2. Classification of Service Touchpoints
Service touchpoints refer to different points at which customers come into contact with service providers or service systems during the process of using services. In the context of the Type II Diabetes Health Management System, these touchpoints form a crucial part of the customer experience during the glycemic control and diagnosis and treatment processes. They can be classified in various ways. The following are several common classification methods for service touchpoints:
2.2.1. Classification by Interaction Mode
Touchpoints can be classified into interpersonal touchpoints, physical touchpoints, and digital touchpoints.
Interpersonal touchpoints involve direct interactions between customers and service personnel during the service process, significantly impacting the customer experience. The attitudes, professional knowledge, problem-solving abilities, and level of personalized service provided by service personnel directly influence customer satisfaction.
Physical touchpoints involve direct contact between customers and the physical environment or products, such as store layout, ambiance, cleanliness, usability, and efficiency of self-service devices, and the appearance and packaging of products. Effective design and management of these touchpoints are crucial for customer experience and satisfaction. A comfortable environment and convenient service enhance perceived quality.
Digital touchpoints are critical service contact channels, including websites, mobile applications, and social media. Key to customer experience is smooth navigation, complete functionality, and timely interaction. Effective management of digital touchpoints aids in building long-term relationships, improving brand loyalty, and gaining insights into customer needs through data analysis.
2.2.2. Classification by Temporal Sequence
Touchpoints can be classified into pre-service touchpoints, in-service touchpoints, and post-service touchpoints based on temporal sequence.
Pre-service touchpoints refer to the moment when customers first encounter a service or brand and make purchase decisions. Key elements include advertising, creating initial impressions through visual and auditory forms; search engine optimization to ensure easy discovery when potential customers search; and online customer service to address questions during the customer decision-making process. Effective management of these touchpoints is crucial for enhancing brand awareness and promoting purchases.
In-service touchpoints affect customers' direct experiences during service reception. Factors such as in-store navigation, interaction with service personnel, and the use of self-service devices directly impact customer satisfaction. Positive in-service touchpoints deepen customers' positive experiences and enhance their loyalty.
Post-service touchpoints involve customer feedback and maintenance after service completion. Satisfaction surveys, customer support, and post-service follow-ups, such as thank-you letters or coupons, play a significant role in collecting customer feedback, providing ongoing service improvements, and enhancing customer loyalty. Effective post-service touchpoint management helps build long-term customer relationships.
2.2.3. Classification by Service Channels
Touchpoints can be classified into direct touchpoints and indirect touchpoints based on service channels.
Direct touchpoints are interaction channels between the brand and customers that do not involve third-party intermediaries, such as physical stores, direct sales, and service centers. Customers can directly experience and purchase products or obtain after-sales service. Direct touchpoints are crucial for building brand trust, enhancing customer loyalty, and improving the customer experience.
Indirect touchpoints involve customers' indirect interactions with the brand through distributors, agents, or alliance marketing partners. Brands need to ensure that these partners accurately convey their values and maintain service levels to avoid negative experiences affecting customer perceptions. Effective management of these touchpoints is key to improving customer experience and maintaining brand image.
2.2.4. Classification by Sensory Experience
Touchpoints can be classified into visual touchpoints, auditory touchpoints, tactile touchpoints, and olfactory/gustatory touchpoints based on sensory experience.
Visual touchpoints rely on various visual elements to convey the brand image and reinforce brand recognition. Brand logos serve as visual symbols with unique graphics and colors, while graphic advertisements use a powerful combination of images and text to tell the brand story. Additionally, UI design is a crucial visual touchpoint, directly influencing the digital experience quality of the brand.
Auditory touchpoints encompass all sound elements related to the brand, forming brand memories through auditory experiences. This includes waiting music for telephone services, popular advertising jingles, and even commercial advertisements on the radio. These elements, with unique melodies or iconic slogans, help customers identify and remember the brand.
Tactile touchpoints involve direct physical contact with customers. Product trials allow customers to experience the texture and functionality of products through physical touch, while interactive devices such as touch screens provide satisfying tactile feedback, increasing customer attraction and satisfaction with the product.
Olfactory/gustatory touchpoints typically appear in scenarios involving food and fragrances. For example, tasting promotions convey the taste of food, or using signature scents strengthens consumers' sensory impressions of the brand. These sensory experiences can enhance the overall customer experience and emotional connection to the brand. These are not emphasized in this study.
2.3. Application in Service Design
In service design, the concept and management of touchpoints are essential components for providing a high-quality customer experience. Touchpoints are specific moments when customers interact with the service system, encompassing all the physical, communication channels, personnel, and processes that customers use to evaluate their service experience. Service design focuses on optimizing touchpoints to ensure seamless, coherent, and satisfying experiences for customers.
When designing and developing the Type II Diabetes Health Management System with a service design mindset, the design team needs to collect and assess extensive information related to all health management touchpoints. This involves understanding and analyzing how each touchpoint can impact the experience of diabetes patients.
The design team needs to delve into understanding the impact of touchpoints on patients, including acquiring health information, using monitoring devices, and communicating with healthcare professionals. Subsequently, the team can utilize this information to optimize service delivery, such as designing easily understandable nutrition labels, creating mechanisms that encourage physical activity, or developing applications for convenient medication management. Through collaborative efforts, meeting patient needs can result in the creation of an outstanding management experience.
By applying tools from service design theory, such as patient journey maps and service blueprints, designers can systematically construct the entire diabetes management system. Patient journey maps help identify key touchpoints in managing the condition, while service blueprints ensure that these touchpoints are effectively designed and integrated into the entire service process.
3. Type II Diabetes Characteristics and Management Measures
3.1. Characteristics of Type II Diabetes
Predominantly occurring in middle-aged and elderly individuals, Type II diabetes tends to manifest after the age of 35, particularly being more common among the middle-aged and elderly population.
Gradual Progression: The course of Type II diabetes is generally longer than that of Type I diabetes, progressing slowly. Patients often experience a prolonged period without obvious symptoms.
Non-autoimmune Disease: Unlike Type I diabetes, Type II diabetes is typically not caused by the autoimmune system attacking cells producing insulin. Instead, it results from insufficient insulin secretion or insulin resistance due to various factors.
Obesity and Metabolic Syndrome: In contrast to Type I diabetes, patients with Type II diabetes often accompany obesity and metabolic syndrome, exacerbating insulin resistance.
High Controllability: Despite being a severe metabolic disorder, Type II diabetes can be controlled by adjusting diet, engaging in exercise, and receiving medication. This characteristic makes it more conducive to designing tailored intervention plans.
3.2. Common Glycemic Control Behaviors in Type II Diabetes Patients
For individuals with Type II diabetes, an effective management plan includes dietary control, moderate exercise, appropriate medication, regular monitoring, health records, and psychological support.
Dietary control is crucial and involves selecting low-fat, low-sugar foods while avoiding high-sugar, high-starch, and high-fat products. Regular, balanced meals ensuring adequate intake of proteins, healthy fats, and complex carbohydrates are recommended. Increasing the intake of vegetables and fruits provides vitamins and minerals, controls hunger, and fosters healthy dietary habits. Quitting smoking and limiting alcohol intake are also important.
Exercise plans play a significant role in improving insulin sensitivity and maintaining a healthy weight for Type II diabetes patients. Collaborating with professionals to create a sustainable exercise regimen that aligns with individual interests, suitability, and consistency is essential.
Medication treatment is determined based on the patient's blood glucose levels and the doctor's recommendations. Common treatments include oral hypoglycemic agents such as metformin, sulfonylureas, and insulin therapy. Adjustments to medication dosage should be based on regular blood glucose monitoring.
Regular blood glucose and lipid testing constitute another critical aspect of daily management for patients. This not only aids in tracking disease progression but also allows for timely adjustments to the treatment plan. Home blood glucose monitoring and routine HbA1c testing are common practices. Additionally, maintaining long-term records of health conditions and treatment processes, including medical history, prescription records, and blood glucose records, is crucial for disease management.
Psychological support is paramount in diabetes treatment. Patients should maintain a positive attitude and seek support from family, friends, and the community. Diabetes support groups offer educational resources, facilitate experience sharing, alleviate stress and loneliness, and enhance coping abilities. A comprehensive management plan should address the balance between physical and mental health, effectively control blood glucose levels, and improve overall quality of life.
4. Type II Diabetes Management System: Elements and Feedback of Service Design
4.1. Contact Elements in Service Touchpoints for Diabetes-related Health Management Design
In the design of health management for diabetes, service touchpoints refer to specific points where individuals with diabetes interact with the service system during their health management process. Effective management requires close attention to these touchpoints to ensure that individuals with diabetes receive the necessary information, support, and treatment. The following are key contact elements in the service touchpoints of diabetes health management.
Medical Professionals: Particularly doctors and nutritionists, contribute their expertise and experience to provide accurate disease diagnosis, develop targeted and actionable treatment plans, and offer personalized health education to help patients better understand their condition. The empathy and attention perceived by patients during interactions are not only in terms of technical treatment but also provide psychological support, establishing genuine trust and understanding beyond the clinical procedures.
Health Management Software and Applications: With the advancement of mobile health technology, health management software and applications can now be easily installed on mobile devices such as phones, making it convenient to record blood glucose levels and other health indicators. These applications, with user-friendly interface designs and practical features like automatic statistical analysis and personalized health advice, significantly enhance users' management capabilities and confidence in controlling their health.
Health Devices and Tools: Smart health devices available in the market, such as blood glucose meters and blood pressure monitors, can be used in conjunction with software. They are not only designed to be simple and accurate but also user-friendly. These devices serve as effective auxiliary tools for chronic disease management, allowing patients to conduct daily health monitoring at home with ease. This reduces the perceived burden of disease management and enhances patients' confidence and sense of security in controlling their own health.
Medical and Health Service Systems: The overall medical service system, whether in the form of online software platforms or offline medical institutions, is continually improving its backend operational processes to ensure consistent, timely, and efficient services. When patients realize they don't have to deal with cumbersome procedures or long waiting times, they can readily access the required services. Such an experience undoubtedly significantly increases their satisfaction with the medical system and confidence in their health management.
The experience of individuals with diabetes is a result of personalized attention, technological convenience, encouragement from the social support network, and the commitment of the entire system to efficient and quality services. When patient feedback is taken seriously and used to improve services, both patient satisfaction and health management effectiveness are enhanced.
4.2. Effect Feedback of Service Touchpoints in Diabetes-Related Health Management Design
In the design of health management for diabetes, service touchpoints refer to specific points where individuals with diabetes interact with the service system during their health management process. Effective management requires close attention to these touchpoints to ensure that individuals with diabetes receive the necessary information, support, and treatment. The following are key contact elements in the service touchpoints of diabetes health management.
Feedback between patients and the health service system is crucial at every stage of diabetes health management service touchpoints. The quality of these touchpoints determines the overall user experience for patients, contributing to continuous improvement in treatment plans and enhancing patient satisfaction and health conditions.
4.2.1. Medical Professionals
Medical professionals play a crucial role in the overall diabetes health management system as direct stakeholders responsible for providing patients with professional medical advice, constituting interpersonal touchpoints.
(1) Doctors: Provide professional diagnoses, treatment plans, and medication management.
(2) Nutritionists: Develop dietary plans to help patients control blood sugar.
(3) Nurses: Offer ongoing patient education, guidance on medication injections, and blood glucose monitoring.
4.2.2. Health Management Software and Applications
Relevant diabetes management software is downloaded onto patients' mobile devices, serving as carriers and central components of the Type II Diabetes Health Management System, acting as digital touchpoints within the health management system.
(1) Personal Health Record Apps: Help patients record blood glucose levels, dietary intake, exercise, and medication usage.
(2) Remote Monitoring Software or Websites: Used to record and transmit patients' blood glucose monitoring data for remote viewing by doctors.
(3) Mobile Health Apps: Provide lifestyle advice, medication reminders, nutritional tracking, and other functionalities.
(4) Community Support Platforms: Online support groups facilitating social interaction among patients for information sharing, experiences, and mutual encouragement.
4.2.3. Monitoring-Assistance Hardware
These assist in the control and treatment of Type II diabetes, including but not limited to blood glucose meters, insulin injection devices, and continuous glucose monitoring (CGM) systems. These serve as physical touchpoints between hardware products and patients, assisting patients in data monitoring and treatment within the Type II Diabetes Health Management System.
(1) Blood Glucose Meters: Regular and timely self-monitoring devices for blood glucose.
(2) Insulin Injection Devices: Used for insulin injection; however, patients with Type II diabetes tend to use insulin pumps less frequently. The use of insulin injections can be temporarily suspended under physician guidance based on blood glucose control.
(3) Continuous Glucose Monitoring System (CGM): Provides real-time monitoring of blood glucose levels.
4.2.4. Family and Social Support
Psychological support during the recovery and treatment process is crucial. Family members and fellow patients act as interpersonal touchpoints within the diabetes health management system.
(1) Family Members: Provide daily life support, such as meal preparation, medication management, and supervision.
(2) Social Interaction Among Patients: Local or online self-help organizations facilitating communication with similar patients for sharing experiences in managing diabetes.
4.2.5. Medical and Health Service Systems
The health management system, as the overall framework of services, has a team indirectly serving patients as the second point of contact, also known as indirect touchpoints.
(1) Regular Outpatient Services: Ensure regular assessments of treatment efficacy and adjustment of treatment plans.
(2) Hotlines and Online Consultations: Provide technical guidance and support.
The coordination of various touchpoints forms a comprehensive diabetes health management system. Through intelligent, personalized, and comprehensive service touchpoints, individuals with diabetes can effectively manage the disease and improve their quality of life. When designing diabetes health management services, ensuring seamless connections and efficient interactions among these elements is essential.
5. Conclusion
This study provides an in-depth analysis of service touchpoints within the health management system for Type II diabetes patients, encompassing medical professionals, health management software, smart hardware, and the family and social environment. Optimizing these touchpoints can enhance patients' health management outcomes, increase compliance, and alleviate the burden of the disease. Medical professionals offer professional consultation and education; health management software facilitates self-monitoring; smart hardware enables convenient scheduled monitoring and remote diagnosis; family and community environments provide life and emotional support. Through the comprehensive optimization of these touchpoints, the treatment experience for Type II diabetes patients can be improved, fostering enhancements in their health conditions.
References
[1]. Wang Yun,Zhou Yu,Yang Hai,Yan Xuedong. Integrated optimization of bus bridging service design and passenger assignment in response to urban rail transit disruptions[J]. Transportation Research Part C,2023,150.
[2]. Gu, H. (2023). Research on Shared Space Design of Urban Youth Apartments Based on Service Design: A Case Study of Longfor Crown Yu. Beauty and Time (Urban Edition), 2023(03), 46-48.
[3]. Wu, J. C., Cao, X., & Zhou, X. H. (2023). Research on Smart Museum Guided Design from the Perspective of Service Design. Packaging Engineering, 2023, 44(06), 345-347+351. DOI:10.19554/j.cnki.1001-3563.2023.06.038.
[4]. Fang, X. X., Cui, J. X., & Lin, M. Y. (2023). Research on Tourism Service Design Strategy of West Island Fishing Village in Hainan. Industrial Design, 2023(03), 112-114.
[5]. Nie, H. K., Nie, Y., Lin, J., & Ding, Y. J. (Year not provided). Exploring the Effects of Golden Chrysanthemum Root and Kidney Xiaotong Formula on CD68/iNOS and p38MAPK Signaling Pathways in Kidney Tissues of Diabetic Nephropathy Rats Based on Factorial Design. Chinese Journal of Traditional Chinese Medicine. 聂浩坤,聂远,林健,丁英钧.基于析因设计探讨金雀根及肾消通络方对糖尿病肾病大鼠肾组织CD68/iNOS和p38MAPK信号通路的影响[J].中华中医药杂Lee Jangwon,Yoon Hyoung Ki,Kim Dongho. Design of Metaverse-Based Physical Fitness Service for the Enhancement of Exercise Capability for Youth[J]. Mobile Information Systems,2023,2023.
[6]. Cerchione Roberto,Centobelli Piera,Riccio Emanuela,Abbate Stefano,Oropallo Eugenio. Blockchain’s coming to hospital to digitalize healthcare services: Designing a distributed electronic health record ecosystem[J]. Technovation,2023,120.
[7]. Szkudlarek Betina,Nguyen Linh,Leung Aegean. Effectual entrepreneurship, ethics and suboptimal service designs[J]. Journal of Knowledge Management,2023,27(2).
Cite this article
Li,Z.;Mei,Y. (2024). Analysis of Touchpoints in the Service Design of Type II Diabetes Health Management System. Advances in Humanities Research,4,44-52.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Journal:Advances in Humanities Research
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Wang Yun,Zhou Yu,Yang Hai,Yan Xuedong. Integrated optimization of bus bridging service design and passenger assignment in response to urban rail transit disruptions[J]. Transportation Research Part C,2023,150.
[2]. Gu, H. (2023). Research on Shared Space Design of Urban Youth Apartments Based on Service Design: A Case Study of Longfor Crown Yu. Beauty and Time (Urban Edition), 2023(03), 46-48.
[3]. Wu, J. C., Cao, X., & Zhou, X. H. (2023). Research on Smart Museum Guided Design from the Perspective of Service Design. Packaging Engineering, 2023, 44(06), 345-347+351. DOI:10.19554/j.cnki.1001-3563.2023.06.038.
[4]. Fang, X. X., Cui, J. X., & Lin, M. Y. (2023). Research on Tourism Service Design Strategy of West Island Fishing Village in Hainan. Industrial Design, 2023(03), 112-114.
[5]. Nie, H. K., Nie, Y., Lin, J., & Ding, Y. J. (Year not provided). Exploring the Effects of Golden Chrysanthemum Root and Kidney Xiaotong Formula on CD68/iNOS and p38MAPK Signaling Pathways in Kidney Tissues of Diabetic Nephropathy Rats Based on Factorial Design. Chinese Journal of Traditional Chinese Medicine. 聂浩坤,聂远,林健,丁英钧.基于析因设计探讨金雀根及肾消通络方对糖尿病肾病大鼠肾组织CD68/iNOS和p38MAPK信号通路的影响[J].中华中医药杂Lee Jangwon,Yoon Hyoung Ki,Kim Dongho. Design of Metaverse-Based Physical Fitness Service for the Enhancement of Exercise Capability for Youth[J]. Mobile Information Systems,2023,2023.
[6]. Cerchione Roberto,Centobelli Piera,Riccio Emanuela,Abbate Stefano,Oropallo Eugenio. Blockchain’s coming to hospital to digitalize healthcare services: Designing a distributed electronic health record ecosystem[J]. Technovation,2023,120.
[7]. Szkudlarek Betina,Nguyen Linh,Leung Aegean. Effectual entrepreneurship, ethics and suboptimal service designs[J]. Journal of Knowledge Management,2023,27(2).