1 Introduction
Citizen science engages volunteers in data collection and processing across a broad spectrum of scientific disciplines, including ecology, environmental science, social sciences, and epidemiology. Emerging from the nascent stages of modern science, citizen science has undergone substantial growth and diversification in recent decades. Particularly within ecology and environmental science, it has produced vast quantities of high-quality data, meticulously gathered and classified by volunteers, thereby advancing scientific research and empowering communities to influence policy and decision-making processes [1,2].
Originating in high-income countries, citizen science within ecology and environmental science has served as a foundational model for other disciplines. As its applications have matured, citizen science has expanded into additional domains, facilitating the broader dissemination of scientific knowledge and enhancing community influence in decision-making processes [3,4]. Concurrently, advancements in research methodologies and data validation have further entrenched citizen science’s role in contemporary scientific inquiry [5]. By leveraging citizen science, researchers can access otherwise inaccessible data, foster community engagement, and catalyze changes in policy and practice [6].
In recent years, citizen science has exhibited considerable potential in enhancing public health, optimizing disease prevention, and advancing health surveillance, which has facilitated its substantial expansion into the healthcare domain. Citizen science plays a pivotal role in monitoring vector-borne diseases. For example, a project in Maine, USA, focused on tick distribution and pathogen infection, significantly enhancing data quality and coverage [7]. In Italy, a citizen science initiative monitoring Trichinella infections in wild boar meat strengthened zoonosis control and prevention [8]. During the COVID-19 pandemic, citizen science facilitated the online community’s understanding of COVID-19’s impact on daily life, enabling researchers to comprehensively assess the disease’s complex effects [9].
The role of citizen science in chronic disease prevention is increasingly recognized; these initiatives are instrumental in formulating and evaluating interventions through community engagement and data collection [10]. Additionally, citizen science projects in chronic disease management contribute to enhanced healthcare and patient quality of life by gathering feedback and insights from patients [11]. Moreover, citizen science can bolster vaccine uptake and the implementation of public health policies by identifying factors contributing to vaccine hesitancy and by fostering public trust in science, thereby significantly increasing vaccination rates [12]. In broader efforts to achieve health and well-being goals, citizen science has proven to be a highly effective approach. By systematically collecting and monitoring data, it addresses gaps in traditional data sources and supports the achievement of global health objectives [13]. This methodology not only bridges data gaps but also mobilizes public participation at local, national, and global levels, thereby fostering policy development and action [6]. Furthermore, citizen science has demonstrated adaptability across various cultural and social contexts; for instance, in Nigeria, older participants improved their physical activity by assessing their local environment [14].
As citizen science continues to evolve within the healthcare sector, its scope and impact are anticipated to expand, providing critical support for public health and healthcare policy development. Nevertheless, despite growing international interest, academic research on citizen science remains limited in low- and middle-income countries (LMICs). In these regions, citizen science is still nascent, primarily concentrated in traditional fields such as environmental science, ecology, and biodiversity conservation.
This study aims to conduct a comprehensive bibliometric analysis of citizen science practices in healthcare globally using CiteSpace. Through an in-depth examination of key literature, it reviews the current landscape of citizen science in healthcare, identifies major research hotspots and collaboration networks, and explores specific applications and objectives. Furthermore, the study provides insights into how these practices can be tailored to enhance healthcare development in low- and middle-income countries.
2 Methodology
In this study, CiteSpace 6.3.R3 (Advanced) was employed to conduct a comprehensive bibliometric analysis. CiteSpace is a robust scientometric tool used to visualize and analyze data, revealing the structure, patterns, and dynamics of scientific knowledge across disciplines. It is widely recognized for generating knowledge maps in bibliometric studies [15]. CiteSpace facilitates the extraction of valuable insights from extensive literature, uncovering the frontier dynamics of disciplinary development and the evolution of academic research [16]. The tool effectively detects and visualizes emerging trends and transient patterns in academic literature [17]. Furthermore, its multi-perspective analysis provides multidimensional insights into the identification and labeling of research clusters [18].
To ensure the accuracy, comprehensiveness, and representativeness of the data, the Web of Science Core Collection database (1985-present) was selected as the primary data source for this study. This study specifically utilized the Science Citation Index Expanded (SCI-EXPANDED) and the Social Sciences Citation Index (SSCI) as primary sources of data from various subsets of the Web of Science database.
In addition, this study used Boolean operators for advanced search to accurately filter literature related to citizen science in the healthcare sector. This strategy was chosen to maximize the relevance and accuracy of the search results and minimize the confusion of redundant information. The search topic was ‘citizen science’ or ‘citizen science data,’ and 28 Web of Science categories related to healthcare were included. Document types were restricted to ‘articles,’ and the study period focused on the last decade (2014-2024) to ensure the currency of analysis and timeliness of research.
Applying these stringent search and screening criteria initially yielded 364 documents (search conducted on August 1, 2024). To further ensure the quality and relevance of the data, the study manually reviewed these documents and excluded those that did not align with the research theme or did not meet quality criteria. Ultimately, 248 high-quality documents were selected for the bibliometric analysis in this study.
3 Result
3.1 Overview of the general research landscape
An initial analysis of 248 articles from the Web of Science Core Collection reveals key patterns in the distribution of research across different years, countries, and disciplines.
The trend in annual publication volume shows that 2021 accounted for 18.145% of the dataset, marking the peak year, likely due to the global COVID-19 pandemic, which spurred research demand. In the following years, publication shares fluctuated, with a slight decrease in 2022 to 12.097%, followed by an increase in 2023 to 16.532%. Despite these fluctuations, the citation counts continued to rise significantly, reflecting the ongoing relevance and impact of citizen science in healthcare.
The distribution of research across countries shows that the United States leads with 39.113% of the total, reflecting its robust implementation of citizen science projects supported by strong policies and research funding. The United Kingdom follows with 16.532%, benefiting from proactive policies that promote community engagement. The Netherlands and Germany also contribute significantly, accounting for 12.5% and 10.887%, respectively, highlighting the strong participation of European countries. Australia and Canada add 8.468% and 8.065%, respectively.
In terms of journal distribution, BMC Public Health leads with 5.645% of the total, followed closely by Frontiers in Public Health with 5.242%. These journals emphasize the significant role of citizen science in public health, particularly in enhancing outcomes and informing policy decisions. While prominent journals such as The Lancet Public Health and the American Journal of Public Health also contribute significantly, the distribution of articles across 120 different publications highlights the interdisciplinary nature of citizen science, reflecting its diverse applications in environmental science, social policy, and disease surveillance.
The literature is primarily concentrated in public and environmental health, with 45.968% classified under Public, Environmental, and Occupational Health. This emphasizes citizen science as a mainstream tool in disease surveillance and pollution control. Other key disciplines, including Health Care Sciences (13.71%), Infectious Diseases (10.887%), Health Policy Services (10.484%), Tropical Medicine (10.081%), and Parasitology (9.274%), further illustrate the broad applicability of citizen science. These findings underscore its significant role in monitoring infectious diseases, advancing tropical medicine research, and improving healthcare services, which are crucial for global health goals.
3.2 Research hotspots analysis
This study conducted a comprehensive analysis of literature from January 2014 to August 2024 using CiteSpace to identify research hotspots and trends. The time span was set from 2014 to 2024, with each time slice representing one year, capturing annual shifts in research focus. Titles, abstracts, authors, keywords (DE), and keyword plus (ID) terms were included as vocabulary sources to ensure thorough coverage of research topics. The g-index with a k-value of 50 was selected for node selection due to its effectiveness in highlighting high-impact research nodes by assigning greater weight to highly cited articles. This approach is particularly useful in interdisciplinary fields like the intersection of citizen science and healthcare, where citation distribution is often uneven. The g-index method, therefore, ensures that impactful research, even with fewer publications, is adequately represented, providing a reliable basis for identifying research hotspots [19]. Keywords for each time period were refined and subjected to cluster analysis, with the 10 largest clusters retained to capture the most representative research themes. This step focused on the most significant research hotspots, enhancing the accuracy of the analysis by eliminating noise. Finally, the Cluster View-Static and Show Merged Network functions were utilized for visualization, offering a clearer depiction of the network structure and clustering, and making the analysis of research hotspots and trends more precise.
Cluster analysis identified 10 main clusters, reflecting the academic community’s concentrated focus on specific research directions during this period (Figure 1). These clusters not only represent independent research priorities but also reveal the complex interrelationships among them, demonstrating the extensive interdisciplinary collaboration that characterizes modern healthcare research. Among these, Cluster #0 (West Nile virus) occupies a central position, serving both as a distinct research focus and a crucial link to other topics. Research in this cluster covers infection prevention, transmission pathways, and climate change impacts on disease spread, highlighting its central role in shaping related research areas.
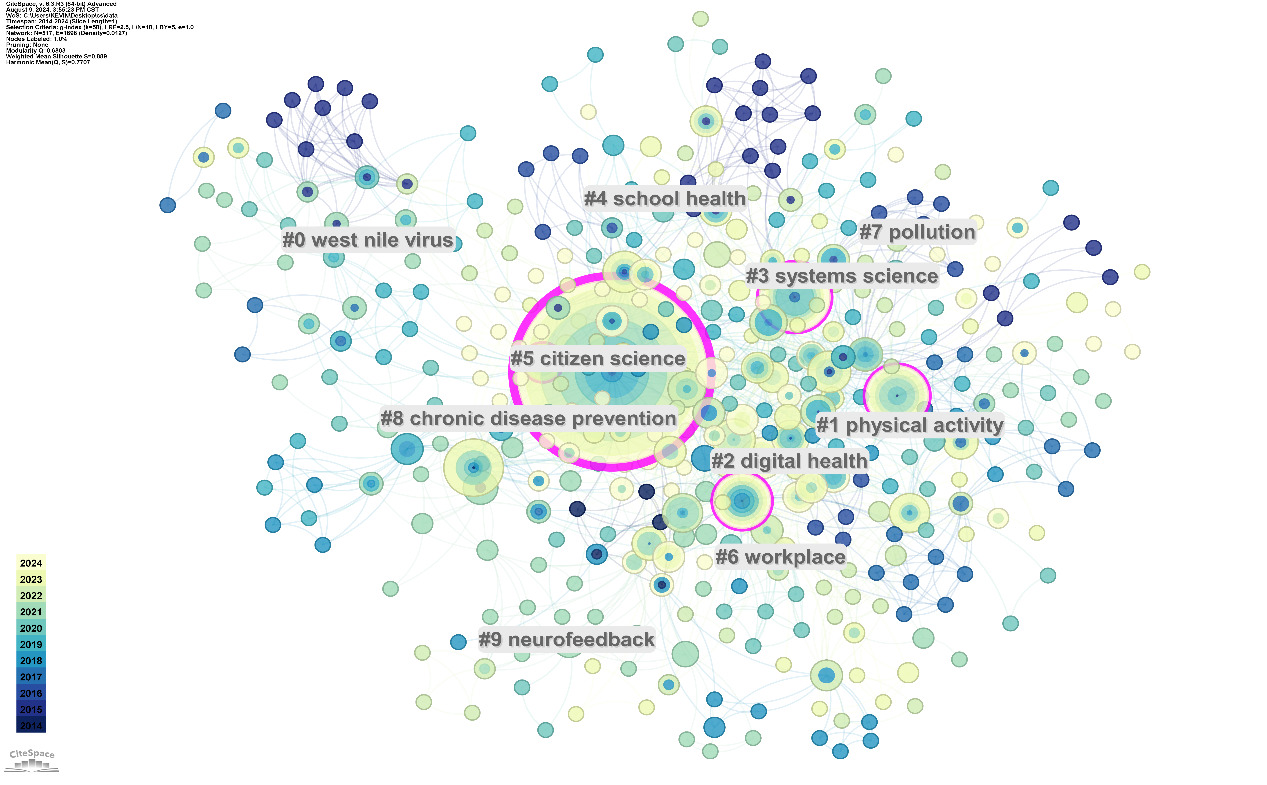
Figure 1. Keyword Clusters from 2014 to 2024
This interdisciplinary nature is further exemplified by the connection between Cluster #3 (systems science) and Cluster #5 (citizen science). These clusters highlight the role of systems science in addressing complex public health challenges and the innovative contributions of citizen science through public data participation. Cluster #1 (physical activity) and Cluster #2 (digital health) highlight two major directions in contemporary health research. Physical activity research, particularly within public health, continues to be a focal point due to its critical role in addressing obesity and cardiovascular disease prevention. The rapid expansion of digital health research, marked by Cluster #2, reflects its rising importance in areas such as wearable devices, telemedicine, and health data analytics, driven by technological advancements. Additionally, Cluster #4 (school health) and Cluster #6 (workplace) illustrate the application of health research in specific populations—school health focusing on children and adolescents, and workplace health targeting employee well-being and productivity.
Further analysis of literature data from 2014 to 2024 using CiteSpace identified keywords with significant citation bursts during this period (Figure 2). These bursts highlight topics that gained substantial attention, often due to emerging trends or significant breakthroughs. For instance, the keyword ‘health’ exhibited the highest burst strength in 2015, with a peak in 2020, likely linked to the global impact of the COVID-19 pandemic. Similarly, ‘public health’ showed strong burst behavior starting in 2023, a trend expected to continue into 2024, reflecting sustained interest in this area. Other notable keywords, such as ‘knowledge,’ ‘Borrelia burgdorferi,’ and ‘older adults,’ also demonstrated significant bursts, indicating growing research interest in knowledge dissemination, Lyme disease, and global aging. Keywords like ‘framework’ and ‘safety’ have also shown bursts in recent years, peaking in 2023 and 2020, respectively, suggesting a heightened focus on building safe health systems and enhancing health policy effectiveness. Figure 2 illustrates these trends by highlighting specific time points, thus reflecting the academic and social context of these research topics. The analysis of citation bursts reveals emerging trends and highlights new research hotspots, deepening the understanding of dynamic shifts in healthcare research.
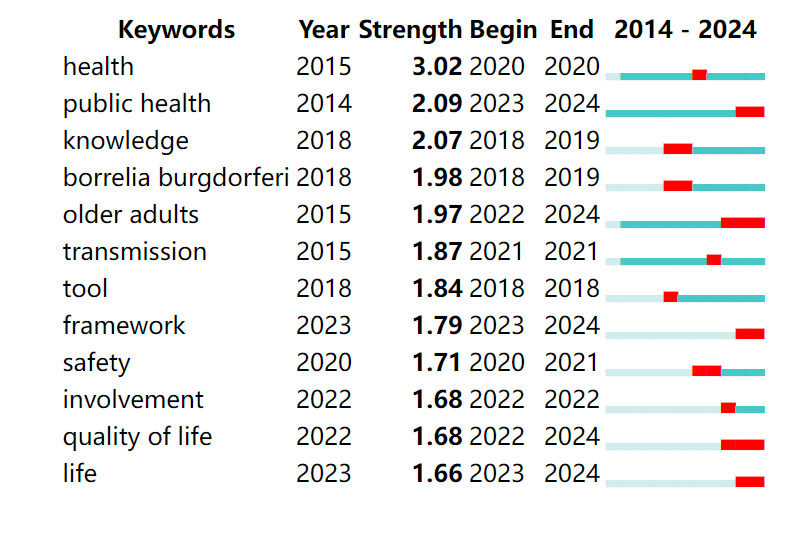
Figure 2. Top 12 Keywords with Strongest Citation Bursts from 2014 to 2024
3.3 Research network analysis
The ‘Co-Authors’ node type was utilized in this study for collaboration network analysis, with the Minimum Spanning Tree (MST) model employed to optimize the network structure. A k-value of 100 was chosen to effectively capture the complexity of co-author relationships, as it allows for the inclusion of more intricate connections while maintaining network clarity. Consistent with the research hotspot analysis, this methodology included identical time span settings, data source selection, and analytical tools. The MST model was selected for its capacity to simplify complex collaboration networks by retaining only the most direct and essential connections, thereby reducing redundancy and enhancing the visibility of core nodes and major collaborative relationships. This approach is particularly effective in highlighting researchers with significant influence in citizen science and healthcare. By filtering out redundant connections, the MST model is well-suited for identifying critical structures within large-scale collaboration networks [20].
Figure 3 reveals that Abby C. King holds a central position in the collaboration network of key researchers from 2014 to 2024. Since her first publication in 2015, King has authored 22 papers, demonstrating a high level of academic collaboration. In CiteSpace, the degree value indicates the number of direct connections a researcher (node) has with others, representing the extent of collaborative relationships. King’s degree value of 21 underscores her extensive collaborative ties, positioning her as a pivotal node in the network. Although her centrality value is relatively low at 0.02—suggesting that her collaborations are concentrated within specific circles—this high degree value highlights her critical role in maintaining the network’s stability and cohesion by fostering strong connections within her collaborative group. Figure 3 also shows that King’s collaboration network has led to the formation of multiple sub-clusters. These sub-clusters are interconnected through key nodes, creating a larger and more cohesive academic network. Researchers such as Olga L. Sarmiento and Sandra J. Winter have played pivotal roles in linking these subsets, thereby strengthening the overall structure of the network.
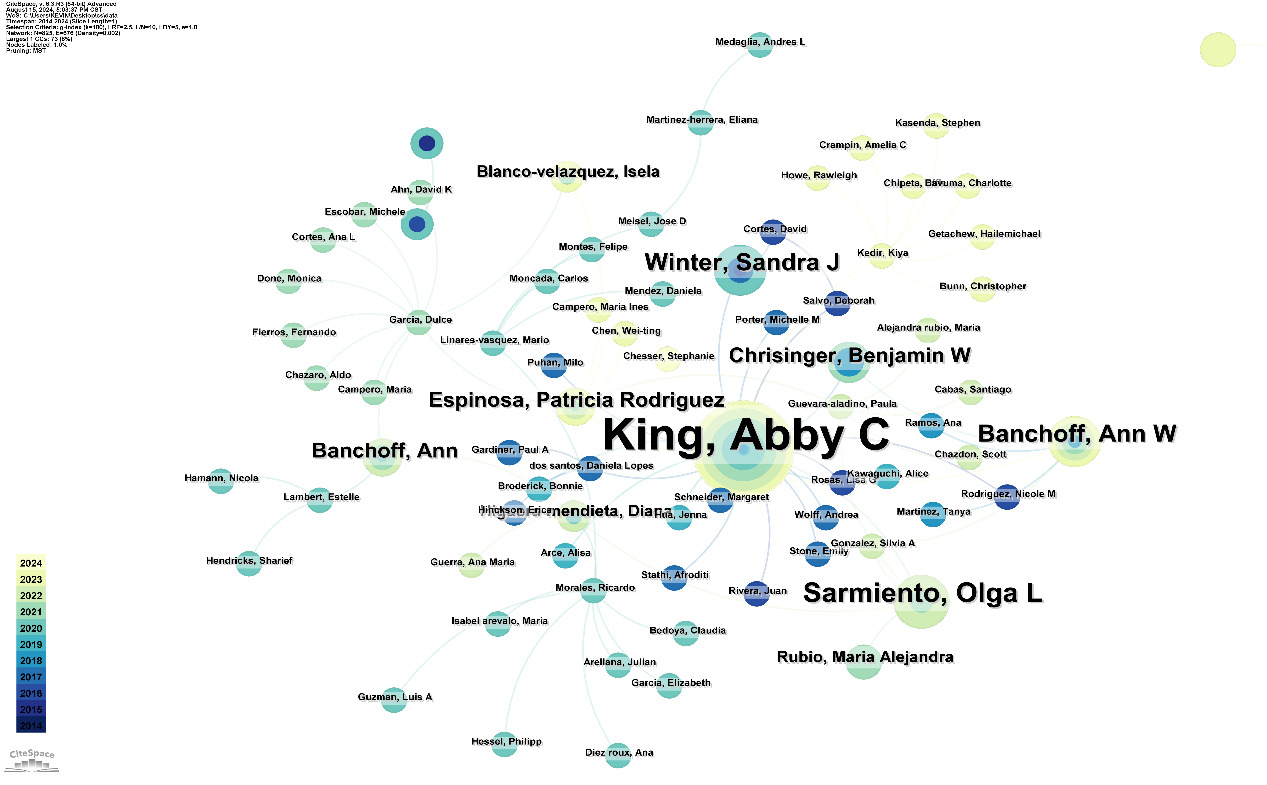
Figure 3. Collaboration Network of Key Researchers from 2014 to 2024
For the collaboration network analysis among research institutions, ‘institutions’ were selected as the node type, with consistent time span and parameter settings to ensure comparability. Unlike the co-author analysis, the MST model was not applied, preserving all connections within the network. This approach provided a comprehensive view of the collaborative relationships among research institutions.
Figure 4 shows that Stanford University and the University of California System hold central positions in the network, emerging as global leaders after 2018 through extensive international collaborations. The color transition in Stanford’s node from dark blue to light green indicates a significant rise in collaboration activity post-2018, particularly in health, medicine, and citizen science projects. Collaborations between Stanford and institutions like the University of Zurich and the University of Oxford have led to successful cross-national research projects, especially those integrating citizen science with health data.
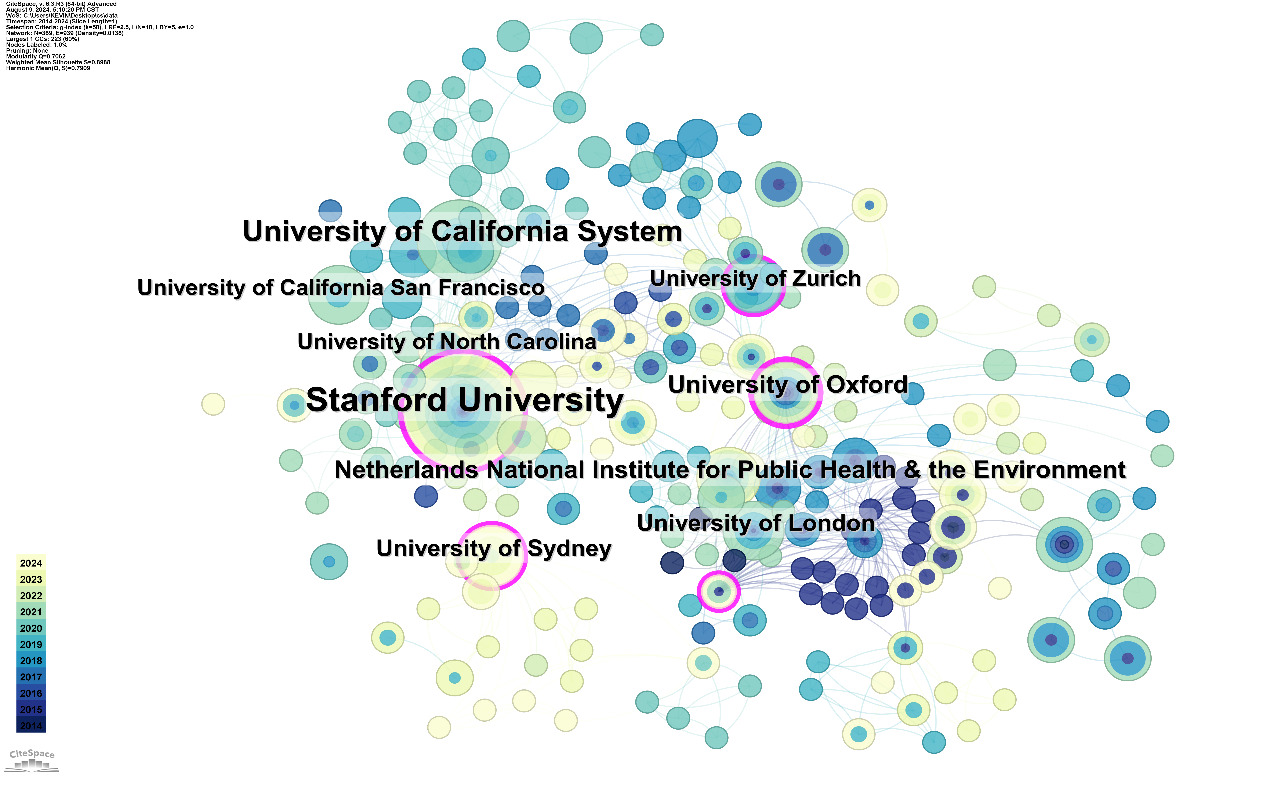
Figure 4. Collaboration Network of Research Institutions from 2014 to 2024
The analysis highlights the significant roles of the University of California, San Francisco, and the University of North Carolina, especially in public health and clinical research. These institutions collaborate closely with leading research centers globally, driving key developments in areas like disease surveillance, vaccine development, and health data analysis. Despite their prominence, the network also reveals smaller or less collaborative institutions, represented by smaller nodes with thinner connections and darker colors. Though currently less influential, these institutions have made significant contributions in specific areas. Participation in targeted projects or collaborations could enhance their research capacity and international influence, gradually strengthening their positions in future collaborations.
3.4 CO-Citation analysis
This study conducted a detailed co-citation analysis using ‘Cited References’ as the node type. Consistent time spans and segmentation methods were applied to ensure the comparability and completeness of the results. This consistency forms a solid foundation for in-depth research. The co-citation network map generated by CiteSpace (Figure 5) reveals relationships and evolution among research topics, highlighting academic dynamics and emerging trends within relevant fields.
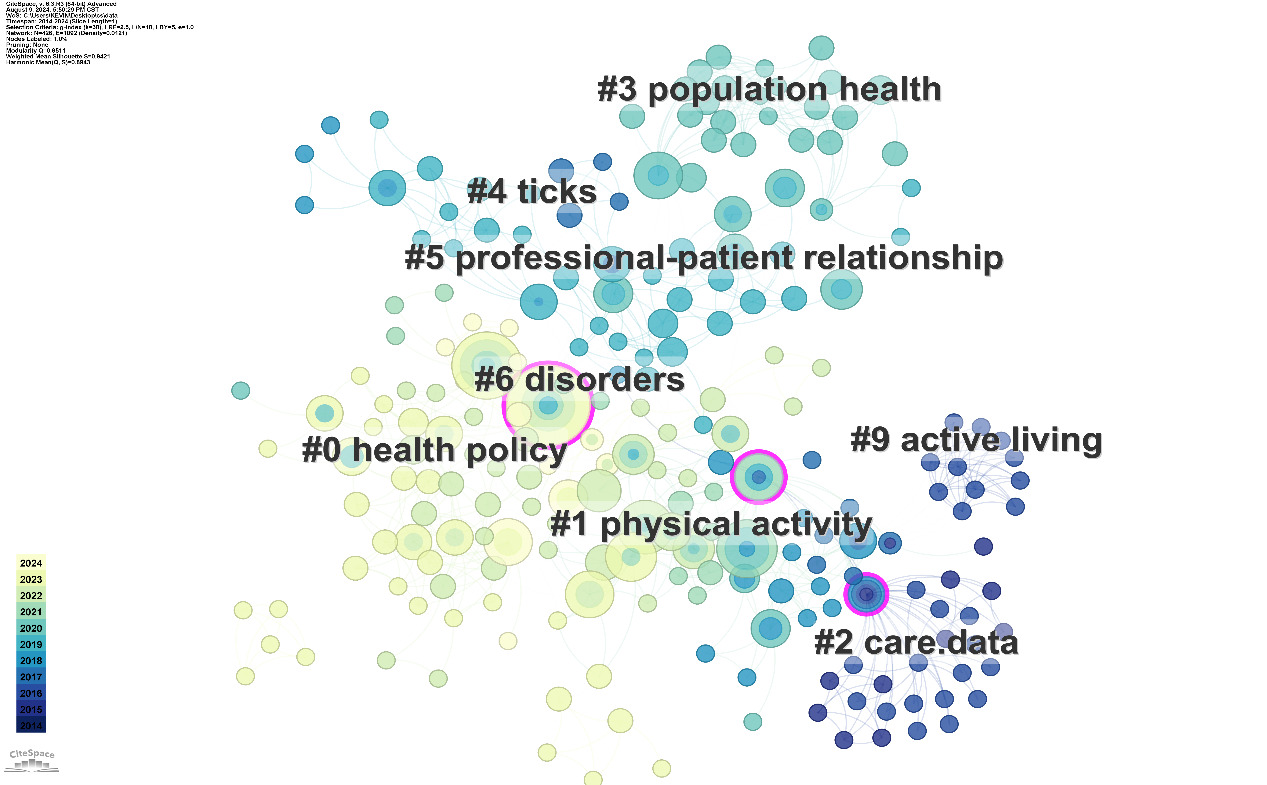
Figure 5. Co-Citation Clusters from 2014 to 2024
Among the various clusters identified, ‘Health Policy’ (#0) is the largest cluster by node quantity, reflecting widespread research interest in policy-level issues. This cluster spans a broad range of topics, from global health initiatives to local policy implementations, emphasizing its global impact. As the role of health policy in shaping public health outcomes has become increasingly evident, research focus on this area has intensified, particularly in response to global challenges like the COVID-19 pandemic. Policy interventions have significantly influenced public health decisions, as highlighted during the COVID-19 pandemic, where policy responses were critical in managing the crisis.
Closely related to health policy is the ‘Physical Activity’ (#1) cluster, which reflects sustained focus within public health and preventive medicine, particularly in chronic disease prevention and health promotion. This research area is closely linked to lifestyle-related diseases such as obesity and cardiovascular conditions. Studies on these diseases provide strong support for public health policy formulation and health behavior interventions. The dense node representation in Figure 5 illustrates the significant breadth and impact of research in this area.
Another critical area of research, ‘Population Health’ (#3), reflects ongoing interest in population-level health issues, including epidemiology, health inequalities, and targeted interventions. These studies generate crucial data for comprehensive public health policy development and highlight global health challenges requiring urgent attention. Epidemiological studies, for example, reveal health inequalities in vulnerable populations, underscoring the need for timely policy interventions to address these disparities.
‘Professional-Patient Relationship’ (#5) adds another dimension to these public health concerns by focusing on interactions in healthcare, particularly concerning care quality, patient satisfaction, and communication strategies between professionals and patients. As healthcare becomes more complex, effective professional-patient relationships have become central to improving care quality. The literature in this cluster is interdisciplinary, spanning sociology, psychology, and medical ethics, highlighting the research area’s diversity and complexity. Emerging methods in patient engagement and communication are improving both patient outcomes and overall care quality.
4 Discussion
4.1 Current status and challenges of citizen science in LMICs
Citizen science research in low- and middle-income countries (LMICs) remains in its early stages, with limited scope and depth compared to the more established frameworks in high-income countries. Although recent years have seen some growth, particularly in nations like India, Brazil, and South Africa, the overall output is inconsistent, fluctuating significantly from year to year. This variability reflects the sporadic and uneven attention given to citizen science across these regions. Research efforts in LMICs are predominantly concentrated in traditional fields such as environmental science (26.2%), ecology (18.6%), biodiversity conservation (11.8%), and marine biology (10.1%), with minimal exploration in critical sectors such as healthcare and social sciences. For instance, in South Africa, citizen science projects such as the Southern African Bird Atlas Project have shown significant potential in species conservation. Through extensive public participation and long-term monitoring of natural resources, these projects provide essential data for species conservation and raise public awareness of environmental protection [21,22]. Additionally, the successful application of the miniSASS method in water quality monitoring serves as a model for how citizen science can contribute to achieving Sustainable Development Goal 6. This method leverages public participation in the biological monitoring of water bodies, offering an effective tool for improving water quality and fostering public engagement in water resource management [23]. South Africa’s marine citizen science projects have also made notable contributions to global marine biodiversity research, particularly in species classification and public awareness of marine environmental protection [24]. However, despite these successes in environmental science, similar efforts in public health remain notably absent, highlighting significant gaps in applying citizen science to address broader societal issues. In Sri Lanka, research demonstrates the potential of citizen science in reducing flood risks by integrating local residents’ perceptions with modern scientific data. For example, in the Kalu River Basin, combining local knowledge with scientific analysis significantly enhanced flood management effectiveness [25]. This integration not only showcases the value of citizen science in natural disaster management but also underscores the importance of incorporating local knowledge into modern scientific practices. Moreover, digital platforms like iNaturalist, widely used in biodiversity research, have further amplified the impact of citizen science by enabling vast amounts of biodiversity data collection and sharing [26]. The integration of satellite remote sensing with citizen science has proven effective in environmental monitoring, though its application remains limited to these traditional domains [27]. Overall, these examples illustrate the potential of citizen science in LMICs while also revealing significant gaps in its application to healthcare and social sciences.
Despite the significant progress and potential of citizen science in environmental and ecological fields within LMICs, its application in critical sectors like healthcare remains limited. This limitation hampers the broader development of citizen science and its capacity to contribute to public health and societal well-being. In contrast, high-income countries have successfully leveraged citizen science for healthcare advancements, with platforms like the UK’s ‘Zooniverse’ and the US’s ‘Flu Near You’ playing key roles in public health surveillance and research [28]. These platforms benefit from robust infrastructures and high levels of public engagement, allowing for large-scale data collection and real-time analysis, as seen in ‘Flu Near You,’ which gathered over 660,000 reports from more than 100,000 participants during the 2012-2013 and 2013-2014 flu seasons, enhancing data coverage beyond traditional systems like the CDC’s ILINet [29]. These successes highlight the potential for citizen science to make significant contributions in healthcare. However, replicating such success in LMICs requires addressing several substantial challenges, including inadequate technological infrastructure, socioeconomic and cultural barriers, and insufficient policy support.
First, technological infrastructure in LMICs is often insufficient, with low internet penetration and outdated equipment limiting public participation in digital citizen science platforms. For example, during the COVID-19 pandemic in Jordan, the shift to remote radiotherapy support was hindered by technological constraints, such as time zone differences and communication barriers [30]. Furthermore, the fragmented adoption of Industry 4.0 technologies in these regions, lacking a unified framework, exacerbates the challenge of optimizing healthcare systems [31]. Beyond technical challenges, socioeconomic and cultural factors also pose significant obstacles. Economic pressures often prevent individuals in LMICs from participating in citizen science activities. For instance, during the COVID-19 pandemic, 18.8% of households were unable to access necessary healthcare services due to financial constraints, directly reflecting the impact of financial conditions on participation in citizen science projects [32]. Socioeconomic inequalities further restrict participation, as seen in urban disparities between slum and non-slum residents regarding healthcare service utilization [33]. Moreover, while mobile technology has improved maternal and newborn healthcare, its adoption remains limited among low-income households due to disparities in mobile phone ownership [34]. The healthcare needs of older adults with multiple comorbidities are also frequently overlooked, complicating the promotion of citizen science in diverse social contexts [35].
Data quality and privacy concerns represent another critical challenge. The accuracy and reliability of data collected by non-professionals in citizen science projects are often questioned, particularly in LMICs where primary healthcare workers may lack the necessary knowledge for tasks such as genetic services, thereby affecting data integrity [36]. Furthermore, inadequate communication and privacy protection mechanisms in remote support projects can lead to risks of data leakage, undermining public trust and participation [30,37]. To address these challenges, implementing advanced data protection measures, such as encryption and privacy-enhancing technologies (PETs), is essential. Moreover, the advancement of citizen science in LMICs is constrained by insufficient policy support and institutional barriers. Effective citizen science initiatives require robust government and institutional backing, which is often lacking in these regions. This lack of support hinders the progress of innovative projects [38]. The COVID-19 pandemic highlighted these systemic barriers, as many primary healthcare systems in LMICs struggled with ineffective policy implementation, reducing the impact of citizen science in public health [39].
Finally, funding insufficiency and sustainability are major challenges. Many citizen science projects in LMICs rely on external funding during their early stages, but this funding is often unsustainable, severely impacting their long-term success [30]. Additionally, limited data availability, lack of trust, and insufficient evidence of cost-effectiveness in LMICs further undermine the sustainability of these initiatives [40]. Ensuring long-term funding stability and sustainable development is essential for the continued growth and impact of citizen science in LMICs.
4.2 Recommendations for advancing citizen science in LMICs
Advancing citizen science in healthcare within low- and middle-income countries (LMICs) requires a strategic approach that effectively utilizes existing resources and enhances community engagement. Leveraging mobile health applications, low-cost sensors, and other accessible technologies can improve public participation in scientific research, even under resource constraints. The FRESH AIR project, for instance, demonstrates how international collaboration can optimize the use of existing technologies to better manage chronic diseases in these settings [41]. By equipping community health workers (CHWs) with these technologies, they can more accurately collect and analyze data, helping to overcome socioeconomic and cultural barriers that often hinder widespread public involvement [42]. Integrating these technological tools into public health initiatives allows LMICs to expand the reach and impact of citizen science without relying heavily on new infrastructure investments.
The development of robust public health policies that integrate citizen-generated data is essential for improving the responsiveness of health systems, especially during crises. The Ebola outbreak highlighted the need for early detection and rapid response mechanisms, which can be strengthened by incorporating citizen science into national health surveillance frameworks [43]. Beyond data integration, these policies should also focus on building community capacity through initiatives like the Health Promoting Schools program. By equipping local leaders and CHWs with the necessary resources and training, these policies can enhance the sustainability and impact of citizen science projects, ensuring ongoing community engagement in health monitoring [44]. Additionally, the adoption of policies that incentivize the use of technology and encourage active community participation—such as through tax benefits or subsidies—can further support the success of these initiatives.
Ensuring the long-term sustainability and credibility of citizen science initiatives in LMICs requires diversified funding strategies and robust data privacy protections. A comprehensive financial framework that includes government backing, international partnerships, and private sector investment is critical to maintaining the stability and scalability of these initiatives [45]. Allocating funds towards the development and implementation of privacy-enhancing technologies (PETs) is crucial for managing and sharing data securely and ethically. Adopting data governance policies inspired by the European Union’s General Data Protection Regulation (GDPR) can help build and sustain public trust, which is essential for encouraging widespread participation in citizen science [46]. By strategically applying these resources, LMICs can foster a supportive environment for citizen science, ultimately leading to significant improvements in public health outcomes.
5 Conclusion
This study conducts a comprehensive bibliometric analysis using CiteSpace to critically review the landscape, objectives, and methodologies of citizen science in the global healthcare sector. By examining 248 high-impact articles from the Web of Science Core Collection, the research highlights the predominant role of citizen science in high-income countries, including the United States, the United Kingdom, Germany, and the Netherlands. These nations have established a strong foundation for citizen science through policy support, targeted public engagement, and innovations in public health, chronic disease management, and infectious disease surveillance.
The analysis shows that in high-income countries, citizen science initiatives are primarily aimed at enhancing public health outcomes, optimizing disease prevention, and improving health monitoring systems. The COVID-19 pandemic notably accelerated the adoption of citizen science, emphasizing its critical role in health surveillance and public health interventions. Research hotspots include infectious disease surveillance, digital health, and chronic disease management, with significant contributions to studies on West Nile Virus and Lyme disease. Furthermore, a robust collaboration network among leading researchers and institutions, such as Stanford University, has been identified, with interdisciplinary cooperation significantly advancing research depth and impact.
Citizen science in low- and middle-income countries (LMICs) remains underdeveloped in the healthcare sector, facing obstacles such as inadequate technological infrastructure, weak policy support, low public engagement, and resource limitations. While nations like India, Brazil, and South Africa have made progress, the overall impact in healthcare remains limited. This study proposes strategies including policy enhancement, improving public scientific literacy, optimizing healthcare resources, and fostering international collaborations. Adapting successful approaches from high-income countries to the LMIC context can expand the role of citizen science in healthcare, improving public health governance and outcomes.
Future research should focus on scaling the application of citizen science in LMICs’ healthcare sectors, with an emphasis on developing adaptable models that account for unique socio-cultural contexts. The integration of emerging technologies—such as AI, IoT, blockchain, and telemedicine—into health data management systems will be crucial. These systems should support personalized health management and precision medicine, and encourage broad citizen participation, thereby amplifying the global impact of citizen science.
Availability of data and material
All of the main data have been included in the results, Additional materials with details may be obtained from the corresponding author.
References
[1]. Silvertown, J. (2009). A new dawn for citizen science. Trends in Ecology & Evolution, 24(9), 467–471. https://doi.org/10.1016/j.tree.2009.03.017
[2]. Kullenberg, C., & Kasperowski, D. (2016). What is citizen science? – A scientometric meta-analysis. PLOS ONE, 11(1), e0147152. https://doi.org/10.1371/journal.pone.0147152
[3]. Bonney, R., Cooper, C. B., Dickinson, J., et al. (2009). Citizen science: A developing tool for expanding science knowledge and scientific literacy. BioScience, 59(11), 977–984. https://doi.org/10.1525/bio.2009.59.11.9
[4]. McKinley, D. C., Miller-Rushing, A. J., Ballard, H. L., et al. (2017). Citizen science can improve conservation science, natural resource management, and environmental protection. Biological Conservation, 208, 15–28. https://doi.org/10.1016/j.biocon.2016.05.015
[5]. Follett, R., & Strezov, V. (2015). An analysis of citizen science based research: Usage and publication patterns. PLOS ONE, 10(11), e0143687. https://doi.org/10.1371/journal.pone.0143687
[6]. Laird, Y., Marks, L., Smith, B. J., et al. (2023). Harnessing citizen science in health promotion: Perspectives of policy and practice stakeholders in Australia. Health Promotion International, 38(5). https://doi.org/10.1093/heapro/daac003
[7]. Ballman, E. S., Leahy, J. E., Sponarski, C. C., et al. (2023). A citizen science approach to investigate the distribution, abundance, and pathogen infection of vector ticks through active surveillance. Ticks and Tick-borne Diseases, 14(3), 102144. https://doi.org/10.1016/j.ttbdis.2022.102144
[8]. Sgroi, G., D’Alessio, N., Marucci, G., et al. (2023). Trichinella britovi in wild boar meat from Italy, 2015–2021: A citizen science approach to surveillance. One Health, 16, 100480. https://doi.org/10.1016/j.onehlt.2023.100480
[9]. Ireson, J., Taylor, A., Richardson, E., et al. (2022). Exploring invisibility and epistemic injustice in Long Covid—A citizen science qualitative analysis of patient stories from an online Covid community. Health Expectations, 25(4), 1753–1765. https://doi.org/10.1111/hex.13511
[10]. Marks, L., Laird, Y., Trevena, H., et al. (2022). A scoping review of citizen science approaches in chronic disease prevention. Frontiers in Public Health, 10. https://doi.org/10.3389/fpubh.2022.805759
[11]. Tran, V.-T., Riveros, C., Péan, C., et al. (2019). Patients’ perspective on how to improve the care of people with chronic conditions in France: A citizen science study within the ComPaRe e-cohort. BMJ Quality & Safety, 28(11), 875–886. https://doi.org/10.1136/bmjqs-2019-009048
[12]. Winter, T., Riordan, B. C., Scarf, D., et al. (2022). Conspiracy beliefs and distrust of science predict reluctance of vaccine uptake of politically right-wing citizens. Vaccine, 40(12), 1896–1903. https://doi.org/10.1016/j.vaccine.2022.02.027
[13]. Fraisl, D., See, L., Estevez, D., et al. (2023). Citizen science for monitoring the health and well-being related Sustainable Development Goals and the World Health Organization’s Triple Billion Targets. Frontiers in Public Health, 11. https://doi.org/10.3389/fpubh.2023.1131154
[14]. Odeyemi, E., Chesser, S., King, A. C., et al. (2023). Engaging Nigerian older persons in neighborhood environment assessment for physical activity participation: A citizen science project. Innovation in Aging, 8(4). https://doi.org/10.1093/geroni/igad002
[15]. Chen, Y., Chen, C., Liu, Z., et al. (2015). The methodological functions of CiteSpace knowledge mapping. Studies in Science of Science, 33(02), 242-253. https://doi.org/10.16192/j.cnki.1003-2053.2015.02.009
[16]. Chen, C. (2004). Searching for intellectual turning points: Progressive knowledge domain visualization. PNAS, 101(suppl_1), 5303-5310. https://doi.org/10.1073/pnas.0307513100
[17]. Chen, C. (2006). CiteSpace II: Detecting and visualizing emerging trends and transient patterns in scientific literature. Journal of the American Society for Information Science and Technology, 57(3), 359-377. https://doi.org/10.1002/asi.20317
[18]. Chen, C., Ibekwe-SanJuan, F., & Hou, J. (2010). The structure and dynamics of cocitation clusters: A multiple‐perspective cocitation analysis. Journal of the American Society for Information Science and Technology, 61(7), 1386-1409. https://doi.org/10.1002/asi.21309
[19]. Egghe, L. (2006). Theory and practice of the g-index. Scientometrics, 69(1), 131–152.
[20]. Chen, X. (2013). Research on the clustering analysis method based on minimum spanning tree (Doctoral dissertation). Chongqing University.
[21]. Harrison, J. A. (2020). Citizen science in South Africa: A personal perspective. OSTRICH, 91(2), 192-194. https://doi.org/10.2989/00306525.2020.1755381
[22]. Russell, C. (2021). Handbook of citizen science in ecology and conservation. African Journal of Range & Forage Science, 38(4), 296-297. https://doi.org/10.2989/10220119.2021.1938673
[23]. Taylor, J., Graham, M., Louw, A., Lepheana, A., Madikizela, B., Dickens, C., ... & Warner, S. (2022). Social change innovations, citizen science, miniSASS and the SDGs. Water Policy, 24(5), 708-717. https://doi.org/10.2166/wp.2021.264
[24]. Potts, W. M., Mann-Lang, J. B., Mann, B. Q., Griffiths, C. L., Attwood, C. G., de Blocq, A. D., ... & Thornycroft, R. (2021). South African marine citizen science - Benefits, challenges and future directions. African Journal of Marine Science, 43(3), 353-366. https://doi.org/10.2989/1814232X.2021.1960890
[25]. Amarakoon, V., Dharmarathne, G., Premasiri, R., Mukherjee, M., Shaw, R., & Wickramasinghe, D. (2024). Potential for the complementary and integrative use of citizen science and modern science in flood risk reduction: A case study from Sri Lanka. International Journal of Disaster Risk Reduction, 103, 104331. https://doi.org/10.1016/j.ijdrr.2024.104331
[26]. Callaghan, C. T., Mesaglio, T., Ascher, J. S., Brooks, T. M., Cabras, A. A., Chandler, M., ... & Young, A. N. (2022). The benefits of contributing to the citizen science platform iNaturalist as an identifier. PLOS Biology, 20(11), e3001843. https://doi.org/10.1371/journal.pbio.3001843
[27]. Khan, S., Hossain, F., Pavelsky, T., Parkins, G. M., Lane, M. R., Gomez, A. M., ... & Ahmad, S. K. (2023). Understanding volume estimation uncertainty of lakes and wetlands using satellites and citizen science. IEEE Journal of Selected Topics in Applied Earth Observations and Remote Sensing, 16, 2386-2401. https://doi.org/10.1109/JSTARS.2023.3250354
[28]. Simpson, R., Page, K. R., & De Roure, D. (2014). Zooniverse. In Proceedings of the 23rd International Conference on World Wide Web. ACM.
[29]. Smolinski, M. S., Crawley, A. W., Baltrusaitis, K., et al. (2015). Flu Near You: Crowdsourced Symptom Reporting Spanning 2 Influenza Seasons. American Journal of Public Health, 105(10), 2124–2130.
[30]. Wadi-Ramahi, S., Li, B., Waqqad, F., & AlSharif, A. (2023). Evolving practice in global healthcare: Remote physics support for low- and middle-income countries. Journal of Applied Clinical Medical Physics, 24(3). https://doi.org/10.1002/acm2.13914
[31]. Mwanza, J., Telukdarie, A., & Igusa, T. (2023). Impact of industry 4.0 on healthcare systems of low- and middle-income countries: A systematic review. Health and Technology, 13(1), 35-52. https://doi.org/10.1007/s12553-022-00714-2
[32]. Kakietek, J. J., Eberwein, J. D., Stacey, N., Newhouse, D., & Yoshida, N. (2022). Foregone healthcare during the COVID-19 pandemic: Early survey estimates from 39 low- and middle-income countries. Health Policy and Planning, 37(6), 771-778. https://doi.org/10.1093/heapol/czac024
[33]. Teixeira de Siqueira Filha, N., Li, J., Phillips-Howard, P. A., Quayyum, Z., Kibuchi, E., Mithu, M. I. H., ... & Elsey, H. (2022). The economics of healthcare access: A scoping review on the economic impact of healthcare access for vulnerable urban populations in low- and middle-income countries. International Journal for Equity in Health, 21(1). https://doi.org/10.1186/s12939-022-01804-3
[34]. De, P., & Pradhan, M. R. (2023). Effectiveness of mobile technology and utilization of maternal and neonatal healthcare in low- and middle-income countries (LMICs): A systematic review. BMC Women’s Health, 23(1). https://doi.org/10.1186/s12905-023-02825-y
[35]. Kwaitana, D., Chisoni, F., van Breevoort, D., Mildestvedt, T., Meland, E., Bates, J., & Umar, E. (2024). Primary healthcare service delivery for older people with progressive multimorbidity in low- and middle-income countries: A systematic review. Transactions of the Royal Society of Tropical Medicine and Hygiene, 118(3), 137-147. https://doi.org/10.1093/trstmh/trad068
[36]. Walters, S., Aldous, C., & Malherbe, H. (2024). Knowledge, attitudes, and practices of primary healthcare practitioners in low- and middle-income countries: A scoping review on genetics. Journal of Community Genetics. https://doi.org/10.1007/s12687-024-00721-y
[37]. Clarke-Deelder, E., Opondo, K., Oguttu, M., Burke, T., Cohen, J. L., & McConnell, M. (2023). Immediate postpartum care in low- and middle-income countries: A gap in healthcare quality research and practice. American Journal of Obstetrics & Gynecology MFM, 5(2), 100764. https://doi.org/10.1016/j.ajogmf.2022.100764
[38]. MacKechnie, M. C., Miclau, T. A., Cordero, D. M., Tahir, P., & Miclau, T., III. (2022). Leadership development programs for healthcare professionals in low-and middle-income countries: A systematic review. International Journal of Health Planning and Management, 37(4), 2149-2166. https://doi.org/10.1002/hpm.3457
[39]. Pradhan, N. A., Samnani, A. A. B. A., Abbas, K., & Rizvi, N. (2023). Resilience of primary healthcare system across low- and middle-income countries during COVID-19 pandemic: A scoping review. Health Research Policy and Systems, 21(1). https://doi.org/10.1186/s12961-023-01031-4
[40]. Ciecierski-Holmes, T., Singh, R., Axt, M., Brenner, S., & Barteit, S. (2022). Artificial intelligence for strengthening healthcare systems in low- and middle-income countries: A systematic scoping review. NPJ Digital Medicine, 5(1). https://doi.org/10.1038/s41746-022-00700-y
[41]. Cragg, L., Williams, S., & Chavannes, N. H. (2016). FRESH AIR: An implementation research project funded through Horizon 2020 exploring the prevention, diagnosis and treatment of chronic respiratory diseases in low-resource settings. npj Primary Care Respiratory Medicine, 26(1). https://doi.org/10.1038/npjpcrm.2016.35
[42]. Killough, C. M., Madaras, A., Phillips, C., Hettema, J., Ceballos, V., Fuentes, J. E., ... & Page, K. (2023). Community health worker insights on promoting research engagement with diverse populations. Frontiers in Public Health, 10. https://doi.org/10.3389/fpubh.2022.959504
[43]. Undurraga, E. A., Carias, C., Meltzer, M. I., & Kahn, E. B. (2017). Potential for broad-scale transmission of Ebola virus disease during the West Africa crisis: Lessons for the Global Health Security Agenda. Infectious Diseases of Poverty, 6(1). https://doi.org/10.1186/s40249-017-0373-4
[44]. van Dongen, B. M., Ridder, M. A. M., Wolters, L., Steenhuis, I. H. M., & Renders, C. M. (2023). Increasing community capacity to improve the implementation of Health Promoting Schools: Barriers and facilitators from the FLASH intervention. Health Promotion International, 38(5). https://doi.org/10.1093/heapro/daad115
[45]. Dreisbach, C., Grayson, S., Leggio, K., Conway, A., & Koleck, T. (2022). Predictors of unrelieved symptoms in All of Us Research Program participants with chronic conditions. Journal of Pain and Symptom Management, 64(6), 555-566. https://doi.org/10.1016/j.jpainsymman.2022.08.018
[46]. de Kok, J. W. T. M., de la Hoz, M. Á. A., de Jong, Y., Brokke, V., Elbers, P. W. G., Thoral, P., ... & Borrat, X. (2023). A guide to sharing open healthcare data under the General Data Protection Regulation. Scientific Data, 10(1). https://doi.org/10.1038/s41597-023-02256-2
Cite this article
Feng,Y. (2024). Bibliometric analysis of citizen science in global healthcare: Current trends, challenges, and future directions. Journal of Clinical Technology and Theory,1,41-50.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Journal:Journal of Clinical Technology and Theory
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Silvertown, J. (2009). A new dawn for citizen science. Trends in Ecology & Evolution, 24(9), 467–471. https://doi.org/10.1016/j.tree.2009.03.017
[2]. Kullenberg, C., & Kasperowski, D. (2016). What is citizen science? – A scientometric meta-analysis. PLOS ONE, 11(1), e0147152. https://doi.org/10.1371/journal.pone.0147152
[3]. Bonney, R., Cooper, C. B., Dickinson, J., et al. (2009). Citizen science: A developing tool for expanding science knowledge and scientific literacy. BioScience, 59(11), 977–984. https://doi.org/10.1525/bio.2009.59.11.9
[4]. McKinley, D. C., Miller-Rushing, A. J., Ballard, H. L., et al. (2017). Citizen science can improve conservation science, natural resource management, and environmental protection. Biological Conservation, 208, 15–28. https://doi.org/10.1016/j.biocon.2016.05.015
[5]. Follett, R., & Strezov, V. (2015). An analysis of citizen science based research: Usage and publication patterns. PLOS ONE, 10(11), e0143687. https://doi.org/10.1371/journal.pone.0143687
[6]. Laird, Y., Marks, L., Smith, B. J., et al. (2023). Harnessing citizen science in health promotion: Perspectives of policy and practice stakeholders in Australia. Health Promotion International, 38(5). https://doi.org/10.1093/heapro/daac003
[7]. Ballman, E. S., Leahy, J. E., Sponarski, C. C., et al. (2023). A citizen science approach to investigate the distribution, abundance, and pathogen infection of vector ticks through active surveillance. Ticks and Tick-borne Diseases, 14(3), 102144. https://doi.org/10.1016/j.ttbdis.2022.102144
[8]. Sgroi, G., D’Alessio, N., Marucci, G., et al. (2023). Trichinella britovi in wild boar meat from Italy, 2015–2021: A citizen science approach to surveillance. One Health, 16, 100480. https://doi.org/10.1016/j.onehlt.2023.100480
[9]. Ireson, J., Taylor, A., Richardson, E., et al. (2022). Exploring invisibility and epistemic injustice in Long Covid—A citizen science qualitative analysis of patient stories from an online Covid community. Health Expectations, 25(4), 1753–1765. https://doi.org/10.1111/hex.13511
[10]. Marks, L., Laird, Y., Trevena, H., et al. (2022). A scoping review of citizen science approaches in chronic disease prevention. Frontiers in Public Health, 10. https://doi.org/10.3389/fpubh.2022.805759
[11]. Tran, V.-T., Riveros, C., Péan, C., et al. (2019). Patients’ perspective on how to improve the care of people with chronic conditions in France: A citizen science study within the ComPaRe e-cohort. BMJ Quality & Safety, 28(11), 875–886. https://doi.org/10.1136/bmjqs-2019-009048
[12]. Winter, T., Riordan, B. C., Scarf, D., et al. (2022). Conspiracy beliefs and distrust of science predict reluctance of vaccine uptake of politically right-wing citizens. Vaccine, 40(12), 1896–1903. https://doi.org/10.1016/j.vaccine.2022.02.027
[13]. Fraisl, D., See, L., Estevez, D., et al. (2023). Citizen science for monitoring the health and well-being related Sustainable Development Goals and the World Health Organization’s Triple Billion Targets. Frontiers in Public Health, 11. https://doi.org/10.3389/fpubh.2023.1131154
[14]. Odeyemi, E., Chesser, S., King, A. C., et al. (2023). Engaging Nigerian older persons in neighborhood environment assessment for physical activity participation: A citizen science project. Innovation in Aging, 8(4). https://doi.org/10.1093/geroni/igad002
[15]. Chen, Y., Chen, C., Liu, Z., et al. (2015). The methodological functions of CiteSpace knowledge mapping. Studies in Science of Science, 33(02), 242-253. https://doi.org/10.16192/j.cnki.1003-2053.2015.02.009
[16]. Chen, C. (2004). Searching for intellectual turning points: Progressive knowledge domain visualization. PNAS, 101(suppl_1), 5303-5310. https://doi.org/10.1073/pnas.0307513100
[17]. Chen, C. (2006). CiteSpace II: Detecting and visualizing emerging trends and transient patterns in scientific literature. Journal of the American Society for Information Science and Technology, 57(3), 359-377. https://doi.org/10.1002/asi.20317
[18]. Chen, C., Ibekwe-SanJuan, F., & Hou, J. (2010). The structure and dynamics of cocitation clusters: A multiple‐perspective cocitation analysis. Journal of the American Society for Information Science and Technology, 61(7), 1386-1409. https://doi.org/10.1002/asi.21309
[19]. Egghe, L. (2006). Theory and practice of the g-index. Scientometrics, 69(1), 131–152.
[20]. Chen, X. (2013). Research on the clustering analysis method based on minimum spanning tree (Doctoral dissertation). Chongqing University.
[21]. Harrison, J. A. (2020). Citizen science in South Africa: A personal perspective. OSTRICH, 91(2), 192-194. https://doi.org/10.2989/00306525.2020.1755381
[22]. Russell, C. (2021). Handbook of citizen science in ecology and conservation. African Journal of Range & Forage Science, 38(4), 296-297. https://doi.org/10.2989/10220119.2021.1938673
[23]. Taylor, J., Graham, M., Louw, A., Lepheana, A., Madikizela, B., Dickens, C., ... & Warner, S. (2022). Social change innovations, citizen science, miniSASS and the SDGs. Water Policy, 24(5), 708-717. https://doi.org/10.2166/wp.2021.264
[24]. Potts, W. M., Mann-Lang, J. B., Mann, B. Q., Griffiths, C. L., Attwood, C. G., de Blocq, A. D., ... & Thornycroft, R. (2021). South African marine citizen science - Benefits, challenges and future directions. African Journal of Marine Science, 43(3), 353-366. https://doi.org/10.2989/1814232X.2021.1960890
[25]. Amarakoon, V., Dharmarathne, G., Premasiri, R., Mukherjee, M., Shaw, R., & Wickramasinghe, D. (2024). Potential for the complementary and integrative use of citizen science and modern science in flood risk reduction: A case study from Sri Lanka. International Journal of Disaster Risk Reduction, 103, 104331. https://doi.org/10.1016/j.ijdrr.2024.104331
[26]. Callaghan, C. T., Mesaglio, T., Ascher, J. S., Brooks, T. M., Cabras, A. A., Chandler, M., ... & Young, A. N. (2022). The benefits of contributing to the citizen science platform iNaturalist as an identifier. PLOS Biology, 20(11), e3001843. https://doi.org/10.1371/journal.pbio.3001843
[27]. Khan, S., Hossain, F., Pavelsky, T., Parkins, G. M., Lane, M. R., Gomez, A. M., ... & Ahmad, S. K. (2023). Understanding volume estimation uncertainty of lakes and wetlands using satellites and citizen science. IEEE Journal of Selected Topics in Applied Earth Observations and Remote Sensing, 16, 2386-2401. https://doi.org/10.1109/JSTARS.2023.3250354
[28]. Simpson, R., Page, K. R., & De Roure, D. (2014). Zooniverse. In Proceedings of the 23rd International Conference on World Wide Web. ACM.
[29]. Smolinski, M. S., Crawley, A. W., Baltrusaitis, K., et al. (2015). Flu Near You: Crowdsourced Symptom Reporting Spanning 2 Influenza Seasons. American Journal of Public Health, 105(10), 2124–2130.
[30]. Wadi-Ramahi, S., Li, B., Waqqad, F., & AlSharif, A. (2023). Evolving practice in global healthcare: Remote physics support for low- and middle-income countries. Journal of Applied Clinical Medical Physics, 24(3). https://doi.org/10.1002/acm2.13914
[31]. Mwanza, J., Telukdarie, A., & Igusa, T. (2023). Impact of industry 4.0 on healthcare systems of low- and middle-income countries: A systematic review. Health and Technology, 13(1), 35-52. https://doi.org/10.1007/s12553-022-00714-2
[32]. Kakietek, J. J., Eberwein, J. D., Stacey, N., Newhouse, D., & Yoshida, N. (2022). Foregone healthcare during the COVID-19 pandemic: Early survey estimates from 39 low- and middle-income countries. Health Policy and Planning, 37(6), 771-778. https://doi.org/10.1093/heapol/czac024
[33]. Teixeira de Siqueira Filha, N., Li, J., Phillips-Howard, P. A., Quayyum, Z., Kibuchi, E., Mithu, M. I. H., ... & Elsey, H. (2022). The economics of healthcare access: A scoping review on the economic impact of healthcare access for vulnerable urban populations in low- and middle-income countries. International Journal for Equity in Health, 21(1). https://doi.org/10.1186/s12939-022-01804-3
[34]. De, P., & Pradhan, M. R. (2023). Effectiveness of mobile technology and utilization of maternal and neonatal healthcare in low- and middle-income countries (LMICs): A systematic review. BMC Women’s Health, 23(1). https://doi.org/10.1186/s12905-023-02825-y
[35]. Kwaitana, D., Chisoni, F., van Breevoort, D., Mildestvedt, T., Meland, E., Bates, J., & Umar, E. (2024). Primary healthcare service delivery for older people with progressive multimorbidity in low- and middle-income countries: A systematic review. Transactions of the Royal Society of Tropical Medicine and Hygiene, 118(3), 137-147. https://doi.org/10.1093/trstmh/trad068
[36]. Walters, S., Aldous, C., & Malherbe, H. (2024). Knowledge, attitudes, and practices of primary healthcare practitioners in low- and middle-income countries: A scoping review on genetics. Journal of Community Genetics. https://doi.org/10.1007/s12687-024-00721-y
[37]. Clarke-Deelder, E., Opondo, K., Oguttu, M., Burke, T., Cohen, J. L., & McConnell, M. (2023). Immediate postpartum care in low- and middle-income countries: A gap in healthcare quality research and practice. American Journal of Obstetrics & Gynecology MFM, 5(2), 100764. https://doi.org/10.1016/j.ajogmf.2022.100764
[38]. MacKechnie, M. C., Miclau, T. A., Cordero, D. M., Tahir, P., & Miclau, T., III. (2022). Leadership development programs for healthcare professionals in low-and middle-income countries: A systematic review. International Journal of Health Planning and Management, 37(4), 2149-2166. https://doi.org/10.1002/hpm.3457
[39]. Pradhan, N. A., Samnani, A. A. B. A., Abbas, K., & Rizvi, N. (2023). Resilience of primary healthcare system across low- and middle-income countries during COVID-19 pandemic: A scoping review. Health Research Policy and Systems, 21(1). https://doi.org/10.1186/s12961-023-01031-4
[40]. Ciecierski-Holmes, T., Singh, R., Axt, M., Brenner, S., & Barteit, S. (2022). Artificial intelligence for strengthening healthcare systems in low- and middle-income countries: A systematic scoping review. NPJ Digital Medicine, 5(1). https://doi.org/10.1038/s41746-022-00700-y
[41]. Cragg, L., Williams, S., & Chavannes, N. H. (2016). FRESH AIR: An implementation research project funded through Horizon 2020 exploring the prevention, diagnosis and treatment of chronic respiratory diseases in low-resource settings. npj Primary Care Respiratory Medicine, 26(1). https://doi.org/10.1038/npjpcrm.2016.35
[42]. Killough, C. M., Madaras, A., Phillips, C., Hettema, J., Ceballos, V., Fuentes, J. E., ... & Page, K. (2023). Community health worker insights on promoting research engagement with diverse populations. Frontiers in Public Health, 10. https://doi.org/10.3389/fpubh.2022.959504
[43]. Undurraga, E. A., Carias, C., Meltzer, M. I., & Kahn, E. B. (2017). Potential for broad-scale transmission of Ebola virus disease during the West Africa crisis: Lessons for the Global Health Security Agenda. Infectious Diseases of Poverty, 6(1). https://doi.org/10.1186/s40249-017-0373-4
[44]. van Dongen, B. M., Ridder, M. A. M., Wolters, L., Steenhuis, I. H. M., & Renders, C. M. (2023). Increasing community capacity to improve the implementation of Health Promoting Schools: Barriers and facilitators from the FLASH intervention. Health Promotion International, 38(5). https://doi.org/10.1093/heapro/daad115
[45]. Dreisbach, C., Grayson, S., Leggio, K., Conway, A., & Koleck, T. (2022). Predictors of unrelieved symptoms in All of Us Research Program participants with chronic conditions. Journal of Pain and Symptom Management, 64(6), 555-566. https://doi.org/10.1016/j.jpainsymman.2022.08.018
[46]. de Kok, J. W. T. M., de la Hoz, M. Á. A., de Jong, Y., Brokke, V., Elbers, P. W. G., Thoral, P., ... & Borrat, X. (2023). A guide to sharing open healthcare data under the General Data Protection Regulation. Scientific Data, 10(1). https://doi.org/10.1038/s41597-023-02256-2