1 Introduction
Globally, there are 2450 per 100,000 people suffering the neck pain, while upper crossed syndrome is one of the most common reasons of it [1]. Upper crossed syndrome (UCS) is an anterior and posterior muscle imbalance pattern in the deep cervical flexors, lower trapezius and anterior serratus muscles are overstretched or over-weak, meanwhile, the muscles of the superior trapezius, levator scapulae, sternocleidomastoid, pectoralis major and pectoralis minor are shortened due to excessive tightness [2]. UCS causes numerous complications and clinical manifestations, including cervical degenerative diseases, cervical antiarch, cervical headache, neck pain, disorders of temporomandibular joint and scapular instability [2]. Min Cheol last year published a narrative systematic review of UCS arguing the effectiveness of various treatments, for example, muscle energy technique, soft-tissue mobilization and stretching exercises, which played effective roles in reducing neck pain, and improving imbalance postural pattern and neck disabilities [3]. It supplements the conditions and reasons for choosing different treatments for a previous review of Sajjad in 2017, which preferred muscle energy technique to stretching exercises attributed to effectiveness [4]. However, preceding systematic reviews and meta-analysis mainly focus on the ways or effectiveness of treatments, yet, the epidemiological review is a gap in the research of UCS.
This paper is a systematic review implying the prevalence of UCS in different countries. It searched all English papers reporting UCS in the electronic databases during the dates from the establishment of the database to June 2024 and conducted a meta-analysis of the national prevalence of UCS extracted from various studies, and a meta-regression of basic and social factors (gender, average age, economy and industrial structure) with national UCS prevalence. This systematic review indicated a need to further standardize the gold standard for UCS diagnosis between countries or continents, as well as mechanisms for UCS screening in the public health field.
2 Method
This study including the systematic review under the guide of PRISMA Guide2020, conducts a meta-analysis to calculate the prevalence of UCS in different countries and uses meta-regression to investigate the relationship between the prevalence of UCS, and basic factors (gender and average age) and national factors (economy and work time) [5].
2.1 Literature Search strategy
This paper searched the following electronic databases by comprehensive search strategy: (1) Guideline Website: the Cochrane Library; (2) Database: PubMed, Web of Science, Scopus, Science Direct. Adopt the method of combining subjective words (‘upper crossed syndrome’ and ‘prevalence of upper crossed syndrome’ or ‘prevalence of upper crossed syndrome’) and free words (‘age’ or ‘gender’ or ‘work time’) to search all types of paper published from the establishment of the database to June 2024.
2.2 Criteria
All papers were double-checked after being selected and screened twice by a master student of Public Health in University of Sydney.
Include criteria: (1) Age of participants >18 years old and with Upper Cross Syndrome: forward head posture (FHP) and forward shoulder posture (FSP), associated spinal changes and changes in shoulder girdle function; (2) Including prevalence of upper cross syndrome; (3) Participants are fully competent and conscious; (4) Language is English. The paper is adopted only if all inclusion criteria are met.
Exclude criteria: (1) Without Upper Cross Syndrome or prevalence; (2) Full text is not available; (3) Multiple diseases in one study; (4) Grey literature; (5) Sample size <10. If any condition of the exclusion criteria is met, the paper is deleted.
2.3 Data extraction
This systematic review extracted the following factors from total studies: the first author, published year, study type, sample size, country, prevalence, 95% Confidence interval, sex ratio and age.
The Joanna Briggs Institute Critical Appraisal tools for use in JBI Systematic Reviews were used to assess the 7 papers in this review (Yes: 1 score, NO, Unclear and Not applicable: 0 score) [6]. Finally, all scores would sum up to assess the quality of papers (7-8: high quality, under 7: fair quality).
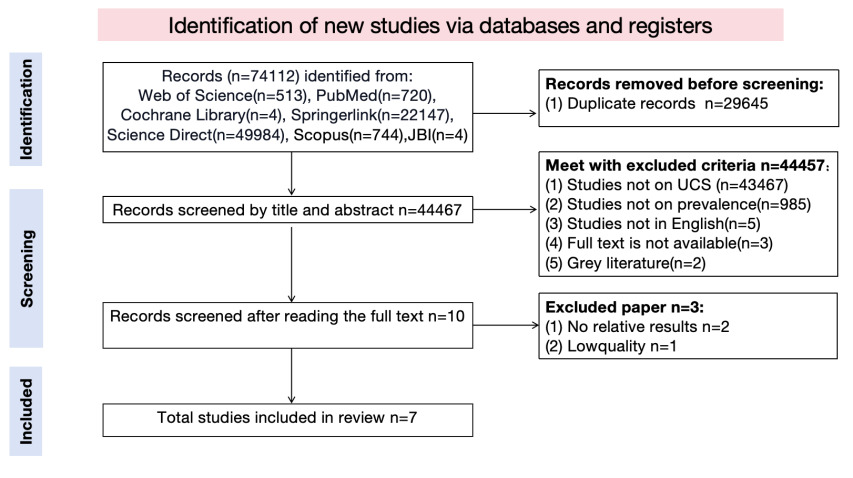
Figure 1. Flow diagram of literature search
2.4 Data analysis
As Figure 2 shows, this systematic review used Jamovi Version 2.3 to analyze all data collected from 7 papers and a random-effect meta-analysis to pool the prevalence rate of UCS [7-8]. Cochran’s Q and I2 Statistics calculated the heterogeneity between studies (I2=25%: low heterogeneity, I2=50%: medium heterogeneity, I2=75%: high heterogeneity). The sex ratio, assessment way and quality of paper were used to analyze the origin of heterogeneity between studies. Fail-safe n analysis (file drawer analysis) and rank correlation test for funnel plot asymmetry were the ways of publication bias assessment (statistical significance: p=0.05) [9].
3 Result
Figure 1 shows after screening 74112 records in the database, 7 papers met with included criteria in this systematic review to have meta-analysis. 29645 out of 74112 were deleted as duplicate records and 44457 records were deleted due to being in the excluded criteria or not in the included criteria.
3.1 Characteristics of included papers
The main characteristics of the included papers are shown in Table 1. Finally, there are have 7 papers in this systematic review, which involved 3722 participants with UCS. All studies were published in 2019-2023 and taken in Asia, most of which were in Pakistan (n=5, 71.4%) [10-13]. The sample size was from 37 Pakistan therapists to 2552 Chinese students. The assessment tools were divided into a pain questionnaire (NRS, Neck Disability Index and Modified Oswestry Neck Disability Index Questionnaire) and posture evaluation (Reedco Postural Assessment Scale, Self-designed Posture Motion and The American College of Sport Medicine) [14-16].
3.2 Quality of included papers
Table 2 shows all the characteristics of the paper this systematic review included. 6 out of 7 studies made specific standards of included samples (86.71%). 3 studies identified the confounding factors in the research (42.9%) and only 2 of them claimed the strategies for dealing with confounding factors (28.57%). Moreover, objective standard criteria were used for the measurement of the condition in all studies. Meanwhile, outcomes of all studies were measured in a valid and reliable way and in the appropriate statistical analysis.
According to the JBI Critical Appraisal Checklist for systematic review, the average score of all included papers was 6.71(from 6 to 8). The average score of 4 high quality studies (57.14%) was 7.25 while the average score of 3 fair quality studies (42.8%) was 6.
According to Figure 2, the pooled prevalence estimate of UCS was found to be 0.35 (95%CI: 0.25-0.44). There was significant heterogeneity across studies used for this analysis (I2:95.5%, P<0.0001).
In the subgroup analysis of the sex ratio, when the sex ratio>1, the prevalence of UCS was 0.26 (95%CI: 0.22-0.30). However, if the sex ratio <1, the prevalence of UCS was 0.39 (95%CI: 0.24-0.53). In addition, there were significant statistical differences between the two subgroups.
In the subgroup analysis of the assessment tool, the prevalence of UCS was both 0.30 found on the pain questionnaire (95%CI:0.25-0.34) and posture evaluation (95%CI: -0.01-0.62). Yet, there were significant statistical differences between the two subgroups.
In the end, the subgroup analysis based on the quality of studies still had significant statistical differences. The prevalence of UCS in high quality studies was 0.38(95%CI:0.23-0.54). And the prevalence of UCS in fair quality studies was 0.19(95%CI:0.04-0.34).
3.3 Sensitive analysis
To ensure the potential origin of the heterogeneity in all studies and check the difference between study groups, this systematic review had stratification analysis in all included papers. As Table 3 shows, the analysis range was from sex ratio (sex ratio >1 and sex ratio <1), assessment tool (pain questionnaire and posture evaluation) and quality of included papers (high quality and fair quality). The results of this systematic review indicated that the prevalence of two subgroups of sex ratio and quality of papers existed diversity and significant statistical differences. Nevertheless, assessment too would not act on the prevalence of UCS even if there were significant statistical differences between subgroups.
3.4 Publication Bias
As Figure 3 shows, there was no potential evidence of publication bias, which was proved by the symmetrical Funnel plot, Rank Correlation Test (τ=0.143, P=0.7726) and Regression Test for Funnel Plot Asymmetry (Z=-1.280, P=0.20006).
Table 1. Research Characteristics
Study name |
Study type |
Country |
Sample size |
Case (n) |
Eventrate |
95% Confidence interval |
Data collection tool |
Sexratio |
Mean age |
Ayesha 2020[10] |
Cross sectional study |
Pakistan |
430 |
n=113 |
0.26 |
0.22-0.30 |
Reedco postural assessment scale |
3.10 |
29.63 |
Rizmi 2021[11] |
Cross sectional study |
Pakistan |
37 |
n=8 |
0.32 |
0.17-0.48 |
NRS/Neck disability index (pain) |
1.19 |
32.11 |
Hussaiz 2023[12] |
Cross sectional study |
Pakistan |
200 |
n=63 |
0.32 |
0.25-0.38 |
The Oswestry neck Disability index Questionnaire |
All female |
27.92 |
Mariyam 2021[13] |
Cross sectional study |
Pakistan |
148 |
n=40 |
0.27 |
0.20-0.34 |
Modified Oswestry Neck and Disability Index |
0.44 |
NT |
Ayesha 2022[14] |
Cross sectional study |
Pakistan |
305 |
n=110 |
0.36 |
0.31-0.41 |
self-designed questionnaire |
All female |
21.60 |
Chaowei 2023[15] |
Cross sectional study |
China |
2552 |
n=1524 |
0.60 |
0.58-0.62 |
The American Colege of Sport Medicine |
0.38 |
19.20 |
Junaid 2019[16] |
Cross sectional study |
India |
50 |
n=14 |
0.28 |
0.16-0.40 |
The Oswestry neck Disability index Questionnaire |
All male |
NT |
Total |
3722 |
1876 |
0.35 |
0.25-0.44 |
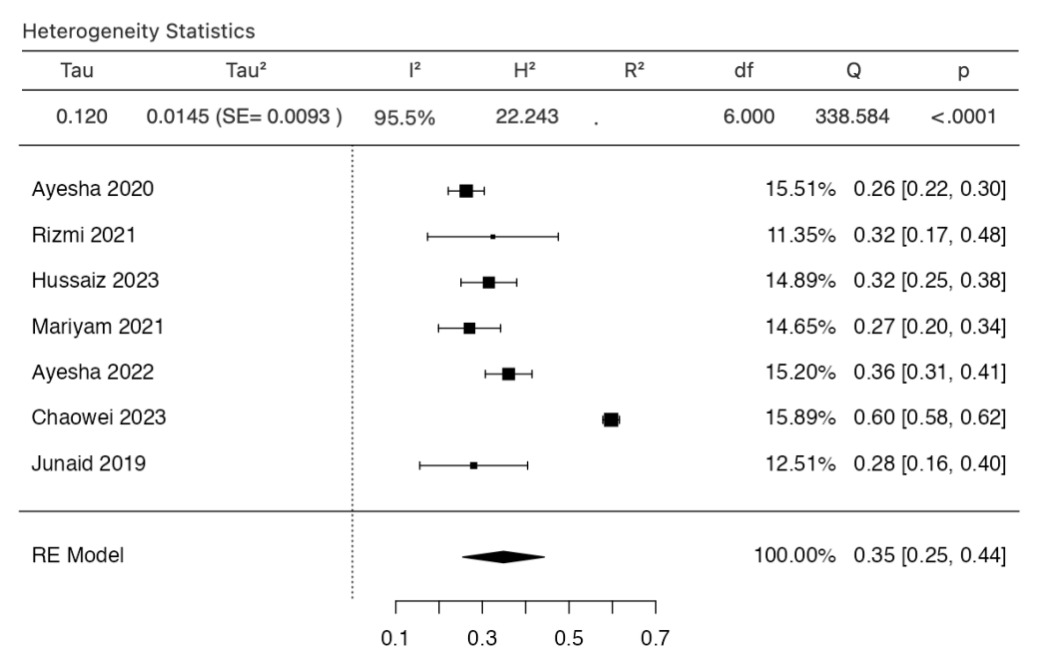
Figure 2. Forest plot
Table 2 The Joanna Briggs Institute Critical Appraisal tools for use in JBI Systematic Reviews [6]
Study name |
Q1 |
Q2 |
Q3 |
Q4 |
Q5 |
Q6 |
Q7 |
Q8 |
Total |
Quality |
Ayesha 2020 |
Y |
Y |
Y |
Y |
N |
N |
Y |
Y |
6 |
FAIR |
Rizmi 2021 |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
8 |
High |
Hussaiz 2023 |
Y |
Y |
Y |
Y |
Y |
N |
Y |
Y |
7 |
High |
Mariyam 2021 |
Y |
Y |
Y |
Y |
Y |
N |
Y |
Y |
7 |
High |
Ayesha 2022 |
Y |
Y |
Y |
Y |
N |
N |
Y |
Y |
6 |
FAIR |
Chaowei 2023 |
N |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
7 |
High |
Junaid 2019 |
Y |
Y |
Y |
Y |
N |
N |
Y |
Y |
6 |
FAIR |
Q1. Were the criteria for inclusion in the sample clearly defined? Q2. Were the study subjects and the setting described in detail? Q3. Was the exposure measured in a valid and reliable way? Q4. Were objective, standard criteria used for measurement of the condition? Q5. Were confounding factors identified? Q6. Were strategies to deal with confounding factors stated? Q7. Were the outcomes measured in a valid and reliable way? Q8. Was appropriate statistical analysis used? Y: Yes, N: No, U: Unclear NA: Not applicable |
||||||||||
Table 3 Sensitive analysis
Subgroups |
Studies, n |
Prevalence |
95%CI |
Heterogeneity across the studies |
Heterogeneity between groups (P-value) |
|
I2 |
P-value |
|||||
Sex ratio |
||||||
>1 |
3 |
0.26 |
0.22-0.30 |
0 |
0.7656 |
<0.0001 |
<1 |
4 |
0.39 |
0.24-0.53 |
97.3% |
<0.0001 |
|
Assessment |
||||||
Pain questionnaire |
4 |
0.30 |
0.25-0.34 |
0 |
0.7940 |
<0.0001 |
Posture evaluation |
3 |
0.30 |
-0.01-0.62 |
99.75% |
<0.0001 |
|
Quality of studies |
||||||
High |
4 |
0.38 |
0.23-0.54 |
0 |
0.6183 |
<0.0001 |
Fair |
3 |
0.19 |
0.04-0.34 |
96.62% |
<0.0001 |
|
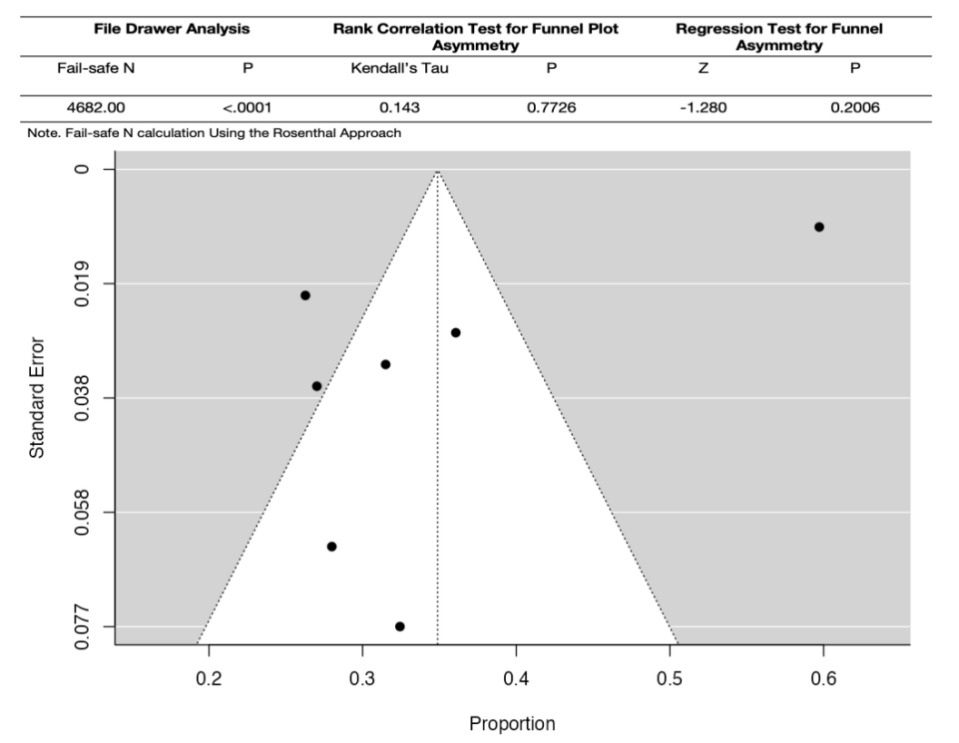
Figure 3. Funnel plot
4 Discussion
4.1 Main findings
This is a systematic review and meta-analysis of the prevalence of UCS. This systematic review included 7 studies to estimate the prevalence of UCS in different populations, which involved 3722 participants in total. All included studies were in Asia. Combining with qualitative and quantitative research, there was notable diversity in the prevalence of UCS, which depends on the sex ratio of participants, assessment tools and quality of papers.
In sum, the meta-analysis of this systematic review showed that the prevalence of UCS was higher in trials with more women (sex ratio< 1, 0.35) than in trials with more men (sex ratio>1, 0.26). In the high-quality papers, the prevalence of UCS (0.38) was well above the prevalence of fair quality papers (0.19). However, assessment tools would not differ in the prevalence of UCS (0.30).
4.2 Interpretation of the previous studies
The pooled estimated prevalence of UCS in this systematic review and meta-analysis was 0.35. It was 2.32 times compared to the previous symptomatic cervical spondylosis (0.138), which purports the significance necessary to put emphasis on UCS [17]. There were the following reasons for the more frequent prevalence of UCS rather than other symptomatic cervical Spondylosis: On the one hand, the systematic review of Min Cheol found that prior to clinical manifestations of pain and nerve compression, UCS presented obvious postural change such as anterior neck movement, which would be more conducive to effective intervention in the early stage of the disease, yet, symptomatic cervical spondylosis focused on the clinical manifestation such as headache and numbness in the arm [18]. On the other hand, Ather in 2008 presented that 88.8% women put emphasis on their appearance so that they would in the first time to seek professional help of postural change [19].
This systematic review found that there was a higher prevalence (0.39) in the study of sex ratio<1(sex ratio >1: 0.26), in other words, the prevalence would be higher if females more than males in this study. This was consistent with and further expanded previous conclusions by HUSSAIN that females (0.29) were found to be more prone to UCS than males (0.27) in Pakistan [12]. Combined with previous relevant studies, the possible reasons are discussed: Haizlip found that males’ muscle cross-sectional area and muscle mass were larger than women's overall, therefore females were more likely to fall into muscular imbalances [20]. From the perspective of anatomy, the cervical vertebrae of women are smaller and have more movements, and the Angle of movement is larger. Moreover, the physiological structure of the cervical vertebrae of men and women is different, and the intervertebral disc heights of C2-C3 and C6-C7 of women are lower than those of men (p < 0.05) [21-22]. These would both increase the prevalence of UCS. At last, in Llanos’s studies in 2022, from a psychological point of view, compared to men, women had a poorer perception of their own bodies and lower self-confidence, so it was easier to put their bodies in a crouching position [23]. In a nut, females should take more action to prevent themselves from UCS.
4.3 Implications of the findings
There were several significant strengths in this systematic review. It was the first systematic review and meta-analysis to reveal the prevalence of UCS in Asia. Furthermore, this systematic review had a paper quality evaluation and publication bias in details. last but not least, it had a sensitive analysis and subgroups analysis depending on the origin of papers, sex ratio, assessment tools and paper quality.
This systematic review had certain research significance and clinical practice potential. First of all, there was a need to further standardize the gold standard for UCS diagnosis between countries or continents, as well as mechanisms for UCS screening in the public health field. Moreover, it should have further studies in middle-income countries and high-income countries. In addition, for the complications related to UCS, such as cervical headache, community science popularization and school education were needed to increase the early diagnosis rate and intervention rate of UCS. Finally, the risk factors of UCS in daily life need further research and exploration to lay the foundation for public health interventions.
5 Conclusion
In conclusion, the prevalence of UCS was higher in females and people performing repeated movements for a long time. The subgroup studies showed a significant statistical difference, which means early screening and intervention based on different features of included samples have certain clinical significance. At the same time, it was necessary to explore the potential reasons for the high prevalence of UCS in Asia. Additionally, there is also a need to establish a unified gold standard for UCS diagnosis, as well as a standardized screening mechanism. There were few included papers, which could influence the accuracy of the estimated prevalence. At the same time, there were great differences between the sample size of all studies, in other words, it could cause heterogeneity. Moreover, all included papers were from developing countries and concentrated in Asia. Therefore, it existed selection bias of the study base. Besides, this systematic review only included English papers, which insinuates some potential studies in other languages would be left out.
References
[1]. GBD 2021 Neck Pain Collaborators. (2024). Global, regional, and national burden of neck pain, 1990-2020, and projections to 2050: A systematic analysis of the Global Burden of Disease Study 2021. The Lancet Rheumatology, 6(3), e142–e155. https://doi.org/10.1016/S2665-9913(23)00321-1
[2]. Thacker, D., Jameson, J., Baker, J., Divine, J., & Unfried, A. (2011). Management of upper cross syndrome through the use of active release technique and prescribed exercises. Logan College of Chiropractic.
[3]. Chang, M. C., Choo, Y. J., Hong, K., Boudier-Revéret, M., & Yang, S. (2023). Treatment of upper crossed syndrome: A narrative systematic review. Healthcare, 11(16), 2328. https://doi.org/10.3390/healthcare11162328
[4]. Gillani, S. N., Ain, Q., Rehman, S. U., & Masood, T. (2020). Effects of eccentric muscle energy technique versus static stretching exercises in the management of cervical dysfunction in upper cross syndrome: A randomized control trial. JPMA. The Journal of the Pakistan Medical Association, 70(3), 394–398. https://doi.org/10.5455/JPMA.300417
[5]. Page, M. J., McKenzie, J. E., Bossuyt, P. M., & Boutron. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ (Clinical Research Edition), 372, n71. https://doi.org/10.1136/bmj.n71
[6]. Joanna Briggs Institute. (2017). The Joanna Briggs Institute Critical Appraisal tools for use in JBI Systematic Reviews. https://joannabriggs.org/research/critical-appraisal-tools
[7]. The jamovi project. (2022). jamovi (Version 2.3) [Computer software]. https://www.jamovi
[8]. R Core Team. (2021). R: A language and environment for statistical computing (Version 4.1) [Computer software]. Retrieved from https://cran.r-project.org (R packages retrieved from MRAN snapshot 2022-01-01).
[9]. Viechtbauer, W. (2010). Conducting meta-analyses in R with the metafor package. Journal of Statistical Software, 36(1), 1-48. https://doi.org/10.18637/jss.v036.i03
[10]. Fatima, A., Ashraf, H. S., & Sohail, M. (2020). Prevalence of upper cross syndrome and associated postural deviations in computer operators: A qualitative study. Asian Journal of Allied Health Sciences, 7(3), 1-5. https://doi.org/10.52229/ajahs.v7i3.1645
[11]. Naseer, R., & Tauqeer, S. (2021). Prevalence of upper cross syndrome in different occupations. Pakistan Journal of Physical Therapy, 1-10. https://journals.uol.edu.pk/PJPT/article/view/980/708
[12]. Hussain, G., Nawaz, A., & Haroon, M. (2023). Prevalence of upper cross syndrome in working female physiotherapists: A cross-sectional survey. Bioscience Research Journal, 2023(1), 1-8. https://doi.org/10.54112/bcsrj.v2023i1.402
[13]. Mubashir, M. (2021). A cross-sectional survey on prevalence of upper cross syndrome and its correlation to WRMSDs in working physiotherapists. Pakistan Journal of Rehabilitation, 1-6. https://ojs.zu.edu.pk/pjr/article/view/920
[14]. Javed, A., Fatima, U., & Jadoon, I. J. (2022). Prevalence of upper cross syndrome in medical students of Women Medical College, Abbottabad, Khyber Pakhtunkhwa, Pakistan. Journal of Women Medical & Dental College, 1(1), 1-10. https://www.jwmdc.com/index.php/jwmdc/article/view/42/26
[15]. Zhang, C., Zhang, J., & Yang, G. (2023). Association between internet addiction and the risk of upper cross syndrome in Chinese college students: A cross-sectional study. Medicine, 102(30), e34273. https://doi.org/10.1097/MD.0000000000034273
[16]. Mujawar, J. C., & Sagar, J. H. (2019). Prevalence of upper cross syndrome in laundry workers. Indian Journal of Occupational and Environmental Medicine, 23(1), 54–56. https://doi.org/10.4103/ijoem.IJOEM_169_18
[17]. Lv, Y., Tian, W., Chen, D., Liu, Y., Wang, L., & Duan, F. (2018). The prevalence and associated factors of symptomatic cervical spondylosis in Chinese adults: A community-based cross-sectional study. BMC Musculoskeletal Disorders, 19(1), 325. https://doi.org/10.1186/s12891-018-2234-0
[18]. Chang, M. C., Choo, Y. J., Hong, K., Boudier-Revéret, M., & Yang, S. (2023). Treatment of upper crossed syndrome: A narrative systematic review. Healthcare, 11(16), 2328. https://doi.org/10.3390/healthcare11162328
[19]. Taqui, A. M., Shaikh, M., Gowani, S. A., et al. (2008). Body dysmorphic disorder: Gender differences and prevalence in a Pakistani medical student population. BMC Psychiatry, 8, 20. https://doi.org/10.1186/1471-244X-8-20
[20]. Haizlip, K. M., Harrison, B. C., & Leinwand, L. A. (2015). Sex-based differences in skeletal muscle kinetics and fiber-type composition. Physiology, 30(1), 30–39. https://doi.org/10.1152/physiol.00024.2014
[21]. Purushothaman, Y., & Yoganandan, N. (2022). Gender differences in cervical spine motions and loads with head supported mass using finite element models. Journal of Engineering and Science in Medical Diagnostics and Therapy, 5(4), 041004. https://doi.org/10.1115/1.4054856
[22]. Yoganandan, N., Bass, C. R., Voo, L., & Pintar, F. A. (2017). Male and female cervical spine biomechanics and anatomy: Implication for scaling injury criteria. Journal of Biomechanical Engineering, 139(5), 10.1115/1.4036313. https://doi.org/10.1115/1.4036313
[23]. de-la-Iglesia, L., Bravo, C., & Rubí-Carnacea, F. (2023). Upper crossed syndrome in secondary school students: A mixed-method study. Journal of Taibah University Medical Sciences, 18(4), 894–907. https://doi.org/10.1016/j.jtumed.2023.01.008
Cite this article
Xu,J. (2024). Prevalence of upper crossed syndrome: a systematic review and meta-analysis. Journal of Clinical Technology and Theory,1,28-34.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Journal:Journal of Clinical Technology and Theory
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. GBD 2021 Neck Pain Collaborators. (2024). Global, regional, and national burden of neck pain, 1990-2020, and projections to 2050: A systematic analysis of the Global Burden of Disease Study 2021. The Lancet Rheumatology, 6(3), e142–e155. https://doi.org/10.1016/S2665-9913(23)00321-1
[2]. Thacker, D., Jameson, J., Baker, J., Divine, J., & Unfried, A. (2011). Management of upper cross syndrome through the use of active release technique and prescribed exercises. Logan College of Chiropractic.
[3]. Chang, M. C., Choo, Y. J., Hong, K., Boudier-Revéret, M., & Yang, S. (2023). Treatment of upper crossed syndrome: A narrative systematic review. Healthcare, 11(16), 2328. https://doi.org/10.3390/healthcare11162328
[4]. Gillani, S. N., Ain, Q., Rehman, S. U., & Masood, T. (2020). Effects of eccentric muscle energy technique versus static stretching exercises in the management of cervical dysfunction in upper cross syndrome: A randomized control trial. JPMA. The Journal of the Pakistan Medical Association, 70(3), 394–398. https://doi.org/10.5455/JPMA.300417
[5]. Page, M. J., McKenzie, J. E., Bossuyt, P. M., & Boutron. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ (Clinical Research Edition), 372, n71. https://doi.org/10.1136/bmj.n71
[6]. Joanna Briggs Institute. (2017). The Joanna Briggs Institute Critical Appraisal tools for use in JBI Systematic Reviews. https://joannabriggs.org/research/critical-appraisal-tools
[7]. The jamovi project. (2022). jamovi (Version 2.3) [Computer software]. https://www.jamovi
[8]. R Core Team. (2021). R: A language and environment for statistical computing (Version 4.1) [Computer software]. Retrieved from https://cran.r-project.org (R packages retrieved from MRAN snapshot 2022-01-01).
[9]. Viechtbauer, W. (2010). Conducting meta-analyses in R with the metafor package. Journal of Statistical Software, 36(1), 1-48. https://doi.org/10.18637/jss.v036.i03
[10]. Fatima, A., Ashraf, H. S., & Sohail, M. (2020). Prevalence of upper cross syndrome and associated postural deviations in computer operators: A qualitative study. Asian Journal of Allied Health Sciences, 7(3), 1-5. https://doi.org/10.52229/ajahs.v7i3.1645
[11]. Naseer, R., & Tauqeer, S. (2021). Prevalence of upper cross syndrome in different occupations. Pakistan Journal of Physical Therapy, 1-10. https://journals.uol.edu.pk/PJPT/article/view/980/708
[12]. Hussain, G., Nawaz, A., & Haroon, M. (2023). Prevalence of upper cross syndrome in working female physiotherapists: A cross-sectional survey. Bioscience Research Journal, 2023(1), 1-8. https://doi.org/10.54112/bcsrj.v2023i1.402
[13]. Mubashir, M. (2021). A cross-sectional survey on prevalence of upper cross syndrome and its correlation to WRMSDs in working physiotherapists. Pakistan Journal of Rehabilitation, 1-6. https://ojs.zu.edu.pk/pjr/article/view/920
[14]. Javed, A., Fatima, U., & Jadoon, I. J. (2022). Prevalence of upper cross syndrome in medical students of Women Medical College, Abbottabad, Khyber Pakhtunkhwa, Pakistan. Journal of Women Medical & Dental College, 1(1), 1-10. https://www.jwmdc.com/index.php/jwmdc/article/view/42/26
[15]. Zhang, C., Zhang, J., & Yang, G. (2023). Association between internet addiction and the risk of upper cross syndrome in Chinese college students: A cross-sectional study. Medicine, 102(30), e34273. https://doi.org/10.1097/MD.0000000000034273
[16]. Mujawar, J. C., & Sagar, J. H. (2019). Prevalence of upper cross syndrome in laundry workers. Indian Journal of Occupational and Environmental Medicine, 23(1), 54–56. https://doi.org/10.4103/ijoem.IJOEM_169_18
[17]. Lv, Y., Tian, W., Chen, D., Liu, Y., Wang, L., & Duan, F. (2018). The prevalence and associated factors of symptomatic cervical spondylosis in Chinese adults: A community-based cross-sectional study. BMC Musculoskeletal Disorders, 19(1), 325. https://doi.org/10.1186/s12891-018-2234-0
[18]. Chang, M. C., Choo, Y. J., Hong, K., Boudier-Revéret, M., & Yang, S. (2023). Treatment of upper crossed syndrome: A narrative systematic review. Healthcare, 11(16), 2328. https://doi.org/10.3390/healthcare11162328
[19]. Taqui, A. M., Shaikh, M., Gowani, S. A., et al. (2008). Body dysmorphic disorder: Gender differences and prevalence in a Pakistani medical student population. BMC Psychiatry, 8, 20. https://doi.org/10.1186/1471-244X-8-20
[20]. Haizlip, K. M., Harrison, B. C., & Leinwand, L. A. (2015). Sex-based differences in skeletal muscle kinetics and fiber-type composition. Physiology, 30(1), 30–39. https://doi.org/10.1152/physiol.00024.2014
[21]. Purushothaman, Y., & Yoganandan, N. (2022). Gender differences in cervical spine motions and loads with head supported mass using finite element models. Journal of Engineering and Science in Medical Diagnostics and Therapy, 5(4), 041004. https://doi.org/10.1115/1.4054856
[22]. Yoganandan, N., Bass, C. R., Voo, L., & Pintar, F. A. (2017). Male and female cervical spine biomechanics and anatomy: Implication for scaling injury criteria. Journal of Biomechanical Engineering, 139(5), 10.1115/1.4036313. https://doi.org/10.1115/1.4036313
[23]. de-la-Iglesia, L., Bravo, C., & Rubí-Carnacea, F. (2023). Upper crossed syndrome in secondary school students: A mixed-method study. Journal of Taibah University Medical Sciences, 18(4), 894–907. https://doi.org/10.1016/j.jtumed.2023.01.008