1. Introduction
With the development of nanotechnology, the intersection and penetration with modern medicine and biology has become a brand-new research field, and the progress and development of this field will provide a brand-new technology and viewpoint for the research of modern biology and medicine, especially the application of nanomaterials, which has brought a profound change to the medical field. As early as 1959, Feynman, the famous Nobel Prize winner in physics, predicted the emergence of nanotechnology and its promising future, and scientists tried to use nanotechnology to solve the problems of medicine. In 1991, at K Eric Drexler, Chris Peterson, and Gayle Pergamit published the book ‘Unbounding the Future’, in which the professional term ‘nanomedicine’ was used for the first time.and in 1999, Freitas, a famous advocate of nanomedicine, gave at least two definitions of nanomedicine in his treatise [1]: he believed that nanomedicine is the use of fabricated nano-equipment and nano-devices to treat the whole biological system of the organism on molecular level. Firstly, he believes that nanomedicine is the use of manufactured nano-equipment and nano-devices at the molecular level to monitor, control, build, repair, defend and improve the entire biological system of the organism. Later he gave a more comprehensive definition that nanomedicine is the science and technology of using human molecular tools and molecular knowledge to prevent, diagnose and treat diseases and traumas, get rid of pain, and protect and improve human health. With the unremitting efforts of scientists from various countries, many significant achievements have been made in the field of nanomedicine research, and some of them are close to clinical application.
At the 4th International Conference on Nanomedicine in 2021, Shi Jianlin, an academician of the Chinese Academy of Sciences, pointed out that nanomedicine can realize drug delivery by nucleus-targeting, but there are still problems of high cytotoxicity and lack of oxygen. Using the concept of nanocatalytic medicine, the generation of reactive oxygen species through ROS in-situ catalytic reaction and the improvement of microenvironmental response through Fenton reaction can overcome the drawbacks of traditional nanomedicine, providing a new development idea for nanomedicine. Prof. Wolfgang Parak from the University of Hamburg, Germany, gave a presentation on “Quantitative Particle Uptake and Fate by Cells”, in which he elaborated on the interaction between cells and nanoparticles, and revealed that both receptor-ligand binding strength and cell culture environment have a significant influence on cell interaction. He explained the interaction between cells and nanoparticles, revealing that the binding strength of the receptor-ligand and the cell culture environment has a close influence on the cell interaction, which lays a foundation for further research on the technology of drug slow release and the reduction of the toxicity of nanomaterials.
In 2022, a team from Harvard Medical School published a research paper in the journal Nature Communications etitled: Combining p53 mRNA nanotherapy with immune checkpoint blockade reprograms the immune microenvironment for effective cancer therapy. The paper proposes the use of this new type of lipid nanoparticles as a delivery carrier to specifically deliver p53 mRNA to liver cancer cells, while being used in conjunction with anti PD-1 monoclonal antibodies. Through drug action, the global programming of the tumor microenvironment (TME) can be effectively re programmed, which can better combat cancer and improve treatment effectiveness.
Nanotechnology is one of the most prominent emerging technologies and is considered a key enabling technology (KET) by the European Commission’s High-Level Group on Key Enabling Technologies (HLG) [2]. It is highly innovative and provides a solid foundation for further innovation in medicine and research and development of new products and technologies, and is an important topic for medical development in the 21st century. This paper reviews the applications of nanotechnology in drug delivery, diagnostic diagnosis and treatment of diseases, and tissue repair and regeneration, and discusses the problems and risks that nanomaterials have to face in the process of application. Nanotechnology has great potential in the field of medicine, solving problems that are difficult for doctors to solve with traditional techniques, and will bring breakthroughs to the current state of medicine.
2. Nanotechnology in biomedicine
2.1. Drug delivery applications
In recent years, the development of nanoparticles (NPs) has expanded into clinical applications. Nanoparticles are smaller than normal drug molecules, with particle sizes ranging from 1 to 100 nm. The use of these particles as nanocarriers to carry drugs has revolutionized the application of drug delivery in medical conditions, and in the treatment of brain cancers such as glioblastoma multiforme, the drugs in this unique carrier also have the ability to cross the blood-brain barrier, allowing the treatment of brain cancers such as glioblastoma multiforme.
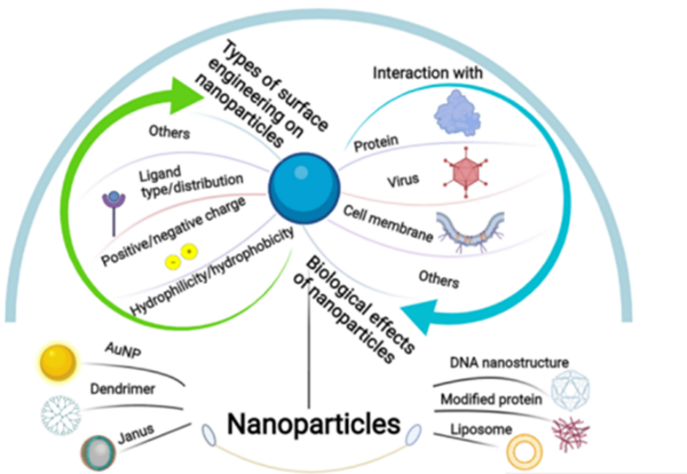
Figure 1. Nanoparticles [3].
In addition, nanoparticles embody physicochemical properties that are different from those of macroscopic particles due to their small particle size, large specific surface area and surface curvature See Fig.1[3]. Surface functionalization of nanoparticles, including the use of ligands. Nanoparticle surface modifiers can modulate the surface electronic structure and spatial environment of nanoparticles, and thus their activity and selectivity. Nanoparticle-carrier interactions can further enhance the precise targeting of nanoparticles, which can ensure that the nanoparticles are efficiently directed in vivo to effectively deliver the drug to the region of interest (See Fig.1).
Nano controlled release system can extend the time of action of drugs in vivo, drug-carrying nanoparticles can penetrate the tissue interstitial space and capillary wall to reach the target tissue, with the degradation of the surface polymer material will be gradually released, improving the stability of the drug, so that the drug plays a role in the different cell cycle, it reduces the dose of the drug administered, but also reduces the drug brought about by the toxic side effects [4]. Some scholars used polyvinyl glycol polyhydroxyacetate to prepare magnetic nanoparticles as a carrier for bovine serum proteins, and it was confirmed that bovine serum proteins can be released slowly. Fundaro used nanoliposomes carrying adriamycin for animal experiments, and it was found that the half-life of the drug was significantly prolonged.
2.2. Applications for disease detection and diagnosis
Due to the unique optical, magnetic, electrical, and thermal properties of nanomaterials, these properties can be used to emit various types of detection signals, enhance detection signals, and simplify detection procedures. The most typical nanomaterials, such as semiconductor quantum dots, gold nanoparticles, and magnetic nanoparticles, have been widely used in various in vitro diagnostic technologies
Gold nanoparticles are often used for in vitro assays due to their large specific surface area, superb adsorption and electron transfer capabilities, as well as the large differences in color, UV absorption and plasmonic effects with variations in composition, shape and aggregation state. In recent years, gold nanoparticles have often used for the in vitro detection of nucleic acids, DNA, proteins and immunoassay studies. Zhou et al. successfully applied the self-assembly of gold nanoparticles to biosensing [5]. In this system, the gold nanoparticles were modified with a single-stranded DNA on the surface, which mainly plays the roles of targeting and protection. In the dispersed state, the ultraviolet absorption of the gold nanoparticle solution is located at 520 nm, and there is no obvious warming phenomenon under near-infrared irradiation. When the target DNA is added, the single-stranded DNA nanoprobe will hybridize with the target DNA, which will lead to the formation of gold nanoparticles as an aggregate, and the absorption peak will redshift to around 650 nm, and the temperature can be increased by 11oC under laser irradiation. Therefore, by measuring the temperature change of gold nano solutions, it is possible to quantitatively detect nucleic acids or DNA. This method is simple, inexpensive and highly sensitive, and is expected to become a universal photothermal immunoassay in the future.
In addition, it is also possible to detect the distribution of drugs in the body and their metabolism in cells and tissues after labelling the nanoparticles with drugs. This technology can reduce the need for animal experiments and improve the efficiency and safety of in vitro experiments.
Nanobiotechnology scientists have used nanotechnology to successfully produce microchips coated with biomolecules. The chip is designed to signal electrical impulses when the molecules detect signs of disease. Special sensor nanobots can be inserted into the bloodstream under the skin to check blood composition and warn of any possible disease. They can also be used to monitor blood sugar levels in the blood. The advantage of using such nanorobots is that they are very cheap to produce and easy to carry. Similarly, nanoparticles can be functionalized with metals and used to detect tumors during imaging. This also helps in precise targeting of cancerous tissues to ensure comprehensive treatment. The diagnostic efficacy of malignant tumors involves both sensitivity and specificity, and the development of new types of molecular imaging probes based on nanotechnology can enhance both sensitivity and specificity.
2.3. Applications in gene therapy
Gene therapy is a new therapy developed in recent years to supplement missing genes or turn off abnormal genes in the human body, and vector has been one of the most important issues in the field of gene therapy research. How to choose a suitable vector to make the target gene expressed stably and effectively is one of the key factors for the success of gene therapy. There are two types of gene vectors, namely, viral vectors and non-viral vectors, and nanobiological vectors are non-viral vectors. With the research and innovation of nanotechnology, nano-biological vectors as gene therapy vectors have gradually shown their advantages of safety, stability and efficiency.
Nanobiomaterials, due to their good biosafety, can easily and effectively achieve gene targeting and efficient expression, and become a good medium for the preparation of efficient and targeted gene therapy vector systems. Zhou et al. showed that silicon nanoparticles can be used as a gene transfection vector and can effectively transfect adult isolated keratinocytes. It can effectively transfect adult isolated keratinocytes by binding to PEGFP-N, DNA, with a transfection rate of about 20% - 30% [6]. For example, antisense oligonucleotides can inhibit gene expression at the level of protein translation, which is valuable in the treatment of viral infections and cancer. However, oligonucleotides have weak intracellular permeability and poor intra- and extracellular stability, so the clinical application of oligonucleotides is limited. In contrast, using nanoparticles as carriers, the intracellular permeability and intracellular stability of oligonucleotides can be significantly increased. The 15mer thymine oligonucleotide fragments were adsorbed onto poly(isobutyl cyanoacrylate) nanoparticles and incubated with U937 cells respectively with free oligonucleotide fragments as a control, and it was found that the uptake of the nanoparticle-bound oligonucleotide fragments was 8 fold higher than that of the free oligonucleotide fragments[7]. In addition, the use of isobutyl cyanoacrylate (PIBCA) nanoparticles as a carrier resulted in the uptake of oligonucleotides predominantly by liver cells, reducing the distribution of oligonucleotides in other organs. The concentration of oligonucleotides aggregated in the lungs using alginate nanoparticles as a carrier was 10-fold higher than that of the PIBCA as a carrier [8].
2.4. Applications in tissue Repair and regeneration and transplantation
Nanocomposites and nanopolymers have good biocompatibility and biodegradability, and the rate of degradation should match the rate of new tissue formation, excellent three-dimensional structure, which is conducive to cellular nutrient delivery and vascularisation process, so nanocomposites and nanopolymers are commonly used biomaterials for tissue repair and transplantation.
In 1994, Bonfield successfully developed nanomaterials that mimic bone structure, the main component of which is a hydroxyapatite mesh mixed with polyethylene and compressed, with physical properties that are consistent with an ideal bone substitute. Nanostructures can achieve synergistic regulation of multilevel structures and jointly promote tissue regeneration: on the one hand, nanostructures can provide space for the growth, proliferation, osteogenic differentiation, mineralization and eventual bone formation of osteoblast cell lineages; on the other hand, nanostructures can regulate the activity of osteogenesis-related cells and produce a microenvironment favorable to osteogenesis in order to enhance bone formation [9,10].
In November 2011, ‘the Lancet’ reported that a team of thoracic surgeons at Karolinska University Hospital, including Paolo Macchiarini, had performed the world’s first autologous stem cell-complexed bio-nano-artificial trachea, which was the first time that an artificial trachea had been transplanted into a patient that had been completely “grown up” in the laboratory. For the first time, a fully “grown” artificial trachea was successfully transplanted into a patient. This is the world’s first successful transplant of a cultured organ and is considered a milestone in the medical world.
Nanomaterials have become a hotspot for transplantation-related research due to their editable and highly targeted properties [11]. The deepening of the concept of precision medicine, offers the possibility of rapid and accurate assessment of human organ function, timely diagnosis and treatment of complications, and immunosuppressive protocols with low adverse effects during the management of organ transplantation patients.
3. Problems faced in the application of nanotechnology
3.1. Toxic side effects
Li et al. found that TiO2 NPs did not reduce the diversity of intestinal microorganisms in mice, and rutile TiO2 NPs accumulated in the spleen, lungs, and kidneys of mice, disrupted the morphology and arrangement of intestinal epithelial cells, and altered the composition of intestinal flora [12]. Jing found that TiO2 NPs decreased the cell viability of intestinal epithelial IEC-6 cells, interfered with the expression of tight junction proteins in IEC-6 cells, and also produced an inflammatory response. TiO2 NPs may also be toxic to other organs of the digestive system, indirectly affecting the intestinal flora(See Table 1) [13].
Table 1. Effect of nano on intestinal flora [13].
Subject (of an experiment) | Poisoning dose | Poisoning time | Changes in intestinal flora | Other effects |
infancy mice | 0.1 percent in the diet | 90 d | The effect on the diversity of intestinal flora is not significant, but it significantly reduces the abundance of concentrated probiotics including bifidobacteria and lactobacilli | Lower body weight than controls and increased Dextran Sulfate Sodium Salt (DSS)-induced chronic colitis and immune response. |
rats | 0, 2, 10, 50 mg (/ kg-d) | 30 d | Lactobacillus gasseri ↑ Trichosporonaceae NK4A136 group (L.NK4A136_group) ↑ | The intestinal morphology is markedly altered by pathological inflammatory infiltrates and mitochondrial abnormalities. |
rats | 0, 2, 10, 50 mg (/ kg-d) | 90 d | Lactobacillus_reuteri↑ (Romboutsia) bacteria ↓ | Mild hepatotoxicity with mitochondrial swelling. 29 metabolites and two metabolic pathways were significantly altered, with a marked increase in lipopolysaccharide (LPS) production by gut microbes |
In the use of nanoparticles stronger passive targeting biodistribution to treat tumors localized in MPS (e.g., hepatocellular carcinoma), this targeting will enhance the toxic side effects of anticancer drugs: such as inducing apoptosis of hepatic Kupfer cells, followed by Kupffer cell defects, so that the liver’s uptake of the drug is reduced , which is not conducive to hepatocellular carcinoma therapy[14]; nanoparticles into the organism, on body fluids, cells, tissues, Nanoparticles enter the organism and produce toxic reactions to body fluids, cells, tissues, molecules and even nucleotide fragments, therefore, from the contact pathway to the distribution in the body, the target organs and target tissues should attract our sufficient attention. Nanoparticles can enter the bloodstream or the central nervous system and may affect the function of the heart and brain.
3.2. Experimental conditions and ethical constraints
Most of the research on nanoparticle carriers is still in the stage of in vitro and in vivo animal testing, and large-scale application requires long-term clinical trials, as well as pharmacological efficacy and toxicological points. Due to the experimental conditions, technology and ethical restrictions, it is difficult to directly carry out experimental research on intestinal flora in the human body, so we usually choose common experimental animals or in vitro experiments to carry out the research, and the animal experimental research is only for reference, and is not suitable for extrapolation to human beings. Species differences play a more important role in nanomedicine research, but it is difficult to directly carry out population experiments.
3.3. Relevant policy constraints
Most pharmaceutical nanoparticles have more complex properties, numerous components, and heterogeneous structures compared to traditional pharmaceutical products that typically use a single active agent. Some components can affect the pharmacological behavior of the active ingredients in pharmaceutical products. Considering these complexities, the supervision and management of nanomedicines may face some problems [15]. Currently, FDA, EMA, and other agencies evaluate new drugs based on the specific conditions of the disease within the traditional benefit/risk analysis framework. The list of nanoparticle-based drugs approved by the US FDA remains limited, with over 500 active clinical trials involving nanoparticles identified by the end of 2022. To date, the U.S. Food and Drug Administration (FDA) has approved more than 60 nanomedicines, most of which are used to treat cancer (53%) and infectious diseases (14%).
3.4. Biological barrier crossing
Nanoparticles have developed different drug delivery pathways in the process of drug delivery, such as oral cavity, nasal cavity, eye, transdermal, parenteral, etc. Nanoparticles need to break through several biological barriers in order to successfully reach their desired disease site, which mainly depends on the drug delivery pathway and target organs [16]. The most preferred pathway for bioactive molecules and drugs is oral drugs, but oral drugs face many challenges, such as overcoming the low stability, low solubility, and low bioavailability of many drugs. For example, some drugs lose their activity in the gastrointestinal tract (GIT) before being absorbed, because the wide pH value in the GIT system creates an acidic environment in the gastric cavity and a large number of degrading enzymes hinder drug dissolution. Furthermore, the mucous layer in the intestine covers the epithelial surface, hindering NPs from penetrating the intestinal epithelium, as the rapid secretion and shedding of GIT mucus greatly limits the nanoparticle drug delivery system.
3.5. Occupational risks
The article “Exposure to nanoparticles may cause pleural effusion, lung fibrosis and granulomas” published in the European Respiratory Journal in August 2009 has triggered a heated debate in the academic community. Occupational environmental health experts believe that improving the working environment and ensuring occupational safety is a priority, regardless of whether the death of the worker was caused by nanoparticles. Although there is no clear report on the pathogenic mechanism of nanoparticles on human body, there are animal experiments suggesting that nanoparticles can cause direct damage to living organisms. At the very least, this incident highlights the importance of occupational risk management in nanotechnology, especially for those who are exposed to nanoparticles for prolonged periods. Considering that nanotechnology, like the discovery of X-rays, may be a double-edged sword, it is important to pay attention to the health of occupational groups while developing nanotechnology.
4. Conclusion
To sum up, nanobiomaterials, as a new type of biomaterials, can well solve many drawbacks of traditional biotechnology, and have shown unique advantages in the field of biomedicine, with good application prospects. The development of polymer materials, biotechnology, information technology, nanotechnology, and tissue engineering technology, will accelerate the promotion of basic research on nanoparticles and biomedical applications, so that it will enter a new stage. The research of medical nanoparticles will provide a brand-new technical platform for precise drug delivery, treatment of malignant tumors and infectious diseases, and conquering genetic diseases. The development of nanotechnology will certainly promote the progress and development of medical technology. The wide application of various experimental methods containing nanoparticles and the value of nanoparticles in laboratory medicine will greatly improve the performance of detection methods such as specificity, sensitivity and speed. It is believed that more new nanomaterials will appear and be applied in new disease detection and treatment in the near future.
References
[1]. Freitas, R. A. “Nanomedicne, Volume Ⅰ: Basic capabilities “. landes bioscience, TX,1999.
[2]. Commission Recommendation 2011/696/EU on the Definition of Nanomaterial , OJ L 275/38, 20.10. 2011.
[3]. Boyang, H.and Qingyue, L. “Engineering surface patterns on nanoparticles: new insights on nano-bio interactions.” J MATER CHEM. Issue 14, 2022.
[4]. Sahoo, SK.and Labhasetwar, V. “Nanotech approachesto drug delivery and imaging” ,DRUG DISCOV TODAY. 2003; 8(24): 1112-1120.
[5]. Zhou, W. and Hu, K. et al. “Gold nanoparticle aggregation-induced quantitative photothermal biosensing using a thermometer: a simple and universal biosensing platform”.[J]. Analytical Chemistry, 2020, 92(3): 2739-2747.
[6]. Jiangda,Z. chengqun,L. yong,C. et al. “Preliminary study of silicon nanocarriers transfected into keratin-forming cells”. Journal of Chinese Physician, 2005, 7(10): 1332. 1334.
[7]. lambert, G.Fattal, E.Couvreur, P. “Nanoparticlate systems for thedelivery of antisense oligonucleotides”.[J] Adv Drug Deliv Rev,2001 ,47(1): 99-112.
[8]. Aynie, I. Vauthier, C and Chacun, E. et al. Spongelike alginate nanoparticles as a new potential system for the delivery of antisense oligonucleotides [J]. Antisense Nucleic Arid Drug Dev,1999,9(3):301-312.
[9]. Ying,D. Jason L, G. and Jianglin,W. et al. “Hierarchically designed bone scaffolds: from internal cues to external stimuli”. Biomaterials, 2019, 218:119334
[10]. Yong,Z. Lu, B and Yanan,Z. et al. “Type I collagen decorated nanoporous network on titanium implant surface promotes osseointegration through mediating immunomodulation, angiogenesis, and osteogenesis”.Biomaterials, 2022, 288: 121684.
[11]. Bujie, D.Mengxiao,Yu.and Jie, Z. “Transport and interactions of nano-particles in the kidneys” [j].Nat Rev Mater;2018.3(10):358-374.
[12]. Juan, L. Shengmei, Y.and Runhong, Lei.Gu et al. “Oral administration of rutile and anatase TiO2 nanoparticles shifts mouse gut microbiota structure” [J]. Nanoscale, 2018, 10(16):7736-7745.
[13]. William, D.Kristy, Moniz .Emma Allen,V.et al. “Impact of food grade and nano-TiO2 particles on a human intestinal community” [J]. Food Chem Toxicol, 2017, 106 (Pt A): 242-249.
[14]. Nano Foreign Medicine Biomedical Engineering Subsection Volume 28, Issue 3, June 2005.
[15]. Neil,d. “Challenges in Development of Nanoparticle-Based Therapeutics”. Aaps j. 2012, 14, 282-295.
[16]. Jie,w. Ze,l. and Guillaume Wientjes,M et al. Au “Delivery of siRNA Therapeutics: Barriers and Carriers”. AAPS J. 2010, 12, 492-503.
Cite this article
Geng,X. (2024). Research on the application of nanotechnology in biomedicine. Applied and Computational Engineering,60,133-140.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 4th International Conference on Materials Chemistry and Environmental Engineering
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Freitas, R. A. “Nanomedicne, Volume Ⅰ: Basic capabilities “. landes bioscience, TX,1999.
[2]. Commission Recommendation 2011/696/EU on the Definition of Nanomaterial , OJ L 275/38, 20.10. 2011.
[3]. Boyang, H.and Qingyue, L. “Engineering surface patterns on nanoparticles: new insights on nano-bio interactions.” J MATER CHEM. Issue 14, 2022.
[4]. Sahoo, SK.and Labhasetwar, V. “Nanotech approachesto drug delivery and imaging” ,DRUG DISCOV TODAY. 2003; 8(24): 1112-1120.
[5]. Zhou, W. and Hu, K. et al. “Gold nanoparticle aggregation-induced quantitative photothermal biosensing using a thermometer: a simple and universal biosensing platform”.[J]. Analytical Chemistry, 2020, 92(3): 2739-2747.
[6]. Jiangda,Z. chengqun,L. yong,C. et al. “Preliminary study of silicon nanocarriers transfected into keratin-forming cells”. Journal of Chinese Physician, 2005, 7(10): 1332. 1334.
[7]. lambert, G.Fattal, E.Couvreur, P. “Nanoparticlate systems for thedelivery of antisense oligonucleotides”.[J] Adv Drug Deliv Rev,2001 ,47(1): 99-112.
[8]. Aynie, I. Vauthier, C and Chacun, E. et al. Spongelike alginate nanoparticles as a new potential system for the delivery of antisense oligonucleotides [J]. Antisense Nucleic Arid Drug Dev,1999,9(3):301-312.
[9]. Ying,D. Jason L, G. and Jianglin,W. et al. “Hierarchically designed bone scaffolds: from internal cues to external stimuli”. Biomaterials, 2019, 218:119334
[10]. Yong,Z. Lu, B and Yanan,Z. et al. “Type I collagen decorated nanoporous network on titanium implant surface promotes osseointegration through mediating immunomodulation, angiogenesis, and osteogenesis”.Biomaterials, 2022, 288: 121684.
[11]. Bujie, D.Mengxiao,Yu.and Jie, Z. “Transport and interactions of nano-particles in the kidneys” [j].Nat Rev Mater;2018.3(10):358-374.
[12]. Juan, L. Shengmei, Y.and Runhong, Lei.Gu et al. “Oral administration of rutile and anatase TiO2 nanoparticles shifts mouse gut microbiota structure” [J]. Nanoscale, 2018, 10(16):7736-7745.
[13]. William, D.Kristy, Moniz .Emma Allen,V.et al. “Impact of food grade and nano-TiO2 particles on a human intestinal community” [J]. Food Chem Toxicol, 2017, 106 (Pt A): 242-249.
[14]. Nano Foreign Medicine Biomedical Engineering Subsection Volume 28, Issue 3, June 2005.
[15]. Neil,d. “Challenges in Development of Nanoparticle-Based Therapeutics”. Aaps j. 2012, 14, 282-295.
[16]. Jie,w. Ze,l. and Guillaume Wientjes,M et al. Au “Delivery of siRNA Therapeutics: Barriers and Carriers”. AAPS J. 2010, 12, 492-503.