1. Introduction
Schizophrenia is a severe and enduring mental illness that generally develops before age 25 and lasts for the rest of an individual’s life. Approximately 24 million people around the world are believed to suffer from this mental health condition.[1] Schizophrenia can develop varies symptoms, including positive and negative symptoms such as hallucinations, delusions, and disorganized speech. These symptoms have a considerable negative impact on all areas of life, including personal, family, social, educational, and professional functioning. Schizophrenia is distinguished by a markedly distorted perception of reality, which is detached from reality itself. Despite extensive research, the precise cause of schizophrenia remains unknown. Instead, several risk factors have been identified that contribute to the development of the condition. There is a common misconception between schizophrenia and dissociative identity disorder (DID). This may be attributed to the similarities between their symptoms and influencing factors.
2. Causes for schizophrenia
The exact causes that lead to schizophrenia are poorly understood. Studies suggest that multiple factors including physical and genetic, psychological and environmental may come into play that may make a person vulnerable to developing this disease. [2] Nature-nurture is a common debate among scientists. There is a longstanding controversy over the relative contributions that genes and experience make to developing psychological traits and behaviors. It is the same for schizophrenia. Genetic, environmental factors, and brain changes all contribute to schizophrenia development to some extent.
2.1. Genetics
First, genes exert a significant influence on the development of mental illness, with schizophrenia representing an illustrative example. The data indicated that the risk of developing schizophrenia is elevated by 40% in identical twins with the disease. This high concordance rate in monozygotic twins suggests a strong genetic component. The risk of developing schizophrenia is also increased for individuals with a relative diagnosed with the disease, with the degree of increased risk dependent on the closeness of the genetic relationship.[3]
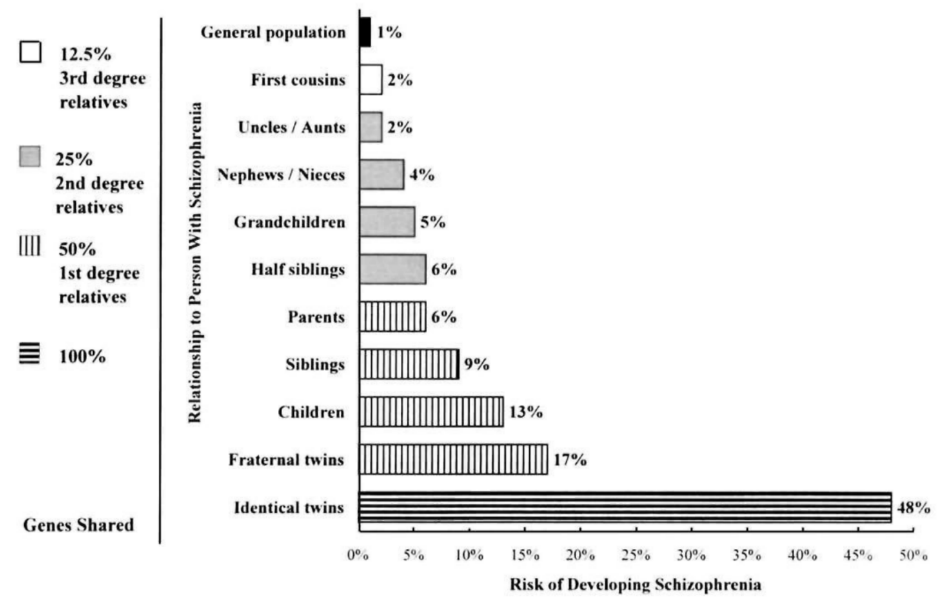
Figure 1: the risk of developing schizophrenia based on genes shared[4].
An additional data set provides further evidence to support the gene hypothesis. In the data set below, the variable "DZ" represents dizygotic twins, while the variable "MZ" represents monozygotic twins. The histogram demonstrates that monozygotic twins possess an average probability of over 50% for schizophrenia, whereas dizygotic twins exhibit an average probability of approximately 10%.[5] The evidence suggests that schizophrenia affects less than one in ten dizygotic twins, but approximately five in ten monozygotic twins. Gottesman’s research on familial and twin studies supports the view that genetics significantly contribute to schizophrenia, with the nature-nurture model being roughly balanced.
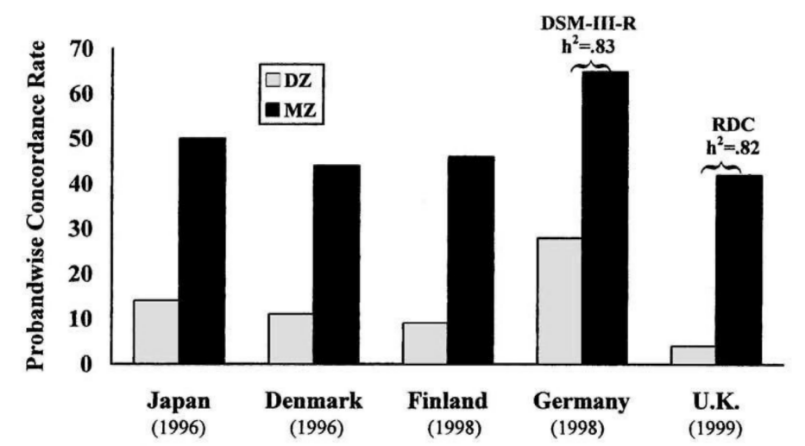
Figure 2: the risk of developing schizophrenia for dizygotic and monozygotic twins in different countries[6].
Furthermore, it is important to note that there are rare disruptive mutations that are implicated in schizophrenia. The scientists used whole-genome sequencing study to compare the samples from the schizophrenia subjects with those of their unaffected first-degree relatives in order to obtain a polygenic burden of rare mutations.[7] The studies indicate that patients with schizophrenia have a higher risk of having these rare mutations; these are believed to disrupt the function of genes that are essential for neuronal transmission and synaptic integration.[8] The reduction in synaptic connection might lead to the loss of some functionalities in the brain. Thus, it can be hypothesized that such rare mutations may play a role in the development of schizophrenia.
Moreover, there are associations between schizophrenia and variants in genes encoding synaptic proteins. A genetic analysis involving a large sample of individuals with schizophrenia and controls was conducted by a group of researchers. There is a significant association between specific genetic variants of synaptic vesicle glycoprotein 2A gene (SV2A) and the risk of developing schizophrenia. The study emphasizes the potential role of SV2A in synaptic transmission and its relevance to the pathophysiology of schizophrenia.[9] The findings suggest that genetic variations in SV2A may contribute to the disorder's development, highlighting the importance of synaptic mechanisms in schizophrenia. The increasing risk of getting schizophrenia has a correlation with a polymorphism in the SV2A gene, although this finding has not been replicated in genome-wide association studies.
Finally, it has been demonstrated that individuals with 22q11.2 deletion syndrome are at an elevated risk of developing schizophrenia. 22q11.2 deletion syndrome is defined by a microdeletion of a specific region on chromosome 22. This deletion encompasses multiple genes that are believed to be instrumental in neural development and function. 22q11.2 deletion syndrome has been linked to disruptions in brain development, specifically in regions involved in cognitive processes and emotion regulation.[10] Additionally, alterations in dopamine and glutamate signaling pathways, which are recognized as contributing to the pathophysiology of schizophrenia, and abnormalities in neural circuit connectivity may contribute to the cognitive and behavioral symptoms observed in affected individuals.[11] Estimates suggest that approximately 25-30% of individuals with this syndrome will experience psychotic symptoms in their lifetime, elevating the chance of developing schizophrenia.
2.2. Environment
Environmental factors refer to a number of variables. Substance abuse, stressful life events, and prenatal events are all potential contributors that may increase the likelihood for people to develop schizophrenia in their life.
The use of tobacco and other substances, including cannabis, is highly prevalent among individuals diagnosed with schizophrenia. According to the study, smoking increases the vulnerability to schizophrenia. The effects of nicotine on the brain and release of dopamine, a neurotransmitter that plays a role in how we feel pleasure. There is an excess amount of dopamine receptors in people’s brain who have schizophrenia. It is theorized that an overactive dopamine system may intensify brain signals in schizophrenia, thereby creating positive symptoms such as hallucinations and paranoia. Not to mention that Smoking brought 14.5 year for patients with shorter-than-average life expectancy of the negative effects.[12] Cannabis use also has a high prevalence in patients with diagnosed schizophrenia. 67% of patients initiating substance abuse prior to the onset of schizophrenia symptoms.[13] These patients tend to display positive symptoms, especially delusions and hallucinations, when compared to the other abusers.
There is a strong correlation between experiences of childhood trauma, such as abuse, neglect, and loss, and an increased risk of developing psychotic disorders later in life, including schizophrenia. Various forms of trauma were examined, including physical, emotional, and sexual abuse. The researchers emphasized that both the severity and the chronicity of trauma are significant factors in the risk of developing psychosis. Childhood trauma may lead to psychosis through multiple pathways, including neurobiological changes and cognitive psychological mechanisms. Trauma can affect brain development, stress response systems, and neurochemical processes; it may also disrupt normal cognitive development and coping mechanisms, leading to maladaptive beliefs and behaviors associated with psychosis.[14]
Stressful life events, particularly those involving significant changes or crises, such as the loss of a loved one, are often reported in the histories of individuals who develop schizophrenia. The research classified life events into two categories: negative life events and positive life events. They found that both can contribute to the onset of psychosis. Negative life events include stressful situations that can lead to emotional distress and are more likely to precipitate schizophrenia. On the other hand, positive life events like marriage or job promotions can lead to stress and subsequently trigger psychotic episodes. The onset of schizophrenia frequently occurred shortly after major life events, suggesting a temporal link between life crises and the onset of symptoms.[15] However, not everyone exposed to life crises develops schizophrenia, individual vulnerability factors are different, such as pre-existing psychological conditions or genetic predisposition, and this changes their risk of getting schizophrenia when facing stress.
Prenatal development or delivery has been identified as a potential influencing factor in the occurrence of brain abnormalities in individuals diagnosed with schizophrenia. The development of the brain during critical periods may be a contributing factor to the formation of psychopathology observed in schizophrenia. Evidence from various studies indicates that factors such as genetic predisposition, prenatal exposures, and environmental stressors contribute to abnormal neurodevelopment. Some of the factors are low birth weight, maternal diabetes, older age of the father, and lack of oxygen during birth.[16] It has been proposed that infections during pregnancy, especially at different phases of fetal brain development, are associated with schizophrenia and other neurodevelopmental disorders.[17] Data obtained from clinical research indicates that immune dysfunction could be a major contributing factor in the development of the condition.
2.3. Neurodevelopmental Factor
One important discovery in schizophrenia research is the finding that medications which inhibit dopamine receptors can effectively decrease the intensity of symptoms such as hallucinations and delusions.[18] This has led to the development of the dopamine hypothesis of schizophrenia, suggesting that overactive dopamine receptors may be responsible for causing schizophrenia. [19] The study found that patients with schizophrenia exhibited significantly higher levels of dopamine D2 receptors in the striatum compared to healthy controls. This finding suggests a hyperdopaminergic state in individuals with schizophrenia. The researchers noted a correlation between increased dopamine receptor density and the severity of positive symptoms, such as hallucinations and delusions, in patients.[20] This supports the hypothesis that dopaminergic dysregulation is associated with the manifestation of psychotic symptoms. The results provide strong empirical support for the dopamine hypothesis of schizophrenia, which posits that overactivity of dopamine transmission contributes to the pathophysiology of the disorder.
3. Similarities Between Schizophrenia and DID
Schizophrenia and dissociative identity disorder (DID) are two very different but often confused mental disorders. Because the name "schizophrenia" comes from the Greek words for "split" ("schizo") and "mind" ("phren"), people may mistakenly think it is related to DID, which mental health professionals previously called "dissociative identity disorder." Schizophrenia is a mental disorder with pronounced signs of reality distortion. Hallucinations, delusions, and disorganized thinking are well-known features of psychosis, where your brain perceives things that are not real. Dissociative identity disorder is a mental illness characterized by recurrent memory loss and two or more distinct personality states.[21]
3.1. Causes
What has been shown is that both DID and schizophrenia can be triggered by exposure to stressful stimuli. DID can be the consequence of traumatic events, and as is mentioned in the previous section, it is the same for schizophrenia. DID is often brought on by a traumatic event, which can occur at an early age, with the development of the disorder taking place before the age of nine. According to the American Psychiatric Association, it was found that 90 percent of people diagnosed with DID in the USA, Canada, and Europe had a history of severe neglect and abuse during childhood.[22] These include experiences that involve physical abuse, sexual abuse, and emotional abuse, which have similarities with the predisposing factors of schizophrenia.
3.2. Symptoms
Dissociative disorders involve impairments in cognitive processes, personal identity, and memory, which in turn give the patient a feeling of being disconnected from reality. The most striking feature of schizophrenia is represented by impaired thinking, emotion, behavior, and perception, rather than the impairment of different personality states. DID and schizophrenia both cause a person to have changes in behavior, thought patterns, memory, emotional functioning, and social relationships. Both disorders also share many signs and symptoms such as hallucinations, psychosis, memory loss or amnesia, and feeling detached from people.[23]
Many people confuse the two disorders because their criteria overlap. One study found that 74.3 percent of patients diagnosed with DID also meet the criteria for schizophrenia, while 18.7 percent of those with schizophrenia met the criteria for DID. Furthermore, 27 to 41 percent of DID patients have had a previous diagnosis of schizophrenia.[24] Hearing voices in the mind can lead individuals to experience a sense of having multiple identities in their brain.
3.3. Misconceptions
The problem of misdiagnosing DID for schizophrenia is a common and concerning issue, especially in clients with histories of trauma, because both disorders can present psychotic features.[25] This is a result of historical misconceptions and complicated presentations of the symptoms associated with the conditions. There is a common misconception that schizophrenia and DID can be used interchangeably being schizophrenic and having symptoms like hallucinations mean a person has multiple personalities. Consequently, many DID patients are misdiagnosed as schizophrenic and receive treatment for conditions they do not have.
Misdiagnosis does not only hinder treatment, but it also impacts the patient’s health and healing process. This issue shows the importance of expert clinical evaluations and increased awareness among practitioners concerning the characteristics of each of the disorders. In this case, enhanced training in the differential diagnosis between psychotic and dissociative symptoms can make a positive impact through accurate diagnosis of the disorder to enable the patients to receive the right treatment. While research is still being conducted to distinguish and compare the two disorders and their causes, the information that is being gathered will help to eliminate confusion and misdiagnosis to ensure that the patients suffering from the two disorders receive the right treatment. It is crucial to meet these diagnostic challenges to improve mental health services and guarantee that those affected get the proper help.
4. Conclusion
Overall, many factors change the risk of getting schizophrenia, including but not limited to genes, substance abuse, prenatal development, and the number of dopamine receptors. Childhood trauma is the cause of both schizophrenia and DID. The symptoms of these two disorders make people confused, which leads to misconception and misdiagnosis. Misdiagnosis not only hinders the treatment process but also influences patients’ mental health. Therefore, education for people about mental disorders and carefulness in diagnosing the disorder should be a field for people to look at in the future.
References
[1]. World Health Organization. (n.d.). Schizophrenia. Retrieved August 3, 2024, from https://www.who.int/news-room/fact-sheets/detail/schizophrenia
[2]. National Health Service. (n.d.). Schizophrenia: Causes. Retrieved August 3, 2024, from https://www.nhs.uk/mental-health/conditions/schizophrenia/causes/
[3]. Gottesman, I. I. (1991). Schizophrenia genesis: The origins of madness. WH Freeman/Times Books/Henry Holt & Co.
[4]. Compiled From Family and twin studies in European populations between 1920 and 1987 From Schizophrenia Genesis: The Origins of Madness (p 96). by I. I. Gottesman 1991 New York: Freeman. Copyright 1991 by I. I. Gottesman.
[5]. Gottesman, I. I. (2001). Psychopathology through a life span-genetic prism. American Psychologist, 56(11), 867–878. https://doi.org/10.1037/0003-066X.56.11.867
[6]. A. G. Cardno and I. I. Gottesman, personal communication, July 27, 1999.
[7]. Halvorsen, M., Huh, R., Oskolkov, N., et al. (2020). Increased burden of ultra-rare structural variants localizing to boundaries of topologically associated domains in schizophrenia. Nature Communications, 11, 1842. https://doi.org/10.1038/s41467-020-15707-w
[8]. Howes, O. D., & Onwordi, E. C. (2023). The synaptic hypothesis of schizophrenia version III: A master mechanism. Molecular Psychiatry, 28, 1843–1856. https://doi.org/10.1038/s41380-023-02043-w
[9]. Onwordi, E. C., Halff, E. F., Whitehurst, T., et al. (2020). Synaptic density marker SV2A is reduced in schizophrenia patients and unaffected by antipsychotics in rats. Nature Communications, 11, 246. https://doi.org/10.1038/s41467-019-14122-0
[10]. Qin, X., Chen, J., & Zhou, T. (2020). 22q11.2 deletion syndrome and schizophrenia. Acta Biochimica et Biophysica Sinica, 52(11), 1181–1190. https://doi.org/10.1093/abbs/gmaa113
[11]. Frith, C. D., & Blakemore, S.-J. (2004). Schizophrenia: Neuroscience perspective. The British Journal of Psychiatry, 185(Supplement 47), s30-s37. https://doi.org/10.1192/bjp.185.47.s30
[12]. Owen, M. J., Sawa, A., & Mortensen, P. B. (2016). Schizophrenia. The Lancet, 388(10039), 86-97. https://doi.org/10.1016/S2215-0366(17)30078-0
[13]. Bersani, G., Orlandi, V., Kotzalidis, G., et al. (2002). Cannabis and schizophrenia: Impact on onset, course, psychopathology and outcomes. European Archives of Psychiatry and Clinical Neurosciences, 252, 86–92. https://doi.org/10.1007/s00406-002-0366-5
[14]. Read, J., Fosse, R., Moskowitz, A., & Perry, B. (2005). Childhood trauma, psychosis and schizophrenia: A literature review with theoretical and clinical implications. Acta Psychiatrica Scandinavica, 112(5), 330–350. https://doi.org/10.1111/j.1600-0447.2005.00634.x
[15]. Brown, G. W., & Birley, J. L. T. (1968). Crises and life changes and the onset of schizophrenia. Journal of Health and Social Behavior, 9(3), 203–214. https://doi.org/10.2307/2948405
[16]. King, M. D., Fountain, C., Dakhlallah, D., & Bearman, P. S. (2010). KING ET AL. RESPOND. American Journal of Public Health, 100(3), 390. https://doi.org/10.2105/AJPH.2009.184168
[17]. Wakefield, J. (2004). Children’s health: Flu, fetuses, and schizophrenia. Environmental Health Perspectives, 112(17), A986. https://doi.org/10.1289/ehp.112-a986
[18]. Seeman, P. (1986). Dopamine receptor binding and the dopamine hypothesis of schizophrenia. Journal of Psychiatric Research, 20(3), 259–274. https://doi.org/10.1016/0022-3956(86)90021-7
[19]. van Rossum, J. M. (1966). The significance of dopamine-receptor blockade for the mechanism of action of neuroleptic drugs. Archives Internationales de Pharmacodynamie et de Thérapie, 160(2), 492–494.
[20]. Wong, D. F., Wagner, H. N. Jr., Binswanger, U., et al. (1986). Dopamine and schizophrenia: A study with positron emission tomography. Archives of General Psychiatry, 43(3), 266–272. https://doi.org/10.1001/archpsyc.1986.01800030034006
[21]. American Psychiatric Association. (n.d.). DSM-5. Retrieved August 3, 2024, from https://www.psychiatry.org/psychiatrists/practice/dsm
[22]. American Psychiatric Association. (n.d.). What are dissociative disorders? Retrieved August 3, 2024, from https://www.psychiatry.org/patients-families/dissociative-disorders/what-are-dissociative-disorders
[23]. American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Association.
[24]. Renard, S. B., Huntjens, R. J., Lysaker, P. H., Moskowitz, A., Aleman, A., & Pijnenborg, G. H. (2017). Unique and overlapping symptoms in schizophrenia spectrum and dissociative disorders in relation to models of psychopathology: A systematic review. Schizophrenia Bulletin, 43(1), 108–121. https://doi.org/10.1093/schbul/sbw063
[25]. Healthline. (n.d.). DID vs. schizophrenia. Retrieved August 3, 2024, from https://www.healthline.com/health/schizophrenia/did-vs-schizophrenia#causes
Cite this article
Li,P. (2025). Investigating the Etiological Factors of Schizophrenia and Its Diagnostic Overlap with Dissociative Identity Disorder . Communications in Humanities Research,56,183-189.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of 3rd International Conference on Interdisciplinary Humanities and Communication Studies
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. World Health Organization. (n.d.). Schizophrenia. Retrieved August 3, 2024, from https://www.who.int/news-room/fact-sheets/detail/schizophrenia
[2]. National Health Service. (n.d.). Schizophrenia: Causes. Retrieved August 3, 2024, from https://www.nhs.uk/mental-health/conditions/schizophrenia/causes/
[3]. Gottesman, I. I. (1991). Schizophrenia genesis: The origins of madness. WH Freeman/Times Books/Henry Holt & Co.
[4]. Compiled From Family and twin studies in European populations between 1920 and 1987 From Schizophrenia Genesis: The Origins of Madness (p 96). by I. I. Gottesman 1991 New York: Freeman. Copyright 1991 by I. I. Gottesman.
[5]. Gottesman, I. I. (2001). Psychopathology through a life span-genetic prism. American Psychologist, 56(11), 867–878. https://doi.org/10.1037/0003-066X.56.11.867
[6]. A. G. Cardno and I. I. Gottesman, personal communication, July 27, 1999.
[7]. Halvorsen, M., Huh, R., Oskolkov, N., et al. (2020). Increased burden of ultra-rare structural variants localizing to boundaries of topologically associated domains in schizophrenia. Nature Communications, 11, 1842. https://doi.org/10.1038/s41467-020-15707-w
[8]. Howes, O. D., & Onwordi, E. C. (2023). The synaptic hypothesis of schizophrenia version III: A master mechanism. Molecular Psychiatry, 28, 1843–1856. https://doi.org/10.1038/s41380-023-02043-w
[9]. Onwordi, E. C., Halff, E. F., Whitehurst, T., et al. (2020). Synaptic density marker SV2A is reduced in schizophrenia patients and unaffected by antipsychotics in rats. Nature Communications, 11, 246. https://doi.org/10.1038/s41467-019-14122-0
[10]. Qin, X., Chen, J., & Zhou, T. (2020). 22q11.2 deletion syndrome and schizophrenia. Acta Biochimica et Biophysica Sinica, 52(11), 1181–1190. https://doi.org/10.1093/abbs/gmaa113
[11]. Frith, C. D., & Blakemore, S.-J. (2004). Schizophrenia: Neuroscience perspective. The British Journal of Psychiatry, 185(Supplement 47), s30-s37. https://doi.org/10.1192/bjp.185.47.s30
[12]. Owen, M. J., Sawa, A., & Mortensen, P. B. (2016). Schizophrenia. The Lancet, 388(10039), 86-97. https://doi.org/10.1016/S2215-0366(17)30078-0
[13]. Bersani, G., Orlandi, V., Kotzalidis, G., et al. (2002). Cannabis and schizophrenia: Impact on onset, course, psychopathology and outcomes. European Archives of Psychiatry and Clinical Neurosciences, 252, 86–92. https://doi.org/10.1007/s00406-002-0366-5
[14]. Read, J., Fosse, R., Moskowitz, A., & Perry, B. (2005). Childhood trauma, psychosis and schizophrenia: A literature review with theoretical and clinical implications. Acta Psychiatrica Scandinavica, 112(5), 330–350. https://doi.org/10.1111/j.1600-0447.2005.00634.x
[15]. Brown, G. W., & Birley, J. L. T. (1968). Crises and life changes and the onset of schizophrenia. Journal of Health and Social Behavior, 9(3), 203–214. https://doi.org/10.2307/2948405
[16]. King, M. D., Fountain, C., Dakhlallah, D., & Bearman, P. S. (2010). KING ET AL. RESPOND. American Journal of Public Health, 100(3), 390. https://doi.org/10.2105/AJPH.2009.184168
[17]. Wakefield, J. (2004). Children’s health: Flu, fetuses, and schizophrenia. Environmental Health Perspectives, 112(17), A986. https://doi.org/10.1289/ehp.112-a986
[18]. Seeman, P. (1986). Dopamine receptor binding and the dopamine hypothesis of schizophrenia. Journal of Psychiatric Research, 20(3), 259–274. https://doi.org/10.1016/0022-3956(86)90021-7
[19]. van Rossum, J. M. (1966). The significance of dopamine-receptor blockade for the mechanism of action of neuroleptic drugs. Archives Internationales de Pharmacodynamie et de Thérapie, 160(2), 492–494.
[20]. Wong, D. F., Wagner, H. N. Jr., Binswanger, U., et al. (1986). Dopamine and schizophrenia: A study with positron emission tomography. Archives of General Psychiatry, 43(3), 266–272. https://doi.org/10.1001/archpsyc.1986.01800030034006
[21]. American Psychiatric Association. (n.d.). DSM-5. Retrieved August 3, 2024, from https://www.psychiatry.org/psychiatrists/practice/dsm
[22]. American Psychiatric Association. (n.d.). What are dissociative disorders? Retrieved August 3, 2024, from https://www.psychiatry.org/patients-families/dissociative-disorders/what-are-dissociative-disorders
[23]. American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Association.
[24]. Renard, S. B., Huntjens, R. J., Lysaker, P. H., Moskowitz, A., Aleman, A., & Pijnenborg, G. H. (2017). Unique and overlapping symptoms in schizophrenia spectrum and dissociative disorders in relation to models of psychopathology: A systematic review. Schizophrenia Bulletin, 43(1), 108–121. https://doi.org/10.1093/schbul/sbw063
[25]. Healthline. (n.d.). DID vs. schizophrenia. Retrieved August 3, 2024, from https://www.healthline.com/health/schizophrenia/did-vs-schizophrenia#causes