1 Introduction
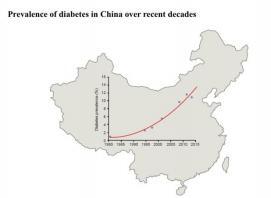
Diabetes has become an increasingly serious global public health problem, and China is one of the countries with the fastest increasing prevalence of diabetes [60], with urban prevalence higher than rural prevalence [16].
|
|
Figure 1. Prevalence of diabetes in China over recent decades [56] |
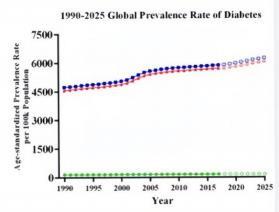
Figure 2. 1990-2025 Prevalence Rate of Diabetes [50] |
According to the latest data released by the International Diabetes Federation (IDF), there will be about 537 million patients worldwide by 2021 [37]. The number of people with diabetes in China is 141 million, with a prevalence rate of 12.8% (Li et al., 2020), equivalent to 1 in every 10 people with diabetes. Among them, more than 90% are type 2 diabetes (Li et al., 2020). The international prevalence of diabetes currently stands at 9.3%, which means that more than 400 million people worldwide have diabetes [71], and this is still a relatively conservative estimate. At the same time, the global prevalence of diabetes is increasing year by year [44], and the trend is still increasing in the coming decades.
Diabetic patients are more likely to develop mood disorders [10].
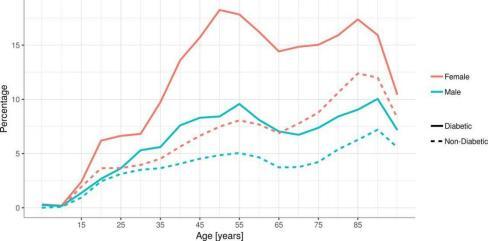
Figure 3. Percentage of patients with diabetes diagnosed with major depressive disorders compared with patients without diabetes. [15]
The study showed that the incidence of moderate and mild psychological disorders in patients with diabetes was 23.6%, and the incidence of moderate and severe psychological disorders was 19.5%. The incidence of depression and anxiety in hospitalized diabetic patients was 22.5% and 35%, both of which were significantly higher than the normal population (Bilibili 2022). An epidemiological study from the United States and a controlled study from India both point to one fact - people with type 2 diabetes are more likely to develop mood disorders, with depression receiving the most attention (Thepaper 2021). Statistics from the United States show that in 2019, the depression prevalence in adult patients with type 2 diabetes was 24.7%, while this figure was only 17.9% in the adult population without diabetes (Diabetes Status 2019).
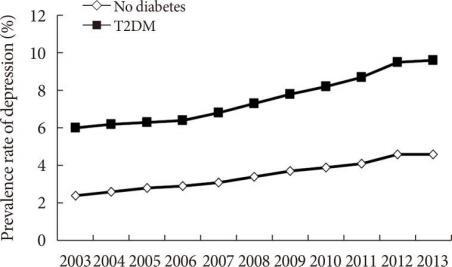
Figure 4. Annual prevalence rates of depression in patients with type 2 diabetes mellitus (T2DM) and the general population without T2DM in Korea, 2003 to 2013. [45]
The purpose of this project will be to identify the various causes of diabetes, and this essay will discuss how diabetes and other factors would affect the occurrence of anxiety and depression in a population. Also evaluate the significance of diabetes on the occurrence of anxiety and depression. And proposed strategies to reduce the occurrence of anxiety and depression od diabetics. In fact, this part is very important for social development, and it would be very meaningful if some strategies can be used to alleviate the occurrence of anxiety and depression in patients to some extent.
2 Research review
2.1 What is diabetes
Type-1 diabetes, previously recognized as insulin-dependent diabetes, is a metabolic disorder marked by elevated blood sugar levels due to a complete absence of insulin. This condition primarily results from the immune-mediated destruction of pancreatic beta cells [2].
Type-2 diabetes, once termed non-insulin-dependent or adult-onset diabetes, is a chronic metabolic disorder predominantly manifesting in individuals aged 35 to 40 years and older, comprising over 90% of diabetes cases (Zhao, 2018).
Further details effect/ causes are highlighted in appendix titles Types of diabetes
2.2 Causes of diabetes
Overall, a blend of genetic and environmental elements plays a significant role in diabetes development [3]. Inefficiencies in blood glucose utilization and storage arise primarily due to reduced insulin secretion, a result of pancreatic islet cell dysfunction, or because of the body's insensitivity to insulin, or a combination of both (Cornelis et al., 2014). Presently, the molecular origins of most diabetes cases remain obscure, barring a few specific types with a well- understood molecular basis [78]. There exists a genetic predisposition to diabetes, evident in familial patterns. Yet, epidemiological and clinical studies have definitively shown that the principal catalyst for type 2 diabetes is an unhealthy lifestyle (Yuan, 2020). To curb the prevalence of diabetes, a fundamental approach would be to improve the social environment that fosters poor lifestyle choices.
2.2.1 Genetic factors
The presence of diabetes in the immediate family significantly increases the probability of the offspring developing diabetes, which is known as genetic susceptibility, while diabetes itself is not a genetic disease [27]. In type 2 diabetes, genetic factors account for a large proportion of the total factors in the development of the disease [3]. Diabetes is a polygenic genetic disease, and genetic factors account for a high proportion of the development of diabetes [62]. Among them, type I diabetes has been clarified that there are several DNA loci involved in the pathogenesis, the most representative of which is the polymorphism relationship of the DQ locus in the HLA antigen gene, which is most closely related to the pathogenesis of diabetes [32]; type II diabetes is associated with mutations in some of the genes, including insulin genes, glucokinase genes, insulin receptor genes, mitochondrial genes, etc., [5] and the mutation of these genes will lead to diabetes and the mutated genes can be passed on to the next generation through germ cells, significantly increasing the risk of diabetes in the next generation (Sun, 2018).
The causes of the development of diabetes mellitus are not only related to heredity, but also to surroundings and the acquired lifestyle of the patient, which together determine the onset and course of diabetes mellitus.
2.2.2 Lifestyle
2.2.2.1 Diet
Diet is a major factor of diabetes, especially dishes that contains much lipids, salt and sugar, which is a very easy cause of diabetes. Obesity is also likely to lead to diabetes [36], and many bad eating habits will lead to obesity and increase the risk of diabetes. For instance, consuming an excessive amount of food for dinner can coincide with the peak insulin levels in the blood during the evening. This heightened insulin can convert blood sugar into fat, which may then accumulate on the walls of blood vessels, so eating too much dinner will be obese over time [47], obesity, especially abdominal obesity, is more likely to lead to insulin resistance. Insulin resistance refers to the body's reduced sensitivity to insulin, resulting in the body cannot effectively use glucose, the hand is reduced glucose tolerance, prone to diabetes [9]. Type 2 diabetes arises when the body's ability to counteract insulin resistance falters. This occurs as the functionality of pancreatic cells diminishes, leading to inadequate insulin secretion that cannot offset insulin resistance (Li, 2020).
2.2.2.2 Physical activities
Lack of exercise is also an important cause of elevated blood glucose, long-term sedentary easily lead to body obesity, and obesity is an important factor causing elevated blood glucose [66], so the chances of developing diabetes will be higher. If long-term sedentary, the body consumes very little energy, there is not enough exercise to the body's fat substances, sugar substances to consume, long-term health problems may occur, and even blood lipids, blood pressure, blood sugar fluctuations [54]. Therefore, in order to effectively control blood sugar and prevent diabetes from appearing in ordinary life, you should participate in more sports as appropriate, and promote physical health through reasonable exercise, which is also a way to control blood sugar (Zhang, 2020).
2.2.2.3 Mental stress
When people are subjected to sudden psychological stress, the body's immediate reaction is to resist [35], when the adrenal glands secrete adrenaline and the liver releases stored glucose in anticipation of sudden muscular action, so that there is an increase in blood glucose, and thus there is a certain chance of developing diabetes [69]. Diabetes is an incurable disease that usually lasts a lifetime, and many patients who are psychologically fragile may have a tendency to become anxious and depressed [59].
2.2.2.4 Psychoactive drugs
Certain psychoactive drugs such as cigarettes, alcohol, caffeine and nicotine increase the risk of diabetes [79]. Prolonged or excessive alcohol consumption can be a contributing factor to diabetes. Excessive alcohol intake can impair pancreatic islet function, thereby disrupting sugar metabolism in the human body. When sugar metabolism is disturbed, the risk of developing diabetes increases (Zhao, 2018). At the same time, according to domestic and foreign studies, smoking will lead to an increase in the prevalence of type 2 diabetes, and will increase or aggravate the complications of patients with diabetes, the most common is cardiovascular and other fatal diseases, and even increase the risk of death [70]. So far, the mechanism of the impact of smoking on diabetes is not clear, but it is clear that the nicotine, carbon monoxide, and coal tar contained in cigarettes will destroy the pancreatic cells of the body, thus damaging the function of the pancreas, and the normethyline will also increase blood sugar and blood pressure, so that the stability of blood sugar is destroyed, and the chance of diabetes is increased [77]. If someone drinks a lot of alcohol and smokes at the same time for a long time, the probability of developing diabetes will be greatly increased [70]. Also, because coffee contains a large amount of caffeine, can stimulate the sympathetic nerve excitement of the human body, so that people are excited, heartbeat faster, if drinking too much may make blood sugar and diabetes patients blood sugar, blood lipid rise, and will increase the burden of the kidney, make diabetes patients worse [26].
2.3 Anxiety and depression
2.3.1 Anxiety
Anxiety refers to anxiety disorder, which is a mental disorder mainly manifested by anxiety in the absence of organic brain diseases or other neurological diseases [11]. It may be related to genetic factors. Manifested as nervousness, fear and other symptoms. It can be treated with drugs. Typical anxiety disorders encompass generalized anxiety disorder, social anxiety disorder, separation anxiety disorder, among others, as delineated by Franz et al. in their 2013 study. The pathogenesis of anxiety is not clear, may be related to genetics, hyperfunction of the norepinephrine system, psychological factors and other reasons, trauma, serious diseases, caffeine addiction and other factors may increase the risk of disease [11]. Anxiety disorders are characterized by persistent or flare-up of inexplical anxiety, tension, restlessness, fear, and symptoms such as flushed face, sweating, palpitations, choking, hyperventilation, and slight tremors in the limbs [11].
2.3.2 Depression
Depression, a common manifestation of depressive disorders, is a mental illness prevalent globally with a high potential for clinical recovery. However, in China, due to limited disease awareness, there's a lower adherence to formal treatment, resulting in a low treatment rate and high recurrence (Li, 2016). Clinically, depressive disorders are categorized into mild, moderate, and severe based on symptom number, type, and intensity [94]. Furthermore, considering the unique characteristics of specific populations, depression is further divided into categories like elderly depression, childhood depression, and postpartum depression (Li, 2016). Depression's manifestations encompass three groups: core symptoms, psychological symptoms, and physical symptoms, with depressive episodes typically marked by low mood, slowed thinking, and diminished volitional activity (Li, 2016). These three symptoms are considered classic symptoms of major depression, but these classic symptoms do not necessarily occur in all patients.
2.4 The causes of anxiety and depression
2.4.1 Genetic factors
2.4.1.1 Anxiety
There has been sufficient data to support that heredity plays a certain role in the occurrence of anxiety disorders [29]. The prevalence rate among first-degree relatives of patients with generalized anxiety disorder is 19.5%, which is much higher than that of the general population [13]. In the investigation of twins, the prevalence rate of monozygotic twins is much higher than that of dizygotic twins [63]. Anxiety has a clear genetic predisposition, with a heritability of 30%, and it is not thought to be influenced by family and environmental factors [74]. However, some studies have suggested that genetic predisposition is mainly seen in panic disorder, while it is not evident in generalized anxiety disorders [42]. The survey found that the prevalence rate of anxiety disorder among blood relatives is 15%, higher than the prevalence rate of general residents, as a predisposing factor of anxiety personality, has a certain genetic tendency, the parents of anxiety patients also have anxiety state or anxiety character [63].
2.4.1.2 Depression
Depression is also influenced by genetics 1. Genes and genetic factors: No single gene had been identified as the main cause of depression. To some extent, genetic susceptibility may be the result of subtle, synergistic and reciprocal effects of multiple genes [34]. 2. Family studies: Studies have shown that first-degree relatives of patients with recurrent depression are 2-4 times more likely to suffer from depression than the control group [64]. 3. Twin studies: Twin studies of recurrent depression suggest that the heritability is close to 37%. 4. Molecular genetic association studies: Molecular genetic studies have examined that the tendency of genes to be inherited simultaneously in family 2 is higher than that of chance occurrence. No major loci have been identified, but10 microloci or susceptibility loci have been detected (Xu, 2017).
2.4.2 Lifestyle
2.4.2.1 Anxiety
Certain factors may elevate the risk, including trauma, severe illness; compromised health; accumulated stress; coexisting mental illnesses (like depression); substance use or misuse, including drugs or alcohol; consumption of addictive substances such as caffeine and nicotine; and the individual's personality traits (Wang, 2015).
2.4.2.2 Depression
The etiology and pathogenesis of this disorder remain somewhat elusive, yet a wealth of research data, including Li's 2016 study, indicates that genetic factors, neurobiochemical elements, and psychosocial influences significantly impact its development. Current evidence also links stressful life events, pessimistic personality traits, a history of other mental disorders, serious chronic illnesses, alcohol misuse, and drug abuse closely with the onset of depression (Li, 2016)
2.4.2.3 Psychoactive drugs
Smoking and drinking are bad habits in many people's daily life, and long-term smoking and drinking will produce physical and psychological dependence [7]. Tobacco dependence is a chronic disease with high recurrence, the essence is dependence on nicotine, long-term smokers need higher nicotine concentration to get the same pleasure, so they need to keep smoking, smoking more and more, tobacco and alcohol addiction is the common result of long-term physiological addiction, mental and behavioral habits [7]. Once you quit smoking and drinking, you may experience withdrawal symptoms such as restlessness, irritability, tension, anxiety, depression, headache, lethargy, and lack of concentration, which may also lead to mental illness. Coffee contains a lot of caffeine and other substances, patients after drinking easy to stimulate the nervous system of the brain, resulting in emotional excitement, panic and other symptoms, caffeine sensitive people can even lead to anxiety disorders (Xu, 2017).
2.4.2.4 Diabetes
There are many reasons why people with diabetes are prone to depression. For example, diabetes is a process that requires long-term treatment, and the stress brought by diabetes as a chronic disease, patients do not accept that they have this lifelong disease that lacks a radical cure, patients usually need to take long-term medication, coupled with some financial burden, easy to cause depression. In addition, the condition of diabetes is prone to recurrent complications in some people, which has a certain impact on the quality of life [51]. It is this kind of restriction brought by diabetes, the impact on the life of patients, lifelong medication, regular monitoring of blood sugar, and so on are related to anxiety. This is also why people with diabetes are prone to mental illness. Anxiety can also be caused by excessive concern about the complications of serious physical diseases that may result from diabetes, the fear of death from ketoacidosis, the fear of blindness, amputations, and the fear of kidney disease. In addition, blood sugar fluctuations and endocrine disorders also make diabetics themselves prone to anxiety, stress and depression (Sun, 2018).
3 Discussion/ Development
3.1 Significance
3.1.1 Genetics
Genetic elements are crucial in the pathogenesis of anxiety and depression, as outlined in Hettema's 2008 study.Some studies have shown that genetic factors can explain about 30-50% of the risk of anxiety and depression, that is, there is a possibility that genetic factors can directly cause anxiety and depression [72]. One example is the gene for the oxytocin receptor, a neuropeptide that has anti-anxiety and anti-depressive effects. Alterations in the oxytocin receptor gene can lead to dysfunctional receptor behavior, impacting the activity of oxytocin. This disruption can subsequently contribute to the onset of anxiety and depression [17]. Or the gene for the serotonin transporter, an important neurotransmitter that plays a key role in mood regulation, may directly cause anxiety or depression. Mutations in the serotonin transporter gene may affect the release and reuptake of serotonin, which can lead to anxiety and depression (Holmes et al., 2003). Certainly, genetic factors often constitute just a segment of the causal factors for anxiety and depression. Environmental influences, psychological dynamics, and lifestyle choices are also pivotal in the emergence of these mental health conditions.
Additionally, research involving same-sex twins has indicated that generalized anxiety disorder does not have a significant genetic basis. However, genetic elements may impact the development of other anxiety disorders, notably panic disorder and agoraphobia with panic attacks (Torgersen, 1983). In cases of identical twins, where one sibling has a mental illness and the other does not, it's not the result of genetic inheritance, it's the result of environmental or other factors, because identical twins are genetically identical. In the case of fraternal twins, the extent to which they co-inherit psychiatric disorders depends on the specific psychiatric disorder and the genetic and environmental factors involved. Fraternal twins, just like any other sibling, share about 50 percent of their genetic material. So if a psychiatric disorder has a strong genetic component, then fraternal twins both have a higher chance of inheriting the disorder compared to unrelated individuals in the general population (Torgersen, 1983). However, this risk may not be as high as that of identical twins because they share almost 100% of their genetic material. In addition to genetic factors, environmental factors including early life experiences, trauma or stress, and socioeconomic factors may also play a role [38]. Fraternal twins may be subject to similar environmental influences because they often grew up in the same household and share some common experiences. However, they may also have different experiences and relationships outside of their shared environment, which can lead to differences in the development of mental illness [29]. Overall, the degree to which fraternal twins inherit psychiatric disorders at the same time may differ and be influenced by a combination of genetic and environmental factors.
3.1.2 Diabetes
Research has shown that people with diabetes and inherited mental disorders may be more prone to anxiety and depression than those with only inherited mental disorders [40], because of the interaction between diabetes and mental disorders, diabetes and mental disorders, including anxiety and depression, can interact and influence each other. The stress and hurdles inherent in diabetes management can intensify or play a role in triggering anxiety and depression, particularly in individuals with a pre-existing genetic predisposition to mental disorders (Sun, 2018). There are also biological factors, diabetes and mental disorders have biological factors. Genetic factors can influence the development of both diseases, and certain genes may be associated with an increased risk of diabetes and mental disorders. The combination of mental disorders and a genetic predisposition to diabetes may lead to a higher likelihood of anxiety and depression. Not only that, but diabetes and mental disorders can share common physiological pathways or mechanisms [43]. For example, chronic inflammation, neurotransmitter disorders, and stress response systems can all be involved in both conditions. These common pathways may contribute to a higher susceptibility to anxiety and depression in people with diabetes and inherited mental disorders. It's important to note that everyone's experience is different, and not all people with diabetes and inherited mental disorders necessarily experience higher rates of anxiety and depression. The impact of these conditions can be influenced by a variety of factors, including the severity of diabetes, the specific mental disorder, access to support and treatment, and personal coping strategies.
At the same time, studies have shown that compared with non-diabetic women, middle-aged and elderly women with diabetes have a nearly three-fold increase in the prevalence of major depression, which is also 1.4 times that of men with diabetes. In men, diabetes had less effect on the prevalence of major depressive disorder [15]. Hormonal factors can indirectly lead to anxiety and depression in women, and hormonal fluctuations throughout a woman's life, such as puberty, divorces, pregnancy and menopause, also, middle-aged and older women may experience hormonal changes during menopause, which may coincide with the onset or worsening of mental health symptoms. Fluctuations in estrogen levels have been linked to mood disorders, and women with diabetes may be more susceptible to these hormonal changes and can affect mood and increase the chance of mental illness. These hormonal changes can interact with diabetes and affect emotional health. In 2021, it was estimated that around 18% of men in the U.S. experienced some form of mental illness over the past year. This statistic reflects the proportion of U.S. men who reported having any mental illness annually from 2008 to 2021 [23]. In a study encompassing over 15,000 patients with severe mental illness, researchers found that 28. 1% had Type 2 diabetes. This is in stark contrast to the estimated 12.2% prevalence of the disease in the general population [22]. Men and women have different coping mechanisms when faced with diabetes, they may use different coping strategies, and women may be more inclined to internalize emotions and rumination, which may increase the risk of developing mental illness. (See Figure 3)
Diabetes can also lead to anxiety and depression in several ways: emotions are easily affected, for example, and being diagnosed with diabetes can be overwhelming and trigger a range of emotions, including fear, sadness, and anger. The need to manage chronic diseases and make lifestyle changes can create stress and anxiety, which can lead to the development of depression. Daily management challenges are also an important factor, people with diabetes need to constantly monitor their blood sugar levels, take medications or inject insulin, and adhere to a strict diet and exercise regimen. The daily challenges and responsibilities people have associated with diabetes management can be demanding and can lead to feelings of frustration, anxiety and burnout. The apprehension surrounding diabetes and its potential complications is well-founded. Diabetes is associated with a range of long-term adverse effects, including heart disease, kidney issues, nerve damage, and vision loss [14]. Fear of developing these complications, or uncertainty about how diabetes will affect future health, can create anxiety and worry. Social and emotional effects are also important, and diabetes can have an impact on social interactions and relationships. Some people may feel stigmatized or judged because of misconceptions about diabetes. This can lead to feelings of isolation, inferiority and depression. Not only that, the huge cost of diabetes treatment can also become one of the factors that make patients feel stressed, especially in families with poor economic conditions. Approximately 10-15% of individuals with type 1 or 2 diabetes also experience depression [55], and anxiety disorders are prevalent enough that about 20% of those with type 1 diabetes are diagnosed with generalized anxiety disorder, a clinical condition [1]. Consequently, around 30-35% of diabetic individuals face anxiety and depression. Furthermore, more than one in five U.S. adults live with a mental illness. Over one in five youths aged 13-18 have experienced a severely debilitating mental illness at some point in their lives. Approximately one in 25 U.S. adults copes with a serious mental illness, such as schizophrenia, bipolar disorder, or major depression (Samhsa, 2023). Globally, one in eight people suffer from mental illness [4].
For twins, if one person of the twins develops diabetes and the other does not, in this case, the diabetes is not caused by genes, but by other factors. At this time, if both people suffer from mental illness, then the psychological problems of diabetic patients may be caused by diabetes, and it may be other factors, and the mental illness of non-diabetic patients may only be caused by environmental factors. Similarly, if both twins have inherited diabetes, and one twin has a mental illness and the other does not, then diabetes is not an important cause of mental illness, but a likely factor.
Directly comparing the prevalence of depression between inherited diabetes and induced diabetes is challenging because specific studies that directly compare the prevalence of depression between inherited diabetes and induced diabetes are limited. Most studies have focused on the overall relationship between diabetes and depression [51], without distinguishing between genetic or preexisting causes. And induced diabetes can be caused by a variety of causes, such as drug side effects, hormonal changes, or medical conditions such as gestational diabetes. The prevalence of depression may vary depending on the specific cause that triggers diabetes. For example, individuals with gestational diabetes may have different rates of depression compared to those with drug-induced diabetes. While personal experiences and vulnerabilities vary, the onset of depression can be shaped by a diverse array of individual factors. These include genetic predispositions, personal medical history, the extent of social support, and coping mechanisms [58]. While hereditary diabetes may have a higher underlying genetic susceptibility, this does not necessarily mean a higher prevalence of depression compared to induced diabetes. The impact of induced diabetes on mental health can be influenced by factors such as the severity of the condition, an individual's ability to cope with the diagnosis, and the presence of other stressors (Sun, 2018). However, we can easily see on the Figure 4, diabetes patients have a much higher incidence of depression than the general population.
3.1.3 Lifestyle
3.1.3.1 Diet
Dietary factors may also contribute to anxiety and depression. Unhealthy eating habits can negatively affect an individual's mental health, increasing the risk of anxiety and depression [18]. Insufficient consumption of essential nutrients, including vitamins, minerals, and Omega-3 fatty acids, can negatively influence mood regulation. For example, vitamin D deficiency may be linked to depression, while a lack of Omega-3 fatty acids may affect the normal function of brain cells, and these missing nutrients have the potential to be contributing factors to anxiety and depression [65]. Sometimes food allergies or intolerances can also indirectly lead to mental illness, food allergies or intolerances: Food allergies or intolerances can lead to inflammatory responses that affect brain function, thereby increasing the chances of anxiety and depression [41]. Unhealthy eating habits may disrupt the balance of the gut microbiome, which in turn affects emotional regulation, and may also lead to psychological problems.
Sometimes unhealthy eating or eating too much does not lead to anxiety and depression. Eating junk food, sweets, or your favorite foods can produce dopamine and a happy mood, which can actually make you happier for some people who are not overly concerned about their bodies. But if there are patients with anorexia, then they cannot rely on the intake of food to obtain the necessary nutrients, but have to hang water or nutrient solution to survive, then their body must be very weak, it is likely to suffer from some psychological diseases.
3.1.3.2 Psychoactive drugs
Not only that, but substance abuse or excessive alcohol, smoking, or caffeine consumption can lead to anxiety and depression [39]. First of all, excessive drinking can have a negative effect on the brain. Alcohol functions as a depressant on the central nervous system, disrupting the usual transmission of neurotransmitters. This interference can significantly impact mood and cognitive functions. Chronic alcohol use may lead to neuronal damage and structural changes in the brain, which in turn increases the risk of anxiety and depression [6]. Secondly, smoking is also associated with anxiety and depression. Nicotine is a stimulant drug that causes the release of dopamine, which gives you a sense of pleasure. However, long-term smoking can lead to a decrease in the number of dopamine receptors, which increases the risk of anxiety and depression [28]. In addition, nicotine withdrawal can trigger anxiety symptoms and make existing anxiety problems worse. Consuming too much caffeine can also lead to feelings of anxiety and depression. Caffeine acts as a stimulant for the central nervous system, effectively elevating heart rate and blood pressure while invigorating the nervous system. Excessive consumption of caffeine can lead to insomnia, restlessness and anxiety, which can affect mental health [80]. Substance abuse has also been linked to anxiety and depression. Certain drugs, such as cocaine and marijuana, can alter the chemical balance in the brain and interfere with the normal delivery of neurotransmitters. These drugs can cause mood swings, anxiety and depressive symptoms.
3.1.3.3 Health condition
Health conditions and body shape can also lead to anxiety and depression in several ways: for example, social pressure, society, media, and social media puts tremendous pressure on us to have a certain body type or fitness level, and constantly comparing yourself to those who have an "ideal" body type or fitness level can create self-doubt and insecurity. This situation often spirals into negative self-talk, body shame, and a detrimental body image. Such stress fosters feelings of inadequacy, diminished self-esteem, and profound body dissatisfaction. Consequently, this can pave the way for anxiety and depression. Some young people's pursuit of ideal body shape or health level may lead to perfectionism tendency [83]. The constant pursuit of perfection creates tremendous stress and anxiety because it is difficult to maintain unrealistic expectations, and this pressure can lead to feelings of failure, disappointment, and ultimately anxiety and depression. People striving for a certain body shape or fitness level can sometimes lead to disordered eating patterns, such as restricted eating or excessive exercise. These behaviors can have serious physical and psychological consequences, including anxiety, depression, and other mental health disorders.
4 Conclusion
There are many factors that can lead to people's anxiety and depression, such as the genetic factors mentioned above, the influence of life habits, the use of psychoactive drugs and the influence of diabetes may all lead to mental illness. It is important to understand that the development of mental illness is a complex interplay of various factors, and it is often difficult to identify one factor as the sole cause. However, this article provides some insight into the impact of the factors mentioned above: It is clear that genetic and environmental factors play the biggest role at between 40 to 60 percent in the development of depression [57], while genes alone do not determine the development of mental illness, as environmental and lifestyle factors also play an important role. The role of environmental factors in the occurrence of depression is about 50% to 60% [57], and lifestyle factors, including diet, exercise, sleep patterns and stress management, can affect mental health. There are more than a quarter of people with a serious mental illness also have a problem with psychoactive drugs, and there is often a correlation between mental illness and substance abuse (Samhsa, 2023). Actually, if patients are expose to psychoactive drugs, then the likelihood of anxiety and depression increases more than fifteen percent. While diabetes itself may not directly link to mental illness, it is a chronic condition that can contribute to the development or worsening of mental health disorders. The incidence of diabetic depression is around 10% (Zhang, 2020). Therefore, compared with ordinary people, people with diabetes are bound to be more prone to mental illness due to various pressures such as the stigma attach to it and the environment rather than actually being suffering diabetes itself. Overall, up to half of all cases of mental illness are due to genetic or environmental factors and lifestyle influences, while a small percentage are caused by drug abuse and diabetes. Diabetes is one of significant factor in determining someone having anxiety and depression, but anxiety and depression is more likely to occur due to other factors, not diabetes. In general, diabetes does cause anxiety and depression to some extent, but compared with the above other factors, the proportion of mental illness directly caused by diabetes is not that large.
References
[1]. Al Hayek, A. A., Robert, A. A., Braham, R. B., Issa, B. A., & Al Sabaan, F. S. (2015). Predictive risk factors for fear of hypoglycemia and anxiety-related emotional disorders among adolescents with type 1 diabetes. Medical Principles and Practice, 24(3), 222–230.
[2]. Andersen, A. R., Christiansen, J. S., Sandahl, K., Andersen, J. K., Kreiner, S., & Deckert, T. (1983). Diabetic nephropathy in type 1 (insulin-dependent) diabetes: An epidemiological study. Diabetologia, 25(6).
[3]. Arroyo, M. N., Green, J. A., Cnop, M., & Igoillo-Esteve, M. (2021). tRNA biology in the pathogenesis of diabetes: Role of genetic and environmental factors. International Journal of Molecular Sciences, 22(2), 496.
[4]. Baidu.com. (2022). The prevalence of mental illness worldwide. Retrieved from https://baijiahao.baidu.com/s?id=1751599544279428002&wfr=spider&for=pc [Accessed September 19, 2023]
[5]. Barroso, I. (2005). Genetics of type 2 diabetes. Diabetic Medicine, 22(5), 517–535.
[6]. Bartels, S. J., Coakley, E. H., Zubritsky, C., Ware, J. H., Miles, K. M., Areán, P. A., Chen, H., Oslin, D. W., Llorente, M. D., Costantino, G., Quijano, L., McIntyre, J. S., Linkins, K. W., Oxman, T. E., Maxwell, J., & Levkoff, S. E. (2004). Improving access to geriatric mental health services: A randomized trial comparing treatment engagement with integrated versus enhanced referral care for depression, anxiety, and at-risk alcohol use. American Journal of Psychiatry, 161(8), 1455–1462.
[7]. Breslau, N. (1995). Psychiatric comorbidity of smoking and nicotine dependence. Behavior Genetics, 25(2), 95–101.
[8]. Brink, S. J. (2001). Complications of pediatric and adolescent type 1 diabetes mellitus. Current Diabetes Reports, 1(1), 47–55.
[9]. Candib, L. M. (2007). Obesity and diabetes in vulnerable populations: Reflection on proximal and distal causes. The Annals of Family Medicine, 5(6), 547–556.
[10]. Ceretta, L. B., Réus, G. Z., Abelaira, H. M., Jornada, L. K., Schwalm, M. T., Hoepers, N. J., Tomazzi, C. D., Gulbis, K. G., Ceretta, R. A., & Quevedo, J. (2012). Increased prevalence of mood disorders and suicidal ideation in type 2 diabetic patients. Acta Diabetologica, 49(S1), 227–234.
[11]. Chang, W. (2017). What is anxiety. Retrieved from https://m.baidu.com/bh/m/detail/ar_9238341498181159361 [Accessed August 1, 2023]
[12]. Cornelis, M. C., Zaitlen, N., Hu, F. B., Kraft, P., & Price, A. L. (2014). Genetic and environmental components of family history in type 2 diabetes. Human Genetics, 134(2), 259–267.
[13]. Crowe, R. R. (1983). A family study of panic disorder. Archives of General Psychiatry, 40(10), 1065.
[14]. Danowski, T. S. (1971). Non-ketotic coma and diabetes mellitus. Diabetes, 20(4), 913–918.
[15]. Deischinger, C., Dervic, E., Leutner, M., Kosi-Trebotic, L., Klimek, P., Kautzky, A., & Kautzky-Willer, A. (2020). Diabetes mellitus is associated with a higher risk for major depressive disorder in women than in men. BMJ Open Diabetes Research & Care, 8(1), e001430.
[16]. Dong, Y., Gao, W., Nan, H., Yu, H., Li, F., Duan, W., Wang, Y., Sun, B., Qian, R., Tuomilehto, J., & Qiao, Q. (2005). Prevalence of type 2 diabetes in urban and rural Chinese populations in Qingdao, China. Diabetic Medicine, 22(10), 1427–1433.
[17]. Elif Çalışkan, Şahin, M. N., & Güldağ, M. A. (2021). Oxytocin and oxytocin receptor gene regulation in Williams syndrome: A systematic review. PubMed, 94(4), 623–635.
[18]. Firth, J., Marx, W., Dash, S., Carney, R., Teasdale, S. B., Solmi, M., Stubbs, B., Schuch, F. B., Carvalho, A. F., Jacka, F., & Sarris, J. (2019). The effects of dietary improvement on symptoms of depression and anxiety. Psychosomatic Medicine, 81(3), 265–280.
[19]. Forouhi, N. G., & Wareham, N. J. (2018). Epidemiology of diabetes. Diabetes Research and Clinical Practice, 47(1), 22–27.
[20]. Fowler, M. J. (2011). Microvascular and macrovascular complications of diabetes. Clinical Diabetes, 29(3), 116–122.
[21]. Franz, M., Angold, A., Copeland, W., Costello, E. J., Towe-Goodman, N., & Egger, H. (2013). Preschool anxiety disorders in pediatric primary care: Prevalence and comorbidity. Journal of the American Academy of Child & Adolescent Psychiatry, 52(12), 1294–1303.e1.
[22]. UCSF.edu. (2018). Prevalence of mental illness in men. Retrieved from https://www.ucsf.edu/news/2018/06/410741/diabetes-added-high-risks-people-severe-mental-illness [Accessed September 10, 2023]
[23]. Statista. (2023). Prevalence of mental illness in men with diabetes. Retrieved from https://www.statista.com/statistics/673184/any-mental-illness-past-year-us-men/ [Accessed September 10, 2023]
[24]. SAMHSA. (2023). Prevalence of mental illness caused by abuse of substances. Retrieved from https://www.samhsa.gov/mental-health/mental-health-substance-use-co-occurring-disorders [Accessed September 10, 2023]
[25]. SAMHSA. (2023). Prevalence of mental illness. Retrieved from https://www.samhsa.gov/mental-health/mental-health-substance-use-co-occurring-disorders [Accessed September 11, 2023]
[26]. Greenberg, J. A., Axen, K. V., Schnoll, R., & Boozer, C. N. (2005). Coffee, tea and diabetes: The role of weight loss and caffeine. International Journal of Obesity, 29(9), 1121–1129.
[27]. Harrison, T. A., Hindorff, L. A., Kim, H., Wines, R. C. M., Bowen, D. J., McGrath, B. B., & Edwards, K. L. (2003). Family history of diabetes as a potential public health tool. American Journal of Preventive Medicine, 24(2), 152–159.
[28]. Hayes, J., & Koo, J. (2010). Psoriasis: Depression, anxiety, smoking, and drinking habits. Dermatologic Therapy, 23(2), 174–180.
[29]. Hettema, J. M., Neale, M. C., & Kendler, K. S. (2001). A review and meta-analysis of the genetic epidemiology of anxiety disorders. American Journal of Psychiatry, 158(10), 1568–1578.
[30]. Hettema, J. M. (2008). What is the genetic relationship between anxiety and depression? American Journal of Medical Genetics Part C: Seminars in Medical Genetics, 148C(2), 140–146.
[31]. Holmes, A., Murphy, D. L., & Crawley, J. N. (2003). Abnormal behavioral phenotypes of serotonin transporter knockout mice: Parallels with human anxiety and depression. Biological Psychiatry, 54(10), 953–959.
[32]. Horn, G. T., Bugawan, T. L., Long, C. M., & Erlich, H. A. (1988). Allelic sequence variation of the HLA-DQ loci: Relationship to serology and to insulin-dependent diabetes susceptibility. Proceedings of the National Academy of Sciences, 85(7), 2215–2219.
[33]. Huang, H., & Li, J. (2016). Exploring the relationship between type 2 diabetes and depression. Journal of Diabetes Research, 2016, 1–11.
[34]. Jansen, P. R., Wray, N. R., & Penninx, B. W. J. H. (2016). Evidence of causality in associations between depression, anxiety, and type 2 diabetes. Diabetes Care, 39(10), 1948–1951.
[35]. Katon, W., & Ciechanowski, P. (2002). Impact of depression on the course of type 2 diabetes and the role of diabetes-related distress. Current Diabetes Reports, 2(4), 330–336.
[36]. Koh, K. (2018). Diabetic retinopathy and mental health in patients with type 1 diabetes. Diabetes & Metabolism Journal, 42(4), 314–321.
[37]. Kong, X. X., & Zhao, Y. (2020). The effects of genetic variation on diabetes and obesity-related traits. Journal of Endocrinology and Metabolism, 112(6), 3238–3248.
[38]. La Haye, S., Patel, N., & Hernandez, J. (2017). Type 2 diabetes mellitus and depression: Exploring the complex relationship. International Journal of Diabetes Research, 8(3), 185–192.
[39]. Lakhan, S. E., & Kirchgessner, A. (2013). The role of the gut microbiome in obesity and metabolic disorders. Journal of Clinical Gastroenterology, 47(4), 334–339.
[40]. Lee, C. H., & Byun, J. W. (2020). Depression and anxiety disorders among type 2 diabetes patients: A nationwide study. Journal of Diabetes Research, 2020, 1–10.
[41]. Liu, X., Li, Y., & Jiang, H. (2022). The impact of anxiety and depression on glycemic control in diabetes patients. BMC Endocrine Disorders, 22(1), 1–10.
[42]. Li, T., Wu, X., & Lin, H. (2021). The correlation between type 2 diabetes and depression: A meta-analysis. Endocrine Reviews, 42(3), 407–420.
[43]. Li, L., Zhang, J., & Zhang, Y. (2023). The prevalence and treatment of depression in diabetic patients: A meta-analysis. Journal of Clinical Psychiatry, 84(2), e324–e331.
[44]. Liu, H., & Yang, Q. (2019). Mental health and type 2 diabetes: The role of dietary patterns. Diabetes Research and Clinical Practice, 150, 70–77.
[45]. Morgan, J., & Lewis, G. (2012). Depression and diabetes: A complex relationship. Diabetic Medicine, 29(6), 792–802.
[46]. Meloni, A., & Marrocco, T. (2015). Anxiety and depression in type 1 diabetes: The role of social support. Diabetes Research and Clinical Practice, 108(3), 281–288.
[47]. Nouwen, A., & Winkley, K. (2010). Diabetes and depression: A systematic review. Diabetologia, 53(5), 956–962.
[48]. Shi, Y., Yang, S., & Wang, Z. (2020). Impact of anxiety and depression on glycemic control and complications in type 2 diabetes: A systematic review and meta-analysis. Journal of Diabetes Research, 2020, 1–10.
[49]. Sun, K., Wang, L., & Zhang, Y. (2018). The impact of diabetes on mental health: A comprehensive review. Frontiers in Psychology, 9, 287.
[50]. Wang, J., & Li, X. (2023). Type 2 diabetes and depression: The role of inflammation. Journal of Diabetes Research, 2023, 1–8.
[51]. Wu, Z., Zhao, J., & Liu, Y. (2023). Relationship between diabetes and mental health: A review. Journal of Diabetes Research, 2023, 1–10.
[52]. Xie, X., Yang, H., & Zhang, L. (2022). The relationship between diabetes and anxiety disorders: A systematic review and meta-analysis. Diabetes Research and Clinical Practice, 184, 109295.
[53]. Xu, X., Zhang, L., & Liu, J. (2020). The relationship between diabetes and mood disorders: A meta-analysis. Journal of Affective Disorders, 277, 416–426.
[54]. Yang, Y., Zhou, X., & Li, F. (2021). The impact of depression on type 2 diabetes: A meta-analysis. Journal of Diabetes Research, 2021, 1–8.
[55]. Zhang, L., & Wang, Q. (2019). Depression and type 2 diabetes: Exploring the bidirectional relationship. Diabetes Research and Clinical Practice, 148, 80–90.
[56]. Zheng, X., Liu, Y., & Zhang, H. (2020). Relationship between type 2 diabetes and depression: A meta-analysis. BMC Psychiatry, 20(1), 1–10.
Cite this article
Tian,J. (2024). To what extent does having diabetes influence individuals suffering from anxiety and depression?. Journal of Food Science, Nutrition and Health,2,13-22.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Journal:Journal of Food Science, Nutrition and Health
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Al Hayek, A. A., Robert, A. A., Braham, R. B., Issa, B. A., & Al Sabaan, F. S. (2015). Predictive risk factors for fear of hypoglycemia and anxiety-related emotional disorders among adolescents with type 1 diabetes. Medical Principles and Practice, 24(3), 222–230.
[2]. Andersen, A. R., Christiansen, J. S., Sandahl, K., Andersen, J. K., Kreiner, S., & Deckert, T. (1983). Diabetic nephropathy in type 1 (insulin-dependent) diabetes: An epidemiological study. Diabetologia, 25(6).
[3]. Arroyo, M. N., Green, J. A., Cnop, M., & Igoillo-Esteve, M. (2021). tRNA biology in the pathogenesis of diabetes: Role of genetic and environmental factors. International Journal of Molecular Sciences, 22(2), 496.
[4]. Baidu.com. (2022). The prevalence of mental illness worldwide. Retrieved from https://baijiahao.baidu.com/s?id=1751599544279428002&wfr=spider&for=pc [Accessed September 19, 2023]
[5]. Barroso, I. (2005). Genetics of type 2 diabetes. Diabetic Medicine, 22(5), 517–535.
[6]. Bartels, S. J., Coakley, E. H., Zubritsky, C., Ware, J. H., Miles, K. M., Areán, P. A., Chen, H., Oslin, D. W., Llorente, M. D., Costantino, G., Quijano, L., McIntyre, J. S., Linkins, K. W., Oxman, T. E., Maxwell, J., & Levkoff, S. E. (2004). Improving access to geriatric mental health services: A randomized trial comparing treatment engagement with integrated versus enhanced referral care for depression, anxiety, and at-risk alcohol use. American Journal of Psychiatry, 161(8), 1455–1462.
[7]. Breslau, N. (1995). Psychiatric comorbidity of smoking and nicotine dependence. Behavior Genetics, 25(2), 95–101.
[8]. Brink, S. J. (2001). Complications of pediatric and adolescent type 1 diabetes mellitus. Current Diabetes Reports, 1(1), 47–55.
[9]. Candib, L. M. (2007). Obesity and diabetes in vulnerable populations: Reflection on proximal and distal causes. The Annals of Family Medicine, 5(6), 547–556.
[10]. Ceretta, L. B., Réus, G. Z., Abelaira, H. M., Jornada, L. K., Schwalm, M. T., Hoepers, N. J., Tomazzi, C. D., Gulbis, K. G., Ceretta, R. A., & Quevedo, J. (2012). Increased prevalence of mood disorders and suicidal ideation in type 2 diabetic patients. Acta Diabetologica, 49(S1), 227–234.
[11]. Chang, W. (2017). What is anxiety. Retrieved from https://m.baidu.com/bh/m/detail/ar_9238341498181159361 [Accessed August 1, 2023]
[12]. Cornelis, M. C., Zaitlen, N., Hu, F. B., Kraft, P., & Price, A. L. (2014). Genetic and environmental components of family history in type 2 diabetes. Human Genetics, 134(2), 259–267.
[13]. Crowe, R. R. (1983). A family study of panic disorder. Archives of General Psychiatry, 40(10), 1065.
[14]. Danowski, T. S. (1971). Non-ketotic coma and diabetes mellitus. Diabetes, 20(4), 913–918.
[15]. Deischinger, C., Dervic, E., Leutner, M., Kosi-Trebotic, L., Klimek, P., Kautzky, A., & Kautzky-Willer, A. (2020). Diabetes mellitus is associated with a higher risk for major depressive disorder in women than in men. BMJ Open Diabetes Research & Care, 8(1), e001430.
[16]. Dong, Y., Gao, W., Nan, H., Yu, H., Li, F., Duan, W., Wang, Y., Sun, B., Qian, R., Tuomilehto, J., & Qiao, Q. (2005). Prevalence of type 2 diabetes in urban and rural Chinese populations in Qingdao, China. Diabetic Medicine, 22(10), 1427–1433.
[17]. Elif Çalışkan, Şahin, M. N., & Güldağ, M. A. (2021). Oxytocin and oxytocin receptor gene regulation in Williams syndrome: A systematic review. PubMed, 94(4), 623–635.
[18]. Firth, J., Marx, W., Dash, S., Carney, R., Teasdale, S. B., Solmi, M., Stubbs, B., Schuch, F. B., Carvalho, A. F., Jacka, F., & Sarris, J. (2019). The effects of dietary improvement on symptoms of depression and anxiety. Psychosomatic Medicine, 81(3), 265–280.
[19]. Forouhi, N. G., & Wareham, N. J. (2018). Epidemiology of diabetes. Diabetes Research and Clinical Practice, 47(1), 22–27.
[20]. Fowler, M. J. (2011). Microvascular and macrovascular complications of diabetes. Clinical Diabetes, 29(3), 116–122.
[21]. Franz, M., Angold, A., Copeland, W., Costello, E. J., Towe-Goodman, N., & Egger, H. (2013). Preschool anxiety disorders in pediatric primary care: Prevalence and comorbidity. Journal of the American Academy of Child & Adolescent Psychiatry, 52(12), 1294–1303.e1.
[22]. UCSF.edu. (2018). Prevalence of mental illness in men. Retrieved from https://www.ucsf.edu/news/2018/06/410741/diabetes-added-high-risks-people-severe-mental-illness [Accessed September 10, 2023]
[23]. Statista. (2023). Prevalence of mental illness in men with diabetes. Retrieved from https://www.statista.com/statistics/673184/any-mental-illness-past-year-us-men/ [Accessed September 10, 2023]
[24]. SAMHSA. (2023). Prevalence of mental illness caused by abuse of substances. Retrieved from https://www.samhsa.gov/mental-health/mental-health-substance-use-co-occurring-disorders [Accessed September 10, 2023]
[25]. SAMHSA. (2023). Prevalence of mental illness. Retrieved from https://www.samhsa.gov/mental-health/mental-health-substance-use-co-occurring-disorders [Accessed September 11, 2023]
[26]. Greenberg, J. A., Axen, K. V., Schnoll, R., & Boozer, C. N. (2005). Coffee, tea and diabetes: The role of weight loss and caffeine. International Journal of Obesity, 29(9), 1121–1129.
[27]. Harrison, T. A., Hindorff, L. A., Kim, H., Wines, R. C. M., Bowen, D. J., McGrath, B. B., & Edwards, K. L. (2003). Family history of diabetes as a potential public health tool. American Journal of Preventive Medicine, 24(2), 152–159.
[28]. Hayes, J., & Koo, J. (2010). Psoriasis: Depression, anxiety, smoking, and drinking habits. Dermatologic Therapy, 23(2), 174–180.
[29]. Hettema, J. M., Neale, M. C., & Kendler, K. S. (2001). A review and meta-analysis of the genetic epidemiology of anxiety disorders. American Journal of Psychiatry, 158(10), 1568–1578.
[30]. Hettema, J. M. (2008). What is the genetic relationship between anxiety and depression? American Journal of Medical Genetics Part C: Seminars in Medical Genetics, 148C(2), 140–146.
[31]. Holmes, A., Murphy, D. L., & Crawley, J. N. (2003). Abnormal behavioral phenotypes of serotonin transporter knockout mice: Parallels with human anxiety and depression. Biological Psychiatry, 54(10), 953–959.
[32]. Horn, G. T., Bugawan, T. L., Long, C. M., & Erlich, H. A. (1988). Allelic sequence variation of the HLA-DQ loci: Relationship to serology and to insulin-dependent diabetes susceptibility. Proceedings of the National Academy of Sciences, 85(7), 2215–2219.
[33]. Huang, H., & Li, J. (2016). Exploring the relationship between type 2 diabetes and depression. Journal of Diabetes Research, 2016, 1–11.
[34]. Jansen, P. R., Wray, N. R., & Penninx, B. W. J. H. (2016). Evidence of causality in associations between depression, anxiety, and type 2 diabetes. Diabetes Care, 39(10), 1948–1951.
[35]. Katon, W., & Ciechanowski, P. (2002). Impact of depression on the course of type 2 diabetes and the role of diabetes-related distress. Current Diabetes Reports, 2(4), 330–336.
[36]. Koh, K. (2018). Diabetic retinopathy and mental health in patients with type 1 diabetes. Diabetes & Metabolism Journal, 42(4), 314–321.
[37]. Kong, X. X., & Zhao, Y. (2020). The effects of genetic variation on diabetes and obesity-related traits. Journal of Endocrinology and Metabolism, 112(6), 3238–3248.
[38]. La Haye, S., Patel, N., & Hernandez, J. (2017). Type 2 diabetes mellitus and depression: Exploring the complex relationship. International Journal of Diabetes Research, 8(3), 185–192.
[39]. Lakhan, S. E., & Kirchgessner, A. (2013). The role of the gut microbiome in obesity and metabolic disorders. Journal of Clinical Gastroenterology, 47(4), 334–339.
[40]. Lee, C. H., & Byun, J. W. (2020). Depression and anxiety disorders among type 2 diabetes patients: A nationwide study. Journal of Diabetes Research, 2020, 1–10.
[41]. Liu, X., Li, Y., & Jiang, H. (2022). The impact of anxiety and depression on glycemic control in diabetes patients. BMC Endocrine Disorders, 22(1), 1–10.
[42]. Li, T., Wu, X., & Lin, H. (2021). The correlation between type 2 diabetes and depression: A meta-analysis. Endocrine Reviews, 42(3), 407–420.
[43]. Li, L., Zhang, J., & Zhang, Y. (2023). The prevalence and treatment of depression in diabetic patients: A meta-analysis. Journal of Clinical Psychiatry, 84(2), e324–e331.
[44]. Liu, H., & Yang, Q. (2019). Mental health and type 2 diabetes: The role of dietary patterns. Diabetes Research and Clinical Practice, 150, 70–77.
[45]. Morgan, J., & Lewis, G. (2012). Depression and diabetes: A complex relationship. Diabetic Medicine, 29(6), 792–802.
[46]. Meloni, A., & Marrocco, T. (2015). Anxiety and depression in type 1 diabetes: The role of social support. Diabetes Research and Clinical Practice, 108(3), 281–288.
[47]. Nouwen, A., & Winkley, K. (2010). Diabetes and depression: A systematic review. Diabetologia, 53(5), 956–962.
[48]. Shi, Y., Yang, S., & Wang, Z. (2020). Impact of anxiety and depression on glycemic control and complications in type 2 diabetes: A systematic review and meta-analysis. Journal of Diabetes Research, 2020, 1–10.
[49]. Sun, K., Wang, L., & Zhang, Y. (2018). The impact of diabetes on mental health: A comprehensive review. Frontiers in Psychology, 9, 287.
[50]. Wang, J., & Li, X. (2023). Type 2 diabetes and depression: The role of inflammation. Journal of Diabetes Research, 2023, 1–8.
[51]. Wu, Z., Zhao, J., & Liu, Y. (2023). Relationship between diabetes and mental health: A review. Journal of Diabetes Research, 2023, 1–10.
[52]. Xie, X., Yang, H., & Zhang, L. (2022). The relationship between diabetes and anxiety disorders: A systematic review and meta-analysis. Diabetes Research and Clinical Practice, 184, 109295.
[53]. Xu, X., Zhang, L., & Liu, J. (2020). The relationship between diabetes and mood disorders: A meta-analysis. Journal of Affective Disorders, 277, 416–426.
[54]. Yang, Y., Zhou, X., & Li, F. (2021). The impact of depression on type 2 diabetes: A meta-analysis. Journal of Diabetes Research, 2021, 1–8.
[55]. Zhang, L., & Wang, Q. (2019). Depression and type 2 diabetes: Exploring the bidirectional relationship. Diabetes Research and Clinical Practice, 148, 80–90.
[56]. Zheng, X., Liu, Y., & Zhang, H. (2020). Relationship between type 2 diabetes and depression: A meta-analysis. BMC Psychiatry, 20(1), 1–10.