1. Introduction
The influence of social media usage (SMU) on depression is of significant and pressing concern among adolescents. The negative impact of excessive SMU on the mental health and well-being of adolescents may be the underlying cause. Research indicates an association between heavy SMU and heightened levels of depression in young adults. This relationship underscores the need for active monitoring and intervention regarding social media habits and associated depressive symptoms among adolescents.
Adolescence is a critical developmental stage, during which individuals are particularly vulnerable to external influences, including those from social media. Excessive exposure to social media platforms can exacerbate feelings of loneliness, inadequacy, and comparison among adolescents, leading to a heightened risk of depression. Moreover, the constant online presence and pressure to project an idealized self-image can contribute to feelings of anxiety and low self-esteem, further exacerbating the risk of depression.
Recent research has investigated the complex relationship between SMU, depression, and sleep among adolescents. Lin et al. found that adolescents who frequently use social media are more likely to experience decreased sleep quality, and this association is partially moderated by depressive symptoms [1]. Levenson et al. revealed a bidirectional relationship between social media usage, depression, and sleep, indicating that SMU and depressive symptoms can mutually influence each other, thereby affecting both the quality and duration of adolescents' sleep [2]. Orzech et al. further confirmed the association between excessive social media use, depressive symptoms, and poor sleep quality in college students [3].
These studies collectively highlight a concerning trend: increased SMU is often accompanied by more depressive symptoms and sleep distributions. The underlying mechanisms might be multifaceted. From one perspective, social media platform can foster social comparison, cyberbullying, and exposure to negative content, all of which can exacerbate depressive symptoms and disrupt sleep patterns. On the other hand, becoming depressive can cultivate loneliness and the need to browse online social media to mitigate the negative feelings. Additionally, it is crucial to note that the relationship between SMU, depression, and sleep might be non-linear and have a circular influence on each other. These theoretical underpinnings warrant further research and investigations to study the impact of social media on mental health and sleep among young adolescents.
2. Methods
2.1. Participants
Participants were recruited through an online survey tool called Questionnaire Star. Each participant completed 60 questions. Initially, a total of 115 participants filled out the survey. However, 4 participants were excluded due to missing data, thus the final pool of participants consisted only of 111 subjects. All of the participants were Mandarin speakers, residing in China (n=109), United States (n=1), or Spain (n=1).
2.2. Study Design
The 60-question survey contained four distinct sections: 1) demographic information (age [7.2% below age 16, 75.7% age 16-20, 11.7% age 20-24, 5.4% above age 24], gender [67.6% female, 32.4% male], occupation [70.3% high school, 23.4% undergraduate, 6.3% others (graduate students and working individuals)]), 2) a depressive symptom questionnaire, 3) a sleep duration and sleep quality questionnaire, and 4) a social media usage questionnaire. All questionnaires were translated and delivered in Chinese.
To assess depression levels, the Self-Rating Depression Scale (SDS) was modified [4]. The SDS originally comprised 20 items, each requiring responses on a four-point Likert scale. The current survey included 19 of these items and employed a five-point Likert scale to determine the final depression level. For each item, participants indicated whether their level of agreement with the statement as follows: a) strongly disagreed, b) disagreed, c) neutral, d) agreed, and e) strongly agreed. Of the 19 items, ten were positively worded, and the rest nine were negatively worded. For the positively worded questions, items were scored 5 = a), 4 = b), 3 = c), 2 = d), and 1 = e). Conversely, the negative items were scored inversely with 1 = a), 2 = b), 3 = c), 4 = d), and 5 = e). The sum of the scores for the 19 items constituted the final depression total score, ranging from 19 to 95. The higher the score, the more depressed the participant was.
A subsection of the Pittsburgh Sleep Quality Index (PSQI) was modified to evaluate participant’s sleep duration and sleep quality [5]. Specifically, the survey directly asked the participants to self-report their average hours of sleep over the past month. In addition, items in questions 5 of the PSQI were used to assess their sleep quality. The question asked: During the past month, how often have you had trouble sleeping because you… a) Cannot get to sleep within 30 minutes; b) Wake up in the middle of the night or early morning; c) Have to get up to use the bathroom; d) Cannot breathe comfortably; e) Cough or snore loudly; f) Feel too cold; g) Feel too hot; h) Had bad dreams; i) Have pain. Unlike the original PSQI, which asked participants about the frequency of encountering these situations, we used a five-point Likert scale to determine how much they agree or disagree with each statement. Items were scored as follows: 5 = strongly disagreed, 4 = disagreed, 3 = neutral, 2 = agreed, and 1 = strongly agreed. A higher score indicated better sleep quality.
Several questions about SMU were modified from Social Anxiety Scale for Social Media Users (SAS-SMU) [6]. However, these questions were not analyzed due to their lack of comprehensive coverage over the concept of social anxiety induced by social media. Two additional questions were included to assess: 1) the duration of electronic device usage every day (8.2% below 1h, 31.5% 1-3h, 31.5% 3-6h, 14.4% 6-9h, 11.7% 9-12h, 2.7% above 12h), and 2) the duration of social media usage online every day (54.1% 1-2h, 27.9% 2-4h, 13.5% 4-6h, 4.5% above 6h).
2.3. Statistical Analysis
Pearson correlation analyses were conducted to examine the associations between three continuous variables: depression, sleep duration, and sleep quality. One-way ANOVAs were used to compare differences in depression and sleep health scores across various demographic and behavioral factors, such as age, gender, occupation, electronic device usage, and SMU. All analyses were subjected to Bonferroni-Holm’s correction to control for multiple comparisons.
One goal of the current study is to address the potential mediating role of SMU in the relationship between depression and sleep health. To tackle this hypothesis, a mediation model was constructed with depression as the predictor variable, sleep duration and sleep quality as the outcome variable, and SMU as the mediator. Model parameters were estimated using a bootstrapped approach with 10000 iterations in lavaan package within R, and all effects were standardized.
All statistical analyses were performed using the R programming language, employing both base functions and the lavaan package for structural equation modeling.
3. Results
3.1. Relationship between depression and sleep health
To investigate the relationship between depression, sleep duration, and sleep quality, Pearson’s correlation analyses were conducted. The results are shown in Table 1 below.
Table 1: Pearson Correlation between depression, sleep duration and sleep quality.
Depression | Sleep Quality | Sleep Duration (hrs) | |
Depression | |||
Sleep Quality | -0.36*** | ||
Sleep Duration (hrs) | -0.37*** | 0.03 | |
Mean | 52.4 | 34.6 | 7.5 |
S.D. | 7.6 | 7.2 | 2.7 |
*** p < 0.001, Bonferroni-Holm corrected
Depression was found to be negatively correlated with both sleep quality (r(109) = -0.36, p < 0.001) and sleep duration (r(109) = -0.37, p < 0.001). This suggests that higher levels of depression are associated with poorer sleep quality and shorter sleep duration. Interestingly, sleep quality and sleep duration were insignificantly weakly correlated (r(109) = 0.043, p = 0.654), suggesting that their influence of depression on sleep quality and sleep duration arises from distinct factors.
3.2. The influence on depression and sleep health
After applying Bonferroni-Holm’s correction for multiple comparisons, none of the factors -- age, gender, electronic device usage or social media usage -- exhibited a significant influence on depression or sleep health (p > 0.05). However, a one-way ANOVA revealed a significant difference in sleep duration among the different occupations (F(2, 108) = 15.25, p < 0.001). Table 2 displays the summary statistics grouped by occupation. Post-hoc two-sample t-tests indicated that high school students slept significantly less that undergraduates (t(45.5)= -5.87, p < 0.001), but there was no significant difference in sleep duration between high school students and others (graduate student and working individuals) (t(6.38)= -1.24, p = 0.6). Additionally, there was no significant difference in sleep duration between undergraduates and individuals in other occupations (t(7.02)= -0.7, p = 0.669).
Table 2: Summary Statistics of Life Quality and Depress.
Depression | Sleep Quality | Sleep Duration (hrs) | |
High school | 53.0 (7.8) | 35.2 (7.0) | 6.6 (2.1) |
Undergraduate | 50.7 (8.7) | 33.7 (5.4) | 9.3 (3.2) |
Others (graduates/working) | 52.0 (9.4) | 31.4 (8.0) | 8.3 (3.6) |
Notes: The values in the table are mean (standard deviation). Bolded summary statistics are significant different after Bonferroni-Holm correction.
3.3. Mediation effect on sleep health
Figure 1 below shows the effect of depression on sleep duration and sleep health, both of which were not mediated by SMU. The mediation model suggested that there is only a direct effect of depression on sleep duration (B = -0.12, p < 0.001; bootstrapped CI = [-0.17, -0.06]) and sleep health (B = -0.33, p < 0.001; bootstrapped CI = [-0.5, -0.13]). All effect sizes are non-standardized.
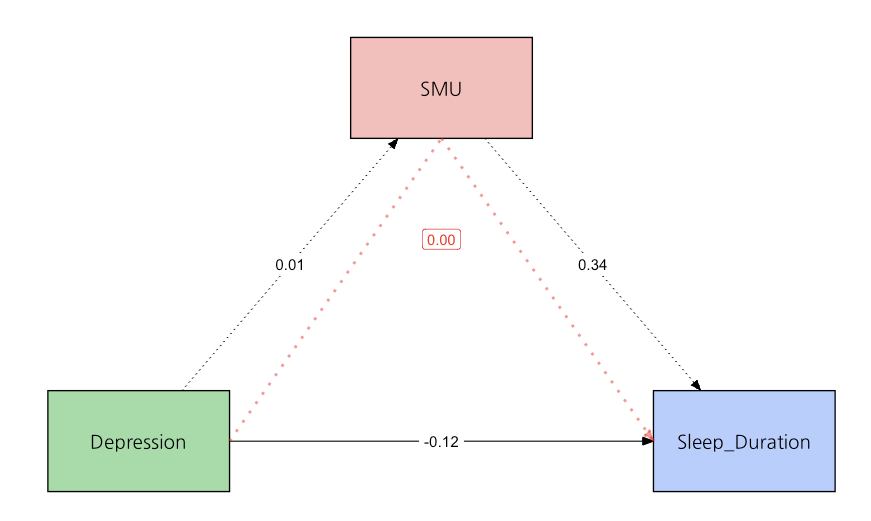
Figure 1: Mediation model on sleep duration.
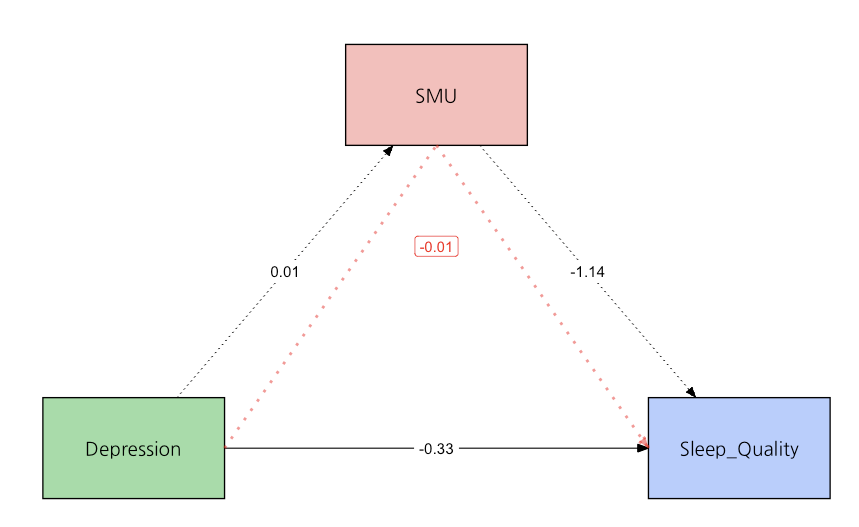
Figure 2: Mediation model on sleep quality.
Notes: Black lines and arrows indicate = direct effect (solid = significant, dotted = non-significant). Red dotted line and arrow = insignificant indirect effect.
3.4. Social media usage self-reports
Two of the questions in the survey inquired about the effect of social media usage on individuals’ overall lives and sleep quality, without specifically defining each statement. Regarding life in general, 67.6% (n=75) of the participants reported that they felt much happier when viewing social media, while only 7.2% (n=8) rated that they felt unhappier. The remaining 25.2% (n=28) had mixed feelings about social media usage. Interestingly, despite nearly 70% of people self-reporting increased happiness with more SMU, the effect between SMU and depression is non-significant. This suggest that increased SMU does not necessarily correlate with reduced depression, and the mechanisms of which SMU affects happiness and depression might be different.
Regarding sleep quality, the survey indicated that 17.1% (n=19) of the participants reported that SMU never affected their sleep quality, 30.6% (n=34) reported it rarely affected them, 39.6% (n=44) reported it sometimes affected them, and 12.6% (n=14) reported it often affected them. However, even with over 50% of respondents self-reporting that SMU does at least somewhat affects their sleep quality, the negative impact of SMU on sleep quality remains statistically insignificant in the mediation model.
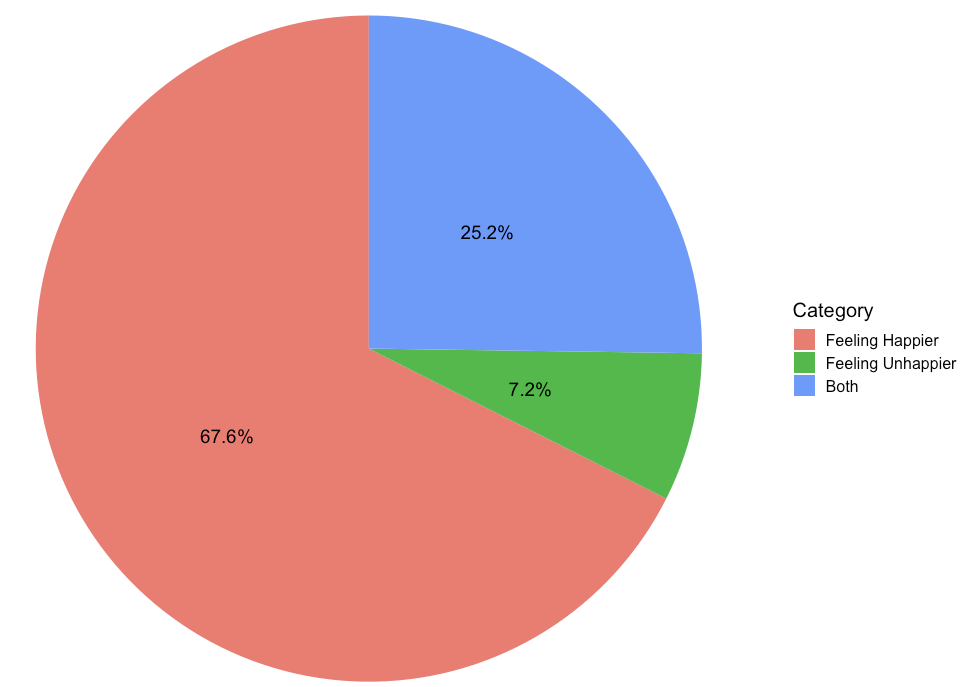
Figure 3: Effect of social media usage on life
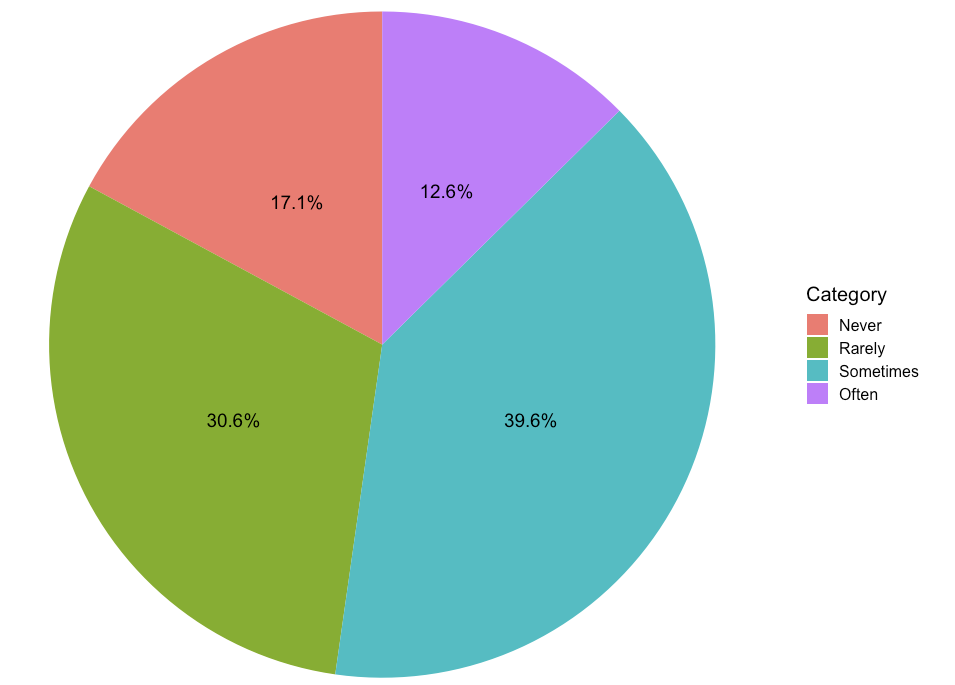
Figure 4: Effect of social media usage on sleep quality.
Notes: Pie chart displaying the percentage of people (total n = 111) indicating the effect of SMU on life (top) and on sleep quality (bottom).
4. Discussion
The current study investigated the relationship between SMU, depression, and sleep health among adolescents. It involved assessing participants' levels of social media use, depressive symptoms, and various sleep health metrics such as sleep duration and quality. Consistent with previous research, a significant negative correlation was found between depression and sleep health indices (i.e., sleep duration and sleep quality). This aligns with findings from Roberts and Duong, who examined a sample of 4,175 adolescents and found that those with higher levels of depression reported significantly shorter sleep durations and poorer sleep quality compared to their peers [7]. Similarly, a study by Lovato and Gradisar involving 386 adolescents revealed that depressive symptoms were strongly linked to increased sleep onset latency and decreased sleep efficiency [8]. Moreover, other research has highlighted several potential mechanisms underlying this relationship. For example, a study by Baglioni and colleagues with a sample of 1,257 adults found that depression is often associated with heightened physiological arousal and increased stress hormone levels, which can interfere with the ability to fall and stay asleep [9].
High school students often get significantly less sleep compared to undergraduates, a trend particularly pronounced in China due to the pressures of the National College Entrance Examination (Gaokao). The Gaokao is an exam that largely determines a Chinese student's future academic performances and career opportunities, necessitating comprehensive preparation. As a result, high school students typically have rigorous academic schedules, long school hours, extensive homework, and additional tutoring sessions. This leaves them with little time for adequate sleep.
Interestingly, our study found that SMU did not significantly impact sleep quality and depression symptoms, which might be due to the objective measurement methods used not capturing subtle effects. Despite many participants reporting in self-reports that SMU affects their sleep and mental health, these subjective perceptions may be influenced by other factors such as psychological state. Additionally, the impact of social media on sleep and mental health can vary widely among individuals, necessitating more refined research designs and in-depth qualitative analysis to comprehensively understand its complex mechanisms of influence.
Recognizing the seriousness of this issue, it is imperative for parents, educators, and healthcare professionals to remain vigilant and proactive in monitoring the social media usage patterns of adolescents. Regularly assessing the severity of any depressive symptoms and intervening early can help mitigate the negative impact of social media on mental health. By fostering open communication, providing support, and promoting healthy online habits, we can empower young people to navigate social media in a way that preserves their mental well-being and fosters positive self-esteem. Ultimately, addressing the relationship between social media usage and depression among adolescents is paramount for safeguarding their overall health and happiness.
5. Conclusion
This study investigated the relationships between SMU, depression, and sleep health among adolescents. Higher levels of depression are consistently associated with poorer sleep quality and shorter sleep duration. Specifically, symptoms of depression such as low mood, anxiety, and a diminished interest in daily activities often lead to difficulties in falling asleep, disrupted sleep cycles, and consequently reduced total sleep time and lower sleep quality. The negative impact of depression on sleep may also be related to physiological changes it induces.
However, the study reveals that the influence of social media use is more complex and less direct. Despite social media's significant role in adolescents' lives, its mechanism of affecting depression and sleep health is not clear. This finding suggests that the impact of social media may be moderated by various factors, rather than just its frequency of use or content. For example, the effects of social media use may vary depending on individual social networks and the quality of online interactions. Additionally, the lack of significant SMU mediation suggests that while social media is a prevalent part of adolescents’ lives, its underlying role in affecting depression and sleep health requires further investigation. This indicates that social media may not be a direct factor affecting adolescents' depression and sleep health, and its role may be more intricate, involving other potential moderating variables. For instance, the positive or negative interactions on social media might have different effects on adolescents' psychological states, potentially linked to their overall social support, life events, and coping strategies.
Therefore, although social media has become a part of adolescents' lives, its specific role in depression and sleep health still requires further investigation. Future research may need to examine more closely the specific patterns and content of social media use and its interactions with other life factors to fully understand its potential impacts on adolescents' mental and physical health.
References
[1]. Lin, L. Y., Sidani, J. E., Shensa, A., Radovic, A., Miller, E., Colditz, J. B., Hoffman, B. L., Giles, L. M., & Primack, B. A. (2016). ASSOCIATION BETWEEN SOCIAL MEDIA USE AND DEPRESSION AMONG U.S. YOUNG ADULTS. Depression and anxiety, 33(4), 323–331. https://doi.org/10.1002/da.22466
[2]. Levenson, J. C., Shensa, A., Sidani, J. E., Colditz, J. B., & Primack, B. A. (2016). The association between social media use and sleep disturbance among young adults. Preventive medicine, 85, 36–41. https://doi.org/10.1016/j.ypmed.2016.01.001
[3]. Orzech, K. M., Grandner, M. A., Roane, B. M., & Carskadon, M. A. (2016). Digital media use in the 2 h before bedtime is associated with sleep variables in university students. Computers in human behavior, 55(A), 43–50. https://doi.org/10.1016/j.chb.2015.08.049
[4]. Zung, W.W. (1965). A self-rating depression scale. Arch Gen Psychiatry, 12, 63-70. https://doi:10.1001/archpsyc.1965.01720310065008
[5]. Buysse, D. J., Reynolds, C. F., 3rd, Monk, T. H., Berman, S. R., & Kupfer, D. J. (1989). The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry research, 28(2), 193–213. https://doi.org/10.1016/0165-1781(89)90047-4
[6]. Alkis, Y., Kadirhan, Z., & Sat, M. (2017). Development and validation of social anxiety scale for social media users. Computers in Human Behavior, 72, 296-303. https://doi.org/10.1016/j.chb.2017.03.011
[7]. Roberts, R. E., & Duong, H. T. (2014). The prospective association between sleep deprivation and depression among adolescents. Sleep, 37(2), 239–244. https://doi.org/10.5665/sleep.3388
[8]. Lovato, N., & Gradisar, M. (2014). A meta-analysis and model of the relationship between sleep and depression in adolescents: recommendations for future research and clinical practice. Sleep medicine reviews, 18(6), 521–529. https://doi.org/10.1016/j.smrv.2014.03.006
[9]. Baglioni, C., Battagliese, G., Feige, B., Spiegelhalder, K., Nissen, C., Voderholzer, U., Lombardo, C., & Riemann, D. (2011). Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. Journal of affective disorders, 135(1-3), 10–19. https://doi.org/10.1016/j.jad.2011.01.011
Cite this article
Xiao,Y. (2024). Investigating the Relationship Between Sleep Health, Depression, and Social Media Usage among Adolescents. Lecture Notes in Education Psychology and Public Media,64,21-28.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 2nd International Conference on Global Politics and Socio-Humanities
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Lin, L. Y., Sidani, J. E., Shensa, A., Radovic, A., Miller, E., Colditz, J. B., Hoffman, B. L., Giles, L. M., & Primack, B. A. (2016). ASSOCIATION BETWEEN SOCIAL MEDIA USE AND DEPRESSION AMONG U.S. YOUNG ADULTS. Depression and anxiety, 33(4), 323–331. https://doi.org/10.1002/da.22466
[2]. Levenson, J. C., Shensa, A., Sidani, J. E., Colditz, J. B., & Primack, B. A. (2016). The association between social media use and sleep disturbance among young adults. Preventive medicine, 85, 36–41. https://doi.org/10.1016/j.ypmed.2016.01.001
[3]. Orzech, K. M., Grandner, M. A., Roane, B. M., & Carskadon, M. A. (2016). Digital media use in the 2 h before bedtime is associated with sleep variables in university students. Computers in human behavior, 55(A), 43–50. https://doi.org/10.1016/j.chb.2015.08.049
[4]. Zung, W.W. (1965). A self-rating depression scale. Arch Gen Psychiatry, 12, 63-70. https://doi:10.1001/archpsyc.1965.01720310065008
[5]. Buysse, D. J., Reynolds, C. F., 3rd, Monk, T. H., Berman, S. R., & Kupfer, D. J. (1989). The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry research, 28(2), 193–213. https://doi.org/10.1016/0165-1781(89)90047-4
[6]. Alkis, Y., Kadirhan, Z., & Sat, M. (2017). Development and validation of social anxiety scale for social media users. Computers in Human Behavior, 72, 296-303. https://doi.org/10.1016/j.chb.2017.03.011
[7]. Roberts, R. E., & Duong, H. T. (2014). The prospective association between sleep deprivation and depression among adolescents. Sleep, 37(2), 239–244. https://doi.org/10.5665/sleep.3388
[8]. Lovato, N., & Gradisar, M. (2014). A meta-analysis and model of the relationship between sleep and depression in adolescents: recommendations for future research and clinical practice. Sleep medicine reviews, 18(6), 521–529. https://doi.org/10.1016/j.smrv.2014.03.006
[9]. Baglioni, C., Battagliese, G., Feige, B., Spiegelhalder, K., Nissen, C., Voderholzer, U., Lombardo, C., & Riemann, D. (2011). Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. Journal of affective disorders, 135(1-3), 10–19. https://doi.org/10.1016/j.jad.2011.01.011