1. Introduction
Dental Fear and Anxiety (DFA) is a kind of persistent excessive anxiety and fear, which usually shows a series of symptoms such as irritability, palpitations, sweating and increased sensitivity to pain [1, 2]. Due to the huge cultural, social and economic differences among populations and the disunity of measurement design and tools, the prevalence of DFA varies greatly. However, many studies have pointed to the prevalence of DFA among adults, adolescents, and children globally [3, 4].
As an intersection of oral and psychiatric diseases, the etiology of DFA has unique complexity. So far, it has been found that DFA is closely related to a variety of factors, which can be roughly divided into two categories: internal factors include gender [5], age [6], temperament [7], pain sensitivity [8], etc., and external factors including poor medical experience [9], cultural values [10], setting for treatment, etc., and even the color of the treatment equipment [11]. At the same time, these influencing factors can also interfere with each other [12], presenting a dynamic mechanism.
DFA has led to many hazards due to its complexity and prevalence. At the same time, its dynamic mechanism is summarized as a vicious cycle of DFA, which may be the key to understanding and improving DFA.
2. Hazards
The American Psychiatric Association classifies DFA as a specific type of phobia [13]. In severe cases, people may have severe pain, and refuse to receive treatment due to fear and anxiety, thus avoiding dental treatment, resulting in dental caries, periodontitis and other diseases.
At the same time, oral diseases and systemic diseases are inseparable. And some scientific evidence supports those oral diseases may be an independent risk factor for certain diseases, including diabetes, cardiovascular disease, dementia, etc., affecting the health of the whole body [14, 15].
Although one study has proposed that DFA do not adversely affect oral health behaviors [16], DFA can also have a negative impact on Oral Health Related Quality of Life (OHRQ-oL), causing patients to have symptoms such as dietary difficulties and dysphonia, affecting patients' normal life [17, 18].
During dental treatment, patients with high dental anxiety may also increase the work pressure of dentists, increase the treatment time [19], and even lead to misdiagnosis [20], which further worsens the doctor-patient relationship and increases the difficulty of diagnosis and treatment [6, 21].
3. The vicious circle of DFA
In addition to the above hazards, DFA can lead to a vicious circle, deepening DFA and its hazards.
The currently recognized vicious circle model of DFA contains several common factors and processes, such as avoidance of dental care, deterioration of oral health, further or symptom-driven treatment, feelings of guilt, shame and inferiority, etc. The interaction and causality between these factors ultimately exacerbate the occurrence and development of DFA, so it is called the vicious circle of DFA [22-27].
The earliest description of the vicious cycle of DFA dates back to the 1960s, and explores its role in dental fear in children [28]. Subsequently, more and more researchers began to pay close attention to the application of the vicious circle in the field of DFA, verify various factors and start to create models.
3.1. The single-pathway vicious cycle of DFA
Berggren’s vicious cycle of DFA [22] is one of the typical models (see Figure 1). Berggren proposed that dental fear arises from the apprehension and unease associated with avoiding dental care, which subsequently leads to tooth deterioration. He emphasized that feelings of guilt, shame, and inferiority resulting from poor oral conditions ultimately contribute to a detrimental circle of dental fear.
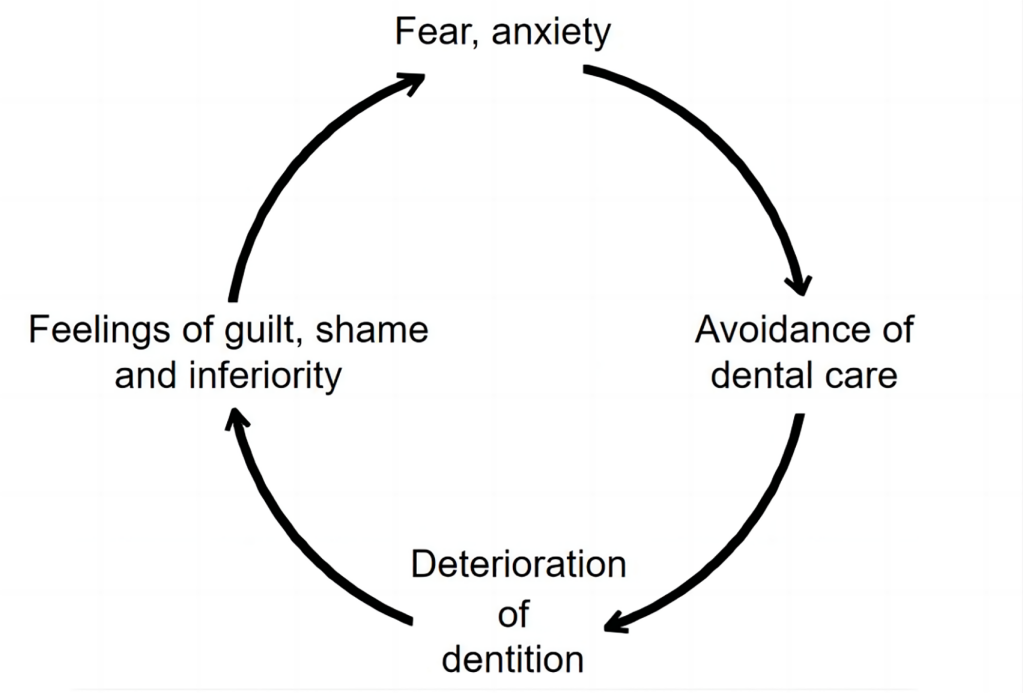
Figure 1. Berggren’s vicious circle of DFA
Some researchers hold a positive attitude towards this model and have conducted various studies to verify its rationality statistically. At the same time, they also make new findings. Jongh [29], for example, has established a model to test Berggren’ s vicious circle of DFA, and proves that the correlation between various factors in the circle is significant. Carlsson’s research [30] provides further support for the association between DFA, avoidance and health-related outcomes, which contributes to the validation of the vicious circle model. Carlsson also believes that there is a certain correlation between dental anxiety and sense of coherence. Besides, Moore [31] points out the contribution of embarrassment to phobic dental anxiety and validates the relevance of embarrassment in the vicious cycle of dental fear. Most importantly, many scholars believe that the patient's pain and unpleasant treatment experience are important for the generation of DFA deterioration and avoidance, and some studies also point to the negative behaviors of dentists as the trigger of high anxiety [32-35]. Therefore, Berggren's theoretical construction is not perfect and comprehensive, especially the factors related to oral treatment have not been incorporated into the cycle. But the contribution of this model in the field of DFA is undeniable.
Bouma [23] and Thomson [25] et al acknowledged the importance of fear, anxiety and avoidance in the vicious cycle of DFA, and on this basis further put forward the deterioration of oral conditions caused by these factors and further symptom-driven treatment. Armfield [26] highlighted and pointed out that symptom-driven treatment forms a chain reaction that feeds back into the vicious cycle of DFA (see Figure 2). Symptom-driven treatment is considered to be associated with more serious dental treatment, leading to a higher degree of DFA.
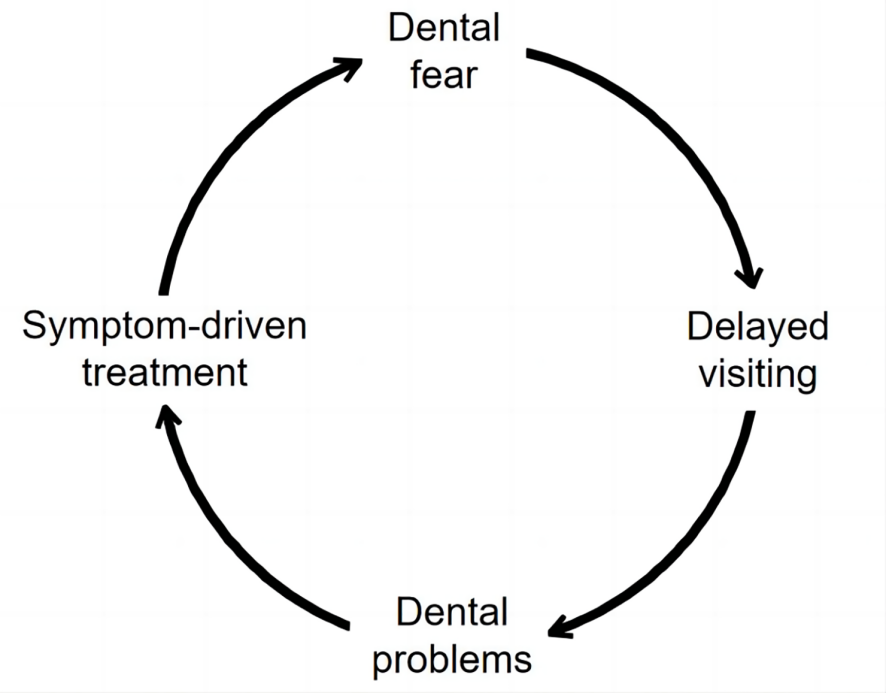
Figure 2. Model of the vicious circle of dental fear as Armfield describled
Armfield conducted two telephone interviews [26, 27] before and after to verify the model and obtained positive results. The results of a cohort study reported by Silveirai [24] also support this vicious circle of dental fear. As a result, Armfield emphasizes the factors associated with symptoms and treatment role in the vicious cycle of DFA, this is undeniable, but at the same time, although psychological factors such as cognitive vulnerability [36] have been noted, more pure feelings such as embarrassment and inferiority are also important to the model. Researchers may have tried to incorporate psychological and treatment related factors into the same model, but there seems to be a missing key point linking the two.
3.2. The dual channel vicious circle of DFA
To sum up, Berggren’ vicious circle emphasizes the feelings of guilt, shame and interiority, but ignores the influence of treatment. In fact, an effective treatment will relieve the patients’ DFA, while a treatment bringing bad experience and pain will aggravate the degree of DFA. On the contrary, Armfield underlines the symptom-driven treatment, which neglected the influence of the internal psychological factors, such as negative emotion. As a result, a single cycle is difficult to fully explain the vicious circle of DFA. To perfect the dynamic mechanism of DFA and explore ways to alleviate the degree of DFA (see Figure 3), this review article put forward the Dual Channel Vicious Circle of Dental fear and Anxiety (DCVC-oDFA).
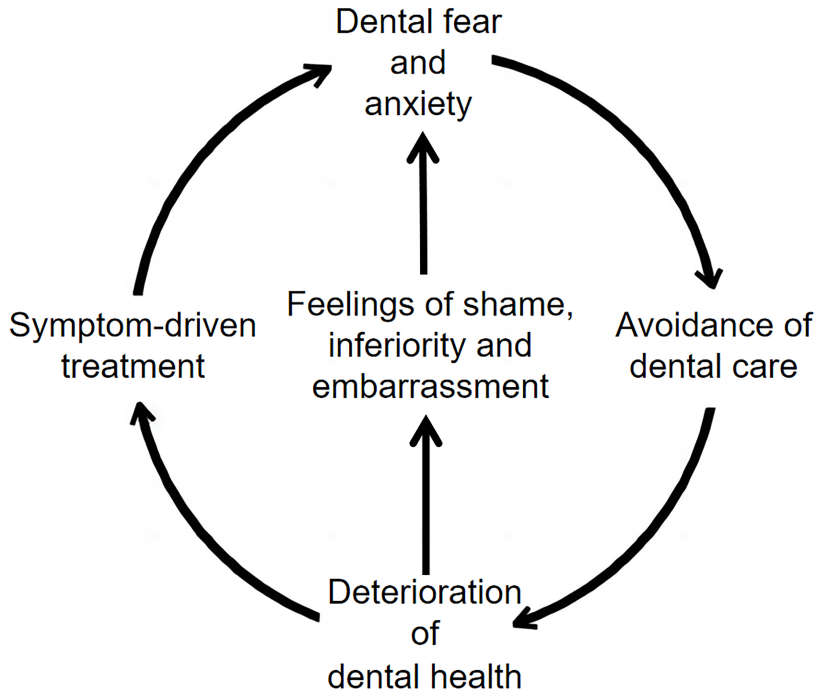
Figure 3. DCVC-oDFA
To explain the DCVC-oDFA, after experiencing anxiety and fear, people will often develop a mentality of avoidance. As coping behaviors, avoidance or evasion is at the core of maintaining anxiety and fear in various mental illnesses, which is described as a valuable reaction to avoid danger [37, 38]. Therefore, the DFA will unavoidably cause the mentality of avoidance. The deterioration of oral conditions caused by avoidance of treatment and care is also difficult to avoid [39].
As oral health deteriorates, different situations and people make different choices, but different choices lead to similar results. Those who do not choose to seek medical treatment will lead to the aggravation of negative emotions such as embarrassment and inferiority by the deterioration of DFA [29, 31]. Symptom-driven seeking for medical treatment will also lead to the aggravation of DFA due to the unpleasant experience caused by the severity of their illness and the difficulty of treatment [24].
This new model, centered on a key choice, divides the progression of worsening oral conditions into psychological factors and symptom-driven related treatments, and both contribute to further worsening of DFA. It is more comprehensive than existing models, explaining dynamic mechanisms that cannot be adequately explained by a single pathway. Besides, embarrassment as a complex dental fear factor was also included in the vicious cycle [31].
4. Solutions
Current DFA treatments primarily utilize in-clinic sedatives, such as nitrous oxide for rapid sedation [40], combined with psychotherapy, yet face challenges including side effects like drowsiness and hypoxemia at higher nitrous oxide concentrations [41], as well as risks from drugs such as diazepam [42]. Given limitations in safety, efficacy, and practicality of existing methods, this review proposes a dual intervention strategy integrating direct and indirect approaches under the DCVC-oDFA framework.
First, addressing dental avoidance through health education on dental fear's risks and advocating timely treatment. Government and clinical initiatives like free fissure sealants and fear-management lectures can demystify procedures, while painless experiences enhance treatment acceptance.
Second, addressing the feelings of shame, inferiority and embarrassment. The psychological problems related to DFA are closely related to the patient's personality [43], psychological resilience [44], and the ability to perceive pain [45], and solutions can be explored from many perspectives like CBT [36, 46] and psychological counseling.
Third, addressing the symptom-driven treatment. Prioritize accurate diagnosis of oral diseases to distinguish chronic versus acute and primary versus secondary conditions. Implement root-cause-targeted treatments using minimally invasive techniques, complemented by music or aromatherapy, to enhance patient comfort during procedures [47].
5. Conclusion
This review has limitations requiring further model validation. Additional factors like OHRQ-oL may can be incorporated into the vicious cycle of DFA, where breaking this cycle remains a key challenge needing stronger evidence. The article reviews existing DFA models' mechanisms and features, introducing an enhanced DCVC-oDFA model that synthesizes previous frameworks with enhanced realism to clarify DFA dynamics. Applying strategies based on this model may help mitigate DFA severity.
Disclosure statement
The authors declare no conflict of interest.
References
[1]. Murad, M. H., Ingle, N. A., & Assery, M. K. (2020). Evaluating factors associated with fear and anxiety to dental treatment-A systematic review. Journal of family medicine and primary care, 9(9), 4530–4535.
[2]. Liu, D., Liu, Y., Wang, J. (2022). Research progress of dental phobia. Guangxi Medical Journal, 44(20), 2418-2421.
[3]. Silveira, E. R., Cademartori, M. G., Schuch, H. S., Armfield, J. A., & Demarco, F. F. (2021). Estimated prevalence of dental fear in adults: A systematic review and meta-analysis. Journal of dentistry, 108, 103632.
[4]. Grisolia, B. M., Dos Santos, A. P. P., Dhyppolito, I. M., Buchanan, H., Hill, K., & Oliveira, B. H. (2021). Prevalence of dental anxiety in children and adolescents globally: A systematic review with meta-analyses. International journal of paediatric dentistry, 31(2), 168–183.
[5]. Dadalti MT, Cunha AJ, Souza TG, Silva BA, Luiz RR, Risso PA. Anxiety about dental treatment - a gender issue. Acta Odontol Latinoam. 2021 Aug 1;34(2):195-200.
[6]. Katanec T, Singh S, Majstorovic M, Klaric I, Herman NG, Moursi AM. Gender Differences in Dental Anxiety and Medical Fear in Croatian Adolescents. J Clin Pediatr Dent. 2018;42(3):182-187.
[7]. Gustafsson A, Broberg A, Bodin L, Berggren U, Arnrup K. Dental behaviour management problems: the role of child personal characteristics. Int J Paediatr Dent. 2010;20:242–53.
[8]. Yap AU, Lee DZR. Dental fear and anxiety in Asian youths: response components and inducing stimuli. Clin Oral Investig. 2022 Sep;26(9):5953-5960.
[9]. Wang Z.Analysis of the utilization and cost of oral health care services for urban and rural residents in Beijing. Chin J Stomatol. 2003;2:70–73.
[10]. Chang DJ, Debiec J. Neural correlates of the mother-to-infant social transmission of fear. J Neurosci Res. 2016 Jun;94(6):526-34.
[11]. Maganur, P. C., Vishwanathaiah, S., Ali Quadri, M. F., Alsabi, M., Modarba, W., Aqeel, W., Rawi, N. A., Uthman, A., Reda, R., Jafer, M., Testarelli, L., & Patil, S. (2024). Color perception and its relation to dental anxiety in children. Dental and medical problems, 61(5), 671–677.
[12]. Stein Duker, L. I., Grager, M., Giffin, W., Hikita, N., & Polido, J. C. (2022). The Relationship between Dental Fear and Anxiety, General Anxiety/Fear, Sensory Over-Responsivity, and Oral Health Behaviors and Outcomes: A Conceptual Model. International journal of environmental research and public health, 19(4), 2380.
[13]. Seligman LD,Hovey JD,Chacon K,et al.Dental anxiety: an understudied problem in youth[J].Clin Psychol Rev,2017,55:25-40.
[14]. Meurman JH, Sanz M, Janket SJ. Oral health, atherosclerosis, and cardiovascular disease. Crit Rev Oral Biol Med. 2004 Nov 1;15(6):403-13.
[15]. Gil-Montoya JA, de Mello AL, Barrios R, Gonzalez-Moles MA, Bravo M. Oral health in the elderly patient and its impact on general well-being: a nonsystematic review. Clin Interv Aging. 2015 Feb 11;10:461-7.
[16]. Supriya, Singh, R., & Ahsan, A. (2024). Relevance of Emotion of Anxiety and Fear of Dentistry as Motivational Conflict in Oral Health Behaviors. The journal of contemporary dental practice, 25(3), 280–288.
[17]. Locker D. Psychosocial consequences of dental fear and anxiety. Community Dent Oral Epidemiol. 2003 Apr;31(2):144-51.
[18]. Armfield JM. Predicting dental avoidance among dentally fearful Australian adults. Eur J Oral Sci. 2013 Jun;121(3 Pt 2):240-6.
[19]. Moore R, Brødsgaard I.(2001).Dentists' perceived stress and its relation to perceptions about anxious patients. [J]. Community dentistry and oral epidemiology,29,73-80.
[20]. Eli I.(1993).Dental anxiety: a cause for possible misdiagnosis of tooth vitality. International endodontic journal, 26, 251–253.
[21]. Cianetti, S., Lombardo, G., Lupatelli, E., Pagano, S., Abraha, I., Montedori, A., Caruso, S., Gatto, R., De Giorgio, S., and Salvato, R. (2017). Dental fear/anxiety among children and adolescents. A systematic review. European journal of paediatric dentistry, 18, 121–130.
[22]. Berggren U, Meynert G. Dental fear and avoidance: causes, symptoms, and consequences. J Am Dent Assoc. 1984 Aug;109(2):247-51.
[23]. Bouma J, Uitenbroek D, Westert G, Schaub RM, van de Poel F. Pathways to full mouth extraction. Community Dent Oral Epidemiol. 1987 Dec;15(6):301-5.
[24]. Silveira ER, Cademartori MG, Schuch HS, Corrêa MB, Ardenghi TM, Armfield J, Horta BL, Demarco FF. The vicious cycle of dental fear at age 31 in a birth cohort in Southern Brazil. Community Dent Oral Epidemiol. 2021 Aug;49(4):354-361.
[25]. Thomson WM, Stewart JF, Carter KD, Spencer AJ. Dental anxiety among Australians. Int Dent J. 1996 Aug;46(4):320-4.
[26]. Armfield JM, Stewart JF, Spencer AJ. The vicious cycle of dental fear: exploring the interplay between oral health, service utilization and dental fear. BMC Oral Health. 2007 Jan 14;7:1.
[27]. Armfield JM. What goes around comes around: revisiting the hypothesized vicious cycle of dental fear and avoidance. Community Dent Oral Epidemiol. 2013 Jun;41(3):279-87.
[28]. Hall RK. Management of the sick and handicapped child in general dental practice. Aust Dent J. 1967 Aug;12(4):323-31.
[29]. De Jongh A, Schutjes M, Aartman IH. A test of Berggren's model of dental fear and anxiety. Eur J Oral Sci. 2011 Oct;119(5):361-5.
[30]. Carlsson V, Hakeberg M, Wide Boman U. Associations between dental anxiety, sense of coherence, oral health-related quality of life and health behavior--a national Swedish cross-sectional survey. BMC Oral Health. 2015 Sep 2;15:100.
[31]. Moore R, Brødsgaard I, Rosenberg N. The contribution of embarrassment to phobic dental anxiety: a qualitative research study. BMC Psychiatry. 2004 Apr 19;4:10.
[32]. Locker D, Shapiro D, Liddell A. Negative dental experiences and their relationship to dental anxiety. Community Dent Health. 1996 Jun;13(2):86-92. PMID: 8763138IF: 1.7 B4.
[33]. Vassend O. Anxiety, pain and discomfort associated with dental treatment. Behav Res Ther. 1993 Sep;31(7):659-66.
[34]. Moore R, Brødsgaard I. Differential diagnosis of odontophobic patients using the DSM-IV. Eur J Oral Sci. 1995 Apr;103(2 ( Pt 1)):121-6.
[35]. Liddell A, Gosse V. Characteristics of early unpleasant dental experiences. J Behav Ther Exp Psychiatry. 1998 Sep;29(3):227-37.
[36]. Armfield JM, Slade GD, Spencer AJ. Cognitive vulnerability and dental fear. BMC Oral Health. 2008 Jan 24;8:2.
[37]. Barlow DH. Anxiety and its disorders: the nature and treatment of anxiety and panic. New York: Guilford press; 2002.
[38]. Skinner BF. Science and human behavior. New York: Free Press; 1965.
[39]. Appukuttan D. P. (2016). Strategies to manage patients with dental anxiety and dental phobia: literature review. Clinical, cosmetic and investigational dentistry, 8, 35–50.
[40]. Buhre W,Disma N,Hendrickx J,et al.European society of anaesthesiology task force on nitrous oxide:a practice [J]. BrJAnaesth,2019,122(5):587-604.
[41]. Kharouba J,Somri M,Hadjittofi C,et al.Effectiveness and safety of nitrous oxide as a sedative agent at 60%and 70% compared to 50% concentration in pediatric dentistry setting [J].J Clin Pediatr Dent,2020,44(1):60-65.
[42]. Atkin T, Comai S, Gobbi G. Drugs for insomnia beyond benzodiazepines:pharmacology, clinical applications, and discovery[J]. Pharmacol Rev, 2018,70(2): 197-245.
[43]. Steinvik, L. M., Svartdal, F., & Johnsen, J. K. (2023). Delay of Dental Care: An Exploratory Study of Procrastination, Dental Attendance, and Self-Reported Oral Health. Dentistry journal, 11(2), 56.
[44]. Anderson, K., & Priebe, S. (2021). Concepts of Resilience in Adolescent Mental Health Research. The Journal of adolescent health : official publication of the Society for Adolescent Medicine, 69(5), 689–695.
[45]. Sharma, R., George, M., & Krishnan, M. (2024). Efficacy of Preemptive Analgesia on Pain Perception After Simple Tooth Extraction: A Prospective Study. Cureus, 16(4), e58262.
[46]. Davis TE, May A, Whiting SE. Evidence-based treatment of anxiety and phobia in children and adolescents: current status and effects on the emotional response. Clin Psychol Rev. 2011 Jun;31(4):592–602.
[47]. Janthasila, N., & Keeratisiroj, O. (2023). Music therapy and aromatherapy on dental anxiety and fear: A randomized controlled trial. Journal of dental sciences, 18(1), 203–210.
Cite this article
Li,Y.;Zhang,Y.;Huang,J.;Wu,X.;Hu,W.;Zhao,Y. (2025). Work along both lines: a modified model of the vicious circle of Dental Fear and Anxiety (DFA). Journal of Clinical Technology and Theory,3(2),40-45.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Journal:Journal of Clinical Technology and Theory
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Murad, M. H., Ingle, N. A., & Assery, M. K. (2020). Evaluating factors associated with fear and anxiety to dental treatment-A systematic review. Journal of family medicine and primary care, 9(9), 4530–4535.
[2]. Liu, D., Liu, Y., Wang, J. (2022). Research progress of dental phobia. Guangxi Medical Journal, 44(20), 2418-2421.
[3]. Silveira, E. R., Cademartori, M. G., Schuch, H. S., Armfield, J. A., & Demarco, F. F. (2021). Estimated prevalence of dental fear in adults: A systematic review and meta-analysis. Journal of dentistry, 108, 103632.
[4]. Grisolia, B. M., Dos Santos, A. P. P., Dhyppolito, I. M., Buchanan, H., Hill, K., & Oliveira, B. H. (2021). Prevalence of dental anxiety in children and adolescents globally: A systematic review with meta-analyses. International journal of paediatric dentistry, 31(2), 168–183.
[5]. Dadalti MT, Cunha AJ, Souza TG, Silva BA, Luiz RR, Risso PA. Anxiety about dental treatment - a gender issue. Acta Odontol Latinoam. 2021 Aug 1;34(2):195-200.
[6]. Katanec T, Singh S, Majstorovic M, Klaric I, Herman NG, Moursi AM. Gender Differences in Dental Anxiety and Medical Fear in Croatian Adolescents. J Clin Pediatr Dent. 2018;42(3):182-187.
[7]. Gustafsson A, Broberg A, Bodin L, Berggren U, Arnrup K. Dental behaviour management problems: the role of child personal characteristics. Int J Paediatr Dent. 2010;20:242–53.
[8]. Yap AU, Lee DZR. Dental fear and anxiety in Asian youths: response components and inducing stimuli. Clin Oral Investig. 2022 Sep;26(9):5953-5960.
[9]. Wang Z.Analysis of the utilization and cost of oral health care services for urban and rural residents in Beijing. Chin J Stomatol. 2003;2:70–73.
[10]. Chang DJ, Debiec J. Neural correlates of the mother-to-infant social transmission of fear. J Neurosci Res. 2016 Jun;94(6):526-34.
[11]. Maganur, P. C., Vishwanathaiah, S., Ali Quadri, M. F., Alsabi, M., Modarba, W., Aqeel, W., Rawi, N. A., Uthman, A., Reda, R., Jafer, M., Testarelli, L., & Patil, S. (2024). Color perception and its relation to dental anxiety in children. Dental and medical problems, 61(5), 671–677.
[12]. Stein Duker, L. I., Grager, M., Giffin, W., Hikita, N., & Polido, J. C. (2022). The Relationship between Dental Fear and Anxiety, General Anxiety/Fear, Sensory Over-Responsivity, and Oral Health Behaviors and Outcomes: A Conceptual Model. International journal of environmental research and public health, 19(4), 2380.
[13]. Seligman LD,Hovey JD,Chacon K,et al.Dental anxiety: an understudied problem in youth[J].Clin Psychol Rev,2017,55:25-40.
[14]. Meurman JH, Sanz M, Janket SJ. Oral health, atherosclerosis, and cardiovascular disease. Crit Rev Oral Biol Med. 2004 Nov 1;15(6):403-13.
[15]. Gil-Montoya JA, de Mello AL, Barrios R, Gonzalez-Moles MA, Bravo M. Oral health in the elderly patient and its impact on general well-being: a nonsystematic review. Clin Interv Aging. 2015 Feb 11;10:461-7.
[16]. Supriya, Singh, R., & Ahsan, A. (2024). Relevance of Emotion of Anxiety and Fear of Dentistry as Motivational Conflict in Oral Health Behaviors. The journal of contemporary dental practice, 25(3), 280–288.
[17]. Locker D. Psychosocial consequences of dental fear and anxiety. Community Dent Oral Epidemiol. 2003 Apr;31(2):144-51.
[18]. Armfield JM. Predicting dental avoidance among dentally fearful Australian adults. Eur J Oral Sci. 2013 Jun;121(3 Pt 2):240-6.
[19]. Moore R, Brødsgaard I.(2001).Dentists' perceived stress and its relation to perceptions about anxious patients. [J]. Community dentistry and oral epidemiology,29,73-80.
[20]. Eli I.(1993).Dental anxiety: a cause for possible misdiagnosis of tooth vitality. International endodontic journal, 26, 251–253.
[21]. Cianetti, S., Lombardo, G., Lupatelli, E., Pagano, S., Abraha, I., Montedori, A., Caruso, S., Gatto, R., De Giorgio, S., and Salvato, R. (2017). Dental fear/anxiety among children and adolescents. A systematic review. European journal of paediatric dentistry, 18, 121–130.
[22]. Berggren U, Meynert G. Dental fear and avoidance: causes, symptoms, and consequences. J Am Dent Assoc. 1984 Aug;109(2):247-51.
[23]. Bouma J, Uitenbroek D, Westert G, Schaub RM, van de Poel F. Pathways to full mouth extraction. Community Dent Oral Epidemiol. 1987 Dec;15(6):301-5.
[24]. Silveira ER, Cademartori MG, Schuch HS, Corrêa MB, Ardenghi TM, Armfield J, Horta BL, Demarco FF. The vicious cycle of dental fear at age 31 in a birth cohort in Southern Brazil. Community Dent Oral Epidemiol. 2021 Aug;49(4):354-361.
[25]. Thomson WM, Stewart JF, Carter KD, Spencer AJ. Dental anxiety among Australians. Int Dent J. 1996 Aug;46(4):320-4.
[26]. Armfield JM, Stewart JF, Spencer AJ. The vicious cycle of dental fear: exploring the interplay between oral health, service utilization and dental fear. BMC Oral Health. 2007 Jan 14;7:1.
[27]. Armfield JM. What goes around comes around: revisiting the hypothesized vicious cycle of dental fear and avoidance. Community Dent Oral Epidemiol. 2013 Jun;41(3):279-87.
[28]. Hall RK. Management of the sick and handicapped child in general dental practice. Aust Dent J. 1967 Aug;12(4):323-31.
[29]. De Jongh A, Schutjes M, Aartman IH. A test of Berggren's model of dental fear and anxiety. Eur J Oral Sci. 2011 Oct;119(5):361-5.
[30]. Carlsson V, Hakeberg M, Wide Boman U. Associations between dental anxiety, sense of coherence, oral health-related quality of life and health behavior--a national Swedish cross-sectional survey. BMC Oral Health. 2015 Sep 2;15:100.
[31]. Moore R, Brødsgaard I, Rosenberg N. The contribution of embarrassment to phobic dental anxiety: a qualitative research study. BMC Psychiatry. 2004 Apr 19;4:10.
[32]. Locker D, Shapiro D, Liddell A. Negative dental experiences and their relationship to dental anxiety. Community Dent Health. 1996 Jun;13(2):86-92. PMID: 8763138IF: 1.7 B4.
[33]. Vassend O. Anxiety, pain and discomfort associated with dental treatment. Behav Res Ther. 1993 Sep;31(7):659-66.
[34]. Moore R, Brødsgaard I. Differential diagnosis of odontophobic patients using the DSM-IV. Eur J Oral Sci. 1995 Apr;103(2 ( Pt 1)):121-6.
[35]. Liddell A, Gosse V. Characteristics of early unpleasant dental experiences. J Behav Ther Exp Psychiatry. 1998 Sep;29(3):227-37.
[36]. Armfield JM, Slade GD, Spencer AJ. Cognitive vulnerability and dental fear. BMC Oral Health. 2008 Jan 24;8:2.
[37]. Barlow DH. Anxiety and its disorders: the nature and treatment of anxiety and panic. New York: Guilford press; 2002.
[38]. Skinner BF. Science and human behavior. New York: Free Press; 1965.
[39]. Appukuttan D. P. (2016). Strategies to manage patients with dental anxiety and dental phobia: literature review. Clinical, cosmetic and investigational dentistry, 8, 35–50.
[40]. Buhre W,Disma N,Hendrickx J,et al.European society of anaesthesiology task force on nitrous oxide:a practice [J]. BrJAnaesth,2019,122(5):587-604.
[41]. Kharouba J,Somri M,Hadjittofi C,et al.Effectiveness and safety of nitrous oxide as a sedative agent at 60%and 70% compared to 50% concentration in pediatric dentistry setting [J].J Clin Pediatr Dent,2020,44(1):60-65.
[42]. Atkin T, Comai S, Gobbi G. Drugs for insomnia beyond benzodiazepines:pharmacology, clinical applications, and discovery[J]. Pharmacol Rev, 2018,70(2): 197-245.
[43]. Steinvik, L. M., Svartdal, F., & Johnsen, J. K. (2023). Delay of Dental Care: An Exploratory Study of Procrastination, Dental Attendance, and Self-Reported Oral Health. Dentistry journal, 11(2), 56.
[44]. Anderson, K., & Priebe, S. (2021). Concepts of Resilience in Adolescent Mental Health Research. The Journal of adolescent health : official publication of the Society for Adolescent Medicine, 69(5), 689–695.
[45]. Sharma, R., George, M., & Krishnan, M. (2024). Efficacy of Preemptive Analgesia on Pain Perception After Simple Tooth Extraction: A Prospective Study. Cureus, 16(4), e58262.
[46]. Davis TE, May A, Whiting SE. Evidence-based treatment of anxiety and phobia in children and adolescents: current status and effects on the emotional response. Clin Psychol Rev. 2011 Jun;31(4):592–602.
[47]. Janthasila, N., & Keeratisiroj, O. (2023). Music therapy and aromatherapy on dental anxiety and fear: A randomized controlled trial. Journal of dental sciences, 18(1), 203–210.