1. Introduction
Social cognition refers to the cognitive processes needed to understand the behavioural intentions of oneself and others in social situations [1, 2]. It was found that impairments in social cognition are observed in various neurological, psychiatric, and developmental disorders, including Major Depressive Disorder (MDD) [3]. MDD is the most common stress-related mood disorder characterised by a persistently depressed mood and loss of interest and pleasure in life [4]. Although there is increasing interest in understanding how social cognition deficits contribute to the common psycho-social disabilities in MDD, the relationship between MDD and high-order social cognition abilities (i.e., mentalization and metacognition) remains under investigation. Understanding the role of mentalization and metacognition in MDD is crucial for delivering effective therapy and improving functional outcomes for MDD patients. This paper aims to provide a holistic review of the existing evidence on mentalization and metacognition in patients with MDD.
2. The Concept of Social Cognition, Mentalization and Metacognition
Social cognition is a complex multifaceted construct, which can be divided into three categories with increasing complexity and synthesis. It was proposed that lower-order social cognition concerns the ability to identify, categorise and exhibit affective stimuli, such as the interpretation of facial expressions [5]. Lower-order social cognition is generally fast, unconscious, and domain-specific. Furthermore, intermediate-level social cognition involves perspective-taking or theory of mind (ToM), which is characterised by the capacity to ascribe mental states to others and make inferences about their beliefs, desires, intentions, emotions, and thoughts [6, 7]. Besides, social perception is another important aspect of intermediate-level social cognition, which involves making inferences about others based on their behaviours and the situation [8]. Finally, higher-order social cognition involves the meta-state representations of the mental and affective states of oneself or others [9, 10]. This level of social cognition is controlled, imaginative, and demanding. Two distinct processes are involved in higher-order social cognition, namely mentalization and metacognition [11, 12].
Mentalization is generally defined as the mental ability by which an individual monitors, interprets, and understands human behaviours in terms of their cognitive processes [13]. However, certain inconsistencies have been identified in the operationalization of mentalization across various studies. For instance, there is a debate regarding whether mentalization captures the same concept with the Theory of Mind (ToM). The first definition of mentalization was introduced by Peter Fonagy [11], and operationalised by developmental researchers investigating ToM [14]. Therefore, earlier studies often used the term mentalization and ToM interchangeably to describe the understanding of others’ behaviours in terms of their mental states. However, as the concept evolved, mentalization and ToM are now recognised as capturing distinct levels of social cognition. While ToM involves the semantic representation of others’ experiences through reasoning, mentalization requires relational and emotional representations in terms of desires, needs, feelings, and beliefs in addition to reasoning [15]. In a succinct manner, mentalization involves self-reflective and interpersonal components that are not captured by ToM. The current paper will refer to the matured definition of mentalization by examining it as an independent concept from ToM. Besides concept distinction from ToM, the orientation of mentalization also received considerable debate. While some researchers believe mentalization involves imagining the mental state of oneself and others [16], others believe it is oriented towards others only. Quoting Fonagy and Allison, who introduced the concept, mentalization involves “Infer others’ mental states from subtle behavioural and contextual cues” [17]. For the purpose of drawing concepts distinction from metacognition, the current paper will refer to mentalization as the understanding of others’ mental states.
On the contrary, metacognition is often succinctly defined as “thinking about thinking” [18]. It involves the awareness and understanding of one’s own cognitive processes and conscious executive control through self-monitoring and self-regulation [19, 20]. Mentalization and metacognition are two distinct aspects of high-order social cognition. Not only do they differ in orientations (i.e., towards oneself or others), but they also exhibit distinct underlying neurological processes. A recent study examined the underlying neural representations of metacognition and mentalization during decision-making [21]. Using three functional magnetic resonance imaging (fMRI) experiments, the authors identified neural signatures of mentalization and metacognition. While the former was mainly represented in the right inferior parietal lobe (IPL) and the dorsomedial prefrontal cortex, the latter was processed in the dorsal anterior cingulate cortex (dACC).
Mentalization and metacognition are both perceived to play a crucial role in MDD from theoretical and clinical perspectives. For instance, mentalization and metacognition ability are important for realistic evaluations of oneself and relationships with others [22]. Since MDD is often characterised by consistent negative self-focused rumination and deficits in social relationships [22], these symptoms do converge with deficits in mentalization and metacognition to a large extent. Therefore, the relationship between MDD, mentalization and metacognition has attracted considerable interest from researchers. The empirical evidence will be described and evaluated in detail in the following sections.
3. Association Between MDD and Mentalization
The first supporting evidence for the correlation between mentalization and MDD came from Fisher-Kern et al. [23, 24]. The mentalization ability among chronic MDD female inpatients and healthy controls was examined using the Reflective Functioning Scale (RFS) [25], the most prominent measure of mentalization with high inter-rater reliability [26]. The mentalization capacity was found to be severely impaired in MDD patients compared to healthy controls. About 80% of MDD patients were classified as having a complete lack of mentalization or low mentalization. However, all patients were taking pharmacological treatments at the time of the assessment, which could have compromised the internal validity of the finding. On the contrary, Taubner et al. [27] failed to replicate the previous finding [23] utilising the same assessments. No significant difference in mentalization was detected between chronic MDD patients and their matched healthy controls, although MDD patients tended to have lower RF scores concerning the issue of loss.
The difference in results of the two studies could potentially be attributed to the different samples employed. The clinical samples in Fisher-Kern et al. [24] and Taubner et al. [27] differed in functioning level and comorbidity. While the former employed more severely comorbid and low-functioning inpatients samples, MDD patients in the latter were stable enough for regular outpatient therapy. Therefore, the low mentalization capacity in MDD patients [24] could reflect low social functioning in general rather than impaired mentalization. Additionally, the healthy control in Taubner et al. [27] demonstrated a low average RF score, potentially attributed to the prevalent insecure and disorganized attachment representations among this small sample. Therefore, the control sample’s failure to represent the general population may have contributed to the non-significant finding. Nonetheless, the convergent discoveries in both studies have provided important insights into the role of mentalization in MDD. For instance, RF scores did not correlate with measures of depression symptom severity in either study. Since this finding was consistent across different samples and different assessments of symptom severity, it granted reliability to the finding that mentalization ability impairment may reflect chronicity rather than the severity of MDD.
Other empirical evidence on the relationship between MDD and mentalization mainly came from studies on therapeutic outcomes. Bressi et al. [22] examined the RF scores of MDD patients before, after, and at a one-year follow-up of psychotherapy with a special focus targeting mentalization (STAMP). The authors found that baseline RFS was predictive of therapeutic outcomes. Patients with lower RFS showed fewer improvements in depressive symptoms than those with relatively higher RFS. This finding underlined an important relationship between mentalization ability and MDD by highlighting the mediating role of mentalization in MDD treatment outcomes. Similar results were derived from a longitudinal study investigating the association between RF scores, symptomatic distress, and depression symptom severity, along with other factors [28]. The authors found a significant association between the improvement in RF and the reduction of depressive symptoms. This finding reinforced the close association between mentalization ability and MDD, adding to the reliability of [19]. However, whether mentalization directly influences MDD or functions as a moderator remains unknown from studies investigating therapeutic outcomes.
4. Association Between MDD and Metacognition
The study conducted by Ladegaard et al. [5] has provided direct evidence of the correlation between MDD and metacognition. Along with other measures, the authors compared the metacognition ability (operationalised as the score of Metacognition Assessment Scale-Abbreviated [29]) between MDD outpatients and matched healthy controls. Impairment in all domains of higher-order social cognitive ability was found among MDD patients, including metacognition ability. Although MDD patients in this study were generally able to express their thoughts and feelings, they struggled to understand the relationship among thoughts, feelings, behaviours, and interpersonal processes within events in their lives, highlighting the metacognition impairments. The significance of social cognitive impairment was retained after controlling for possible covariates, including neurocognition, suggesting the high internal validity of the finding.
Another line of supporting evidence came from decision-making tasks [30]. In this experiment, MDD patients and healthy controls were instructed to indicate whether they agreed with attitude statements shown on the computer task by pressing computer keys. Three different attitude statements were presented, including functional, dysfunctional, and neutral statements. Participants’ mean reaction times for different statements were recorded and analysed. As shown in Figure 1 [30], while the healthy control showed slower agreements with dysfunctional statements and slower disagreements with functional statements, this pattern was absent in MDD patients. Since faster reaction time often reflects a relatively more autonomous and schematic response, this finding suggested that MDD patients had a relative lack of metacognitive monitoring of dysfunctional contents in depression.
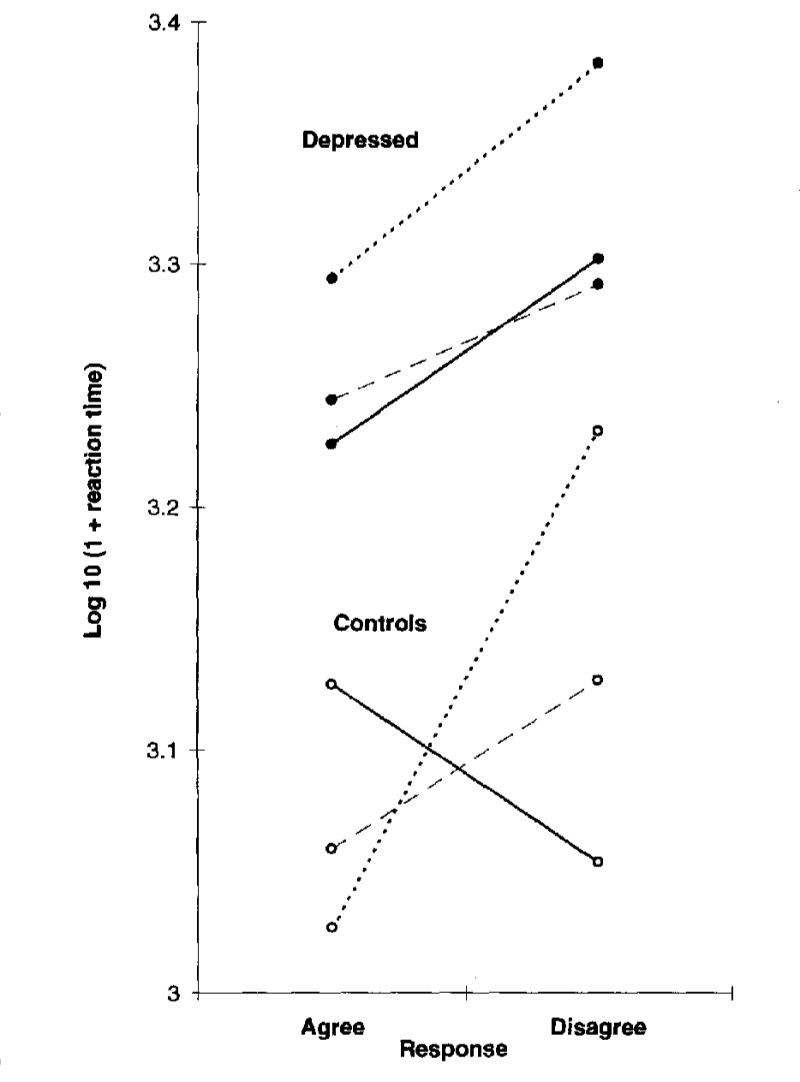
Figure 1: Transformed response latencies (milliseconds) for agreement and disagreement with the functional statement (dotted line), dysfunctional statement (solid line), and neutral statement (dashed line) [30].
Finally, most investigations on the relationship between MDD and metacognition have come from studies examining therapeutic outcomes. Hjemdal et al. [31] introduced MDD patients to therapy that targeted metacognition ability (metacognitive therapy [MCT]) and measured their symptoms of depression, metacognition, anxiety and rumination before, post-treatment and at six-month follow-up. All patients in this study have recovered from MDD following the treatment, highlighting the importance of metacognition ability in MDD. More importantly, 70% of patients fully recovered at the six-month follow-up, suggesting the long-term impact of MCT. Callesen et al. [32] also detected the long-term benefit of improved metacognition on MDD patients, adding to the reliability of [31]. The long-term benefit of improved metacognition ability further underscored the close association between MDD and metacognition. Moreover, Winter et al. [33] further emphasised the consistency of the finding across subgroups of MDD by demonstrating that the same pattern was comparable between current and persistent depressive patients.
5. Conclusion
Ultimately, the current paper examined the relationship between MDD and high-order social cognition abilities, including mentalization and metacognition. The majority of evidence reviewed by the current paper has underlined the relationship between mentalization capacity and MDD chronicity. However, the presence of conflicting perspectives within the field coupled with the limited number of replication studies implies that this finding should be interpreted with caution. Future research should compare mentalization ability among MDD patients to larger control samples with normal mentalization capacity to enhance the validity of the existing evidence. On the contrary, a close relationship between MDD and metacognition was consistently highlighted in correlation and decision-making studies, alongside with long-term benefit of improved metacognition following MDD treatments.
Furthermore, studies investigating therapeutic outcomes have provided some idea about the direction of the association between MDD, mentalization and metacognition. Mentalization capacity has been identified as a significant moderator of treatment outcomes. Similarly, the level of metacognitive ability was also found to influence MDD symptoms and diagnosis by longitudinal studies. However, whether high-order social cognition deficits serve a predictive value of MDD onset or merely a mediation of symptom severity remains unknown with studies on therapeutic outcomes. Future evidence from developmental studies will enhance our understanding of the degrees of social cognition deficits’ impact on MDD. Furthermore, neuroimaging studies could also benefit the field of study by revealing the underlying neural mechanisms behind mentalization and metacognition abilities among MDD patients.
References
[1]. Fiske, S. T., & Taylor, S. E. (1991). Social Cognition. McGraw-Hill Humanities, Social Sciences & World Languages.
[2]. Ochsner, K. N., & Gross, J. J. (2008). Cognitive Emotion Regulation. Current Directions in Psychological Science, 17(2), 153–158. https://doi.org/10.1111/j.1467-8721.2008.00566.x.
[3]. Cotter, J., Granger, K., Backx, R., Hobbs, M., Looi, C. Y., & Barnett, J. H. (2018). Social cognitive dysfunction as a clinical marker: A systematic review of meta-analyses across 30 clinical conditions. Neuroscience & Biobehavioral Reviews, 84, 92–99. https://doi.org/10.1016/j.neubiorev.2017.11.014.
[4]. Fava, M., & Kendler, K. S. (2000). Major Depressive Disorder. Neuron, 28(2), 335–341. https://doi.org/10.1016/s0896-6273(00)00112-4.
[5]. Ladegaard, N., Larsen, E., Videbech, P., & Lysaker, P. H. (2014). Higher-order social cognition in first-episode major depression. Psychiatry Research-neuroimaging, 216(1), 37–43. https://doi.org/10.1016/j.psychres.2013.12.010.
[6]. Premack, D., & Woodruff, G. (1978). Does the chimpanzee have a theory of mind? Behavioral and Brain Sciences, 1(4), 515–526. https://doi.org/10.1017/s0140525x00076512.
[7]. Brüne, M. (2003). Theory of mind and the role of IQ in chronic disorganized schizophrenia. Schizophrenia Research, 60(1), 57–64. https://doi.org/10.1016/s0920-9964(02)00162-7.
[8]. Social Perception. (2023). APA Dictionary of Psychology. https://dictionary.apa.org/social-perception.
[9]. Semerari, A., Carcione, A., Dimaggio, G., Falcone, M., Nicolò, G., Procacci, M., & Alleva, G. (2003). How to evaluate metacognitive functioning in psychotherapy? The metacognition assessment scale and its applications. Clinical Psychology & Psychotherapy, 10(4), 238–261. https://doi.org/10.1002/cpp.362.
[10]. Dimaggio, G., & Lysaker, P. H. (Eds.). (2010). Metacognition and severe adult mental disorders: From research to treatment. Routledge/Taylor & Francis Group.
[11]. Fonagy, P. (1989). On Tolerating Mental States: Theory of Mind in Borderline Patients. Bulletin of the Anna Freud Centre, 12, 91-115.
[12]. Flavell, J. H. (1976). Metacognitive Aspects of Problem Solving. In L. B. Resnick (Ed.), The Nature of Intelligence (pp. 231-235). Hillsdale, NJ: Lawrence Erlbaum Associates.
[13]. Fonagy, P., & Luyten, P. (2009). A developmental, mentalization-based approach to the understanding and treatment of borderline personality disorder. Development and Psychopathology, 21(4), 1355–1381. https://doi.org/10.1017/s0954579409990198.
[14]. Leslie, A. M. (1987). Pretense and representation: The origins of “theory of mind.” Psychological Review, 94(4), 412–426. https://doi.org/10.1037/0033-295x.94.4.412.
[15]. Górska, D., & Marszał, M. (2014). [Mentalization and theory of mind in borderline personality organization: exploring the differences between affective and cognitive aspects of social cognition in emotional pathology]. Psychiatria Polska, 48(3), 503–513.
[16]. Choi-Kain, L. W., & Gunderson, J. G. (2008). Mentalization: Ontogeny, Assessment, and Application in the Treatment of Borderline Personality Disorder. American Journal of Psychiatry, 165(9), 1127–1135. https://doi.org/10.1176/appi.ajp.2008.07081360.
[17]. Fonagy, P., & Allison, E. (2012). What is mentalization? The concept and its foundations in developmental research. Routledge eBooks, 25–48. https://doi.org/10.4324/9780203123003-8.
[18]. Flavell, J. H. (1979). Metacognition and cognitive monitoring: A new area of cognitive–developmental inquiry. American Psychologist, 34(10), 906–911. https://doi.org/10.1037/0003-066x.34.10.906.
[19]. McLeod, L. (1997). Young Children and Metacognition: Do we know what they know they Know? And if so, What do we do about it? Australian Journal of Early Childhood, 22(2), 6–11. https://doi.org/10.1177/183693919702200203.
[20]. Lockl, K., & Schneider, W. (2002). Developmental trends in children’s feeling-of-knowing judgements. International Journal of Behavioral Development, 26(4), 327–333. https://doi.org/10.1080/01650250143000210.
[21]. Jiang, S., Wang, S., & Wan, X. (2022). Metacognition and mentalizing are associated with distinct neuralrepresentations of decision uncertainty. PLOS Biology, 20(5), e3001301. https://doi.org/10.1371/journal.pbio.3001301.
[22]. Bressi, C., Fronza, S., Minacapelli, E., Nocito, E., Dipasquale, E., Magri, L., Lionetti, F., & Barone, L. (2015). Short-Term Psychodynamic Psychotherapy with Mentalization-Based Techniques in Major Depressive Disorder patients: Relationship among alexithymia, reflective functioning, and outcome variables - A Pilot study. British Journal of Medical Psychology, 90(3), 299–313. https://doi.org/10.1111/papt.12110.
[23]. Fischer-Kern, M., Tmej, A., Kapusta, N. D., Naderer, A., Leithner-Dziubas, K., Löffler-Stastka, H., & Springer-Kremser, M. (2008). Mentalisierungsfähigkeit bei depressiven Patientinnen: Eine Pilotstudie. Zeitschrift Fur Psychosomatische Medizin Und Psychotherapie, 54(4), 368–380. https://doi.org/10.13109/zptm.2008.54.4.368.
[24]. Fischer-Kern, M., Fonagy, P., Kapusta, N. D., Luyten, P., Boss, S. J., Naderer, A., Blüml, V., & Leithner, K. (2013). Mentalizing in Female Inpatients With Major Depressive Disorder. Journal of Nervous and Mental Disease, 201(3), 202–207. https://doi.org/10.1097/nmd.0b013e3182845c0a.
[25]. Fonagy, P., Target, M., Steele, H., & Steele, M. A. (1998). Reflective Functioning Scale. PsycTESTS Dataset. https://doi.org/10.1037/t03490-000.
[26]. Fonagy, P., Leigh, T., Steele, M., Steele, H., Kennedy, R. L., Mattoon, G., Target, M., & Gerber, A. J. (1996). The relation of attachment status, psychiatric classification, and response to psychotherapy. Journal of Consulting and Clinical Psychology, 64(1), 22–31. https://doi.org/10.1037/0022-006x.64.1.22.
[27]. Taubner, S., Kessler, H., Buchheim, A., Kächele, H., & Staun, L. (2011). The Role of Mentalization in the Psychoanalytic Treatment of Chronic Depression. Psychiatry MMC, 74(1), 49–57. https://doi.org/10.1521/psyc.2011.74.1.49.
[28]. Babl, A., Berger, T., Decurtins, H., Gross, I., Frey, T., Caspar, F., & Taubner, S. (2022). A longitudinal analysis of reflective functioning and its association with psychotherapy outcome in patients with depressive and anxiety disorders. Journal of Counseling Psychology, 69(3), 337–347. https://doi.org/10.1037/cou0000587.
[29]. Lysaker, P. H., Chernov, N., Tn, M., Sozinova, M., Dmitryeva, N., Alyoshin, V., Faith, L. A., Karpenko, O., & Kostyuk, G. P. (2021). Metacognition Assessment Scale--Abbreviated; Russian Version. PsycTESTS Dataset. https://doi.org/10.1037/t79885-000.
[30]. Sheppard, L. C., & Teasdale, J. R. (2000). Dysfunctional thinking in major depressive disorder: A deficit in metacognitive monitoring? Journal of Abnormal Psychology, 109(4), 768–776. https://doi.org/10.1037/0021-843x.109.4.768.
[31]. Hjemdal, O., Hagen, R., Solem, S., Nordahl, H., Kennair, L. E. O., Ryum, T., Nordahl, H. M., & Wells, A. (2017). Metacognitive Therapy in Major Depression: An Open Trial of Comorbid Cases. Cognitive and Behavioral Practice, 24(3), 312–318. https://doi.org/10.1016/j.cbpra.2016.06.006.
[32]. Callesen, P., Reeves, D., Heal, C., & Wells, A. (2020). Metacognitive Therapy versus Cognitive Behaviour Therapy in Adults with Major Depression: A Parallel Single-Blind Randomised Trial. Scientific Reports, 10(1). https://doi.org/10.1038/s41598-020-64577-1.
[33]. Winter, L., Gottschalk, J., Nielsen, J., Wells, A., Schweiger, U., & Kahl, K. G. (2019). A Comparison of Metacognitive Therapy in Current Versus Persistent Depressive Disorder – A Pilot Outpatient Study. Frontiers in Psychology. https://doi.org/10.3389/fpsyg.2019.01714.
Cite this article
Chen,C.A. (2023). Metacognition and Mentalization in Patients with Major Depressive Disorder. Lecture Notes in Education Psychology and Public Media,15,1-7.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 4th International Conference on Educational Innovation and Philosophical Inquiries
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Fiske, S. T., & Taylor, S. E. (1991). Social Cognition. McGraw-Hill Humanities, Social Sciences & World Languages.
[2]. Ochsner, K. N., & Gross, J. J. (2008). Cognitive Emotion Regulation. Current Directions in Psychological Science, 17(2), 153–158. https://doi.org/10.1111/j.1467-8721.2008.00566.x.
[3]. Cotter, J., Granger, K., Backx, R., Hobbs, M., Looi, C. Y., & Barnett, J. H. (2018). Social cognitive dysfunction as a clinical marker: A systematic review of meta-analyses across 30 clinical conditions. Neuroscience & Biobehavioral Reviews, 84, 92–99. https://doi.org/10.1016/j.neubiorev.2017.11.014.
[4]. Fava, M., & Kendler, K. S. (2000). Major Depressive Disorder. Neuron, 28(2), 335–341. https://doi.org/10.1016/s0896-6273(00)00112-4.
[5]. Ladegaard, N., Larsen, E., Videbech, P., & Lysaker, P. H. (2014). Higher-order social cognition in first-episode major depression. Psychiatry Research-neuroimaging, 216(1), 37–43. https://doi.org/10.1016/j.psychres.2013.12.010.
[6]. Premack, D., & Woodruff, G. (1978). Does the chimpanzee have a theory of mind? Behavioral and Brain Sciences, 1(4), 515–526. https://doi.org/10.1017/s0140525x00076512.
[7]. Brüne, M. (2003). Theory of mind and the role of IQ in chronic disorganized schizophrenia. Schizophrenia Research, 60(1), 57–64. https://doi.org/10.1016/s0920-9964(02)00162-7.
[8]. Social Perception. (2023). APA Dictionary of Psychology. https://dictionary.apa.org/social-perception.
[9]. Semerari, A., Carcione, A., Dimaggio, G., Falcone, M., Nicolò, G., Procacci, M., & Alleva, G. (2003). How to evaluate metacognitive functioning in psychotherapy? The metacognition assessment scale and its applications. Clinical Psychology & Psychotherapy, 10(4), 238–261. https://doi.org/10.1002/cpp.362.
[10]. Dimaggio, G., & Lysaker, P. H. (Eds.). (2010). Metacognition and severe adult mental disorders: From research to treatment. Routledge/Taylor & Francis Group.
[11]. Fonagy, P. (1989). On Tolerating Mental States: Theory of Mind in Borderline Patients. Bulletin of the Anna Freud Centre, 12, 91-115.
[12]. Flavell, J. H. (1976). Metacognitive Aspects of Problem Solving. In L. B. Resnick (Ed.), The Nature of Intelligence (pp. 231-235). Hillsdale, NJ: Lawrence Erlbaum Associates.
[13]. Fonagy, P., & Luyten, P. (2009). A developmental, mentalization-based approach to the understanding and treatment of borderline personality disorder. Development and Psychopathology, 21(4), 1355–1381. https://doi.org/10.1017/s0954579409990198.
[14]. Leslie, A. M. (1987). Pretense and representation: The origins of “theory of mind.” Psychological Review, 94(4), 412–426. https://doi.org/10.1037/0033-295x.94.4.412.
[15]. Górska, D., & Marszał, M. (2014). [Mentalization and theory of mind in borderline personality organization: exploring the differences between affective and cognitive aspects of social cognition in emotional pathology]. Psychiatria Polska, 48(3), 503–513.
[16]. Choi-Kain, L. W., & Gunderson, J. G. (2008). Mentalization: Ontogeny, Assessment, and Application in the Treatment of Borderline Personality Disorder. American Journal of Psychiatry, 165(9), 1127–1135. https://doi.org/10.1176/appi.ajp.2008.07081360.
[17]. Fonagy, P., & Allison, E. (2012). What is mentalization? The concept and its foundations in developmental research. Routledge eBooks, 25–48. https://doi.org/10.4324/9780203123003-8.
[18]. Flavell, J. H. (1979). Metacognition and cognitive monitoring: A new area of cognitive–developmental inquiry. American Psychologist, 34(10), 906–911. https://doi.org/10.1037/0003-066x.34.10.906.
[19]. McLeod, L. (1997). Young Children and Metacognition: Do we know what they know they Know? And if so, What do we do about it? Australian Journal of Early Childhood, 22(2), 6–11. https://doi.org/10.1177/183693919702200203.
[20]. Lockl, K., & Schneider, W. (2002). Developmental trends in children’s feeling-of-knowing judgements. International Journal of Behavioral Development, 26(4), 327–333. https://doi.org/10.1080/01650250143000210.
[21]. Jiang, S., Wang, S., & Wan, X. (2022). Metacognition and mentalizing are associated with distinct neuralrepresentations of decision uncertainty. PLOS Biology, 20(5), e3001301. https://doi.org/10.1371/journal.pbio.3001301.
[22]. Bressi, C., Fronza, S., Minacapelli, E., Nocito, E., Dipasquale, E., Magri, L., Lionetti, F., & Barone, L. (2015). Short-Term Psychodynamic Psychotherapy with Mentalization-Based Techniques in Major Depressive Disorder patients: Relationship among alexithymia, reflective functioning, and outcome variables - A Pilot study. British Journal of Medical Psychology, 90(3), 299–313. https://doi.org/10.1111/papt.12110.
[23]. Fischer-Kern, M., Tmej, A., Kapusta, N. D., Naderer, A., Leithner-Dziubas, K., Löffler-Stastka, H., & Springer-Kremser, M. (2008). Mentalisierungsfähigkeit bei depressiven Patientinnen: Eine Pilotstudie. Zeitschrift Fur Psychosomatische Medizin Und Psychotherapie, 54(4), 368–380. https://doi.org/10.13109/zptm.2008.54.4.368.
[24]. Fischer-Kern, M., Fonagy, P., Kapusta, N. D., Luyten, P., Boss, S. J., Naderer, A., Blüml, V., & Leithner, K. (2013). Mentalizing in Female Inpatients With Major Depressive Disorder. Journal of Nervous and Mental Disease, 201(3), 202–207. https://doi.org/10.1097/nmd.0b013e3182845c0a.
[25]. Fonagy, P., Target, M., Steele, H., & Steele, M. A. (1998). Reflective Functioning Scale. PsycTESTS Dataset. https://doi.org/10.1037/t03490-000.
[26]. Fonagy, P., Leigh, T., Steele, M., Steele, H., Kennedy, R. L., Mattoon, G., Target, M., & Gerber, A. J. (1996). The relation of attachment status, psychiatric classification, and response to psychotherapy. Journal of Consulting and Clinical Psychology, 64(1), 22–31. https://doi.org/10.1037/0022-006x.64.1.22.
[27]. Taubner, S., Kessler, H., Buchheim, A., Kächele, H., & Staun, L. (2011). The Role of Mentalization in the Psychoanalytic Treatment of Chronic Depression. Psychiatry MMC, 74(1), 49–57. https://doi.org/10.1521/psyc.2011.74.1.49.
[28]. Babl, A., Berger, T., Decurtins, H., Gross, I., Frey, T., Caspar, F., & Taubner, S. (2022). A longitudinal analysis of reflective functioning and its association with psychotherapy outcome in patients with depressive and anxiety disorders. Journal of Counseling Psychology, 69(3), 337–347. https://doi.org/10.1037/cou0000587.
[29]. Lysaker, P. H., Chernov, N., Tn, M., Sozinova, M., Dmitryeva, N., Alyoshin, V., Faith, L. A., Karpenko, O., & Kostyuk, G. P. (2021). Metacognition Assessment Scale--Abbreviated; Russian Version. PsycTESTS Dataset. https://doi.org/10.1037/t79885-000.
[30]. Sheppard, L. C., & Teasdale, J. R. (2000). Dysfunctional thinking in major depressive disorder: A deficit in metacognitive monitoring? Journal of Abnormal Psychology, 109(4), 768–776. https://doi.org/10.1037/0021-843x.109.4.768.
[31]. Hjemdal, O., Hagen, R., Solem, S., Nordahl, H., Kennair, L. E. O., Ryum, T., Nordahl, H. M., & Wells, A. (2017). Metacognitive Therapy in Major Depression: An Open Trial of Comorbid Cases. Cognitive and Behavioral Practice, 24(3), 312–318. https://doi.org/10.1016/j.cbpra.2016.06.006.
[32]. Callesen, P., Reeves, D., Heal, C., & Wells, A. (2020). Metacognitive Therapy versus Cognitive Behaviour Therapy in Adults with Major Depression: A Parallel Single-Blind Randomised Trial. Scientific Reports, 10(1). https://doi.org/10.1038/s41598-020-64577-1.
[33]. Winter, L., Gottschalk, J., Nielsen, J., Wells, A., Schweiger, U., & Kahl, K. G. (2019). A Comparison of Metacognitive Therapy in Current Versus Persistent Depressive Disorder – A Pilot Outpatient Study. Frontiers in Psychology. https://doi.org/10.3389/fpsyg.2019.01714.