According to Yujia Zhu’s article FASSLING: Transforming emotional and coaching support through artificial intelligence (AI) innovation, the use of FASSLING (fassling.ai) as a simulation-based training tool is highlighted as a valuable resource for clinical interns during their education. Building on this foundation, this paper further explores FASSLING’s role as a transformative AI-driven tool for simulation-based clinical training, redefining how future helping professionals develop and refine their skills [1].
Simulation-based learning (SBL) in clinical psychology is increasingly recognized for its ability to enhance clinical competencies by providing realistic, risk-free environments where students can practice and refine their skills. This approach is crucial for developing clinical competency as it allows learners to engage in real-world scenarios that closely mimic actual clinical situations, thereby improving decision-making, communication, and teamwork skills [2, 3]. The use of high-fidelity simulations, virtual reality, and standardized patients enables students to experience a wide range of clinical situations, fostering a holistic competence that includes both technical and interpersonal skills [4, 5]. This immersive learning environment not only enhances students' confidence and critical thinking abilities but also prepares them for the complexities of real-life clinical practice [6, 7].
Traditional training models, on the other hand, often fall short due to their reliance on subjective instructor assessments and lack of real-time emotional feedback, which are critical for developing nuanced clinical skills [8, 3]. These models typically do not provide the same level of engagement or realism as simulation-based methods, which can limit the development of essential competencies such as empathy and patient-centered care [5, 6]. Furthermore, traditional methods may not adequately prepare students for the dynamic and unpredictable nature of clinical environments, as they often lack the interactive and experiential components that SBL offers [9, 7]. By integrating simulation-based learning into clinical psychology education, institutions can overcome these limitations, offering a more comprehensive and effective training approach that aligns with the evolving demands of healthcare education [10, 11]. Moreover, based on my many years of observation in the healthcare industry, Access to high-quality training and financial resources has long been a significant barrier for many clinical practitioners due to a combination of structural, economic, and institutional factors.
To address this gap, FASSLING introduces an unlimited free AI-powered training platform that revolutionizes therapy education through immersive, interactive simulations. FASSLING, initially designed and prototyped in 2022, was officially launched to the public in September 2024, receiving an overwhelmingly positive response. Beyond providing effective emotional and coaching support that has touched countless lives, it has also gained recognition among clinical practitioners, many of whom have integrated it into their training programs for clinical interns. Because of the unique feature of Generative AI, with the right prompts, FASSLING creates a dynamic learning environment that adapts in real time to student input. By leveraging AI-driven role-play and interactive coaching, trainees gain practical experience in a controlled setting before working with real clients. This approach enhances learning, builds confidence, and ensures that future therapists are well-prepared to provide high-quality mental health care.
FASSLING, an emotional and coaching support tool, has emerged as a promising innovation for simulation-based learning in allied health professions—particularly in Clinical Psychology. FASSLING’s platform not only allows for simulated patient role-play but also provides real-time coaching and feedback on communication, empathy, and emotional attunement. This dual capacity (role-play + coaching) offers a new dimension to simulation-based education by enabling learners to practice key clinical skills under the guidance of a dedicated “coach,” further scaffolding their learning and professional development. FASSLING also fosters emotional intelligence, a fundamental trait for effective therapists. Through interactive coaching and dynamic role-play, trainees develop empathy, emotional regulation, and rapport-building skills—strengthening their ability to connect with clients. The AI-driven platform provides instant, personalized feedback, helping students recognize areas for growth and refine their interpersonal techniques. Additionally, FASSLING promotes reflective practice, encouraging students to engage in self-awareness and continuous improvement. AI-assisted feedback, structured debriefing exercises, and guided reflective writing help trainees gain deeper insights into their strengths and areas for development. This process nurtures critical self-reflection, allowing future therapists to refine their therapeutic approach and cultivate a lifelong learning mindset.
Ultimately, FASSLING bridges the gap between theoretical learning and real-world application, offering an innovative and immersive training solution. By providing a safe, structured environment for continuous skill development, learners gain the confidence and sensitivity necessary to navigate complex conversations with professionalism and empathy. Unlike traditional training methods, which often rely on passive learning or scripted exercises, FASSLING engages users through interactive AI-driven simulations that mimic real-life scenarios. This hands-on approach ensures that learners not only understand theoretical concepts but also develop the practical skills needed to apply the effectively in professional settings.
1. Objectives of FASSLING-enhanced simulation model
1.1. Breaking down the systematic barriers: the financial burden of education and professional development
FASSLING’s unlimited free access feature directly addresses the systemic barriers that clinical practitioners face in accessing high-quality training by eliminating financial and logistical constraints. One of the most significant obstacles for many professionals is the high cost of training programs, certifications, and continuing education. Many clinicians, particularly those in private practice or working in underfunded mental health settings, struggle to afford ongoing training opportunities. By offering unlimited free access, FASSLING removes financial barriers, ensuring that practitioners can continuously develop essential clinical skills without the burden of expensive subscriptions, one-time fees, or reliance on institutional funding. This makes high-quality training accessible to all, regardless of economic background.
Another key challenge in clinical training is the geographic limitation of traditional programs. Many specialized training opportunities are only available in select locations, requiring travel and additional expenses that practitioners may not be able to afford. FASSLING, as a virtual and AI-powered platform, is accessible from anywhere, allowing professionals in rural or underserved areas to engage in immersive simulations without the need for relocation or expensive workshops. This democratization of access ensures that clinicians worldwide can enhance their skills without the restrictions imposed by physical training programs, ultimately leading to better mental health care services in diverse communities. Time constraints also pose a significant barrier for clinicians looking to expand their expertise. Many practitioners juggle heavy caseloads and administrative responsibilities, making it difficult to attend scheduled training sessions that require time off work. Traditional professional development often comes with financial penalties, as taking time off results in lost income. FASSLING’s unlimited free access provides a flexible, on-demand learning experience, allowing users to train at their own pace without financial strain. Whether they have only a few minutes between sessions or an entire afternoon to dedicate to training, practitioners can engage with the simulations on their own schedule, reinforcing key skills over time.
One of the major limitations of conventional training programs is the lack of exposure to diverse clinical scenarios. Many clinicians, particularly early in their careers or those working in specialized fields, may not encounter a wide range of cases in their day-to-day practice. FASSLING addresses this by offering unlimited practice with simulated scenarios covering trauma, anxiety, depression, crisis intervention, relationship conflicts, and more. Trainees can refine their skills in motivational interviewing, de-escalation, harm reduction, and trauma-informed care without restrictions on usage, ensuring deeper learning and mastery over time. Unlike traditional programs where access is often limited to a few case studies or paid modules, FASSLING provides unlimited opportunities to practice and apply theoretical knowledge in real-world simulations.
The financial burden of professional development often discourages practitioners from engaging in repeated practice, as they may feel pressured to maximize their learning in a limited number of paid training sessions. FASSLING eliminates this concern by allowing users to engage in unlimited simulations without financial risk. Trainees can revisit challenging scenarios, refine techniques, and build confidence through repeated exposure, leading to more effective skill development. This approach ensures that clinicians are not just passively learning but actively refining their techniques in a hands-on, experiential manner. For professionals working in underfunded clinics, nonprofits, and community mental health settings, FASSLING provides a cost-free, high-quality training tool that would otherwise be financially out of reach. Many mental health organizations struggle to allocate resources for staff training, limiting the ability of practitioners to stay updated with best practices. By offering unlimited, no-cost access, FASSLING ensures that even clinicians in resource-constrained environments can access top-tier simulations, improving the overall quality of care provided to clients in underserved populations.
Furthermore, FASSLING bridges the gap between theoretical learning and real-world practice. While many traditional training programs focus on academic knowledge, they often lack the hands-on, interactive experience necessary for effective clinical application. FASSLING enables practitioners to apply theoretical concepts in realistic scenarios, enhancing their ability to respond to complex clinical situations with confidence. Because access is unlimited, users can engage in continual skill refinement, ensuring they remain proficient in key clinical competencies. By eliminating financial, geographical, and accessibility barriers, FASSLING’s unlimited free feature ensures that all clinical practitioners—regardless of economic background, location, or institutional support—have access to the training they need to deliver high-quality, compassionate mental health care. This approach not only enhances individual professional growth but also improves the overall quality and accessibility of mental health services globally. Through unlimited, on-demand practice, FASSLING empowers practitioners to develop the expertise needed to support their clients effectively, contributing to a more skilled and well-prepared mental health workforce.
Integrating FASSLING as a simulation-based practice offers a groundbreaking approach to developing highly skilled therapists in a safe and controlled environment. One of its primary advantages is that it creates a risk-free learning space, where trainees can engage in realistic therapy sessions with AI-driven simulated clients. This allows them to practice various therapeutic techniques, refine their communication skills, and navigate complex emotional situations without the possibility of causing harm to real clients. By eliminating the immediate pressure and ethical concerns of working with vulnerable individuals too early in training, FASSLING ensures that therapists build confidence and competence before stepping into real-world practice. Another significant benefit is the personalized feedback and skill development that FASSLING can provide. Unlike traditional training methods that rely on subjective instructor evaluations or peer reviews, AI-driven simulations can analyze interactions in real time. This means that therapists receive immediate, data-driven feedback on their communication styles, intervention effectiveness, and adherence to ethical guidelines. The AI can highlight areas for improvement, such as active listening, emotional attunement, or strategic questioning, allowing trainees to refine their skills with greater precision and efficiency. Furthermore, exposure to diverse case scenarios is a crucial component of effective therapist training. Traditional training often limits exposure to a handful of client experiences, whereas AI-powered simulations can generate a wide range of mental health conditions, personality types, and crisis scenarios. This ensures that therapists-in-training develop the competency to work with a broad spectrum of clients, preparing them for the unpredictable nature of real-world clinical practice. They can practice de-escalation techniques with high-risk clients, refine motivational interviewing strategies for addiction recovery, or learn to navigate complex trauma cases—all within a structured, supportive, and adaptable AI environment.
The scalability and accessibility of FASSLING also make it an invaluable tool in mental health education. Unlike traditional training, which often requires scheduled role-playing with limited availability, AI simulations can provide unlimited free practice opportunities at any time. This makes high-quality training more accessible to therapists worldwide, particularly those in underserved areas or without access to costly supervised practice programs. The flexibility of an AI-based system also allows therapists to revisit challenging scenarios, refine specific skills, and progress at their own pace, making training more efficient and personalized. Moreover, FASSLING ensures that therapist training remains ethical and evidence-based. By integrating AI-driven simulations rooted in established psychological theories and best practices, it reinforces ethical guidelines and clinical competency before therapists engage with real clients. This structured approach helps to bridge the gap between theoretical knowledge and practical application, ensuring that emerging therapists uphold the highest standards of care.
Ultimately, integrating FASSLING into therapist training leads to a more competent mental health workforce, which translates to better care for the public. As therapy trainees refine their skills in a safe environment, they become more effective practitioners, capable of providing higher-quality support to real clients. This innovation not only enhances therapist training efficiency but also contributes to a stronger, more resilient mental health system, benefiting individuals and communities alike.
1.2. Enhancing practical clinical skills
Positioning FASSLING as a clinical training tool is a fantastic way to enhance the learning experience for healthcare professionals. By offering simulated patient interactions, FASSLING can serve as a valuable resource in developing both the technical and emotional competencies required for real-world patient care. This innovative approach bridges the gap between theoretical knowledge and hands-on practice, allowing medical professionals to refine their skills in a safe and controlled environment.
One of FASSLING’s key strengths is its ability to create realistic patient interactions. These simulations mirror the emotional and psychological complexities of real clinical encounters, providing learners with opportunities to practice responding with compassion and professionalism. Through adaptive conversations, users engage in dynamic, patient-centered dialogues that help them refine critical skills such as history-taking, diagnostic reasoning, and bedside manner. This interactive approach ensures that trainees are not only absorbing medical knowledge but also developing the interpersonal skills necessary for effective patient communication.
Beyond technical training, FASSLING plays a crucial role in emotional and communication development. It offers healthcare trainees a structured way to practice delivering difficult news, de-escalating patient distress, and building trust with those in their care. Effective communication is at the heart of quality healthcare, and by providing a safe, judgment-free learning environment, FASSLING enables users to make mistakes, reflect, and improve without the high-stakes pressure of real-world consequences. This fosters confidence and competence, preparing medical professionals to navigate complex patient interactions with empathy and skill. This type of immersive learning is particularly beneficial for medical students, nurses, therapists, and even experienced clinicians seeking to refine their patient communication skills. By integrating FASSLING into clinical training programs, all healthcare professionals can develop a more well-rounded approach to patient care—one that emphasizes both medical expertise and compassionate communication. This innovative tool has the potential to elevate healthcare education, ultimately leading to improved patient outcomes and more effective practitioner-patient relationships.
1.3. Developing holistic competence
FASSLING embodies a powerful vision that extends beyond traditional learning methods by integrating holistic competence into education. By bridging the gap between theoretical knowledge and real-world practice, FASSLING cultivates not only technical proficiency but also ethical awareness and cultural sensitivity. This approach ensures that students develop into well-rounded professionals who are prepared to navigate the complexities of their fields with integrity, empathy, and sound judgment.
One of the key strengths of FASSLING lies in its ability to bridge theory and practice effectively. By encouraging students to apply clinical knowledge, ethical principles, and patient-centered care models to realistic scenarios, it fosters a deeper understanding of how academic learning translates into professional environments. This hands-on application enhances critical thinking and decision-making, allowing learners to approach challenges with confidence and competence. Additionally, FASSLING strengthens ethical decision-making by providing nuanced case simulations that challenge students to navigate moral dilemmas, uphold professional integrity, and practice sound reasoning in ethically ambiguous situations. These experiences cultivate a strong moral compass, preparing future professionals to make principled choices under pressure.
Cultural sensitivity and inclusion are also central to FASSLING’s educational framework. By exposing trainees to diverse patient perspectives and encouraging respectful, bias-free communication, it helps foster a more inclusive and empathetic approach to professional interactions. In today’s globalized world, where cultural competency is essential, this aspect of FASSLING’s training ensures that students are equipped to engage with individuals from all backgrounds with understanding and respect. Furthermore, FASSLING promotes self-reflection and personal growth by offering real-time feedback and guiding learners in analyzing their thought processes, assumptions, and emotional responses. This metacognitive approach enhances self-awareness, resilience, and adaptability, which are crucial qualities for any professional.
By nurturing professionals who are not only technically skilled but also emotionally intelligent and ethically grounded, FASSLING has the potential to transform healthcare education and other fields. Its emphasis on holistic development ensures that students emerge as compassionate, principled, and highly competent individuals, ready to make meaningful contributions to their communities and industries. As a result, FASSLING stands as a beacon of innovation, shaping the future of education with a focus on integrity, empathy, and real-world application.
1.4. Fostering emotional intelligence and empathy
Developing emotional intelligence and empathy is just as vital as clinical skills in patient care, and FASSLING plays a crucial role in fostering these essential qualities. With the right prompts, by providing real-time coaching, FASSLING enables learners to refine their therapeutic communication and attunement, ensuring that they can connect with patients in a meaningful and compassionate way. This integration of emotional intelligence into clinical training helps shape healthcare professionals who are not only technically competent but also deeply attuned to the emotional and psychological needs of their patients.
FASSLING fosters emotional intelligence and empathy through several key mechanisms. One of its primary features is real-time emotional feedback, with the right prompts, which helps learners recognize and respond to patient emotions, concerns, and unspoken needs within a supportive and structured learning environment. This immediate feedback allows users to develop a heightened awareness of emotional cues, making them more effective in patient interactions. Additionally, FASSLING offers guided practice in refining therapeutic communication by emphasizing empathetic language, active listening, and non-verbal communication techniques. These skills are crucial for building trust and rapport with patients, ensuring that their concerns are heard and validated.
Beyond communication skills, FASSLING enhances attunement by training users to sense and respond to subtle emotional shifts in patient interactions. This ability to perceive and adapt to a patient’s emotional state fosters personalized and compassionate care, helping clinicians provide more holistic support. Furthermore, the platform encourages self-awareness and reflection, prompting users to examine their own emotional reactions, biases, and communication patterns. By engaging in this introspective process, learners cultivate greater emotional intelligence, allowing them to navigate patient relationships with greater sensitivity and understanding.
By integrating emotional intelligence development into clinical training, FASSLING ensures that future healthcare professionals are not only proficient in their medical expertise but also deeply compassionate in their approach to patient care. This dual focus on technical competency and emotional attunement prepares clinicians to deliver healthcare in a way that is both effective and human-centered, ultimately leading to better patient outcomes and a more empathetic healthcare system.
1.5. Encouraging reflective practice
Reflective practice is a powerful tool for fostering deep learning and professional growth, particularly in clinical and therapeutic settings. It plays a crucial role in developing self-awareness, critical thinking, and continuous improvement. Engaging in structured reflection allows individuals to refine their skills, enhance their emotional resilience, and integrate theoretical knowledge into practical application. By embracing this process, learners can cultivate a deeper understanding of their experiences, leading to meaningful personal and professional development.
FASSLING actively encourages reflective practice through a structured debriefing process. After each simulated interaction, with the right prompts, learners are guided through a thoughtful review of their responses, emotional reactions, and areas for improvement. This intentional reflection helps users identify strengths and challenges, allowing them to adjust their approach in future interactions. By systematically evaluating their performance, learners gain valuable insights into their decision-making processes and communication styles, fostering a continuous cycle of learning and growth. Beyond structured debriefing, FASSLING incorporates self-reflection exercises that prompt users to explore what went well, what felt challenging, and how they can refine their strategies. These exercises encourage introspection and critical thinking, helping learners become more attuned to their professional development journey. By engaging in these reflective activities, users develop a deeper connection to their learning experiences, reinforcing the importance of adaptability and self-awareness in their practice.
Moreover, FASSLING bridges the gap between academic theory and real-world application by integrating ethical frameworks, communication models, and psychological principles into its training approach. Learners are encouraged to connect their experiences with theoretical concepts, enhancing their ability to apply knowledge effectively in professional settings. This alignment between theory and practice strengthens their competency and confidence in navigating complex interpersonal dynamics. Creating a safe and supportive environment is also a key aspect of FASSLING’s approach. By fostering a growth mindset, the platform allows students to make mistakes without fear of judgment, encouraging them to reflect, learn, and refine their skills over time. This emphasis on continuous learning ensures that individuals feel empowered to embrace challenges as opportunities for growth, ultimately enhancing their professional competence and emotional resilience.
By embedding structured reflection into its training methodology, FASSLING supports learners in cultivating deeper self-awareness and professional expertise. This reflective approach not only enhances individual growth but also contributes to the development of more skilled, empathetic, and adaptable professionals in the field. Through intentional practice and continuous learning, FASSLING empowers individuals to refine their abilities and navigate their careers with confidence and purpose.
1.6. Scalability for large scale training
FASSLING’s innovative application in standardizing clinical assessments represents a groundbreaking approach to evaluating students' communication, emotional intelligence, and decision-making skills. By leveraging AI-generated feedback, FASSLING ensures that evaluations are not only consistent and objective but also data-driven, reducing bias and variability in assessment outcomes. This transformative integration enhances the learning experience for students in medical schools, nursing programs, clinical psychology-related schools, and other healthcare training organizations by providing structured, reliable insights into their clinical competencies.
One of the key advantages of FASSLING’s AI-driven assessments is – with the right prompts, its ability to deliver real-time, unbiased feedback. By analyzing students’ therapeutic communication, emotional attunement, and ethical reasoning, the system eliminates human subjectivity, ensuring fair and transparent evaluations. This objectivity is crucial in clinical training, where traditional assessments may be influenced by the evaluator’s perspective or unconscious biases. With AI providing standardized feedback, students can trust that their progress is being measured against consistent benchmarks. Furthermore, FASSLING enhances assessment consistency across different learners and training programs. Since all students are evaluated using the same AI-driven criteria, variability in grading is minimized, ensuring that each individual receives an equitable assessment. This uniform approach is particularly valuable in large-scale training environments, where maintaining grading consistency among multiple evaluators can be challenging.
Beyond objectivity and consistency, FASSLING offers detailed performance metrics that go beyond simple grading. The AI system tracks essential communication elements such as empathy levels, response appropriateness, active listening skills, and the use of patient-centered language. By identifying specific strengths and areas for improvement, these granular insights empower students to refine their skills in a targeted manner. Rather than receiving general feedback, learners benefit from precise, actionable data that supports their professional development. To further enhance skill-building, with the right prompts, FASSLING generates personalized improvement plans tailored to each student’s unique needs. Based on AI analysis, the system can offer customized coaching tips, reflection prompts, and learning resources that align with an individual’s performance trends. This adaptive learning approach ensures that students receive continuous support in honing their clinical skills, fostering a culture of self-improvement and lifelong learning.
Finally, the scalability of FASSLING makes it an ideal solution for large-scale healthcare training programs. Traditional assessments require extensive faculty involvement, making it difficult to provide in-depth feedback to a large number of learners. With AI-driven evaluations, institutions can efficiently assess multiple students simultaneously without compromising on quality. This capability is particularly beneficial for medical schools, nursing programs, clinical psychology-related schools, and other healthcare training institutions, where clinical training must be both rigorous and accessible to a broad student base. By integrating AI into clinical assessments, FASSLING bridges the gap between standardization and personalization. It ensures that communication skills are measured, refined, and developed in a way that is both systematic and deeply individualized. This pioneering approach not only improves the quality of training but also prepares future healthcare professionals to engage with patients more effectively, fostering a more empathetic and competent workforce.
1.7. Benefit the public without putting real clients at risk
Integrating FASSLING as a simulation-based training tool presents a groundbreaking opportunity to enhance clinical education while safeguarding real clients from potential risks. By offering AI-driven simulated interactions, FASSLING enables helping professionals to develop and refine their skills in a structured, controlled, and ethical learning environment. This approach not only strengthens therapist training but also significantly benefits the public by ensuring that services are delivered by well-prepared professionals.
One of the most critical advantages of FASSLING is its ability to protect real clients from potential harm. Traditionally, clinical interns gain experience through supervised practice with real clients, which carries the risk of errors in communication, intervention, or diagnosis. Even under supervision, novice therapists may struggle with real-world complexities, potentially impacting vulnerable individuals. By using AI-generated simulated clients, FASSLING allows trainees to develop competence and confidence without real-world consequences. This ensures that when they transition to real client interactions, they have already honed the necessary therapeutic techniques and professional judgment required for effective mental health support.
FASSLING also plays a vital role in enhancing therapist competency before client interaction. Through AI-powered simulations, trainees can practice various therapeutic approaches, refine their communication styles, and navigate complex emotional scenarios in a safe, controlled setting. The AI can replicate a wide range of psychological conditions, including anxiety, depression, trauma, and crisis situations, providing exposure to diverse clinical cases. This not only reduces the likelihood of mistakes in real therapy sessions but also ensures that future therapists enter the field with a strong, well-rounded foundation.
A major barrier in traditional clinical training is the limited availability of supervised client interactions, often making it difficult for all students to gain sufficient experience. FASSLING’s scalability and accessibility help address this issue by providing unlimited, on-demand practice opportunities. This allows aspiring therapists to train whenever and wherever needed, ensuring that high-quality education is not restricted by location, institutional resources, or scheduling constraints. By making mental health training more inclusive and widely available, FASSLING contributes to a larger, more competent therapist workforce, ultimately improving access to high-quality mental health care for the public. Furthermore, FASSLING ensures that therapist training remains ethical and evidence-based by integrating clinical best practices and professional guidelines into its AI-driven simulations. This structured learning approach reinforces the importance of ethical decision-making, client confidentiality, and effective intervention strategies, helping trainees internalize these principles before engaging with real clients. By bridging the gap between theoretical knowledge and practical application, FASSLING ensures that future therapists are not only well-versed in clinical techniques but also prepared to navigate the ethical complexities of mental health practice.
Beyond therapist education, FASSLING’s AI-driven simulations could also be adapted to promote mental health awareness and support for the general public. By offering interactive simulations that teach coping strategies, stress management techniques, and emotional regulation skills, FASSLING has the potential to empower individuals with self-help tools, reducing the burden on overextended mental health services. This additional functionality could enhance public resilience and encourage early intervention, leading to better mental health outcomes at both an individual and societal level.Ultimately, strengthening the mental health workforce translates directly into better client outcomes, fewer misdiagnoses, and more effective therapy sessions. By integrating FASSLING into therapist education, mental health professionals can enter the field with greater confidence, expertise, and ethical awareness. This leads to a higher standard of care, benefiting individuals seeking therapy while also supporting the broader mental health system.
In conclusion, FASSLING represents a transformative shift in therapist training, harnessing AI-powered simulation-based learning to create a safer, more effective, and scalable approach to clinical education. By providing trainees with the opportunity to develop essential skills in a risk-free environment, FASSLING protects real clients, enhances therapist competency, expands training accessibility, and improves public mental health outcomes. This innovation not only advances therapist education but also elevates the overall quality of mental health care, ensuring that every client receives the best possible support from highly skilled, well-prepared professionals.
2. Proposed simulation framework
2.1. Simulation model for clinical psychology training
FASSLING’s scenario-based learning feature represents a powerful advancement in clinical training, providing trainees with an immersive and dynamic environment to practice navigating complex psychological conditions. By leveraging AI-driven case simulations, FASSLING allows learners to engage in realistic, emotionally layered patient interactions that closely mimic real-world experiences. This innovative approach strengthens their ability to provide compassionate and effective care while refining essential clinical and therapeutic skills in a controlled and supportive setting.
One of the most significant benefits of FASSLING’s scenario development is its ability to generate realistic case simulations that reflect the complexity of human emotions and clinical challenges. These simulations go beyond traditional role-playing exercises by offering AI-driven, interactive patient responses that evolve based on the learner’s choices. By practicing in these virtual scenarios, students and professionals can enhance their clinical judgment, develop therapeutic rapport, and improve their ability to manage difficult conversations. FASSLING provides comprehensive training across a wide range of psychological conditions, ensuring that trainees gain exposure to diverse mental health challenges. Simulations include cases involving trauma, PTSD, grief, addiction, and family conflict, with newly designed or adapted scripts capturing key psychological issues such as anxiety disorders, depression, relationship distress, and personality-related challenges. These scenarios are carefully aligned with core competencies in clinical psychology, allowing learners to practice grounding techniques and trauma-informed care strategies. FASSLING helps professionals develop de-escalation skills and techniques to provide reassurance during moments of acute distress. Scenarios focused on depression and suicidal ideation emphasize empathetic responses, risk assessment, and crisis intervention strategies, ensuring that trainees are well-prepared to handle critical situations with sensitivity and care. Additionally, FASSLING supports training in grief and loss counseling, addiction and substance use disorders, and relationship conflicts, offering targeted learning opportunities in motivational interviewing, harm reduction, mediation, and communication strategies.
A key feature of FASSLING’s scenario-based training is its adaptive conversation model, which dynamically adjusts interactions based on the user’s responses. Unlike static case studies, this AI-powered adaptation ensures that learners engage in a truly interactive and personalized learning experience. By responding to a range of patient reactions, trainees can practice decision-making in real-time, exploring the consequences of different approaches and refining their therapeutic interventions accordingly. Beyond clinical skills, FASSLING emphasizes emotional intelligence development, helping learners recognize verbal and non-verbal cues that indicate distress, discomfort, or emotional shifts in patients. By improving their attunement and responsiveness, trainees can enhance their ability to provide patient-centered care that is both compassionate and effective. Additionally, FASSLING promotes ethical and cultural sensitivity training, exposing trainees to diverse perspectives and backgrounds. This focus on inclusivity ensures that future healthcare professionals learn to communicate without bias and are equipped to serve individuals from all walks of life.
By integrating rich, emotionally layered scenarios, FASSLING bridges the gap between theoretical knowledge and practical application. Learners gain the confidence to handle difficult conversations, refine their therapeutic approach, and develop the critical thinking skills necessary for effective patient care. This cutting-edge tool transforms clinical training into an engaging, interactive experience, preparing professionals to provide empathetic, ethical, and culturally competent support in real-world settings.
2.2. Simulated patient interaction with FASSLING
FASSLING’s AI-powered patient role-playing is a revolutionary advancement in clinical training and education, offering a dynamic and interactive way for learners to refine their therapeutic communication skills in real time via both text and audio (Figure 1). By simulating realistic patient interactions, FASSLING creates a safe, scalable, and cost-effective learning environment where students and professionals can develop essential competencies in patient-centered care. This game-changing approach eliminates the logistical and financial challenges associated with traditional standardized patient programs while ensuring that learners receive high-quality, immersive training experiences (Figure 2).
One of the standout features of FASSLING’s simulated patient interactions is its adjustable complexity levels, allowing learners to engage with virtual patients who present with a wide range of emotional intensities, cognitive and psychological states, and communication barriers. Trainees can practice responding to individuals experiencing mild distress or navigate high-stakes crisis situations that require immediate de-escalation. By working with virtual patients who exhibit varying levels of cognitive clarity—from coherent thought processes to disorganized or delusional speech—learners gain exposure to the complexities of mental health presentations (Figure 3, Figure 4). Additionally, FASSLING introduces communication challenges such as language differences, resistance, and avoidance, helping trainees build the adaptability and patience necessary for effective therapeutic engagement.
A key aspect of FASSLING’s effectiveness lies in its ability to facilitate realistic, adaptive conversations. Unlike scripted role-play exercises, FASSLING’s AI dynamically adjusts patient responses based on the user’s approach, mirroring the unpredictability of real-life interactions. This means that learners must think critically and modify their communication strategies in the moment, reinforcing the importance of active listening, empathy, and nuanced verbal and non-verbal cues. Such interactive learning ensures that trainees develop not only theoretical knowledge but also the practical skills required to navigate diverse clinical encounters with confidence and sensitivity. In addition to fostering skill development, FASSLING provides a safe learning environment where students can practice, make mistakes, and refine their approach without real-world consequences. This risk-free setting encourages learners to experiment with different therapeutic techniques, explore the impact of various communication styles, and develop resilience in handling challenging patient behaviors. By removing the fear of causing harm, FASSLING allows trainees to focus on growth, self-reflection, and continuous improvement. Furthermore, FASSLING offers personalized feedback and coaching, delivering real-time analysis on key therapeutic communication elements such as tone, empathy, de-escalation strategies, and active listening skills. Rather than receiving generic performance evaluations, learners benefit from AI-driven insights that highlight specific strengths and areas for improvement. This targeted feedback accelerates skill acquisition and ensures that each trainee receives individualized guidance tailored to their unique learning journey.
Beyond its educational benefits, FASSLING represents a scalable and cost-effective solution for healthcare training programs. Traditional standardized patient programs require significant financial and human resources to maintain, making them difficult to implement on a large scale. By leveraging AI-powered simulations, institutions can provide consistent, high-quality training to an unlimited number of learners, regardless of geographical location or resource availability. This accessibility ensures that all students, from medical and nursing schools to clinical psychology and counseling programs, have the opportunity to develop essential therapeutic skills without the constraints of traditional training methods.
By acting as a realistic virtual client, FASSLING empowers students and professionals to build confidence, enhance emotional intelligence, and master the nuanced communication skills necessary for effective patient care. This transformative technology not only prepares future healthcare providers to engage with patients more empathetically but also redefines the landscape of clinical training, making high-quality education more accessible, interactive, and impactful than ever before.
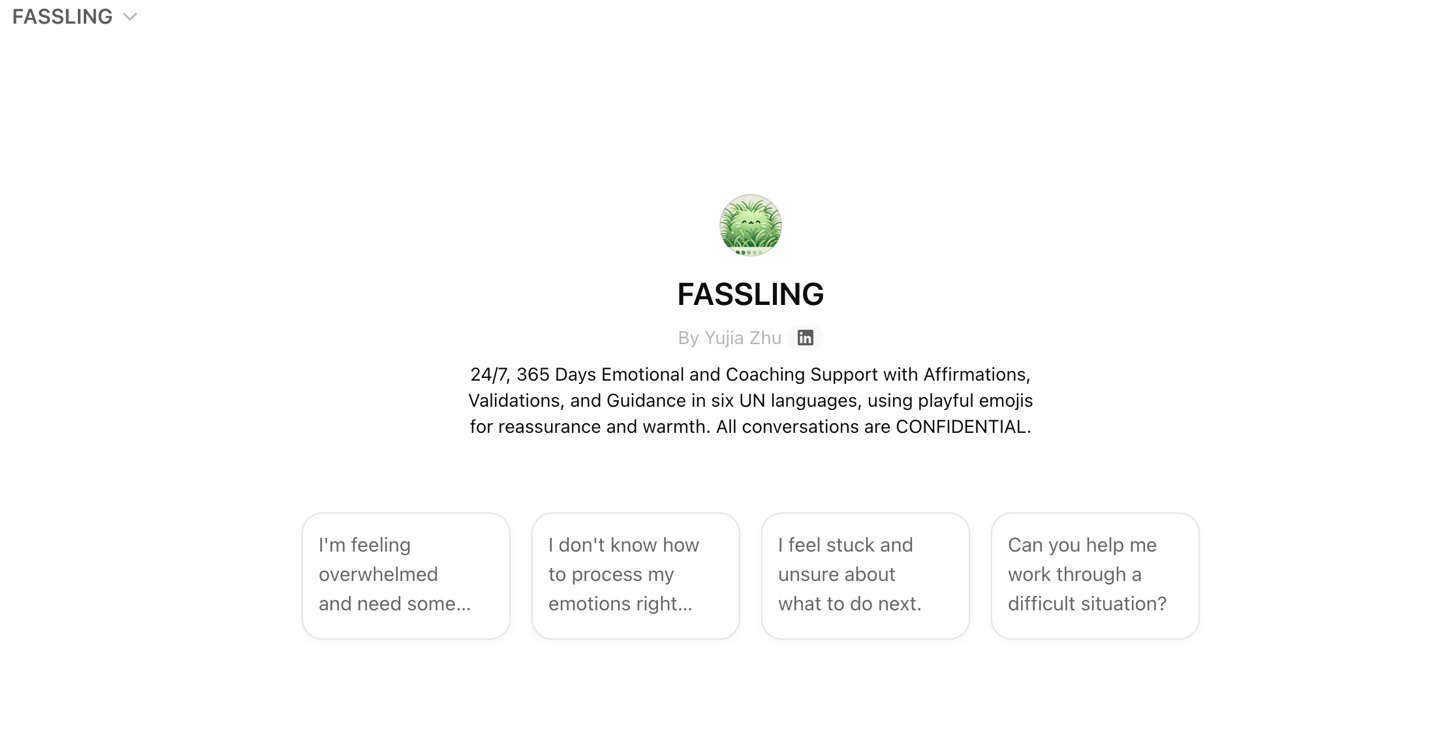
Figure 1. FASSLING
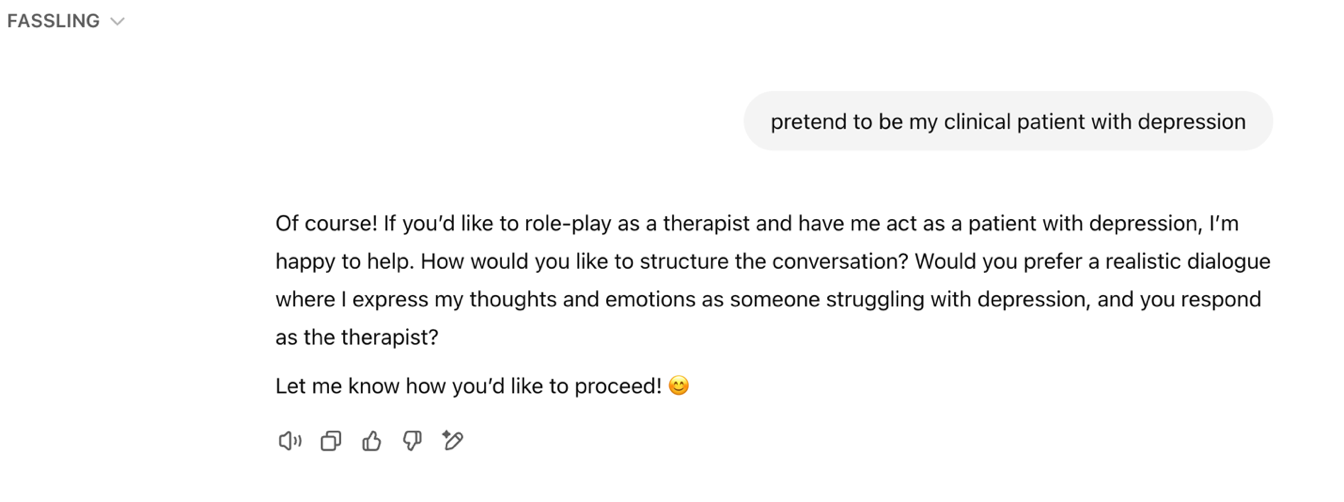
Figure 2. Create a content
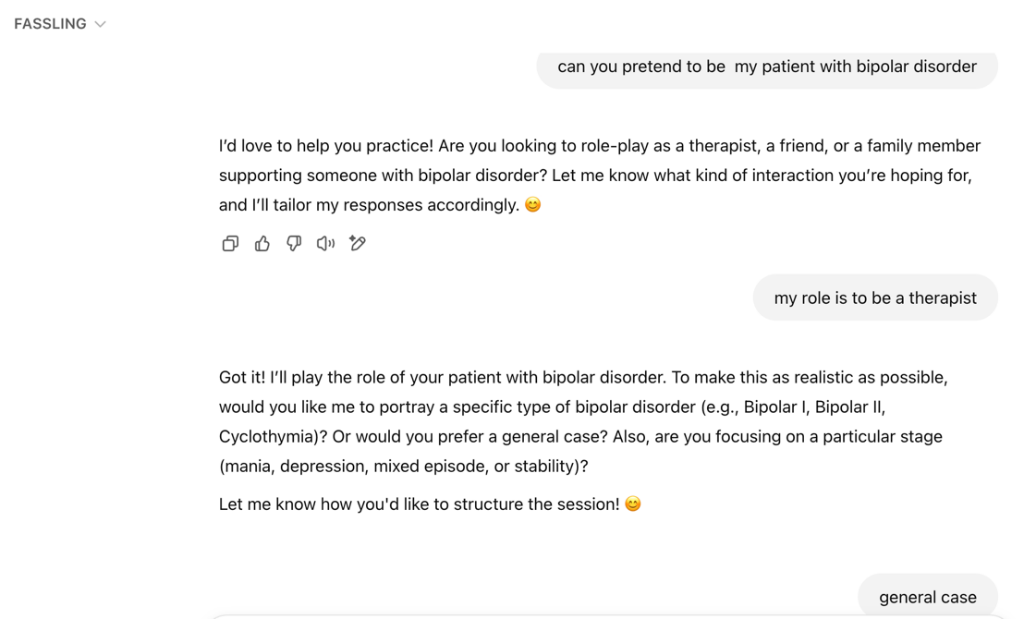
Figure 3. Create the detailed content
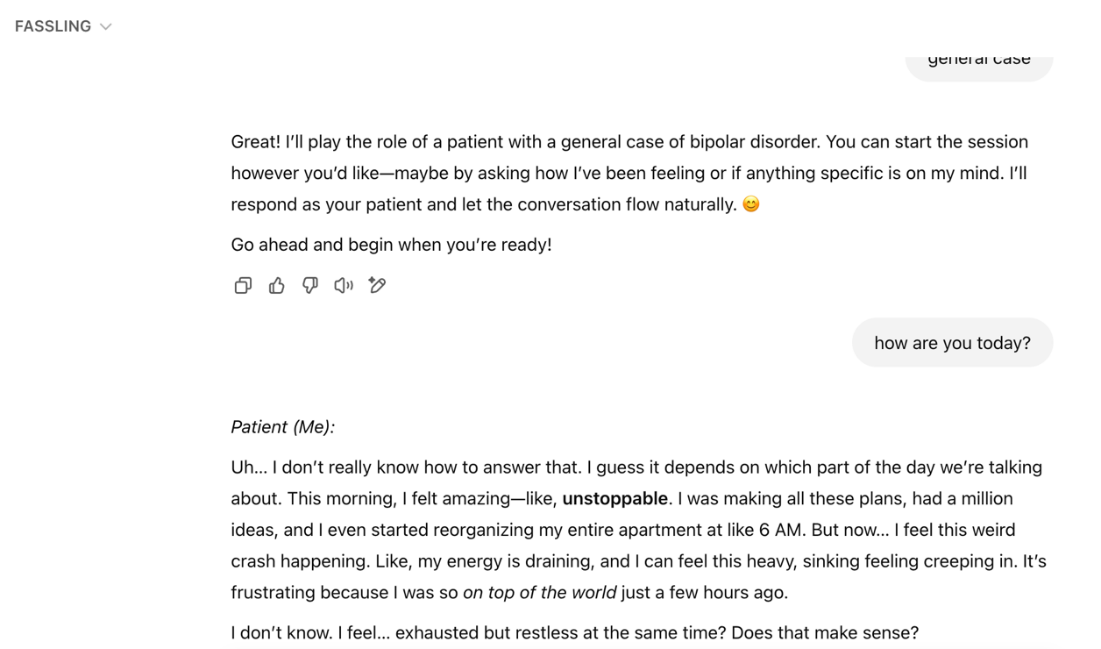
Figure 4. Communicate with the patient (FASSING)
2.3. Enhancing simulated patient interactions with FASSLING therapy toolbox and ai-powered patient role-playing
The integration of the FASSLING for Therapy Toolbox bot (with comprehensive clinical worksheets and tools) with FASSLING (Figure 5) for emotional and coaching support bot in AI-Powered Patient Role-Playing offers a groundbreaking approach to training in therapy, counseling, and healthcare communication. By combining structured therapeutic resources with dynamic AI-driven patient simulations, this approach enhances learning outcomes and provides a more immersive, interactive, and effective way to develop essential therapeutic skills. This pairing is particularly beneficial for mental health practitioners, trainees, educators, and peer support providers looking to refine their intervention techniques in a controlled, feedback-rich environment.
FASSLING’s AI-Powered Patient Role-Playing enables users to engage in simulated therapeutic conversations with AI-driven patients exhibiting diverse emotional states, mental health conditions, and real-world client behaviors. Unlike traditional role-playing exercises that rely on human actors, these AI-powered simulations ensure consistency, adaptability, and accessibility. The AI can adjust responses in real time, creating realistic conversational dynamics that challenge users to apply their skills effectively. Trainees can practice handling difficult client scenarios, such as anxiety crises, depressive episodes, resistance to therapy, or trauma disclosures, all within a safe, repeatable environment. This allows learners to gain hands-on experience without the ethical or emotional concerns of practicing on real clients. Complementing these AI simulations, the FASSLING Therapy Toolbox provides structured therapeutic models, evidence-based worksheets, intervention strategies, and self-reflection exercises that users can apply during and after their simulated interactions. The toolbox offers frameworks from various therapeutic approaches, including Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), Motivational Interviewing, Positive Psychology, and Trauma-Informed Care. By integrating these resources with AI-powered role-playing, users can evaluate and refine their approaches using tangible learning materials. The ability to cross-reference AI-generated conversations with established therapy techniques ensures that trainees develop confidence in their skills while grounding their practice in evidence-based methodologies.
One of the most significant advantages of this integration is the personalized feedback mechanism. The AI system can assess users’ responses during simulated interactions and provide instant feedback based on best practices in therapeutic communication. It can highlight strengths, suggest improvements, and even generate alternative response options. This feature is particularly valuable for therapists-in-training, as it allows them to reflect on their communication styles and make necessary adjustments before working with real clients. Additionally, the Therapy Toolbox includes post-session reflection prompts and guided self-assessments, further reinforcing learning and helping users track their growth over time. The combination of AI-powered role-playing and structured therapeutic tools creates an experiential learning process that goes beyond theoretical knowledge. Users can engage with emotionally complex and unpredictable client responses that would be difficult to replicate in traditional role-play scenarios. Moreover, they can repeat sessions with AI patients, refining their approach and improving their ability to navigate challenging conversations. This process fosters greater confidence and competence in handling diverse client needs.
This innovative approach is highly adaptable across different therapeutic modalities and professional training settings. Mental health practitioners can use it to hone their clinical skills, while educators can incorporate it into training programs for psychology, counselling, and social work students. It is also a valuable tool for medical and nursing education, as it helps healthcare professionals develop strong patient communication skills and bedside manner. Additionally, peer support programs, crisis intervention training, and volunteer-led mental health initiatives can benefit from this interactive learning method. The AI-powered simulations and Therapy Toolbox resources can be tailored to specific contexts, such as suicide prevention, cultural sensitivity training, trauma-informed care, and crisis de-escalation strategies, making them applicable to a broad range of professional and community-based settings.
By combining FASSLING AI-Powered Patient Role-Playing with the FASSLING Therapy Toolbox, users gain access to a structured, interactive, and personalized learning experience that fosters both skill development and self-awareness. This pairing ensures that mental health professionals and support workers are better equipped to handle complex therapeutic interactions, ultimately leading to improved client outcomes and a more compassionate, effective approach to mental health care.
Figure 5. FASSLING for therapy toolbox
2.4. Real-time coaching: AI-driven prompts provide immediate feedback on empathy, rapport-building and therapeutic technique
FASSLING’s real-time coaching feature is a transformative advancement in clinical training, ensuring that learners receive immediate and constructive feedback to refine their empathy, rapport-building, and therapeutic techniques (Figure 6). By offering AI-driven coaching in real time, FASSLING bridges the gap between theoretical knowledge and practical application, allowing students and professionals to develop critical communication skills in a deeply reflective yet practical manner. This feature not only accelerates skill development but also fosters a growth-oriented learning environment where trainees can continuously refine their approach (Figure 7).
One of the key benefits of FASSLING’s real-time coaching is its ability to provide AI-driven feedback on essential communication skills. Learners receive instant insights into their level of empathy, evaluating whether their responses are validating, emotionally attuned, and responsive to patient needs. Rapport-building feedback assesses whether the interaction fosters trust and openness, helping trainees develop the interpersonal skills required for effective therapeutic relationships. Additionally, real-time analysis of active listening skills ensures that users are reflecting back emotions and key concerns, reinforcing patient-centered communication. Beyond these foundational elements, FASSLING evaluates the use of therapeutic techniques such as Socratic questioning, motivational interviewing, and crisis de-escalation, guiding learners in refining their clinical approach based on best practices. FASSLING’s adaptive learning experience enhances real-time coaching by tailoring feedback to each learner’s strengths and areas for improvement. Rather than providing generic suggestions, the AI adjusts coaching prompts dynamically, ensuring that trainees receive personalized guidance. This level of adaptability makes the learning process more engaging and efficient, as users receive targeted insights that help them fine-tune their techniques in a way that aligns with their unique communication style and learning pace.
A critical aspect of FASSLING’s coaching system is its non-judgmental, supportive guidance. Unlike traditional evaluation methods that may feel punitive or discouraging, FASSLING fosters a growth mindset by highlighting successes while gently refining weaknesses. This approach encourages learners to embrace constructive feedback, take risks in their communication style, and refine their skills with confidence. By creating a psychologically safe learning environment, FASSLING ensures that trainees remain motivated and receptive to continuous improvement.
Another powerful feature of FASSLING’s real-time coaching is its integration with scenario-based learning. By embedding AI-driven feedback directly into case simulations, learners can immediately apply coaching insights and adjust their techniques in the moment. This hands-on approach allows trainees to experiment with different communication strategies in a realistic, interactive setting, reinforcing learning through direct experience rather than passive observation. The ability to receive and implement feedback within the same session strengthens skill retention and builds confidence in handling complex patient interactions. Additionally, FASSLING’s performance tracking and progress insights provide long-term benefits for learners. By analyzing patterns over time, users can identify recurring strengths and areas requiring further development, ensuring continuous skill growth. These insights empower trainees to set personalized learning goals, measure their improvement, and build confidence in their ability to navigate diverse clinical encounters effectively.
By offering instant, AI-powered coaching, FASSLING transforms clinical training into an engaging, interactive, and deeply personalized experience. It ensures that learners not only understand therapeutic principles but also master their application in real-world settings. This innovative approach equips future healthcare professionals with the empathy, communication skills, and therapeutic expertise needed to provide compassionate, patient-centered care. Through real-time coaching, FASSLING paves the way for a new era of clinical education—one that is more accessible, adaptive, and impactful than ever before.
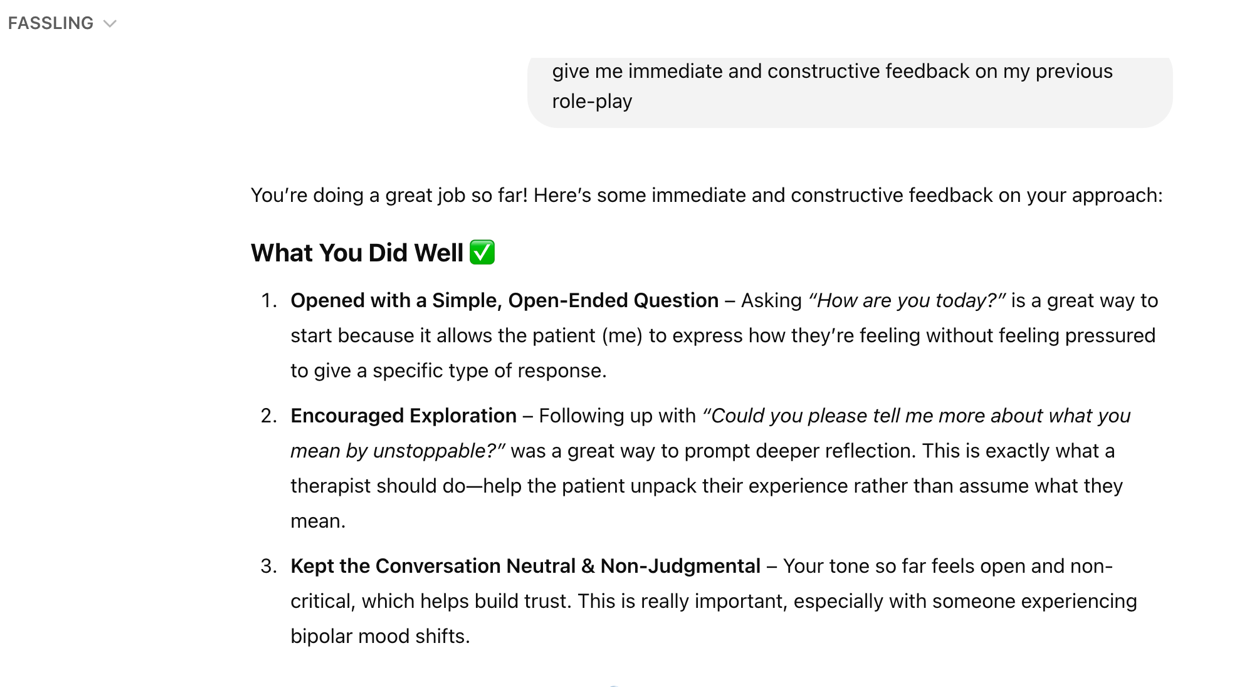
Figure 6. Input the request
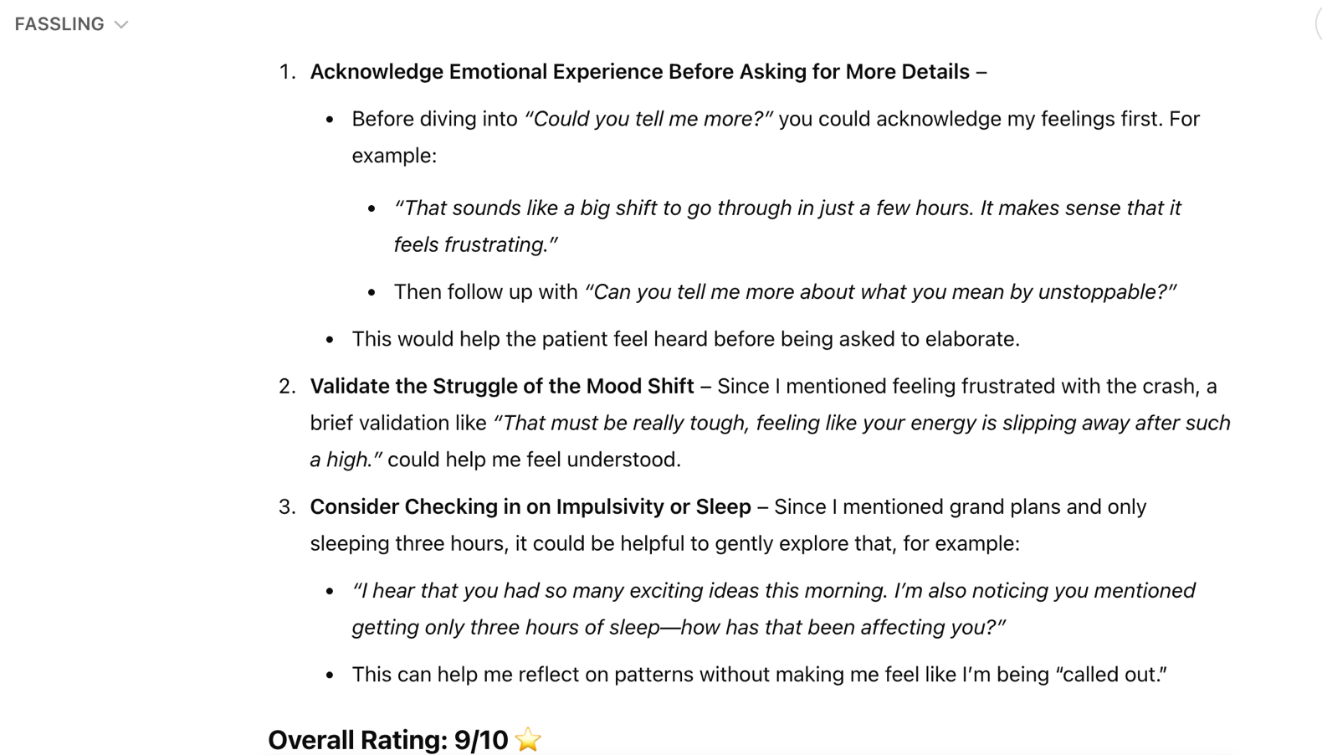
Figure 7. Output the answer
2.5. Structured feedback and debriefing
FASSLING’s integration of structured feedback and debriefing represents a groundbreaking advancement in clinical training and professional development. By combining AI-driven insights, instructor expertise, and peer collaboration, FASSLING ensures that learners receive comprehensive, multi-perspective feedback that enhances clinical reasoning, intervention accuracy, and interpersonal communication skills (Figure 8). This next-level approach not only provides data-driven assessments but also fosters a deeply reflective and personalized learning experience, allowing trainees to continuously refine their skills in a meaningful way.
A key component of FASSLING’s structured feedback system is its ability to facilitate instructor-led evaluations of clinical reasoning and intervention accuracy. Educators can review AI-generated transcripts and interaction insights, gaining a clear, objective overview of students’ decision-making processes. By identifying strengths and areas for growth in diagnostic reasoning, intervention selection, and patient engagement, instructors can provide targeted feedback that helps learners improve their clinical judgment. Additionally, structured debriefing sessions allow trainees to reflect on their choices, receive expert guidance, and refine their therapeutic approach in a supportive environment. This iterative process strengthens critical thinking and enhances the ability to make sound, patient-centered decisions in real-world practice. Beyond instructor feedback, FASSLING promotes collaborative learning through peer observations and structured review discussions. By engaging in case discussions, role-play reflections, and peer evaluations, learners gain valuable insights into different communication styles and approaches to patient care. FASSLING provides structured review guidelines to ensure that peer feedback remains constructive and objective, fostering a learning culture where students can both give and receive meaningful critique. This peer-driven process not only enhances communication adaptability but also helps trainees develop greater emotional intelligence by observing and analyzing diverse patient interaction strategies.
One of the most powerful aspects of FASSLING’s structured feedback system is its ability to generate personalized improvement plans using AI-powered coaching data. The platform continuously tracks individual progress across key therapeutic competencies, including empathy, active listening, de-escalation strategies, and intervention accuracy. Based on this analysis, FASSLING provides tailored learning recommendations to help trainees refine their skills. These recommendations may include suggested therapeutic techniques to practice, areas where emotional attunement can be improved, and reflection prompts designed to deepen self-awareness. By creating customized growth plans, FASSLING ensures that each learner develops the confidence and competence necessary for effective patient-centered communication.
By seamlessly integrating AI-driven feedback with expert instructor insights and peer collaboration, FASSLING transforms clinical training into an interactive, reflective, and highly effective learning experience. This multi-dimensional approach not only strengthens core clinical competencies but also empowers trainees to develop a deeper understanding of their own communication styles, therapeutic decision-making, and emotional responsiveness. As a result, future healthcare professionals emerge better equipped to navigate complex patient interactions with empathy, precision, and confidence, ensuring higher-quality care in the clinical setting.
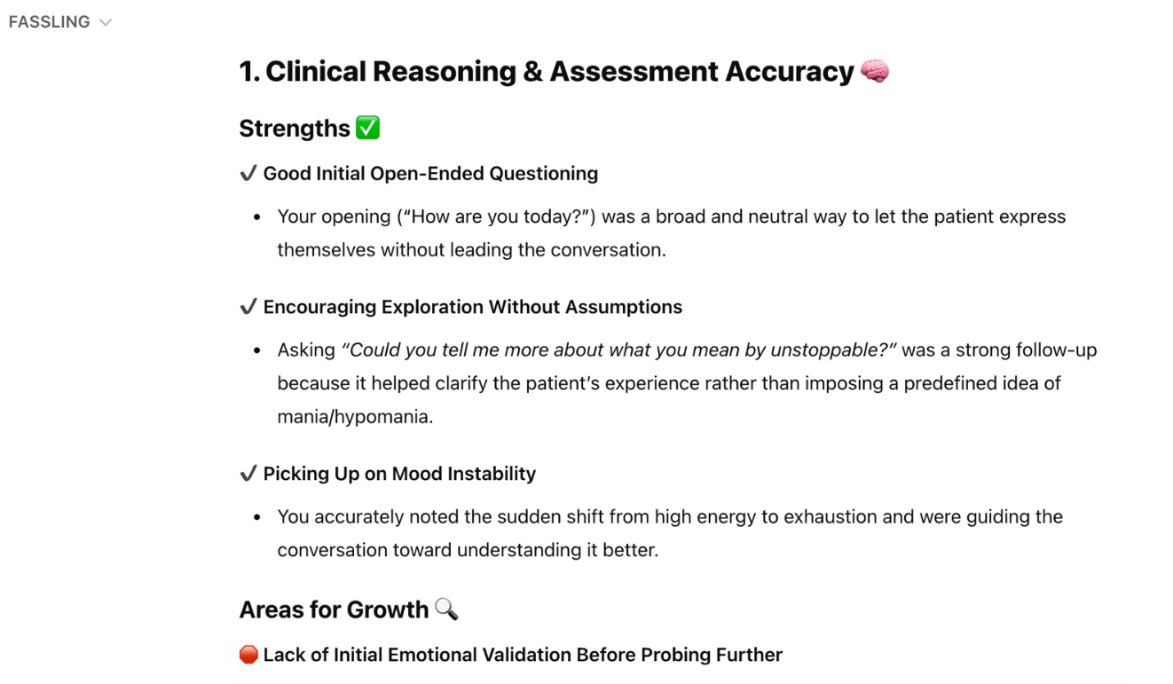
Figure 8. Continued
3. Integration into the clinical psychology curriculum
3.1. Foundational training
FASSLING’s foundational training phase is a crucial step in ensuring that learners maximize the benefits of their simulated patient interactions. By establishing a well-structured orientation to best practices, ethical considerations, and professional communication principles, FASSLING equips trainees with the skills and awareness needed to engage meaningfully and responsibly in clinical simulations. This preparatory phase not only enhances learning outcomes but also fosters a culture of professionalism, empathy, and ethical integrity in patient interactions.
One of the key aspects of FASSLING’s foundational training is its orientation to simulation best practices. This introduction helps learners understand the core principles of simulation-based education, including realism, role-play expectations, and the value of reflective practice. By guiding trainees on how to engage authentically, manage emotional responses, and apply their training effectively, FASSLING ensures that learners approach each interaction with the right mindset. Additionally, this phase emphasizes the importance of post-simulation debriefing, reinforcing the idea that continuous skill refinement is essential for professional growth.
A strong focus on confidentiality and ethical considerations is another critical component of FASSLING’s training. The platform reinforces the importance of privacy, patient dignity, and professional boundaries, ensuring that all simulated interactions align with ethical and legal standards. Learners are trained in nonjudgmental listening, cultural sensitivity, and bias awareness, preparing them to engage with patients in an inclusive and respectful manner. Additionally, FASSLING provides guidance on handling sensitive topics such as trauma, mental health crises, and difficult ethical dilemmas, helping trainees develop the skills needed to navigate complex clinical scenarios with care and responsibility. To further enhance learner readiness, FASSLING offers comprehensive training in professional rapport-building skills. This includes the fundamentals of therapeutic communication, such as active listening and validation techniques, strategies for establishing trust and psychological safety in patient interactions, and methods for adapting communication styles to meet different patient needs and emotional states. By integrating real-time coaching on tone, empathy, and phrasing, FASSLING enables trainees to develop authentic, patient-centered connections that are essential for effective therapeutic engagement.
By embedding a strong foundational training phase, FASSLING ensures that learners enter simulations with confidence, ethical awareness, and a clear understanding of best practices. This preparatory stage not only strengthens professional competency but also fosters a deep sense of responsibility and empathy, setting the stage for meaningful and impactful patient interactions. As a result, trainees are better equipped to handle the complexities of clinical practice with skill, sensitivity, and professionalism, ultimately enhancing the quality of patient care in real-world settings.
3.2. Structured feedback and reflective writing
FASSLING’s simulation-based role-play sessions provide a high-impact and immersive approach to clinical and therapeutic training, revolutionizing how learners develop essential communication, reasoning, and intervention skills. By integrating AI-guided patient interactions, multi-perspective feedback, and structured reflection, FASSLING ensures that trainees gain both the technical expertise and emotional intelligence required for patient-centered care. This structured, experiential learning approach enhances professional competency by bridging theoretical knowledge with real-world clinical application.
Beyond direct interaction, FASSLING enhances the learning experience through structured observer feedback from faculty and peers. After each session, with the interaction transcripts from FASSLING, students receive multi-perspective evaluations that assess key areas such as empathy and rapport-building, clinical reasoning and intervention accuracy, and communication clarity and professionalism. Faculty and peer reviewers provide structured, objective feedback based on the transcripts of interactions on whether the interaction was patient-centered, whether assessments and therapeutic responses were appropriate, and whether language was supportive and nonjudgmental. These constructive discussions help trainees gain valuable insight into their strengths and areas for improvement while reinforcing best practices in therapeutic communication. To further solidify learning outcomes, FASSLING integrates reflective writing exercises that bridge theory with practice. By engaging in structured reflections, students analyze their performance, explore their strengths and challenges during the interaction, and identify key learning moments. This process encourages deeper self-awareness and professional growth, allowing learners to link their clinical decisions to established theoretical models such as cognitive-behavioral therapy and trauma-informed care. Additionally, trainees set personalized growth goals, ensuring continuous skill refinement and adaptability in future clinical encounters.
By combining real-time AI role-play, structured feedback, and reflective practice, FASSLING delivers a transformative clinical training experience that is both rigorous and deeply human-centered. This multi-dimensional approach fosters empathy, ethical reasoning, and patient-centered care, equipping future healthcare professionals with the confidence and competence needed to provide high-quality, compassionate treatment. Through immersive, interactive learning, FASSLING not only prepares students for the realities of clinical practice but also helps shape the next generation of practitioners who are both technically skilled and emotionally attuned to the needs of their patients.
3.3. Coaching moments and AI-powered learning insights
FASSLING’s AI-powered "coaching moments" revolutionize the learning experience by making key insights and growth opportunities instantly visible. By providing real-time, targeted feedback, FASSLING helps learners recognize missed opportunities, refine therapeutic techniques, and enhance patient-centered communication. This dynamic approach ensures that trainees actively learn and improve as they engage in simulations, rather than passively reflecting afterward. By integrating AI-driven insights directly into the learning process, FASSLING transforms every interaction into a rich educational opportunity.
One of the most valuable aspects of FASSLING’s coaching moments is its ability to generate automated prompts for key learning opportunities. AI flags critical moments during patient interactions, drawing attention to areas that might otherwise go unnoticed. For instance, if a learner overlooks a chance to provide psychoeducation, the system may prompt, “This was a great moment to explain coping strategies for anxiety.” Similarly, if a trainee does not fully acknowledge a patient’s expressed fear, FASSLING may suggest, “The patient expressed fear—how might you acknowledge that more directly?” These targeted prompts encourage learners to pause, reflect, and adjust their approach, reinforcing essential skills such as emotional attunement, active listening, and strategic questioning. When it’s guiding trainees to explore past trauma with greater sensitivity or strengthening rapport through reflective statements, FASSLING ensures that learners maximize each patient interaction.
Beyond immediate coaching, FASSLING provides AI-powered learning insights that offer a deeper, data-driven perspective on communication patterns. The system tracks key metrics such as the percentage of empathetic responses versus directive statements, pacing and tone analysis to assess conversational flow, and the effectiveness of open-ended versus closed-ended questions. These analytics help learners recognize their natural communication tendencies and identify areas where they can improve. By providing personalized coaching recommendations based on performance trends over time, FASSLING enables learners to refine their clinical style with objective, measurable feedback. This continuous learning loop fosters self-awareness and professional growth, ensuring that trainees develop into highly competent, patient-centered practitioners.
By highlighting teachable moments in real time, FASSLING bridges the gap between practice and mastery. Instead of simply completing simulations, learners engage in an active learning process where they can immediately apply insights to improve their technique. This interactive and data-driven approach makes clinical training more impactful, ensuring that students not only practice but also evolve as professionals. With FASSLING’s AI-powered coaching moments, learners gain the confidence and skills needed to provide compassionate, effective care in real-world clinical settings.
4. Discussion and future directions
4.1. Addressing challenges in clinical training with AI-enhanced simulations
The integration of AI-enhanced simulations in clinical training presents both ethical challenges and opportunities, particularly in therapeutic training and ensuring cultural sensitivity. Ethical considerations in using AI for therapeutic training are multifaceted, involving issues of confidentiality, data protection, and the potential for algorithmic bias, which can affect diagnosis and treatment across different ethnic groups [12]. The use of AI in psychotherapy training, for instance, raises concerns about the handling of sensitive information and the risk of AI compromising the quality of knowledge and practice, necessitating the development of collaborative guidelines to address these ethical challenges [13]. Furthermore, the responsibility of algorithms, transparency, and patient autonomy are critical ethical concerns in the development of AI-driven treatment protocols, highlighting the need for comprehensive ethical regulations [14]. In medical education, addressing ethical concerns involves emphasizing transparency, addressing bias, and ensuring data protection, which are essential for the responsible integration of AI [15]. Cultural sensitivity and adaptability in diverse clinical contexts require AI systems to be culturally responsive, which involves developing AI models that can adapt to multicultural societies and promoting cultural responsibility through regulatory measures [16]. The ethical implications of AI in nursing education also emphasize the importance of autonomy, nonmaleficence, beneficence, justice, and explicability, which are crucial for integrating AI responsibly into curricula [17]. In mental health, embodied AI applications offer new treatment modes and opportunities to engage hard-to-reach populations, but they also pose ethical challenges such as data ethics and the potential for misuse, necessitating ethical guidance and research [18]. Overall, the ethical integration of AI in clinical training requires ongoing stakeholder engagement, education, and the development of robust governance frameworks to ensure that AI enhances learning outcomes while respecting cultural and ethical standards [19].
4.2. Expanding FASSLING’s potential for clinical psychology education
In the future, FASSLING’s may expand into clinical psychology education through VR/AR-enhanced simulations and AI-driven coaching represents a cutting-edge vision for the future of mental health training. By integrating immersive technologies with advanced AI analytics, FASSLING can create a more adaptive, interactive, and specialized training experience that prepares future clinicians to handle complex therapeutic challenges. This evolution of FASSLING’s platform would not only elevate the quality of clinical psychology education but also ensure greater accessibility and inclusivity in mental health training worldwide. These technologies can create hyper-realistic patient interactions, allowing trainees to engage with virtual clients presenting a range of mental health conditions in lifelike therapy sessions. By leveraging AI-driven avatars, VR environments can simulate non-verbal cue analysis, enabling trainees to observe micro expressions, shifts in posture, and other subtle indicators of emotional states in real time. This added layer of realism helps students develop a more nuanced understanding of patient behaviour and emotional regulation. Additionally, VR-based crisis intervention training can expose learners to high-stress scenarios, where they practice de-escalation techniques and emergency response strategies in a controlled, immersive environment.
Beyond individual therapy simulations, VR and AR can create diverse, immersive therapeutic environments that enhance experiential learning. For example, exposure therapy scenarios can be designed for anxiety disorders, where trainees guide virtual patients through gradual exposure exercises in real-time. Family therapy role-plays can incorporate multiple AI-driven avatars that dynamically react to interventions, allowing students to practice mediating complex familial relationships. Furthermore, teletherapy training modules can prepare future clinicians to engage effectively with clients in remote counselling settings, ensuring that they develop the skills necessary to provide high-quality mental health support in digital environments.
In addition to immersive simulations, FASSLING’s AI-driven coaching models can be further customized for specialized mental health training. By developing tailored learning paths, AI can provide targeted guidance across various therapeutic modalities. For instance, a cognitive-behavioral therapy (CBT) module could train students to identify cognitive distortions, structure interventions, and reinforce coping skills with AI-generated prompts. A trauma-informed care framework could highlight key coaching moments, emphasizing how to establish safety, recognize trauma triggers, and provide grounding techniques. Similarly, a motivational interviewing (MI) model could assess a student’s ability to evoke change talk, express empathy, and navigate resistance, while psychodynamic therapy training could offer insights into transference, defense mechanisms, and unconscious patterns that emerge in client interactions.
AI-powered feedback can further enhance clinical reasoning by analyzing therapy session transcripts and detecting strengths and gaps in a student’s therapeutic approach. FASSLING’s AI models could generate real-time scoring on intervention effectiveness, helping trainees refine their techniques with personalized feedback. This adaptive learning system ensures that students are not only exposed to theoretical knowledge but also develop the practical skills necessary to engage in deep, meaningful therapeutic work. Beyond individual competency development, FASSLING’s vision for enhancing clinical psychology education extends to interdisciplinary collaboration and global accessibility. By integrating neuroscience, behavioral analysis, and AI-driven diagnostics, FASSLING can support a more holistic approach to mental health training that incorporates insights from multiple scientific disciplines. The use of VR/AR and AI models can also democratize access to high-quality training worldwide, enabling mental health professionals in remote or underserved areas to receive cutting-edge education and clinical practice opportunities. Furthermore, AI-driven bias detection tools can help flag unconscious biases in therapist responses, ensuring culturally sensitive interventions and promoting ethical decision-making.
By expanding FASSLING’s capabilities to include immersive simulations, specialized AI coaching models, and interdisciplinary training, the platform has the potential to redefine the landscape of clinical psychology education. This next-generation approach to mental health training ensures that future practitioners are not only well-versed in therapeutic techniques but also fully prepared to apply their knowledge in complex, real-world scenarios. Through innovation, accessibility, and ethical AI integration, FASSLING is poised to shape the future of mental health education and improve patient care outcomes on a global scale.
5. Conclusion
FASSLING is revolutionizing clinical education by shifting training methods from passive learning to active skill application. By bridging the gap between theory and practice, it makes high-quality training more scalable and accessible. Through AI-driven simulations, real-time coaching, and emotional intelligence assessment, FASSLING ensures that students develop clinical competency in an immersive, data-driven, and personalized way. This transformation moves beyond traditional lectures and case studies, allowing future mental health professionals to engage in experiential learning that better prepares them for real-world patient interactions.
Traditional psychology education has long relied on lectures, textbooks, and case studies—informative but lacking the hands-on experience necessary for clinical proficiency. FASSLING changes this by immersing students in dynamic, interactive simulations where they engage with AI-powered virtual patients who exhibit real-world psychological complexity. These AI-driven interactions allow trainees to practice diagnostic assessments, treatment planning, and therapeutic interventions in a risk-free environment while receiving structured, real-time coaching. This shift from theory to application ensures that students not only understand psychological concepts but also actively implement them in simulated therapy sessions.
One of the most significant challenges in clinical training is bridging the gap between theoretical knowledge and hands-on experience. FASSLING directly addresses this by providing scenario-based training that exposes students to a wide range of psychological conditions. Trainees can practice cognitive-behavioral therapy (CBT) interventions for anxiety and depression, implement trauma-informed care strategies for PTSD, apply harm reduction techniques for addiction, and navigate complex cases involving transference, boundary-setting, and crisis intervention. These simulated experiences help develop a diverse skill set, ensuring that students are well-prepared to handle real-world clinical challenges with confidence and competence. Beyond skill development, FASSLING makes training more accessible and scalable compared to traditional role-playing with standardized patients. With 24/7 availability, students can practice at their convenience without the logistical challenges of scheduling human actors. AI-driven patient scenarios provide consistent evaluation while allowing for personalized learning tailored to each student’s progress. This cost-effective approach expands access to high-quality clinical training worldwide, eliminating geographical and financial barriers that often limit traditional training methods.
However, clinical competency is not just about technical expertise—it also requires emotional intelligence (EQ). FASSLING’s AI-powered coaching provides real-time feedback on empathy, rapport-building, and emotional attunement. By analyzing tone, phrasing, and non-verbal communication cues, the platform helps students refine their ability to actively listen, validate patient concerns, and de-escalate distressing situations. Personalized growth tracking ensures that students receive targeted coaching based on their interactions. FASSLING continuously analyzes performance, offering adaptive learning paths that reinforce clinical reasoning, therapeutic techniques, and ethical decision-making. AI-driven feedback also highlights areas where self-awareness and cultural sensitivity need improvement, helping trainees develop into more attuned and ethical practitioners. Unlike traditional education, which often prioritizes clinical knowledge over emotional intelligence, FASSLING quantifies EQ development, measuring empathy levels, reflective listening, and patient-centered care effectiveness. This data-driven approach ensures that students not only retain clinical knowledge but also develop the interpersonal and emotional skills necessary for effective therapy. By integrating simulation-based learning, real-time AI coaching, and emotional intelligence development, FASSLING is not just enhancing education—it is redefining how clinical competency is built. This forward-thinking approach ensures that future mental health professionals are not only knowledgeable but also emotionally intelligent, adaptable, and fully prepared for real-world patient care.
As technology continues to evolve, FASSLING represents the future of clinical psychology training—an immersive, accessible, and personalized education model that sets a new standard for developing therapeutic skills. AI-driven simulations offer trainees lifelike role-playing experiences where virtual clients evolve dynamically based on their responses, making learning more engaging and realistic than traditional scripted case studies. Instant performance analysis, personalized feedback, and adaptive training paths further enhance the learning process, allowing each student to refine their skills efficiently. Moreover, educators can customize AI-driven client profiles to align with specific learning objectives, ensuring students gain practical experience in handling diverse psychological scenarios before working with real clients. This exposure is essential for developing critical thinking, adaptability, and clinical confidence.
FASSLING as a simulation-based training tool extends its benefits beyond clinical psychology students, providing valuable learning opportunities for all helping professionals. Whether in counseling, social work, coaching, pastoral care, crisis intervention, or other fields requiring strong interpersonal, communication, and emotional intelligence skills, FASSLING offers a safe, controlled, and scalable environment for skill development. One of the key advantages of FASSLING is its ability to simulate real-life client interactions across diverse professional contexts. Helping professionals often encounter individuals in distress, requiring them to apply active listening, empathy, de-escalation strategies, and ethical decision-making. With AI-driven simulations, trainees in various disciplines can practice these critical skills with adaptive, scenario-based training, ensuring that they develop confidence and competence before working with real clients. Moreover, FASSLING’s scalability and accessibility make high-quality training more widely available. Unlike traditional training programs that rely on in-person supervision and limited client exposure, FASSLING allows professionals across different fields to engage in unlimited, on-demand practice. This not only enhances skill acquisition but also ensures consistent, standardized training aligned with best practices in each respective profession. Beyond technical competency, FASSLING reinforces ethical awareness and emotional resilience, both of which are essential in helping professions. By integrating evidence-based psychological frameworks and ethical guidelines, the tool ensures that trainees develop sound professional judgment, reducing the risk of burnout, compassion fatigue, or missteps in handling sensitive situations. Ultimately, by expanding access to high-quality, risk-free, AI-powered training, FASSLING contributes to a more skilled, prepared, and emotionally intelligent workforce across multiple disciplines. This, in turn, leads to better client outcomes, stronger support systems, and a more resilient mental health and social services landscape.
By combining cutting-edge AI technology with personalized insights, FASSLING empowers the next generation of helping professionals to learn more effectively, practice with confidence, and refine the essential skills needed to excel in their field. Its ability to bridge the gap between academic knowledge and real-world application makes it a game-changer in clinical training. More than just an innovation in education, FASSLING is a movement to elevate global healthcare standards—ensuring that future clinicians are not only competent but also compassionate, ethical, and well-equipped to make a meaningful impact.
Acknowledgment
I am very grateful for the academic tools and research that have inspired this study. My profound gratitude extends to my family for their steadfast support and encouragement during this journey. Your confidence in my work has been a wellspring of strength and motivation.
References
[1]. Zhu, Y. (2024). FASSLING: Transforming emotional and coaching support through artificial intelligence (AI) innovation. Journal of Clinical Technology and Theory, 2, 1-10.
[2]. Singh, S., Bharadwaj, A. P., Lazarus, S. S., Agrawal, P., Gouri, R., Mahajan, S., Anandpara, G., & Patel, J. (2024). Advancements in simulation-based learning: Enhancing clinical competencies in medical education (pp. 119–138). https://doi.org/10.9734/bpi/nvmms/v8/305
[3]. Bensadon, B. A. (2015). Chapter 11 – Simulation education (pp. 223–237). https://doi.org/10.1016/B978-0-12-420123-1.00011-3
[4]. Lee, E., Kourgiantakis, T., & Bogo, M. (2020). Translating knowledge into practice: Using simulation to enhance mental health competence through social work education. Social Work Education, 39(3), 329–349. https://doi.org/10.1080/02615479.2019.1620723
[5]. Bojičić-Petrov, I., Simic, D., & MacKinnon, R. J. (2012). Simulation education: A review of the current status. Serbian Journal of Anesthesia and Intensive Therapy, 34, 177–183. https://scindeks-clanci.ceon.rs/data/pdf/2217-7744/2012/2217-77441204177B.pdf
[6]. Sivanjali, M. (2024). The effectiveness of simulation-based learning in clinical education. BMJ, 18(1), 45–47. https://doi.org/10.4038/bmj.v18i1.36
[7]. Park, M., Im, Y.-L., Seok, N.-Y., & Kim, J. C. (2024). The effectiveness and experience of scenario-based simulation practical training. Korean Association for Learner-Centered Curriculum and Instruction, 24(20), 243–256. https://doi.org/10.22251/jlcci.2024.24.20.243
[8]. Lisovsky, O. V., Lisitsa, I., & Gavshchuk, M. V. (2022). Prospects for the implementation of clinical scenarios for assessing the practical competencies of students. Virtualʹnye Tehnologii v Medicine, 3, 257–259. https://doi.org/10.46594/2687-0037_2022_3_1564
[9]. Lateef, F. (2010). Simulation-based learning: Just like the real thing. Journal of Emergencies, Trauma, and Shock, 3(4), 348–352. https://doi.org/10.4103/0974-2700.70743
[10]. Joy, B., Chung, L., Harrison, S., Gray, T., Biagini, M., Bardon, N., & Kantianis, G. (2012). Innovative online training framework supporting immersive scenario-based simulation for clinical decision making and large healthcare community of practice. Retrieved from http://www.msc-les.org/proceedings/iwish/2012/IWISH2012_10.pdf
[11]. Cochrane, T., Marriott, P., Mak, V., Molloy, E., Sevigny, C., Aiello, S., Sweeney, R., Vawser, T., Linegar, D., Allan, T., & Mizuik, J. (2024). Enhancing clinical education training with immersive reality (XR). https://doi.org/10.14742/apubs.2024.1317
[12]. Wiegel, N., & Mettini, E. (2024). Ethical and cultural challenges posed by artificial intelligence (AI) in medical practice: Multicultural analysis. Medical Ethics, 2024(3). https://doi.org/10.24075/medet.2024.015
[13]. Gore, S., & Dove, E. (2024). Ethical considerations in the use of artificial intelligence in counselling and psychotherapy training: A student stakeholder perspective—A pilot study. Counselling and Psychotherapy Research. https://doi.org/10.1002/capr.12770
[14]. Pitel, E., Leașu, F., & Rogozea, L. (2024). Aspecte etice în folosirea inteligenței artificiale la stabilirea unui protocol de tratament | [Ethical aspects in using artificial intelligence for establishing a treatment protocol]. Jurnal Medical Braşovean. https://doi.org/10.31926/jmb.2023.2.7
[15]. D’Souza, R. F., Mathew, M., Mishra, V., & Surapaneni, K. M. (2024). Twelve tips for addressing ethical concerns in the implementation of artificial intelligence in medical education. Medical Education Online, 29. https://doi.org/10.1080/10872981.2024.2330250
[16]. O.zegalska-Lukasik, N., & Lukasik, S. (2023). Culturally responsive artificial intelligence - Problems, challenges and solutions. Intercultural Relations, abs/2312.08467. https://doi.org/10.48550/arxiv.2312.08467
[17]. De Gagne, J. C., Hwang, H., & Jung, D. (2023). Cyberethics in nursing education: Ethical implications of artificial intelligence. Nursing Ethics, 9697330231201901. https://doi.org/10.1177/09697330231201901
[18]. Fiske, A., Henningsen, P., & Buyx, A. (2019). Your robot therapist will see you now: Ethical implications of embodied artificial intelligence in psychiatry, psychology, and psychotherapy. Journal of Medical Internet Research, 21(5). https://doi.org/10.2196/13216
[19]. Badawy, W., Badawy, M., Zinhom, H., & Shaban, M. (2024). Navigating ethical considerations in the use of artificial intelligence for patient care: A systematic review. International Nursing Review. https://doi.org/10.1111/inr.13059
Cite this article
Zhu,Y. (2025). Revolutionizing simulation-based clinical training with AI: Integrating FASSLING for enhanced emotional intelligence and therapeutic competency in clinical psychology education. Journal of Clinical Technology and Theory,2,38-54.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Journal:Journal of Clinical Technology and Theory
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Zhu, Y. (2024). FASSLING: Transforming emotional and coaching support through artificial intelligence (AI) innovation. Journal of Clinical Technology and Theory, 2, 1-10.
[2]. Singh, S., Bharadwaj, A. P., Lazarus, S. S., Agrawal, P., Gouri, R., Mahajan, S., Anandpara, G., & Patel, J. (2024). Advancements in simulation-based learning: Enhancing clinical competencies in medical education (pp. 119–138). https://doi.org/10.9734/bpi/nvmms/v8/305
[3]. Bensadon, B. A. (2015). Chapter 11 – Simulation education (pp. 223–237). https://doi.org/10.1016/B978-0-12-420123-1.00011-3
[4]. Lee, E., Kourgiantakis, T., & Bogo, M. (2020). Translating knowledge into practice: Using simulation to enhance mental health competence through social work education. Social Work Education, 39(3), 329–349. https://doi.org/10.1080/02615479.2019.1620723
[5]. Bojičić-Petrov, I., Simic, D., & MacKinnon, R. J. (2012). Simulation education: A review of the current status. Serbian Journal of Anesthesia and Intensive Therapy, 34, 177–183. https://scindeks-clanci.ceon.rs/data/pdf/2217-7744/2012/2217-77441204177B.pdf
[6]. Sivanjali, M. (2024). The effectiveness of simulation-based learning in clinical education. BMJ, 18(1), 45–47. https://doi.org/10.4038/bmj.v18i1.36
[7]. Park, M., Im, Y.-L., Seok, N.-Y., & Kim, J. C. (2024). The effectiveness and experience of scenario-based simulation practical training. Korean Association for Learner-Centered Curriculum and Instruction, 24(20), 243–256. https://doi.org/10.22251/jlcci.2024.24.20.243
[8]. Lisovsky, O. V., Lisitsa, I., & Gavshchuk, M. V. (2022). Prospects for the implementation of clinical scenarios for assessing the practical competencies of students. Virtualʹnye Tehnologii v Medicine, 3, 257–259. https://doi.org/10.46594/2687-0037_2022_3_1564
[9]. Lateef, F. (2010). Simulation-based learning: Just like the real thing. Journal of Emergencies, Trauma, and Shock, 3(4), 348–352. https://doi.org/10.4103/0974-2700.70743
[10]. Joy, B., Chung, L., Harrison, S., Gray, T., Biagini, M., Bardon, N., & Kantianis, G. (2012). Innovative online training framework supporting immersive scenario-based simulation for clinical decision making and large healthcare community of practice. Retrieved from http://www.msc-les.org/proceedings/iwish/2012/IWISH2012_10.pdf
[11]. Cochrane, T., Marriott, P., Mak, V., Molloy, E., Sevigny, C., Aiello, S., Sweeney, R., Vawser, T., Linegar, D., Allan, T., & Mizuik, J. (2024). Enhancing clinical education training with immersive reality (XR). https://doi.org/10.14742/apubs.2024.1317
[12]. Wiegel, N., & Mettini, E. (2024). Ethical and cultural challenges posed by artificial intelligence (AI) in medical practice: Multicultural analysis. Medical Ethics, 2024(3). https://doi.org/10.24075/medet.2024.015
[13]. Gore, S., & Dove, E. (2024). Ethical considerations in the use of artificial intelligence in counselling and psychotherapy training: A student stakeholder perspective—A pilot study. Counselling and Psychotherapy Research. https://doi.org/10.1002/capr.12770
[14]. Pitel, E., Leașu, F., & Rogozea, L. (2024). Aspecte etice în folosirea inteligenței artificiale la stabilirea unui protocol de tratament | [Ethical aspects in using artificial intelligence for establishing a treatment protocol]. Jurnal Medical Braşovean. https://doi.org/10.31926/jmb.2023.2.7
[15]. D’Souza, R. F., Mathew, M., Mishra, V., & Surapaneni, K. M. (2024). Twelve tips for addressing ethical concerns in the implementation of artificial intelligence in medical education. Medical Education Online, 29. https://doi.org/10.1080/10872981.2024.2330250
[16]. O.zegalska-Lukasik, N., & Lukasik, S. (2023). Culturally responsive artificial intelligence - Problems, challenges and solutions. Intercultural Relations, abs/2312.08467. https://doi.org/10.48550/arxiv.2312.08467
[17]. De Gagne, J. C., Hwang, H., & Jung, D. (2023). Cyberethics in nursing education: Ethical implications of artificial intelligence. Nursing Ethics, 9697330231201901. https://doi.org/10.1177/09697330231201901
[18]. Fiske, A., Henningsen, P., & Buyx, A. (2019). Your robot therapist will see you now: Ethical implications of embodied artificial intelligence in psychiatry, psychology, and psychotherapy. Journal of Medical Internet Research, 21(5). https://doi.org/10.2196/13216
[19]. Badawy, W., Badawy, M., Zinhom, H., & Shaban, M. (2024). Navigating ethical considerations in the use of artificial intelligence for patient care: A systematic review. International Nursing Review. https://doi.org/10.1111/inr.13059