1. Introduction
Artificial wombs, as a frontier in reproductive technology, have garnered attention for their potential to revolutionize neonatal care and human reproduction. This technology, often referred to as ectogenesis, involves the use of a highly controlled external environment to simulate the conditions of a natural womb, allowing a fetus to develop outside of a biological mother’s body. The primary aim is to provide optimal support for extremely premature infants, offering them a safer and more controlled developmental environment than traditional neonatal intensive care units (NICUs)[1]. However, artificial wombs also raise numerous social, ethical, and scientific questions about the future of human reproduction, family dynamics, and child development.
Interest in artificial wombs has increased significantly with advancements in neonatal intensive care, which can now support infants born as early as 22 to 24 weeks[2]. Such extreme preterm births often lead to severe health complications due to the incomplete development of essential organs, especially the lungs and cardiovascular system. The mortality rate for such premature infants remains high, and even those who survive often face long-term health challenges. By mimicking the intrauterine environment more effectively than current methods, artificial wombs hold the potential to improve survival rates and reduce complications for preterm infants. In recent years, researchers have demonstrated early-stage artificial womb models, such as the “biobag,” which have shown promise in supporting fetal lambs during critical stages of their development, providing evidence of the viability of artificial gestation[3].
Despite this promise, artificial womb technology is still in the early stages of research and faces numerous hurdles. Biological, technical, and ethical issues must be addressed before artificial wombs can be used for human neonates, let alone for longer-term or full gestation outside of a natural womb. Moreover, the social and ethical implications extend beyond mere viability; the prospect of artificial gestation challenges traditional views of pregnancy, parenthood, and child welfare.
This review paper explores the current state of artificial womb technology, assessing the breakthroughs and limitations of recent research. The paper will also discuss the possible future developments in artificial womb technology, emphasizing the technological innovations and ethical frameworks needed to guide its responsible progression. The focus is not only on medical and technical challenges but also on how artificial wombs might redefine societal views on gestation and early-life care. By assessing the scientific progress and contemplating the societal implications, this paper aims to provide a comprehensive overview of the current and future state of artificial womb research.
2. Current Status of Artificial Womb Technology
2.1. Historical Development
The quest to create a viable artificial womb is rooted in the broader field of neonatal care, which has evolved remarkably over the past century. Neonatal incubation was first developed in the late 19th century, with the introduction of rudimentary incubators that allowed premature infants to survive outside the womb at increasingly earlier stages. These initial devices were groundbreaking but limited in their ability to mimic the comprehensive intrauterine environment. As a result, survival rates for extremely premature infants remained low, and those who survived often faced severe health complications due to underdeveloped organs and systems[4].
2.2. Technical Overview of Artificial Wombs
Creating an artificial womb requires the replication of a highly complex set of biological functions. The primary challenge is simulating the placenta, an organ that plays an essential role in nutrient exchange, oxygenation, and waste removal between the mother and the fetus. Artificial womb systems aim to replace these functions by creating a controlled environment in which the fetus can develop while receiving all necessary nutrients and oxygen through a synthetic, extracorporeal system.
Extracorporeal Membrane Oxygenation (ECMO) is currently one of the most crucial technologies in artificial womb research, as it allows blood oxygenation outside the body. ECMO has been adapted for use in artificial womb prototypes, where it substitutes for the fetal lungs until they are sufficiently developed to function on their own.
In 2017, a significant breakthrough came with the development of the “biobag,” a type of artificial womb that successfully gestated lamb fetuses to near-term, simulating the uterine environment with a clear, sterile bag filled with artificial amniotic fluid (Fig. 1). This fluid mimics the natural protection and nutrient-rich environment of the mother’s womb and is continuously replenished to remove waste and provide nutrients[5].
In addition to oxygenation, artificial wombs have to mimic the way of delivering nutrients that the placent would use. This requires a complex interface between the fetus and the machine that not only delivers nutrients but also removes metabolic waste products, a delicate balance that researchers are still optimizing [6].
Despite these advancements, there remain significant technical challenges, particularly in ensuring biocompatibility and preventing infection. For example, long-term ECMO usage is associated with risks of bleeding and infection, and researchers are actively exploring new materials and designs to address these limitations.
2.3. Recent Case Studies and Experiments
The most prominent demonstration of artificial womb technology thus far was the 2017 experiment at the Children’s Hospital of Philadelphia. In this study, researchers used a biobag system to gestate fetal lambs, successfully allowing them to develop to a stage equivalent to a human preterm infant at 23 to 24 weeks (Figure 1 & 2). The lambs survived for up to four weeks in this system, developing in a manner that closely mirrored normal in-womb growth. These lambs were able to grow without significant health issues, and their lungs and brains continued developing, suggesting that an artificial womb could indeed provide a feasible bridge for extremely preterm infants[2].
Another recent study conducted in Japan expanded on this research by exploring the use of artificial wombs for extended gestation in animal models[7]. The Japanese research team achieved similar results with goat fetuses, suggesting that artificial wombs may be applicable across a range of species, potentially including humans[8]. However, these studies are still in the early stages, and the transition from animal to human trials involves numerous regulatory and ethical hurdles.
Figure 1: Real Lamb Fetus Model Artificial Womb [9]
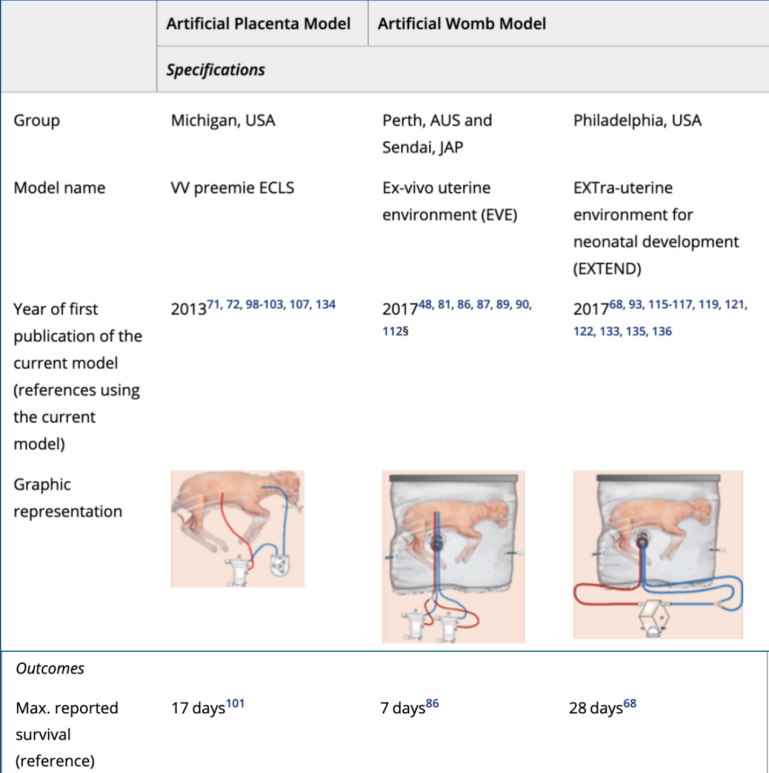
Figure 2: Recent Successful Model[7]
Figure 1 is a picture of what a real lamb fetus model artificial womb looks like. Figure 2 illustrates parts of information of recent successful animal models of artifical wombs. It shows clearly that in 2017, the model “EXTra-uterine environment for neonatal development(EXTEND)” had made the lamb fetus live for longer days compared to “VV preemie ECLS” in 2013 and “Ex-vivo uterine environment (EVE)”.
3. Applications and Implications of Artificial Womb Technology
3.1. Medical Applications
Artificial womb technology promises significant advancements in neonatal and reproductive medicine, primarily aimed at improving survival rates and outcomes for extremely premature infants. Neonatal intensive care units (NICUs) currently support infants born as early as 22 to 24 weeks, but even with advanced care, these preterm infants face high mortality rates and risk of severe developmental complications[10]. Artificial wombs could bridge this gap by providing a more stable, womb-like environment that reduces these risks, offering the potential to support fetal growth during the most vulnerable stages of development.
The core purpose of artificial wombs is to improve the viability of extremely premature infants by better simulating the intrauterine environment. During the late second and early third trimesters in the natural womb, vital stages of lung, brain, and immune system development take place, protected from external pathogens and nurtured in a precisely regulated environment. By enabling more gradual and controlled development, artificial wombs could prevent some long-term health complications commonly associated with premature birth, such as respiratory distress syndrome, cerebral palsy, and neurodevelopmental disorders. Studies have shown that preterm infants supported by artificial womb-like systems demonstrate more natural respiratory development compared to traditional NICU methods[11]. Thus, wombs could reduce reliance on ventilators and other invasive procedures, lowering the risk of infections and physical trauma.
Artificial wombs may also aid in fetal surgery, a field where surgeons operate on fetuses to correct life-threatening abnormalities while still in the womb. Artificial wombs could potentially support these surgeries by providing a more accessible, stable platform for intervention, followed by a secure environment that supports recovery and continued growth[12].
3.2. Socieical Implications and ethical issues
Beyond their medical applications, artificial wombs raise complex societal and ethical questions that challenge existing notions of reproduction, parenthood, and fetal rights. Unlike other reproductive technologies, artificial wombs would fundamentally alter the experience of pregnancy and gestation, with implications that extend to family dynamics, parental roles, and societal expectations around childbirth.
First, it’s about moral and religious objections. The concept of artificial wombs has sparked intense moral and religious debates. Many religious traditions view pregnancy and childbirth as a scarced and natural process ordained by a higher power. The idea of an artificial womb is seen by some as an interference with the natural order of life and a violation of sanctity of human reproduction. For example, in some Christain and Islamic teachings, the role of the mother’s womb in nurturing a new life is considered a central part of God’s plan[13, 14].
The ethical implications of artificially supporting human fetuses revolve around questions of autonomy, consent, and rights. Artificial wombs prompt new debates about when a fetus gains personhood and the rights associated with it, especially since an artificial womb might require novel regulatory approaches distinct from traditional NICU practices. Unlike traditional pregnancy the mother’s body serves as a physical and legal boundary, artificial gestation blurs this distinction, potentially necessitating unique rights and protections for the artificially gestated fetus[15].
Artificial wombs challenge the traditional experience of pregnancy, raising questions about parental roles. For instance, individuals who cannot carry a pregnancy, such as those with specific medical conditions or single fathers, might gain the opportunity to parent a biological child through artificial gestation. This could diversify family structmpower new forms of parenthood. At the same time, society must consider how the absence of a direct maternal-fetal bond, as traditionally understood, might impact family dynamics and the child’s psychological development[16].
Artificial wombs could transform societal perceptions of gender roles in reproduction, potentially decoupling biological motherhood from pregnancy. This decoupling could empower individuals, particularly women, to pursue parenthood without the physical demands and risks associated with pregnancy. Some ethicists argue that artificial wombs could promote gender equality by enabling pregnancy without impacting professional or personal lives[17]. However, there is also concern about potentcialization, where artificial womb technology could create markets for gestation, commodifying reproduction in ways that may raise ethical concerns.
Additionally, the legal and regulatory challenges are coming. The introduction of artificial wombs into clinical practice would require legal systems to address issues of custody, parental rights, and fetal protection in novel ways. For example, questions surrounding custody could become complex if an artificially gestated fetus requires emergency medical intervention or faces a high risk of congenital disability[18]. Legal scholars propose the need for new regulations, potentially similar to those governing adoption or surrogacy, to effectively navigate these complex cases.
Consent and autonomy, often foundational principles in medical ethics, are complicated by artificial gestation. Fetuses cannot provide consent, which necessitates careful consideration of the rights of parents or legal guardians in making medical decisions on behalf of a fetus in an artificial womb. Some argue that parents should have the right to make decisions regarding the fetus’s development, while others suggest that artificial wombs introduce a third-party responsibility—potentially the medical institution or state—to act in the fetus’s best interest[19, 20].
The accessibility and affordability of artificial wombs could raise social inequality issues. If artificial womb technology is initially available only to wealthy individuals or in specific regions, it may widen gaps in access to reproductive healthcare. Additionally, the commercialization of artificial wombs could lead to exploitation, particularly in developing countries, where economic pressures might create ethical dilemmas regarding surrogacy alternatives. Experts warn of a future where artificial wombs could be monetized, leading to a “market” for gestation services that risks commodifying human reproduction[21].
Artificial wombs may alter the maternal-fetal bond, with psychological implications for both parents and the child. Traditional pregnancies allow for early bonding experiences; mothers often form an attachment to their unborn child through physical sensations and emotional anticipation[22]. Artificial gestation may remove this element, which could affect parent-child bonding and psychological development. Psychologists suggest that early bonding experiences could be facilitated through parental involvement during gestation, although further studies are needed to explore how artificial gestation might impact child psychology in the long term[23].
Artificial wombs, by offering a controlled environmental development outside the mother’s body, introduce potential for profound societal shifts. They challenge traditional reproductive roles, redefine the concept of parenthood, and raise ethical questions that demand careful consideration as technology advances.
3.3. Future Directions in Artificial Womb Development
3.3.1. Technological Advancements Needed
Artificial womb technology, while promising, requires significant advancements to safely and effectively support human gestation. The complexity of replicating the uterine environment, particularly the physiological processes that facilitate fetal growth, remains a major hurdle. Several emerging technologies and research areas offer pathways to overcoming these challenges, focusing on improving biocompatibility, developing more sophisticated monitoring systems, and optimizing nutrient and waste exchange mechanisms.
Creating a biocompatible interface between the artificial womb and the fetus is critical. Materials must avoid triggering immune responses, prevent infection, and allow for safe, sustained contact with delicate fetal tissue. Researchers are exploring materials that can emulate the amniotic sac and placenta’s structural properties, which are resilient, flexible, and minimally invasive. Biocompatible hydrogels, for example, might be potential amniotic fluid analogs, as they can deliver essential nutrients while maintaining sterility and stability[24, 25].
Artificial wombs require continuous monitoring to adjust environmental conditions in real time, ensuring that parameters such as temperature, oxygenation, and nutrient levels are maintained within optimal ranges. Machine learning models and artificial intelligence could be crucial in enhancing the precision of these adjustments by analyzing large datasets from previous cases to predict optimal conditions for fetal development at each stage[26].
3.3.2. Long-Term Research and Clinical Trials
For artificial wombs to move from animal models to human applications, extensive research and clinical trials are required. This transition will not only need rigorous safety testing but also ethical considerations and strict regulatory oversight.
Before artificial wombs can be integrated into clinical practice, clear regulatory standards must be established to guide medical practitioners. This includes defining standards for artificial womb setup, monitoring protocols, and emergency intervention procedures. Regulatory bodies such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) may need to work closely with bioethicists and scientists to develop standards for safe and ethical use[27].
3.3.3. Integration with Other Reproductive Technologies
Artificial wombs represent only one part of a broader shift in reproductive technology, and their integration with other fields could expand the possibilities for assisted reproduction.
Artificial wombs may complement IVF technology by providing an alternative to gestational surrogacy, allowing embryos to be gestated entirely in an artificial environment[28]. This integration could benefit individuals unable to carry a pregnancy due to medical or personal reasons. Additionally, combining artificial womb technology with genetic screening could enable early identification and correction of genetic disorders, a practice that could significantly reduce infant mortality and childhood disease burden[29].
Advances in gene editing, such as CRISPR-Cas9, offer potential for correcting genetic anomalies at the embryonic stage[30]. When combined with artificial wombs, gene editing could create a controlled setting for using regenerative treatments or genetic changes to stop or treat diseases that run in families. This raises ethical considerations but also holds potential to revolutionize medical interventions at the earliest stages of life.
The full realization of artificial womb technology might lead to a future where ectogenesis, or complete gestation outside the human body, is feasible. This would redefine the limits of human reproduction, offering potential solutions to infertility and perhaps even enabling human reproduction in space or other extreme environments[31, 32]. While still speculative, these possibilities encourage researchers to explore the long-term implications of artificial reproduction on human evolution and societal structures.
Artificial womb technology, though still in its nascent stages, has far-reaching implications for reproductive medicine, family dynamics, and the future of human society. The progression toward integrating artificial wombs into medical practice will rely on ongoing advancements in biomedical engineering, stringent ethical and regulatory frameworks, and a deeper understanding of how artificial gestation may impact human development. The coming years will likely see increased collaboration between technologists, bioethicists, and policymakers as this transformative technology moves closer to clinical reality.
4. Conclusion
Artificial womb technology, at the frontier of neonatal and reproductive medicine, holds transformative potential. By providing a controlled environment to support fetal development outside the human body, artificial wombs could significantly improve outcomes for extremely premature infants and expand reproductive possibilities. The technology has demonstrated promising results in animal studies, with advancements in extracorporeal membrane oxygenation, biocompatible materials, and nutrient delivery systems paving the way for future clinical applications.
However, the journey from experimental use to routine medical practice remains complex, with significant technical, ethical, and regulatory challenges. Ensuring the safety and developmental normalcy of fetuses, addressing ethical concerns surrounding fetal rights, and establishing fair and robust regulatory standards will be essential to responsibly integrating artificial wombs into healthcare.
Looking ahead, the path to realizing artificial womb technology will require interdisciplinary collaboration among scientists, bioethicists, and policymakers to create ethical frameworks and robust guidelines. Artificial wombs could redefine traditional reproductive roles, reshape societal structures, and expand options for families, underscoring the need for careful, informed guidance as this technology advances. Ultimately, artificial wombs may revolutionize both neonatal care and human reproduction, offering life-saving potential and raising profound questions about the future of human gestation.
References
[1]. Coughlin, M., Gibbins, S., & Hoath, S. (2009). Core measures for developmentally supportive care in neonatal intensive care units: theory, precedence and practice. Journal of Advanced Nursing, 65(10), 2239–2248. https://doi.org/10.1111/j.1365-2648.2009.05052.x
[2]. Hunter, P. (2024). Exogestation for treating premature births and congenital diseases. EMBO Reports. https://doi.org/10.1038/s44319-023-00022-4
[3]. Hughes, J. (2021). ARTIFICIAL WOMB: A SHORT HISTORY. Orbis Idearum, 9(2), 13–23. https://orbisidearum.net/pdf/issue_16_article_100.pdf
[4]. Carpenter, J. (2020, November 12). Circus Babies: The Past, Present, and Future of the Neonatal Incubator. USC Viterbi School of Engineering. https://illumin.usc.edu/circus-babies-the-past-present-and-future-of-the-neonatal-incubator/
[5]. Romanis, E. C. (2018). Artificial womb technology and the frontiers of human reproduction: conceptual differences and potential implications. Journal of Medical Ethics, 44(11), 751–755. https://doi.org/10.1136/medethics-2018-104910
[6]. Cindrova-Davies, T., & Sferruzzi-Perri, A. N. (2022). Human placental development and function. Seminars in Cell & Developmental Biology, 131, 66–77. https://doi.org/10.1016/j.semcdb.2022.03.039
[7]. De Bie, F. R., Davey, M. G., Larson, A. C., Deprest, J., & Flake, A. W. (2020). Artificial placenta and womb technology: Past, current, and future challenges towards clinical translation. Prenatal Diagnosis, 41(1), 145–158. https://doi.org/10.1002/pd.5821
[8]. Hadfield, P. (n.d.). Japanese pioneers raise kid in rubber womb. New Scientist. https://www.newscientist.com/article/mg13418180-400-japanese-pioneers-raise-kid-in-rubber-womb/
[9]. Kozlov, M. (2023). Human trials of artificial wombs could start soon. Here’s what you need to know. Nature. https://doi.org/10.1038/d41586-023-02901-1
[10]. Behrman, R. E., Adrienne Stith Butler, & Institute of Medicine (US) Committee on Understanding Premature Birth and Assuring Healthy Outcomes. (2010). Mortality and Acute Complications in Preterm Infants. Nih.gov; National Academies Press (US). https://www.ncbi.nlm.nih.gov/books/NBK11385/
[11]. MASIH, P. (2024, November 13). Artificial Womb Technology: The Future of Neonatal Intensive Care Unit for Premature Infants. PAUL ACADEMY. https://www.paulmasih.com/post/neonatalintensivecareunit
[12]. Stein, R. (2024, April 12). An artificial womb could build a bridge to health for premature babies. NPR. https://www.npr.org/sections/health-shots/2024/04/12/1241895501/artificial-womb-premature-birth
[13]. God’s Grand Plan for Motherhood. (2016, July 13). Crossway. https://www.crossway.org/articles/gods-grand-plan-for-motherhood/
[14]. Mothers in Islam. (n.d.). Islamweb. https://islamweb.net/en/article/149345/mothers-in-islam
[15]. Ferreira, A. (2022). The (Un)Ethical Womb: The Promises and Perils of Artificial Gestation. Journal of Bioethical Inquiry. https://doi.org/10.1007/s11673-022-10184-w
[16]. Observatory, B. (2023, May 19). The ethical dilemma of artificial wombs for development of the fetonate - Bioethics Observatory - Institute of Life Sciences - UCV. https://bioethicsobservatory.org/2023/05/the-ethical-dilemma-of-artificial-wombs-for-development-of-the-fetonate/45249/
[17]. Horn, C. (2020). Gender, gestation and ectogenesis: self-determination for pregnant people ahead of artificial wombs. Journal of Medical Ethics, 46(11), 787–788. https://doi.org/10.1136/medethics-2020-106156
[18]. Surrogacy and Artificial Conception. (n.d.). Findlaw. https://www.findlaw.com/family/surrogacy-artificial-conception.html
[19]. (2024). Aap.org. https://publications.aap.org/aapnews/news/26150/Experts-discuss-medical-ethical-issues-around?autologincheck=redirected
[20]. Center for Reproductive Rights. (2022). The Constitutional Right to Reproductive Autonomy: Realizing the Promise of the 14th Amendment. Center for Reproductive Rights. https://reproductiverights.org/constitutional-right-reproductive-autonomy-14th-amendment/
[21]. Sanchez-Chapman, S. (2023, October 19). Artificial wombs: The reality, risks, and rewards - Sofia Sanchez-Chapman - Medium. Medium. https://medium.com/@sofiasc/artificial-wombs-the-reality-the-risks-and-the-rewards-3039faca72f6
[22]. Smorti, M., Ponti, L., Ghinassi, S., & Rapisardi, G. (2020). The mother-child attachment bond before and after birth: The role of maternal perception of traumatic childbirth. Early Human Development, 142, 104956. https://doi.org/10.1016/j.earlhumdev.2020.104956
[23]. Khulbe, Y., Gupta, S., Javed, B., Neyazi, A., & Padhi, B. K. (2023). Artificial womb: opportunities and challenges for public health. International Journal of Surgery, 109(3), 618. https://doi.org/10.1097/JS9.0000000000000208
[24]. Golara Kafili, Niknejad, H., Elnaz Tamjid, & Abdolreza Simchi. (2024). Amnion-derived hydrogels as a versatile platform for regenerative therapy: from lab to market. Frontiers in Bioengineering and Biotechnology, 12. https://doi.org/10.3389/fbioe.2024.1358977
[25]. Sannino, A., Madaghiele, M., & Ambrosio, L. (2009). Biocompatibility and other properties of hydrogels in regenerative medicine. Elsevier EBooks. https://doi.org/10.1533/9781845695477.1.114
[26]. Williams, N. J., Fovargue, S., & Wilkinson, S. (2023, December 1). Artificial wombs could someday be a reality – here’s how they may change our notions of parenthood. The Conversation. https://theconversation.com/artificial-wombs-could-someday-be-a-reality-heres-how-they-may-change-our-notions-of-parenthood-217490
[27]. Teixeira, T., Kweder, S. L., & Saint‐Raymond, A. (2020). Are the European Medicines Agency, US Food and Drug Administration, and Other International Regulators Talking to Each Other? Clinical Pharmacology and Therapeutics, 107(3), 507–513. https://doi.org/10.1002/cpt.1617
[28]. Choe, J., & Shanks, A. L. (2023, September 4). In Vitro Fertilization. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK562266/
[29]. Van den Veyver, I. B. (2016). Recent advances in prenatal genetic screening and testing. F1000Research, 5, 2591. https://doi.org/10.12688/f1000research.9215.1
[30]. Schenkwein, D., & Ylä-Herttuala, S. (2018). Gene Editing of Human Embryos with CRISPR/Cas9: Great Promise Coupled with Important Caveats. Molecular Therapy, 26(3), 659–660. https://doi.org/10.1016/j.ymthe.2018.02.007
[31]. Kendal, E. (2021). Ectogenesis for Space Exploration. ELS, 1–5. https://doi.org/10.1002/9780470015902.a0029255
[32]. Wang, T. (2021, October 26). Why We Should Embrace Artificial Wombs. Viterbi Conversations in Ethics. https://vce.usc.edu/volume-5-issue-2/why-we-should-embrace-artificial-wombs/
Cite this article
Zhang,W. (2025). Current Status and Future Development of Artificial Wombs: A Review. Theoretical and Natural Science,81,100-108.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 3rd International Conference on Environmental Geoscience and Earth Ecology
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Coughlin, M., Gibbins, S., & Hoath, S. (2009). Core measures for developmentally supportive care in neonatal intensive care units: theory, precedence and practice. Journal of Advanced Nursing, 65(10), 2239–2248. https://doi.org/10.1111/j.1365-2648.2009.05052.x
[2]. Hunter, P. (2024). Exogestation for treating premature births and congenital diseases. EMBO Reports. https://doi.org/10.1038/s44319-023-00022-4
[3]. Hughes, J. (2021). ARTIFICIAL WOMB: A SHORT HISTORY. Orbis Idearum, 9(2), 13–23. https://orbisidearum.net/pdf/issue_16_article_100.pdf
[4]. Carpenter, J. (2020, November 12). Circus Babies: The Past, Present, and Future of the Neonatal Incubator. USC Viterbi School of Engineering. https://illumin.usc.edu/circus-babies-the-past-present-and-future-of-the-neonatal-incubator/
[5]. Romanis, E. C. (2018). Artificial womb technology and the frontiers of human reproduction: conceptual differences and potential implications. Journal of Medical Ethics, 44(11), 751–755. https://doi.org/10.1136/medethics-2018-104910
[6]. Cindrova-Davies, T., & Sferruzzi-Perri, A. N. (2022). Human placental development and function. Seminars in Cell & Developmental Biology, 131, 66–77. https://doi.org/10.1016/j.semcdb.2022.03.039
[7]. De Bie, F. R., Davey, M. G., Larson, A. C., Deprest, J., & Flake, A. W. (2020). Artificial placenta and womb technology: Past, current, and future challenges towards clinical translation. Prenatal Diagnosis, 41(1), 145–158. https://doi.org/10.1002/pd.5821
[8]. Hadfield, P. (n.d.). Japanese pioneers raise kid in rubber womb. New Scientist. https://www.newscientist.com/article/mg13418180-400-japanese-pioneers-raise-kid-in-rubber-womb/
[9]. Kozlov, M. (2023). Human trials of artificial wombs could start soon. Here’s what you need to know. Nature. https://doi.org/10.1038/d41586-023-02901-1
[10]. Behrman, R. E., Adrienne Stith Butler, & Institute of Medicine (US) Committee on Understanding Premature Birth and Assuring Healthy Outcomes. (2010). Mortality and Acute Complications in Preterm Infants. Nih.gov; National Academies Press (US). https://www.ncbi.nlm.nih.gov/books/NBK11385/
[11]. MASIH, P. (2024, November 13). Artificial Womb Technology: The Future of Neonatal Intensive Care Unit for Premature Infants. PAUL ACADEMY. https://www.paulmasih.com/post/neonatalintensivecareunit
[12]. Stein, R. (2024, April 12). An artificial womb could build a bridge to health for premature babies. NPR. https://www.npr.org/sections/health-shots/2024/04/12/1241895501/artificial-womb-premature-birth
[13]. God’s Grand Plan for Motherhood. (2016, July 13). Crossway. https://www.crossway.org/articles/gods-grand-plan-for-motherhood/
[14]. Mothers in Islam. (n.d.). Islamweb. https://islamweb.net/en/article/149345/mothers-in-islam
[15]. Ferreira, A. (2022). The (Un)Ethical Womb: The Promises and Perils of Artificial Gestation. Journal of Bioethical Inquiry. https://doi.org/10.1007/s11673-022-10184-w
[16]. Observatory, B. (2023, May 19). The ethical dilemma of artificial wombs for development of the fetonate - Bioethics Observatory - Institute of Life Sciences - UCV. https://bioethicsobservatory.org/2023/05/the-ethical-dilemma-of-artificial-wombs-for-development-of-the-fetonate/45249/
[17]. Horn, C. (2020). Gender, gestation and ectogenesis: self-determination for pregnant people ahead of artificial wombs. Journal of Medical Ethics, 46(11), 787–788. https://doi.org/10.1136/medethics-2020-106156
[18]. Surrogacy and Artificial Conception. (n.d.). Findlaw. https://www.findlaw.com/family/surrogacy-artificial-conception.html
[19]. (2024). Aap.org. https://publications.aap.org/aapnews/news/26150/Experts-discuss-medical-ethical-issues-around?autologincheck=redirected
[20]. Center for Reproductive Rights. (2022). The Constitutional Right to Reproductive Autonomy: Realizing the Promise of the 14th Amendment. Center for Reproductive Rights. https://reproductiverights.org/constitutional-right-reproductive-autonomy-14th-amendment/
[21]. Sanchez-Chapman, S. (2023, October 19). Artificial wombs: The reality, risks, and rewards - Sofia Sanchez-Chapman - Medium. Medium. https://medium.com/@sofiasc/artificial-wombs-the-reality-the-risks-and-the-rewards-3039faca72f6
[22]. Smorti, M., Ponti, L., Ghinassi, S., & Rapisardi, G. (2020). The mother-child attachment bond before and after birth: The role of maternal perception of traumatic childbirth. Early Human Development, 142, 104956. https://doi.org/10.1016/j.earlhumdev.2020.104956
[23]. Khulbe, Y., Gupta, S., Javed, B., Neyazi, A., & Padhi, B. K. (2023). Artificial womb: opportunities and challenges for public health. International Journal of Surgery, 109(3), 618. https://doi.org/10.1097/JS9.0000000000000208
[24]. Golara Kafili, Niknejad, H., Elnaz Tamjid, & Abdolreza Simchi. (2024). Amnion-derived hydrogels as a versatile platform for regenerative therapy: from lab to market. Frontiers in Bioengineering and Biotechnology, 12. https://doi.org/10.3389/fbioe.2024.1358977
[25]. Sannino, A., Madaghiele, M., & Ambrosio, L. (2009). Biocompatibility and other properties of hydrogels in regenerative medicine. Elsevier EBooks. https://doi.org/10.1533/9781845695477.1.114
[26]. Williams, N. J., Fovargue, S., & Wilkinson, S. (2023, December 1). Artificial wombs could someday be a reality – here’s how they may change our notions of parenthood. The Conversation. https://theconversation.com/artificial-wombs-could-someday-be-a-reality-heres-how-they-may-change-our-notions-of-parenthood-217490
[27]. Teixeira, T., Kweder, S. L., & Saint‐Raymond, A. (2020). Are the European Medicines Agency, US Food and Drug Administration, and Other International Regulators Talking to Each Other? Clinical Pharmacology and Therapeutics, 107(3), 507–513. https://doi.org/10.1002/cpt.1617
[28]. Choe, J., & Shanks, A. L. (2023, September 4). In Vitro Fertilization. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK562266/
[29]. Van den Veyver, I. B. (2016). Recent advances in prenatal genetic screening and testing. F1000Research, 5, 2591. https://doi.org/10.12688/f1000research.9215.1
[30]. Schenkwein, D., & Ylä-Herttuala, S. (2018). Gene Editing of Human Embryos with CRISPR/Cas9: Great Promise Coupled with Important Caveats. Molecular Therapy, 26(3), 659–660. https://doi.org/10.1016/j.ymthe.2018.02.007
[31]. Kendal, E. (2021). Ectogenesis for Space Exploration. ELS, 1–5. https://doi.org/10.1002/9780470015902.a0029255
[32]. Wang, T. (2021, October 26). Why We Should Embrace Artificial Wombs. Viterbi Conversations in Ethics. https://vce.usc.edu/volume-5-issue-2/why-we-should-embrace-artificial-wombs/