1. Introduction
In recent years, healthcare spending in the United States have reached unprecedented levels, a trend closely related to the demographic ageing of society. As the population aged 65 and above continues to grow, the demand for healthcare resources has increased, further pushing up healthcare spending. According to relevant studies, healthcare spending show a significant positive correlation with the increase in the aging population, which imposes a heavy financial burden on individuals, and puts tremendous pressure on the U.S. healthcare system and public finances. The study aims to examine the key factors contributing to the escalation of healthcare spending in the U.S., with a special focus on the impact of aging on the balance between supply and demand for healthcare services. Although studies have been conducted to discuss the impact of aging on healthcare expenditures, the existing literature still lacks an in-depth exploration of the causes of the slowdown in healthcare cost growth and the effectiveness of government interventions. Therefore, this paper contributes to the analysis of the multiple drivers behind the growth of healthcare spending and further explores the impact on healthcare costs of the policies adopted by the U.S. government in response to the aging problem. By analyzing the existing literature and data, this study reveals the mechanisms behind the high cost of healthcare in the U.S., uncovers the complex relationship between aging and healthcare spending, and provide support for further optimization of healthcare policies.
2. The Current Situation of Aging Society in the U.S.
At present, healthcare spending in the U.S. is much higher than that in other developed countries, although the rate of growth in this aspect has slowed in recent years. Data shows that As of 2023, the average healthcare cost per person in the U.S. is approximately $12,000 to $13,000 annually. However, this figure can vary significantly based on factors like age, location, and insurance coverage. And subsequent studies have continued to demonstrate that the relatively elevated level of healthcare expenditure in the U.S. persists. As can be seen, the financial burden of healthcare in the U.S. has been a persistent concern for an extended period, and the implications of an ageing population are becoming increasingly evident. In addition, National Health Expenditure (NHE) per person in the U.S. was estimated to be around $12,900 in 2021, which typically rises annually due to various factors, including healthcare inflation and changes in services utilized. This trend reflects structural issues facing the U.S. health care system, such as the continued growth in health care demand from an aging population, which suggests that policymakers need to focus on the economic impact of health care spending and its future challenges. Figure 1 compares the U.S. population in 1960 with the projected population in 2060, reflecting the significant changes in population [1]. The 1960 population pyramid has a typical pyramid shape, with a large proportion of young people (0-4 and 5-9 years old), a decreasing population with age, especially the elderly population aged 85 and older, and a significant imbalance in the male/female ratio. By 2060, the shape of the population pyramid will have changed markedly, and in particular the number of people aged 65 and over will have increased markedly, suggesting that the U.S. is facing a serious ageing phenomenon. In order to meet the challenges of the upcoming aging, policymakers will need to proactively adjust policies to ensure that social security, medicare, and economic support systems are able to effectively meet the needs of the changing population.
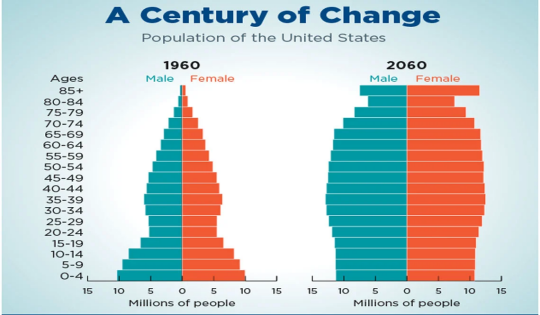
Figure 1: Population Change in US in A Century
3. The Economic Impact of Aging on Healthcare Spending
3.1. The Economic Structure of Healthcare Spending
The structure of healthcare spending in the U.S. shows significant features. And private insurance accounts for the largest share of all health care expenditures, followed by medical insurance. While out-of-pocket spending by individuals is relatively small, expenditures on private insurance and health insurance have continued to grow in recent years. This trend reflects the centrality of private insurance and health insurance in the U.S. healthcare system and its huge impact on the financial burden of households. Within the expenditure structure of U.S. households, housing, transportation, and food are the three items that account for the highest share of household expenditures, according to data from the Bureau of Labor Statistics in Table 1 [2]. However, when insurance and medical expenses are included, their combined share reaches 20%, surpassing transportation to become the second largest share of household expenditures. In addition, insurance and medical expenditures account for about 18% of household income, which further demonstrates the importance of medical expenditures in the household economy. These data show that while health care expenditures in the United States come from multiple sources, the financial burden on individuals and families remains high, reflecting the structural challenges that the U.S. faces in its health insurance system and health care delivery. Policymakers should pay attention to this phenomenon to develop more effective healthcare policies in the future in order to reduce the financial pressure on families and ensure the sustainability of universal healthcare coverage [3].
Table 1: American Households Average Monthly Expenses
Category | Average Monthly Expenditures | Average Annual Expenditures | Percent of Overall Spending | Percent of Income (After Tax) |
Housing | $2,120 | $25,436 | 33% | 29% |
Transportation | $1,098 | $13,174 | 17% | 15% |
Food | $832 | $9,985 | 13% | 11% |
Personal Insurance and Pensions | $796 | $9,556 | 12% | 11% |
Healthcare | $513 | $6,159 | 8% | 7% |
Entertainment | $303 | $3,635 | 5% | 4% |
Cash Contributions | $198 | $2,378 | 3% | 3% |
Apparel and Services | $170 | $2,041 | 3% | 2% |
Education | $138 | $1,656 | 2% | 2% |
Miscellaneous | $110 | $1,326 | 2% | 2% |
Personal Care Products and Services | $79 | $950 | 1% | 1% |
Alcoholic Beverages | $53 | $637 | 1% | 1% |
3.2. Driving Factor of Aging to the Increase of Medical Expenditure
The phenomenon of ageing has contributed significantly to the growth of health-care expenditure. As the proportion of older persons in the population rises, older persons are more prone to disease than younger persons, leading to an increase in per capita health-care expenditures. In the U.S., for example, physicians’ incomes are correlated with the number of prescription drugs and medical services, which in part drives physicians to use more drugs and services. Data show that the U.S. has the highest prescription drug spending in the world, accounting for nearly 84% of total healthcare costs, despite the fact that prescription drugs account for only 8% of the drug market. There are two main reasons for this trend: first, doctors tend to recommend higher-priced drugs, which patients are more likely to accept due to low out-of-pocket payments. By 2022, patients will only be responsible for about 10% of healthcare costs, with the rest covered by insurance, driving up demand for care. Second, doctors often prescribe more to avoid misdiagnosis, and patients' expectation of a thorough examination drives doctors to adopt more cautious strategies. Insurance covering most of the costs is key to patients' willingness to spend more. With private and government health insurance covering the vast majority of healthcare expenditures in 2022 and patient out-of-pocket costs accounting for only about 10 percent, patients are choosing more medications and services to drive spending even though the total cost is high, according to the data. Japan is aging just as badly, with 28.4% of the population aged 65 and over and 9.0% aged 80 and over, well above the 5.6% and less than 1% in 1960. Japan’s healthcare system relies on public funding, with 84.1% of healthcare expenditures borne by the national treasury in 2017, lower out-of-pocket costs for households, and lower per capita expenditures than in the U.S. [4]. The Japanese public healthcare system indicates a capacity to adapt its spending patterns in response to the needs of an aging population. This is a valuable lesson for policymakers seeking to achieve sustainability in healthcare delivery.
3.3. Fiscal Pressures on Social Insurance
The high cost of private insurance in the U.S., which has increased at a rate that outpaces workers’ incomes on an almost annual basis, reflects the challenge insurers face in attracting customers, especially those who want to stay healthy in order to avoid frequent medical claims and ensure that their companies are profitable. In this context, healthy consumers often have reservations about buying insurance because they believe that buying insurance may cause financial losses. In contrast, consumers with poorer health are more inclined to buy insurance, but insurance providers are generally reluctant to sell insurance to these high-risk groups due to the uncertainty of insurance companies about their health status. This situation leads to information asymmetry, that is, unequal access to health information between buyers and sellers.In response to this problem, insurance companies usually choose to increase insurance prices as a strategy to reduce risks. However, the resulting increase in insurance costs has created additional financial pressure on people with lower incomes and poor health, forcing them to bear higher premiums, thus creating an unfair situation. This phenomenon not only exacerbates economic inequality in society, but also poses a serious challenge to the sustainability of the social insurance system, calling on policymakers to conduct in-depth analysis and reform to ensure that everyone has access to fair and affordable medical insurance [5].
3.4. The Influence of Aging on the Balance of Supply and Demand of Medical Service
As the population ages, the demand for medical personnel increases dramatically. In the U.S. health care system, medical personnel are paid at a much higher level than in other countries and account for a larger share of total health care expenditures. This income gap stems primarily from the imbalance between the supply and demand for physicians and the high cost of education and training. In the United States, becoming a doctor requires at least four years of professional education and the cost of education is extremely high, with average annual tuition of about $40,000 and total costs of up to $320,000 per year. This financial burden limits the supply of doctors, and high salaries become a key factor in attracting talent, creating a closed loop of high salaries and talent supply and demand. U.S. hospitals do not hire low-paying foreign doctors, mainly because of strict U.S. medical education standards that require doctors to complete at least four years of specialized training. This restriction has made the U.S. dependent on local doctors, which has further inflated medical costs. In contrast, Hong Kong, China, also faces a shortage of medical personnel, but has eased the situation through effective measures [6,7]. The Hong Kong government increased the number of medical school graduates from 250 to 420 in 2018, while extending the retirement age of doctors from 60 to 65 and allowing overseas doctors to work in public hospitals with special temporary licenses. These initiatives have effectively alleviated the shortage of medical personnel and provided better medical care for an aging society. These experiences serve as references for addressing the medical challenges of ageing.
4. Measures to Address the Impact of Aging on Health Care Expenditures in the U.S.
4.1. Health Insurance Reform
Health insurance in the U.S. can be divided into medical subsidy, government direct provision and private insurance. The first two are provided by government in order to help reducing the price of medical services and insurances, so everyone can enjoy them, including poor people and old people, because people need to spend less on these, healthcare spending per capita can be reduced. The last one is insurances that people need to buy on their own, as there is serious problem of aging and healthy people are unwilling to buy health insurance, in order to earn money, insurance companies have no choice but to set a lower price for people in need. Lower price can also help reducing healthcare spending [8]. The U.S. government is reforming health insurance because of the rising costs of aging. One option would be for the government to provide health insurance directly to everyone. This would prevent some people who are unhealthy or poor from being unable to buy insurance or having to pay a high price for it. Another option is that some insurance companies can accept the purchase of insurance on a company-by-company basis, which can ensure that every employee in the company can buy insurance at a relatively cheap price.
4.2. Health Management and Preventive Measures for the Elderly
In the United States, health management for older adults consists primarily of lifestyle behavioral interventions and disease management interventions. Lifestyle behavior interventions focus on three types of modifiable factors: physical inactivity, healthy eating, and smoking. For example, healthy eating interventions can only be truly effective if there is consistent access to healthy foods. Disease management interventions, on the other hand, are designed for people at high risk for chronic diseases such as diabetes, asthma, and congestive heart failure, and are designed to reduce costs by reducing emergency room visits and hospitalizations, improving quality of life, and improving clinical outcomes through evidence-based practices. In the United States, certification in geriatrics is required to become a physician qualified to treat geriatric diseases, but fewer physicians are willing to pursue this certification because geriatricians typically earn less than physicians in other specialties. To address this problem, the Government has in recent years encouraged medical students to obtain geriatrics certificates through measures such as salary increases to ensure that the elderly receive adequate medical care. In addition, in order to alleviate the pressure on medical costs brought about by ageing, the Government actively promotes vaccination of the elderly and provides subsidized or free benefits to prevent diseases and reduce medical expenses [9].
4.3. Fiscal Policy Adjustment
It would be beneficial to increase competition among insurance companies, as the insurance market in the U.S. is currently dominated by a small number of large companies that form an oligopoly. In oligopoly markets, businesses are disinclined to engage in competitive behavior due to the presence of significant barriers to entry. These barriers may include licensing requirements or brand loyalty, which effectively prevent other firms from entering the market. These big insurance companies may set a high price together, so they can earn at price maximize of monopoly. As such, consumers of health insurance are worse off since they need to pay a lot. Thus, the government sets policies to improve competition, for example preventing big companies from merging with each other in order to occupy larger market share. In addition, health care should be subsidized. For instance, in 2023, federal subsidies for health insurance are estimated to be $1.8 trillion, or 7.0 percent of gross domestic product (GDP). In CBO and JCT’s projections, those net subsidies reach $3.3 trillion, or 8.3 percent of GDP, in 2033. Because of the subsidy, people can pay for the medical services at a lower price, so old people can be more willing to spend money on healthcare, thus they can be more healthy and won’t use as much money as they don’t go to the hospital until they are very sick [10].
5. Conclusion
This paper discusses the determinants of rising healthcare costs in the U.S. as well as factors that have led to a slowdown in cost growth. The causes of rising healthcare costs due to an aging population can be broadly classified into two categories: the increased utilization of more expensive medications and services by the elderly, and the high demand for healthcare workers. The deceleration in cost escalation can be ascribed to governmental policies aimed at curbing healthcare expenditure, including subsidies, direct insurance provision, and enhanced competition among enterprises. Future research could further analyze the specific impact of aging on the demand for various types of healthcare services, especially the cost burden in terms of specific diseases and care, and explore the role of technological advances in reducing healthcare costs, especially the use of telemedicine and artificial intelligence. In addition, assessing the impact of government policies on the sustainability of healthcare costs in the long run will help optimize future policy design.
References
[1]. KFF. (2022) Health Care Costs: A Primer. https://www.kff.org/report-section/health-care-costs-a-primer-2012-report/
[2]. Caporal, K. (2024) American Households' Average Monthly Expenses: $6,440. https://www.fool.com/the-ascent/research/average-monthly-expenses/
[3]. Jones, C.H. and Dolsten, M. (2024) Healthcare on the brink: navigating the challenges of an aging society in the United States. npj Aging 10, 22.
[4]. Ibuka, Y., et al. (2016) Medical Spending in Japan: An Analysis Using Administrative Data from a Citizen's Health Insurance Plan. Fiscal Studies, 37(3-4): 561-592
[5]. Pereno, A. and Eriksson, D. (2020) A multi-stakeholder perspective on sustainable healthcare: From 2030 onwards. Futures, 122: 102605.
[6]. Lam, G. (2022) Shortage of nurses in Hong Kong: the challenges ahead. Asian Education and Development Studies.
[7]. Drennan, V.M. and Ross, F. (2019) Global nurse shortages-the facts, the impact and action for change. Br Med Bull. 130(1): 25-37.
[8]. Rice, T., Rosenau, P., Unruh, L.Y. and Barnes, A.J. (2020) United States: Health System Review. Health Syst Transit. 22(4): 1-441.
[9]. Tkatch, R., et al. (2016) Population Health Management for Older Adults: Review of Interventions for Promoting Successful Aging Across the Health Continuum. Promoting Successful Aging Across the Health Continuum. Gerontology and Geriatric Medicine.
[10]. Trottmann, M., et al. (2023) Balancing between competition and regulation in healthcare markets. Health Econ Policy Law, 21:1-10.
Cite this article
Wang,M. (2025). Research on the Determinants of Elevated Healthcare Costs in the U.S. and the Factors Contributing to the Slowdown in Cost Growth. Advances in Economics, Management and Political Sciences,158,7-12.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of CONF-BPS 2025 Workshop: Sustainable Business and Policy Innovations
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. KFF. (2022) Health Care Costs: A Primer. https://www.kff.org/report-section/health-care-costs-a-primer-2012-report/
[2]. Caporal, K. (2024) American Households' Average Monthly Expenses: $6,440. https://www.fool.com/the-ascent/research/average-monthly-expenses/
[3]. Jones, C.H. and Dolsten, M. (2024) Healthcare on the brink: navigating the challenges of an aging society in the United States. npj Aging 10, 22.
[4]. Ibuka, Y., et al. (2016) Medical Spending in Japan: An Analysis Using Administrative Data from a Citizen's Health Insurance Plan. Fiscal Studies, 37(3-4): 561-592
[5]. Pereno, A. and Eriksson, D. (2020) A multi-stakeholder perspective on sustainable healthcare: From 2030 onwards. Futures, 122: 102605.
[6]. Lam, G. (2022) Shortage of nurses in Hong Kong: the challenges ahead. Asian Education and Development Studies.
[7]. Drennan, V.M. and Ross, F. (2019) Global nurse shortages-the facts, the impact and action for change. Br Med Bull. 130(1): 25-37.
[8]. Rice, T., Rosenau, P., Unruh, L.Y. and Barnes, A.J. (2020) United States: Health System Review. Health Syst Transit. 22(4): 1-441.
[9]. Tkatch, R., et al. (2016) Population Health Management for Older Adults: Review of Interventions for Promoting Successful Aging Across the Health Continuum. Promoting Successful Aging Across the Health Continuum. Gerontology and Geriatric Medicine.
[10]. Trottmann, M., et al. (2023) Balancing between competition and regulation in healthcare markets. Health Econ Policy Law, 21:1-10.