1. Introduction
With the continuous progress of science and technology and people's increasing concern for sports and health, people have higher requirements for the accuracy and professionalism of monitoring equipment, conventional sports monitoring methods can no longer meet people's needs, and wearable technology has gradually become a concern. As an emerging technology, flexible wearable biosensors can real-time, accurate monitoring of the body's physiological conditions during exercise, providing an effective tool for sports training and health management. Wearable flexible biosensors have wide applicability in exercise monitoring applications. Whether it is step counting and sleep monitoring in daily life or training data analysis for professional athletes, wearable flexible biosensors are able to meet the demand. Through real-time monitoring of sports status and body parameters, wearable flexible biosensors can help users understand their sports conditions and provide personalised health advice and training guidance to improve their sports performance and health. Compared with traditional hard sensors, flexible biosensors have better deformability and flexibility, and can more accurately obtain human movement information. At the same time, the characteristics of flexible materials also make the sensor can be closely integrated with the human body, which can provide a comfortable wearing experience and will not cause interference to the movement, people will be more willing to wear and use, which provides a more portable option for sports monitoring and more reliable data support. However, wearable flexogen sensors currently face some challenges in motion monitoring. The stability and precision of the sensors need to be further improved to ensure the accuracy and reliability of the data.
This paper introduces three types of wearable flexible biosensors for blood oxygen saturation monitoring, skin temperature monitoring and heart rate monitoring, respectively. It also describes in detail the components of these wearable biosensors, device structure, and working principle.
Wearable flexible biosensors have great potential and value in motion monitoring applications. Through further research and development, it is believed that it can play a greater role in the field of exercise monitoring in the future and bring more convenience to people's healthy life.
2. Biosensors used to monitor blood oxygen saturation
Blood oxygen saturation measurement is usually divided into electrochemical and optical methods. The electrochemical method is based on the sampling of human blood for electrochemical analysis using a hematology analyzer, and the optical method is based on the non-invasive measurement of the difference in light absorption between oxyhemoglobin and deoxyhemoglobin in blood at different wavelengths. Since our research is based on a wearable flexible monitoring device during motion, we choose optical method sensors here.
Oximetry is generally achieved by the device called Pulse Oximeter. Its working principle is based on the light-absorbing properties of hemoglobin. Hemoglobin is an important molecule in the blood that carries oxygen, and it can combine with oxygen to form oxyhemoglobin, when oxygen binds to hemoglobin, the absorption spectrum of hemoglobin changes. Pulse oximeters use this property to measure blood oxygen saturation. A pulse oximeter typically consists of an infrared light source and a light sensor. The infrared light source tends to emit two different wavelengths of light, one wavelength closer to the absorption peak of hemoglobin and the other unaffected by hemoglobin absorption. These two types of light pass through the skin surface into the blood and are then received by the photosensor. When the oxygenated hemoglobin in the blood meets a wavelength close to the light emitted by the infrared light source, it absorbs more light. In comparison, the deoxygenated hemoglobin in the blood absorbs less light. By measuring the difference in the amount of light absorbed by the two wavelengths emitted by the infrared light source, the pulse oximeter can calculate the percentage of oxygenated hemoglobin in the blood and thus obtain a value for oxygen saturation[1].The detection mechanism of the blood oxygen detector and the PPG signal are as shown in Figure 1.
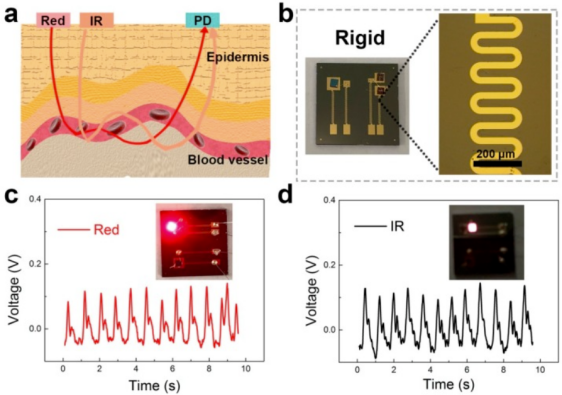
Figure 1. Detection mechanism of the blood oxygen detector [2].
Yuanyuan He, Di Yu, Jiaheng He et al. [3]designed an IoT-based wearable blood oxygen saturation and heart rate real-time monitoring system. Their system collects the photoelectric pulse wave signals detected by optical sensors through a terminal bracelet, and then obtains more accurate heart rate and blood oxygen saturation values after low-pass filtering and dynamic motion compensation processing, and sends them to the cloud platform through the network combined with the positioning information, and manages them using the back-end database, and finally extracts them to the user's cell phone client applet or computer terminal for display. Their system test results show that the network communication error rate of the system is 0; compared with the same type of bracelets, the error of heart rate and blood oxygen saturation detected by the system bracelet is less than 2%, so it has important research significance for real-time monitoring of sports that need high accuracy. Haiming Ai,Fulai Peng, Minlu Hu et al.[4] used a dual-wavelength light emitting diode (LED) as the light source to irradiate the finger in turn, and detected the volumetric pulse wave, pulse rate and oxygen saturation by photodetector of the emitted light. Since the wavelength of the light source is easily shifted by temperature changes and the LED light source is usually not purely monochromatic, they decided to choose the wavelength of the light source in the region of gentle changes in the absorption coefficient of hemoglobin, i.e., 660 nm and 940 nm for red light and near-infrared light, respectively. The AFE4400 series chip with integrated LED driver and signal conditioning circuit was used to improve the system performance, reduce power consumption and design complexity while monitoring the blood oxygen signal in real time. The experimental results show that the correlation coefficient of blood oxygen measurement is 0.995, so it can be considered as a high accuracy. It can be applied to sports real-time monitoring wearable devices.
The future research of blood oxygen saturation monitoring will focus on miniaturization and portability, multi-functional, accuracy improvement and personalized health management. As technology advances, oximeters will tend to be more compact and portable, making it convenient for users to perform oximetry anytime and anywhere. This will promote the popularity of blood oxygen monitoring and the expansion of applications. Future oximeters may integrate more functions, such as heart rate monitoring, sleep quality assessment, and exercise monitoring. This will give users a more comprehensive understanding of their health status and take appropriate measures to improve it. Future blood oxygen detectors may further improve the accuracy and stability of measurement to meet the needs of clinical medicine and health management. Continuous technological innovation and algorithm optimization can improve the accuracy and sensitivity of blood oxygen detection. Future blood oxygen detectors may combine personal health data and lifestyle habits to provide users with personalized health management solutions. More refined and customized health advice can be provided based on individual characteristics and needs through deep learning and other artificial intelligence technologies.
3. Biosensors used to monitor skin temperature
The flexible temperature biosensor is a flexible and bendable sensor for measuring the temperature of the environment or an object. It is made of a flexible material that is highly deformable and adaptable to contact with curved or curved objects. Flexible temperature biosensors usually use thermosensitive materials or thermistors to measure temperature. The resistance value or other electrical properties of these materials change accordingly to the temperature. The temperature of the environment or object can be calculated by measuring the change in resistance or other electrical properties. The advantages of flexible temperature biosensors are that they can adapt to irregular surfaces and curved shapes, can operate over a wide temperature range and have a high sensitivity and response rate. They are often thin, lightweight, soft and comfortable, and can be applied in contact with human skin or attached to the surface of an object.
There are currently two approaches, the first is to assemble devices using conductors that can be stretched, usually made by mixing a conductive substance into a flexible base [5]. The second is the direct bonding of thin conductive materials with low Young's modulus to a flexible base. From a study by Tan and others, they applied the second method to make biosensors. This biosensor comprises four layers: insulating, sensitive, conductive silver wire, and flexible PET (polyethylene terephthalate substrate). The PET is plasma oxygenated to make its surface rough. Conductive silver gel electrodes are then coated onto the PET substrate, coated with a carbon material suspension, encapsulated with RGO (Reduced Graphene Oxide), and finally an insulating layer . This biosensor has many advantages, such as the good TCR (temperature coefficient of resistance) of the RGO material as a sensitive layer, the good linearity of the temperature-resistance curve in experiments, and the good response time and response time in temperature response tests. Due to the tape press encapsulation technique, the RGO layer spacing is significantly reduced, the sensor's resistance is not affected by the applied stresses and, due to the insulation layer, the external humidity does not affect the resistance or the sensor performance .The detecting process of the PET method is as shown in Figure 2.
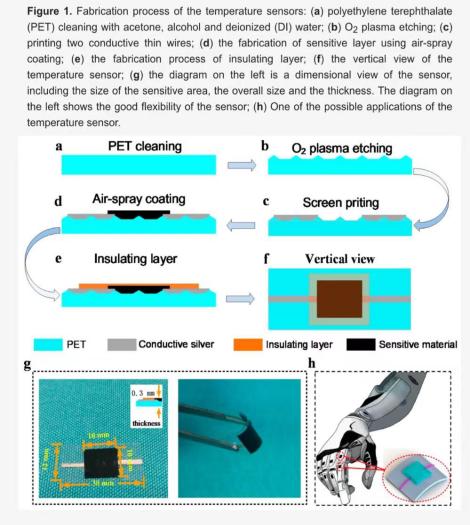
Figure 2. The detecting process of the PET method [6].
Skin temperature biosensor can play an important role in many fields, firstly body temperature is an important health indicator and flexible biosensors are so sensitive to changes in temperature that they can capture subtle temperature changes that allow doctors to assess changes in the physiological characteristics of the human body, such as the thermal conductivity of human tissues, skin water content, blood flow and wound repair processes [7]. For example, during the new coronavirus outbreak in 2020-2022, doctors could use flexible sensors to monitor a patient's temperature and other health indicators in real time without disturbing the patient's rest.
In sports, wearable flexible biosensors also have an important role to play. Flexible biosensors can collect physiological signals from all directions, at multiple levels and from multiple angles, during the athletes' movement to build a database of high-level athletes, and through a large amount of data analysis, monitor the athletes' physiological indicators in real-time, reasonably predict the potential risk of injury during the athletes' training, reduce the athletes' risk of injury This will help to reduce the risk of injury and to develop a more scientific training plan for athletes [8]. Under normal physiological conditions, body temperature can be affected by day and night, age, gender, environment, temperature mental and physical exercise conditions, but body temperature but fluctuates little, so if the body temperature if increased will change the body's ability to exercise. When exercising in a thermal ring, a sharp rise in body temperature increases the probability of shock, and the brain is very susceptible to damage when the body temperature is too high[9]. Damage to the brain caused by hyperthermia may be one of the causes of heat stroke[10] . High body temperatures reduce the body's ability to perform long-term work and can cause significant damage to the cardiovascular system. As a result of dynamic exercise in a hot environment, the cardiovascular system is subjected to heavier load loads, such as accelerated blood flow through the skin to disperse heat and accelerated oxygenation of the muscles to fill their new age. As peripheral blood circulation increases, blood volume increases, leading to a decrease in intracardiac blood volume, a decrease in stroke output and an increase in compensatory heart rate [11]. Therefore, using flexible temperature sensors for real-time body temperature monitoring is essential. Many consumer electronic products now use this technology of flexible temperature sensors, such as sports bracelets and watches, which allow more sports enthusiasts and ordinary consumers to enjoy the benefits of technology for life and health.
4. Biosensors used to monitor heart rate
Wearable heart rate monitors have changed the way we monitor and track cardiovascular health. These devices detect and measure the electrical activity of the heart and are called heart rate monitors. The wearable heart rate detector uses sensors in direct contact with the skin and various methods to record and analyze heart rate data.
The most widely used detection technique today is photodensitometry (PPG), which uses light-emitting diodes (leds) and photodiodes to monitor changes in blood volume. The amount of light absorbed by the blood and the blood flow in the capillaries under the skin change with the heartbeat. These changes are detected by the wearable's photodiode, which then converts them into electrical pulses. These signals are then processed and used to calculate heart rate. ppg based heart rate monitors are widely used in fitness trackers and smartwatches due to their non-invasive nature and ease of use.
The electrocardiogram (ECG) is another instrument that is becoming increasingly popular. An electrocardiogram measures the electrical impulses produced by the heart. In an ECG based heart rate monitor, electrodes in the wrist or chest capture electrical pulses. Electrodes can detect and amplify the smallest electrical changes on the skin's surface. However,
The enhanced signals were then analyzed to accurately calculate the heart rate. Due to their high accuracy, ECG based heart rate monitors are often used in medical Settings and professional sports.
Advanced wearables may include additional accelerometers or gyroscopes to improve the accuracy of heart rate monitoring and account for motion distortion. These sensors detect and quantify movement, allowing the device to filter out noise caused by movement and provide more accurate heart rate measurements. These wearable heart rate trackers provide reliable data even during intense exercise by calculating exercise artifacts, making them beneficial for fitness enthusiasts and sports. Aiming at the low accuracy of heart rate measurement in current wearable heart rate detection devices under exercise conditions, a deep learning algorithm combining convolutional neural network with sequence-to-sequence network (CNN-seq2seq) was proposed to extract heart rate in photoplethysmograph (PPG) under exercise conditions Method of value. Combined with the features of convolutional neural network in feature extraction and the advantage of long short-term memory network in time series data processing, a network model of convolutional neural network combined with sequence-to-sequence + attention mechanism is established. Methods The PPG signals of 30 healthy subjects were collected at rest, walking, jogging and fast running, and their electrocardiogram (ECG) signals were collected synchronously by an electrocardiogram device with anti-interference capability. The PPG signals were used as neural network input signals, and the ECG signals were simplified and retained The CNN-seq2seq network is then trained, and the network outputs PPG-like signals with accurate heart rate characteristics, so as to achieve heart rate measurement under exercise conditions. CNN-seq2seq network output and the corresponding ECG signal were used to calculate the heart rate per minute. The mean error and mean square error of heart rate estimation were 0.25±1.31. The experimental results show that CNN-seq2seq network model can obtain ideal results for the prediction of exercise heart rate. This provides a feasible scheme for portable measurement of exercise heart rate[12].
Wearable heart rate monitors have a wide range of uses. These gadgets allow people to track their heart rate while exercising, provide accurate data and recommendations on their level of physical activity, and enhance their exercise habits in the areas of fitness and sports. To achieve the best results, athletes can monitor their performance and adjust their intensity by focusing on their target heart rate zone. Fitness enthusiasts can also set goals, monitor their progress, and make clearer decisions about what workouts to do.
Medical organizations are also finding important uses for wearable heart rate monitors. A good example of its use in practice is remote patient monitoring. Patients can continuously monitor their heart rate with the convenience of a heart rate monitor at home. This allows doctors to remotely assess a patient's cardiovascular health, identify any abnormalities or irregularities, and seek immediate medical assistance if necessary. This remote monitoring enhances patient convenience while also enabling proactive medical care and reducing the frequency of hospital visits. [13] Heart rate refers to the number of beats of the heart in 1min under peaceful conditions, and the changes of heart rate and other parameters can reflect the operation of various functions of the human body. This paper designs a single chip microcomputer heart rate detection system whose core component is STC89C52. By means of different electrical signals generated by photoelectric sensors, the electrical signals are sent to the single chip microcomputer for analysis and processing, so as to measure the user's heart rate indirectly. This system can improve the portability and accuracy of the heart rate detector, and reduce the cost.
In short, a wearable heart rate device can detect and measure the electrical activity of the heart. With technologies such as PPG and ECG, these devices can accurately and consistently measure heart rate. The practical application of wearable heart rate monitors has evolved into an important tool for enhancing cardiovascular health and well-being, from fitness tracking and exercise performance improvement to remote patient monitoring and proactive healthcare.
5. Conclusion
This study found that optical sensing technology is the most commonly used detection technology when monitoring blood oxygen saturation. Its sensors usually use infrared and red light through the skin to measure oxygen saturation in the blood. In recent years, researchers have improved the measurements' accuracy and stability by improving the sensors' design and algorithms. To improve the accuracy of the oximetry measurements, the researchers also optimized the algorithms of the sensors. Using machine learning and deep learning techniques, sensor data can be analyzed and processed more accurately, reducing errors and providing more accurate results.Common biosensing technologies used in monitoring skin temperature include thermistors, infrared, and thermocouples. Thermistors are among the most commonly used technologies, which utilize the change in resistance of a material with temperature to measure skin temperature. Infrared technology, on the other hand, estimates skin temperature by measuring infrared radiation from the skin surface.
On the other hand, thermocouple technology utilizes the voltage difference created by the difference in the conductive ability of two different materials to measure temperature. Skin temperature monitoring wearable sensors have a wide range of applications in medical, sports, and sleep monitoring areas. Especially in sports, real-time temperature monitoring can be a good way to prevent athletes from becoming overdrawn, thus avoiding injuries and illnesses, and can provide athletes with personalized exercise and rest recommendations based on real-time body temperature changes.For monitoring heart rate, the biosensors they use usually employ electrodes in contact with the skin to measure ECG signals to calculate heart rate. This technology has a high degree of accuracy, but requires full contact with the skin and therefore may be disturbed during exercise. In recent years, heart rate monitoring sensors during exercise are usually connected to a smartphone or other device that can monitor heart rate data in real time and analyze and display the data through an app. This allows users to keep track of their heart rate changes and conduct exercise training and health management based on the data.In general, researchers at home and abroad have made a lot of progress in the study of sensors for monitoring physiological parameters during exercise. These researches are significant for improving people's sports health and monitoring their physical conditions. However, further research and development are still needed to improve the sensors' accuracy, comfort, and reliability to meet the needs in different exercise scenarios.
Authors Contribution
All the authors contributed equally and their names were listed in alphabetical order.
References
[1]. Zhang L. 2021. Chongqing University of Technology.
[2]. Huamin C,Yun X, Jiushuang Z... & Guofeng S. 2019. 5.
[3]. Yuanyuan H, Yu D, Jiaheng H. et al. 2023.Internet of things technology,13(02):59-62+65.
[4]. Ai H-M, Peng F-L, Hu M-L, et al. 2020 Sensors and Microsystems, 39(07):92-94+97.
[5]. Lee P; Lee J; Lee H; Yeo J; Hong S; Nam K. H; Lee D; Lee S. S; Ko S. H. Adv. Mater. 2012, 24, 3326.
[6]. Liu G, Tan Q, Kou H, Zhang L, Wang J, Lv W, ... & Xiong J. 2018. Sensors, 18(5), 1400.
[7]. Hattori, Y.; Falgout, L.; Lee, W.; Jung, S. Y.; Poon, E.; Lee, J. W.; Na, I.; Geisler, A.; Sadhwani, D.; Zhang, Y. H.; Su, Y. W.; Wang, X. Q.; Liu, Z. J.; Xia, J.; Cheng, H. Y.; Webb, R. C.; Bonifas, A. P.; Won, P.; Jeong, J. W.; Jang, K. I.; Song, Y. M.; Nardone, B.; Nodzenski, M.; Fan, J. A.; Huang, Y. G.; West, D. P.; Paller, A. S.; Alam, M.; Yeo, W. H.; Rogers, J. A. 2014 Adv. Healthcare Mater. , 3,1597.
[8]. Bingtian S, Jianliang L, Huihua X, Ze X, Jianxin M, Xiaoping C,and Fengyu L.2022. Science China: Information Science, 52, 54-74.
[9]. Brinnel H, CabanacM, Hales YRS. 1987,Amsterdam: Excerpta Madica, 209-240.
[10]. Hales JRS, Hubbard RW, Gaffin SL.1996,New York: Oxford Universitv Press. 285-355.
[11]. Rowell LB. 1986,NewYork:Oxford University Press,363-406.
[12]. Kai Q, Xu Z, Jiaqi G & Junfeng G.2021. Journal of South-Central University for Nationalities, 05, 489-495.
[13]. Guangjing Z, Ming Z, Youhao Z, & Mengyao X. 2021. Intelligent computer and application, 5, 4.
Cite this article
Sun,H.;Xu,Z.;Zhou,R. (2024). Flexible wearable biosensor for physiological parameters monitoring during exercising. Applied and Computational Engineering,32,117-123.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 2023 International Conference on Machine Learning and Automation
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Zhang L. 2021. Chongqing University of Technology.
[2]. Huamin C,Yun X, Jiushuang Z... & Guofeng S. 2019. 5.
[3]. Yuanyuan H, Yu D, Jiaheng H. et al. 2023.Internet of things technology,13(02):59-62+65.
[4]. Ai H-M, Peng F-L, Hu M-L, et al. 2020 Sensors and Microsystems, 39(07):92-94+97.
[5]. Lee P; Lee J; Lee H; Yeo J; Hong S; Nam K. H; Lee D; Lee S. S; Ko S. H. Adv. Mater. 2012, 24, 3326.
[6]. Liu G, Tan Q, Kou H, Zhang L, Wang J, Lv W, ... & Xiong J. 2018. Sensors, 18(5), 1400.
[7]. Hattori, Y.; Falgout, L.; Lee, W.; Jung, S. Y.; Poon, E.; Lee, J. W.; Na, I.; Geisler, A.; Sadhwani, D.; Zhang, Y. H.; Su, Y. W.; Wang, X. Q.; Liu, Z. J.; Xia, J.; Cheng, H. Y.; Webb, R. C.; Bonifas, A. P.; Won, P.; Jeong, J. W.; Jang, K. I.; Song, Y. M.; Nardone, B.; Nodzenski, M.; Fan, J. A.; Huang, Y. G.; West, D. P.; Paller, A. S.; Alam, M.; Yeo, W. H.; Rogers, J. A. 2014 Adv. Healthcare Mater. , 3,1597.
[8]. Bingtian S, Jianliang L, Huihua X, Ze X, Jianxin M, Xiaoping C,and Fengyu L.2022. Science China: Information Science, 52, 54-74.
[9]. Brinnel H, CabanacM, Hales YRS. 1987,Amsterdam: Excerpta Madica, 209-240.
[10]. Hales JRS, Hubbard RW, Gaffin SL.1996,New York: Oxford Universitv Press. 285-355.
[11]. Rowell LB. 1986,NewYork:Oxford University Press,363-406.
[12]. Kai Q, Xu Z, Jiaqi G & Junfeng G.2021. Journal of South-Central University for Nationalities, 05, 489-495.
[13]. Guangjing Z, Ming Z, Youhao Z, & Mengyao X. 2021. Intelligent computer and application, 5, 4.