1. Introduction
Virtual Reality (VR) refers to the use of computer technology to create simulated environments that users can interact with in a seemingly real or physical way. It leverages immersive, three-dimensional (3D) environments with sensory feedback, including visual, auditory, and sometimes haptic stimuli, allowing users to feel as if they are part of a virtual world [1]. The ability to simulate real-life scenarios, coupled with high levels of interactivity and immersion, has made VR a valuable tool in various industries, including healthcare, education, gaming, and entertainment.
In the medical field, VR is revolutionizing the way healthcare professionals are trained, how surgeries are planned and rehearsed, and how psychological treatments are administered. Traditionally, medical education has relied heavily on textbooks, cadavers, and clinical rotations. [2]While effective, these methods often lack the depth and flexibility needed to fully train students in complex medical procedures or rare conditions. VR addresses this gap by enabling students to repetitively practice procedures in simulated environments, offering a more effective and risk-free learning experience [3]. Similarly, in surgery, VR allows for pre-surgical simulations, giving surgeons the opportunity to rehearse complex procedures and improve their accuracy before operating on actual patients. Moreover, VR’s ability to create customized, controlled environments has proven invaluable in psychological therapy, offering new ways to treat anxiety disorders, phobias, PTSD, and other mental health conditions [4].
This review delves into the expanding role of VR in healthcare, exploring its application in medical education, surgical planning, and psychological therapy. Additionally, the review highlights the future potential of VR in healthcare and discusses the technological and financial challenges that must be overcome for its broader implementation.
2. Literature Survey
A survey of the literature reveals the increasing interest in VR's role in medical applications. Figure 1 illustrates the number of papers retrieved from Google Scholar using the search terms "Virtual Reality" and "Medical" over a ten-year period. The steady growth of relevant publications from 2010 to 2020 demonstrates VR's rising importance in healthcare research.
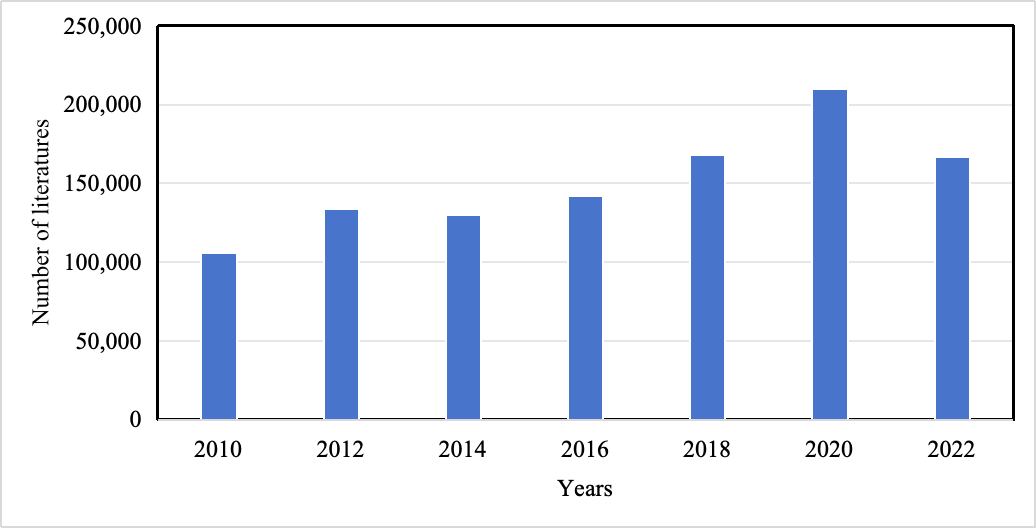
Figure 1. Number of papers searched using “Virtual Reality” and “Medical” every two years in Google Scholar
3. Background on Virtual Reality
VR systems can be broadly classified into two primary types: fully computer-generated environments and hybrid environments that integrate real-world media.[5] The first type generates 3D, interactive virtual worlds, where users can manipulate objects and interact with simulated elements. These environments, while artificial, have become increasingly realistic thanks to advances in rendering, AI, and physics engines. The second type involves 360-degree video or spherical images, offering a high degree of realism but limited interactivity due to the lack of true depth perception. A third emerging category blends these approaches, combining 3D models with real-world imagery to offer an immersive yet photorealistic experience.[6]
Recent innovations in VR hardware, such as lighter and more affordable headsets, as well as improvements in motion tracking and haptic feedback, have significantly enhanced the overall user experience. These technological advances are critical for medical applications, where precision and realism are paramount, whether for educational simulations, surgical planning, or patient therapy. As technology continues to evolve, VR's role in healthcare will likely expand, with potential applications ranging from patient rehabilitation to the creation of virtual hospitals for telemedicine.[7]
4. VR in Medical Education and Training
4.1. Simulation of Complex Medical Scenarios
One of VR’s most valuable contributions to medical education is its ability to simulate complex, high-risk medical scenarios that are difficult to recreate in traditional training environments. This capability is especially important in specialties such as neurosurgery, cardiology, and trauma care, where students can practice procedures repeatedly in a safe, controlled setting [3]. VR not only enhances technical skills but also helps students develop decision-making abilities, critical thinking, and the ability to manage emergencies under pressure.
VR simulations allow for customized learning paths tailored to individual students’ needs. For example, students can practice complex surgeries in virtual operating rooms or explore human anatomy in detailed, interactive 3D models. By replicating the look and feel of real-life medical scenarios, VR helps bridge the gap between theoretical knowledge and practical application.[8]
4.2. Enhanced Learning through Immersion
Research has shown that VR-based learning enhances retention and engagement compared to traditional methods.[9] Immersive learning environments provide students with real-time feedback, which accelerates the learning process and improves comprehension of complex concepts. For example, dental students using VR in implant training showed a significant increase in skill acquisition and confidence, as the virtual platform allowed them to practice various procedures in a realistic, yet controlled, environment. Additionally, VR-based anatomy courses have the potential to reduce the reliance on cadavers, offering an ethical and sustainable alternative that provides an equally rich learning experience.[10]
4.3. Case Studies of VR in Medical Training
Several case studies highlight the successful integration of VR in medical training. Ruthenbeck and Reynolds explored the role of haptic feedback in VR systems for medical training, such as bone and dental surgery, which enabled students to gain hands-on experience in highly specialized areas [6]. Similarly, Santiago González Izard et al. demonstrated how VR can improve the methodologies used in medical training by providing an interactive and immersive platform for learning [11]. These case studies reveal the potential of VR to revolutionize medical education by creating highly interactive and effective training environments.
5. VR in Surgical Planning and Diagnostics
VR’s ability to generate precise, 3D anatomical models has proven indispensable for surgical planning. Surgeons can use VR to simulate procedures before operating on patients, significantly reducing the likelihood of errors. This is particularly valuable in complex surgeries, such as those involving brain tumors, where precision is critical.[12] VR allows surgeons to visualize the anatomy in 3D, assess the surgical approach, and rehearse the operation, all while minimizing risks to the patient.
Bekelis et al. conducted a randomized controlled trial showing that patients exposed to VR simulations before surgery reported lower levels of preoperative anxiety and higher satisfaction with their surgical experience [13]. This demonstrates VR’s potential not only in improving surgical outcomes but also in enhancing the overall patient experience.
Moreover, advancements in VR-assisted diagnostics are helping physicians better understand complex conditions. The integration of 3D imaging and VR platforms allows for the visualization of internal organs and tissues in ways that were previously impossible, enabling more accurate diagnoses and treatment planning.
6. VR in Psychological Therapy
6.1. Exposure Therapy and Behavioral Training
VR has shown great promise in the field of psychological therapy, particularly for treating anxiety disorders, PTSD, and phobias. Exposure therapy, a common treatment for anxiety disorders, involves gradually exposing patients to feared stimuli in a controlled environment. VR enables therapists to simulate these stimuli in a safe and repeatable way, allowing patients to confront their fears without leaving the therapy room [14]. The flexibility of VR environments allows therapists to control the intensity and duration of the exposure, making the treatment more customizable and effective.[15]
Studies have also shown that VR can be used to treat addiction and eating disorders by creating immersive environments that help patients develop coping strategies and avoid triggers [16]. Similarly, VR is being explored as a treatment for autism spectrum disorder (ASD), where it can be used to teach social skills through controlled, virtual interactions.
6.2. Virtual Assessment and Cognitive Training
Beyond treatment, VR offers innovative tools for psychological assessment. By creating real-time simulations of daily life scenarios, VR enables therapists to observe patients' cognitive and emotional responses in real-time. This is particularly useful for patients with cognitive impairments or those recovering from brain injuries. VR-based assessments are more ecologically valid than traditional paper-and-pencil tests, providing therapists with a more accurate understanding of a patient’s functional capabilities in real-world settings [13][17].
7. Challenges and Future Directions
Despite the promising potential of VR in healthcare, several challenges remain. High hardware costs and the need for specialized software are significant barriers to widespread adoption. Future advancements are expected to address these issues by developing cost-effective, tailored software solutions and improving data storage for high-resolution simulations [18]. As these barriers are overcome, VR is likely to become an indispensable tool in both medical education and clinical practice.
8. Conclusion
Virtual Reality (VR) technology presents significant opportunities for advancing various aspects of healthcare, particularly in medical training, surgical planning, and psychological therapy. By providing highly immersive, interactive simulations, VR enables the replication of complex medical scenarios, leading to enhanced skill development, improved diagnostic accuracy, and more precise surgical interventions. Moreover, VR-based therapeutic approaches offer innovative methods for treating psychological disorders through controlled, customizable virtual environments. Despite its current limitations, including high hardware costs and the need for specialized software, the continued development of VR technology is expected to overcome these challenges. Future progress will focus on optimizing data management for high-resolution visualization and expanding the functionality of VR applications. With these advancements, VR is likely to become a critical tool for enhancing medical outcomes and patient care in clinical practice.
References
[1]. Wohlgenannt I, Simons A, Stieglitz S. Virtual reality. Business & Information Systems Engineering. 2020;62:455-461.
[2]. Guttentag DA. Virtual reality: Applications and implications for tourism. Tourism Management. 2010;31(5):637-651.
[3]. Huang Y, Hu Y, Chan U, Lai P, Sun Y, Dai J, Cheng X, Yang X. Student perceptions toward virtual reality training in dental implant education. PeerJ. 2023 May 5;11. doi: 10.7717/peerj.14857. PMID: 37168535; PMCID: PMC10166074.
[4]. Mohd Javaid, Haleem A. Virtual reality applications toward medical field. Clinical Epidemiology and Global Health. 2020;8(2):600-605.
[5]. Buttussi, Fabio, and Luca Chittaro. "Effects of different types of virtual reality display on presence and learning in a safety training scenario." IEEE transactions on visualization and computer graphics 24.2 (2017): 1063-1076.
[6]. Izard, Santiago González, et al. "Virtual reality as an educational and training tool for medicine." Journal of medical systems 42 (2018): 1-5.
[7]. Javaid, Mohd, and Abid Haleem. "Virtual reality applications toward medical field." Clinical Epidemiology and Global Health 8.2 (2020): 600-605.
[8]. Falah, Jannat, et al. "Virtual Reality medical training system for anatomy education." 2014 Science and information conference. IEEE, 2014.
[9]. Ruthenbeck, Greg S., and Karen J. Reynolds. "Virtual reality for medical training: the state-of-the-art." Journal of Simulation 9.1 (2015): 16-26.
[10]. Kockro, Ralf A., et al. "Planning and simulation of neurosurgery in a virtual reality environment." Neurosurgery 46.1 (2000): 118-137
[11]. Bekelis, Kimon, et al. "Effect of an immersive preoperative virtual reality experience on patient reported outcomes: a randomized controlled trial." (2017): 1068-1073.
[12]. Freeman, Daniel, et al. "Virtual reality in the assessment, understanding, and treatment of mental health disorders." Psychological medicine 47.14 (2017): 2393-2400.
[13]. Emmelkamp, Paul MG, and Katharina Meyerbröker. "Virtual reality therapy in mental health." Annual review of clinical psychology 17.1 (2021): 495-519.
[14]. Elphinston, Rachel A., et al. "Psychological therapy using virtual reality for treatment of driving phobia: a systematic review." Disability and rehabilitation 45.10 (2023): 1582-1594.
[15]. Parsons, Thomas D., and Amanda S. Phillips. "Virtual reality for psychological assessment in clinical practice." Practice Innovations 1.3 (2016): 197
[16]. Lumsden, Jim, et al. "Gamification of cognitive assessment and cognitive training: a systematic review of applications and efficacy." JMIR serious games 4.2 (2016): e5888.
[17]. Halbig, Andreas, et al. "Opportunities and challenges of virtual reality in healthcare–a domain experts inquiry." Frontiers in Virtual Reality 3 (2022): 837616.
Cite this article
Ji,S. (2024). The Role of Virtual Reality Technology in Medical Applications: A Review. Applied and Computational Engineering,114,60-64.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 2nd International Conference on Machine Learning and Automation
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Wohlgenannt I, Simons A, Stieglitz S. Virtual reality. Business & Information Systems Engineering. 2020;62:455-461.
[2]. Guttentag DA. Virtual reality: Applications and implications for tourism. Tourism Management. 2010;31(5):637-651.
[3]. Huang Y, Hu Y, Chan U, Lai P, Sun Y, Dai J, Cheng X, Yang X. Student perceptions toward virtual reality training in dental implant education. PeerJ. 2023 May 5;11. doi: 10.7717/peerj.14857. PMID: 37168535; PMCID: PMC10166074.
[4]. Mohd Javaid, Haleem A. Virtual reality applications toward medical field. Clinical Epidemiology and Global Health. 2020;8(2):600-605.
[5]. Buttussi, Fabio, and Luca Chittaro. "Effects of different types of virtual reality display on presence and learning in a safety training scenario." IEEE transactions on visualization and computer graphics 24.2 (2017): 1063-1076.
[6]. Izard, Santiago González, et al. "Virtual reality as an educational and training tool for medicine." Journal of medical systems 42 (2018): 1-5.
[7]. Javaid, Mohd, and Abid Haleem. "Virtual reality applications toward medical field." Clinical Epidemiology and Global Health 8.2 (2020): 600-605.
[8]. Falah, Jannat, et al. "Virtual Reality medical training system for anatomy education." 2014 Science and information conference. IEEE, 2014.
[9]. Ruthenbeck, Greg S., and Karen J. Reynolds. "Virtual reality for medical training: the state-of-the-art." Journal of Simulation 9.1 (2015): 16-26.
[10]. Kockro, Ralf A., et al. "Planning and simulation of neurosurgery in a virtual reality environment." Neurosurgery 46.1 (2000): 118-137
[11]. Bekelis, Kimon, et al. "Effect of an immersive preoperative virtual reality experience on patient reported outcomes: a randomized controlled trial." (2017): 1068-1073.
[12]. Freeman, Daniel, et al. "Virtual reality in the assessment, understanding, and treatment of mental health disorders." Psychological medicine 47.14 (2017): 2393-2400.
[13]. Emmelkamp, Paul MG, and Katharina Meyerbröker. "Virtual reality therapy in mental health." Annual review of clinical psychology 17.1 (2021): 495-519.
[14]. Elphinston, Rachel A., et al. "Psychological therapy using virtual reality for treatment of driving phobia: a systematic review." Disability and rehabilitation 45.10 (2023): 1582-1594.
[15]. Parsons, Thomas D., and Amanda S. Phillips. "Virtual reality for psychological assessment in clinical practice." Practice Innovations 1.3 (2016): 197
[16]. Lumsden, Jim, et al. "Gamification of cognitive assessment and cognitive training: a systematic review of applications and efficacy." JMIR serious games 4.2 (2016): e5888.
[17]. Halbig, Andreas, et al. "Opportunities and challenges of virtual reality in healthcare–a domain experts inquiry." Frontiers in Virtual Reality 3 (2022): 837616.