1. Introduction
The Greater Bay Area (GBA), comprising Hong Kong, Macao, and nine mainland cities, represents one of the most ambitious cross-border healthcare clusters globally. Its strategic position arises from internationally accredited hospitals in Hong Kong, cost-competitive centers in mainland cities like Guangzhou and Shenzhen, and tourism-oriented infrastructure in Macao. By 2024, over 1.3 million patients engaged in medical tourism in the region, with annual growth surpassing 14.5%. Driving this expansion are digital platforms that orchestrate complex cross-border services, from appointment scheduling and teleconsultations to insurance settlement and logistics [1].
Yet ecosystem development is constrained by regulatory heterogeneity. China’s Personal Information Protection Law (PIPL) imposes strict localization and transfer restrictions, Hong Kong’s PDPO permits comparatively liberal flows, while Macao blends EU-inspired rules with domestic mandates. This patchwork raises compliance costs, which rose from $7.8 per transaction in 2019 to $19.6 in 2024, a 151% increase that pressures small and mid-sized facilitators [2]. Previous studies have emphasized macroeconomic impacts or patient-level decisions but seldom addressed systemic ecosystem dynamics under regulation. In reality, hospitals adjust service portfolios, facilitators alter participation, and patients reassess destinations in response to evolving rules. These adaptive interactions produce nonlinear, path-dependent outcomes that static models cannot capture [3].
Agent-based modeling (ABM) offers a suitable approach, encoding heterogeneity, bounded rationality, and adaptive learning. By embedding regulatory variables into decision rules, ABM allows examination of how governance trajectories affect adoption thresholds, transaction growth, and systemic resilience. This study develops and validates a regulation-aware ABM for the GBA, combining simulation experiments and sensitivity analysis to derive insights on how governance can sustain innovation without undermining trust.
2. Literature review
2.1. Digital ecosystems in medical tourism
Digital ecosystems in medical tourism are socio-technical networks where hospitals, intermediaries, and patients co-evolve [4]. Their success depends on interoperability and trust rather than single-firm dominance. Southeast Asian experiences show interoperability standards can cut transaction friction and raise repeat usage by 27% within two years. In Europe, GDPR-compliant systems reveal that even small gains in trust directly boost adoption, with each one-point increase in trust index linked to a 4.2% rise in transaction volume.
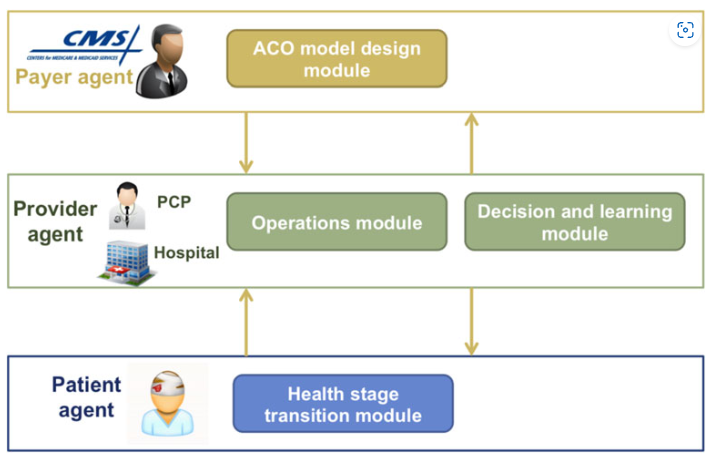
2.2. Agent-based modeling in healthcare
Agent-based modeling (ABM) is particularly well suited to healthcare because it captures heterogeneous actors and their adaptive decision-making processes. Figure 1 illustrates a typical ABM structure in healthcare, where payer agents, provider agents, and patient agents interact through modules for operations, decision-making, and health-stage transitions. Such architectures highlight the capacity of ABM to represent complex feedback loops across different actors [5]. Despite this potential, applications of ABM to medical tourism remain limited, and few incorporate the complexities of multi-jurisdictional regulation.
2.3. Data regulation in the greater bay area
The GBA features a fragmented regulatory landscape. Mainland China mandates domestic storage and government approval for cross-border transfers, with average compliance costs of $37,000 and delays up to 14 weeks by 2024 [6]. Hong Kong permits freer flows aligned with global standards, while Macao blends EU-style consent rules with conditional transfers. These asymmetries give Hong Kong hospitals easier access to international patients, while mainland facilities face heavier burdens. Attempts at “white-list” data transfer remain limited, covering under 8% of transaction types by mid-2024. This regulatory patchwork significantly shapes ecosystem formation and underpins the modeling focus of this study.
3. Methodology
3.1. Conceptual agent-based model
The ABM includes hospitals, facilitators, patients, and regulators. Hospitals reallocate services by profit and compliance cost, facilitators adjust commissions and market presence, and patients choose under peer-influenced trade-offs of quality, cost, travel, and privacy. Regulators set consent, localization, and audit rules. Interactions follow scale-free referral and spatial patient–hospital networks [7]. Calibration experiments indicated that values beyond 0.2 generated unstable oscillations, while values below 0.05 slowed convergence excessively. This update rule ensures that facilitators gradually align strategies toward higher payoff equilibria, reflecting real-world adaptation to regulatory pressures.
3.2. Data sources and regulatory scenarios
Model parameters came from GBA health statistics (2019–2024), 2.3M platform transactions, and 25 stakeholder interviews. Three regulatory scenarios were set: lenient ($10 consent, no localization, 5% audits), phased (consent rising $15→$35, localization after year 3, audits 10–25%), and strict ($50 consent, immediate localization, 40% audits). Uncertainty was modeled with triangular distributions.
3.3. Validation and calibration strategy
Calibration employed approximate Bayesian computation (ABC), aligning simulated adoption curves with historical telehealth data from a large GBA pilot between 2019 and 2022. Posterior distributions for patient adoption parameters exhibited narrow 95% credible intervals, with mean peer influence weights converging at 0.32 [0.29, 0.35]. Validation against out-of-sample Q4 2024 data indicated mean absolute error below 4.6% in transaction volumes across all scenarios [8]. Stakeholder workshops further ensured that simulated behaviors, such as facilitator exit thresholds and hospital compliance strategies, were consistent with observed market practices, reinforcing the model’s face validity.
4. Experimental design
4.1. Scenario construction
Simulations ran over 60 months with shocks including a year-2 pandemic (+18.7% demand), year-3 consent amendments (+$12.4 cost/transaction), and year-4 exchange-rate volatility (±12% demand shift). Hospital counts varied 60–120 and facilitators 100–250 for robustness.
4.2. Simulation execution
Each scenario used 1,000 Monte Carlo runs, producing ~3.6M agent-month records. GPU clusters cut runtime to <2h per 200 runs. Logged outputs included transactions, facilitator margins, hospital compliance, and patient dropout, with sparse networks enabling up to 50k patients per run [9].
4.3. Sensitivity analysis
Sensitivity analysis employed Sobol variance decomposition, enabling attribution of output variance to individual parameters and their interactions. Perturbations of ±20% were applied across five parameters: consent cost, localization enforcement, audit frequency, hospital reputation weight, and patient travel tolerance. First-order and total-effect indices were calculated using 100,000 Latin Hypercube samples, ensuring stable convergence of variance estimators. The Sobol formulation is expressed as equation 1 and 2:
where
5. Results and discussion
5.1. Baseline emergence patterns
Results indicate pronounced divergence across regulatory scenarios. Under lenient regulation, patient adoption plateaued at 37.9% ± 1.8%, with cumulative transaction volumes reaching 2.83 million [2.76M, 2.91M] by year 5. Facilitator retention remained relatively high at 72.1% [70.5%, 73.8%], but average compliance costs per transaction stabilized at only $12.3. In contrast, phased regulation achieved critical mass by month 26, with adoption surpassing the 40% threshold that triggers network externalities (table 1). Adoption reached 63.7% ± 2.3% by year 5, with cumulative transactions of 5.92 million [5.80M, 6.06M].
|
Scenario |
Adoption (%) |
Transactions (millions) |
Facilitator Retention (%) |
Compliance Cost ($) |
|
Lenient |
37.9 ± 1.8 |
2.83 [2.76-2.91] |
72.1 ± 1.7 |
12.3 ± 0.6 |
|
Phased |
63.7 ± 2.3 |
5.92 [5.80-6.06] |
88.2 ± 1.9 |
24.1 ± 1.1 |
|
Strict |
21.8 ± 1.5 |
1.94 [1.87-2.02] |
40.8 ± 1.8 |
51.2 ± 2.3 |
5.2. Impact of regulation strictness
Incremental increases in consent fees revealed nonlinear dampening effects. Facilitator retention remained stable up to $40, declined moderately between $40-45, but collapsed once fees exceeded $45. At $47, retention fell by 49% compared to baseline, effectively dismantling referral networks. Localization enforcement was equally critical: phased introduction allowed hospitals to spread compliance investments across three years, while immediate strict enforcement reduced hospital participation rates by 31.4%, constraining patient choice sets. Transaction elasticity analysis revealed that every $1 increase in consent fee beyond $40 reduced transaction volume by 83,000 [79,000-87,500] annually, underscoring the tipping point dynamics embedded in cost structures.
5.3. Sensitivity analysis
Sobol analysis identified data-localization cost as the most influential factor, explaining 61.2% of total variance, with a total-effect index of 0.673. Cross-border consent fees explained 22.5% of variance, with total-effect 0.266. Audit frequency accounted for 9.4%, while hospital reputation weight and patient travel tolerance contributed less than 2% each. Notably, interaction effects between localization and consent costs accounted for 5.1%, confirming the multiplicative burden of simultaneous enforcement (table 2).
|
Parameter |
First-order Si |
Total-effect STi |
|
Data-localization cost |
0.612 |
0.673 |
|
Cross-border consent fee |
0.225 |
0.266 |
|
Audit frequency |
0.094 |
0.108 |
|
Hospital reputation weight |
0.017 |
0.022 |
|
Patient travel tolerance |
0.009 |
0.015 |
5.4. Policy and managerial implications
These results suggest that phased regulation optimally balances ecosystem growth with trust-building. Regulators are advised to implement sandbox pilots where consent costs and localization requirements are gradually introduced, allowing actors to adapt without market collapse. Platform designers should develop blockchain-based consent ledgers that reduce verification overhead, estimated to lower compliance costs by 12-17% annually.
6. Conclusion
This study demonstrates that digital medical tourism ecosystems in the GBA are highly sensitive to regulatory trajectories. Phased regulation fosters critical mass adoption within three years, whereas strict enforcement prevents ecosystem takeoff. Data-localization costs and consent fees emerge as dominant determinants of systemic outcomes, with interaction effects producing nonlinear tipping points. Methodologically, the integration of reinforcement learning dynamics and variance-based sensitivity analysis provides robust predictive capacity. Practically, the findings recommend adaptive regulatory frameworks, sandbox pilots, and governance innovations such as data trusts to reconcile privacy protection with innovation. Future research will extend the model to multi-platform competition and integrate real-time IoT health data streams for enhanced predictive fidelity.
References
[1]. Al-Romeedy, B. S., Emam, M. E., Hussein, H., Singh, A., & Tyagi, P. K. (2025). Digital Passports to Wellness: How Technology Is Shaping Medical Tourism. In Revolutionizing Healthcare Experience With Digital Medical Tourism (pp. 111-136). IGI Global Scientific Publishing.
[2]. Liu, Y., Zhou, Y., Yang, L., & Xin, Y. (2024). Simulating staff activities in healthcare environments: an empirical multi-agent modeling approach. Journal of Building Engineering, 84, 108580.
[3]. Au, A., & Witzleb, N. (2024). Data flows and data protection in the Greater Bay Area: The need for a coordinated legal framework. The Chinese Journal of Comparative Law, 12, cxae013.
[4]. Reshadi, M. S., & Chehragh, A. M. (2025). A review of medical tourism entrepreneurship and marketing at regional and global levels and a quick glance into the applications of artificial intelligence in medical tourism. AI & SOCIETY, 1-17.
[5]. Kim, S., Lee, S., Kim, M., Lee, C., & Kang, J. Y. (2024). Vulnerability Assessment for Pediatric Healthcare Services Using Agent-based Modeling: A Case Study of Four Districts in Southwest Seoul. Journal of the Korean Geographical Society, 59(2), 196-209.
[6]. Migliorini, S., & Matias, C. (2024). New frontiers of legal integration: Developing the regulatory framework of the Greater Bay Area. The Chinese Journal of Comparative Law, 12, cxae019.
[7]. Talukder, M. B., Huda, M. N., Kumar, S., & Hasan, M. M. (2025). Metaverse Future of Digital Medical Tourism. In Revolutionizing Healthcare Experience With Digital Medical Tourism (pp. 173-198). IGI Global Scientific Publishing.
[8]. Carramiñana, D., Bernardos, A. M., Besada, J. A., & Casar, J. R. (2025). Enhancing healthcare infrastructure resilience through agent-based simulation methods. Computer Communications, 234, 108070.
[9]. Chirmulay, V., & Bhakare, J. (2025). Digital Health and Medical Tourism: A Regulatory Perspective. In Navigating Innovations and Challenges in Travel Medicine and Digital Health (pp. 311-324). IGI Global Scientific Publishing.
[10]. Li, H. (2024). Research on the Cross-boundary Data Transfer within the Guangdong-Hong Kong-Macao Greater Bay Area. Science of Law Journal, 3(1), 95-99.
Cite this article
Qin,Z. (2025). Agent-Based Prediction of Digital Ecosystem Emergence in Medical Tourism under Evolving Greater Bay Area Data Regulation. Applied and Computational Engineering,193,37-42.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 3rd International Conference on Machine Learning and Automation
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Al-Romeedy, B. S., Emam, M. E., Hussein, H., Singh, A., & Tyagi, P. K. (2025). Digital Passports to Wellness: How Technology Is Shaping Medical Tourism. In Revolutionizing Healthcare Experience With Digital Medical Tourism (pp. 111-136). IGI Global Scientific Publishing.
[2]. Liu, Y., Zhou, Y., Yang, L., & Xin, Y. (2024). Simulating staff activities in healthcare environments: an empirical multi-agent modeling approach. Journal of Building Engineering, 84, 108580.
[3]. Au, A., & Witzleb, N. (2024). Data flows and data protection in the Greater Bay Area: The need for a coordinated legal framework. The Chinese Journal of Comparative Law, 12, cxae013.
[4]. Reshadi, M. S., & Chehragh, A. M. (2025). A review of medical tourism entrepreneurship and marketing at regional and global levels and a quick glance into the applications of artificial intelligence in medical tourism. AI & SOCIETY, 1-17.
[5]. Kim, S., Lee, S., Kim, M., Lee, C., & Kang, J. Y. (2024). Vulnerability Assessment for Pediatric Healthcare Services Using Agent-based Modeling: A Case Study of Four Districts in Southwest Seoul. Journal of the Korean Geographical Society, 59(2), 196-209.
[6]. Migliorini, S., & Matias, C. (2024). New frontiers of legal integration: Developing the regulatory framework of the Greater Bay Area. The Chinese Journal of Comparative Law, 12, cxae019.
[7]. Talukder, M. B., Huda, M. N., Kumar, S., & Hasan, M. M. (2025). Metaverse Future of Digital Medical Tourism. In Revolutionizing Healthcare Experience With Digital Medical Tourism (pp. 173-198). IGI Global Scientific Publishing.
[8]. Carramiñana, D., Bernardos, A. M., Besada, J. A., & Casar, J. R. (2025). Enhancing healthcare infrastructure resilience through agent-based simulation methods. Computer Communications, 234, 108070.
[9]. Chirmulay, V., & Bhakare, J. (2025). Digital Health and Medical Tourism: A Regulatory Perspective. In Navigating Innovations and Challenges in Travel Medicine and Digital Health (pp. 311-324). IGI Global Scientific Publishing.
[10]. Li, H. (2024). Research on the Cross-boundary Data Transfer within the Guangdong-Hong Kong-Macao Greater Bay Area. Science of Law Journal, 3(1), 95-99.