1. Introduction
As of the end of 2023, approximately 1.29 million people living with HIV/AIDS (Human Immunodeficiency Virus/Acquired Immune Deficiency Syndrome) were reported to be alive nationwide, with 110,500 new cases reported in 2023, of which 98.5% were transmitted through sexual contact [1]. Currently, sexual transmission is the predominant mode of HIV transmission in China. The epidemic is characterized by a high degree of concealment and extensive social coverage. At the same time, high-risk populations often exhibit complex behaviors and high mobility, making the implementation of prevention and control measures increasingly difficult. As a result, the number of newly reported infections each year shows no significant downward trend [2]. To identify HIV-infected individuals in a timely manner and provide precise intervention strategies, it is of great significance to adopt new research methods that offer novel approaches to intervention. Molecular transmission network technology uses the genetic similarity of HIV sequences to construct a network at the molecular level, reflecting potential associations between infected individuals. This approach holds substantial public health significance for monitoring the HIV epidemic, understanding transmission relationships, and assessing transmission risk [3]. This study conducts a molecular transmission network analysis of HIV-infected individuals in key sub-districts and towns of Jiulongpo District, Chongqing, aiming to provide a reference for precision AIDS intervention efforts in the region.
2. Subjects and methods
2.1. Subjects
Newly reported HIV/AIDS cases from 2021 to 2023 in key sub-districts and towns of Jiulongpo District, Chongqing, were selected as the study subjects. Inclusion criteria: (1) Confirmed HIV infection; (2) Age ≥ 18 years; (3) No history of antiretroviral therapy; (4) Voluntary participation in the study. Exclusion criteria: (1) Failure in gene extraction, amplification, or sequencing; (2) Duplicate sequences; (3) Refusal to participate in the study. All participants were informed of the study’s purpose, and all information and data were kept strictly confidential. This study was approved by the Medical Ethics Committee of the Jiulongpo District Center for Disease Control and Prevention.
2.2. Methods
2.2.1. Epidemiological information
General demographic characteristics and transmission routes were collected from the National AIDS Prevention and Control Information System.
2.2.2. Nucleic acid extraction, amplification, and sequencing
Blood samples from the study subjects were sent to Chongqing Boyao Medical Testing Laboratory Co., Ltd. for purification and sequencing. RNA was extracted and purified from plasma samples, followed by nested PCR to amplify the pol gene.
2.2.3. HIV genotyping analysis
Sequencing results were assembled and cleaned using Sequencer 5.0 software. The processed sequences were then uploaded to the China HIV Sequence Database (https://nmdc.cn/hiv/) for subtype identification using the HIV genotyping tool. A neighbor-joining phylogenetic tree was constructed using MEGA 7.0 software, with the Maximum Likelihood model and a bootstrap value set to 1000.
2.2.4. Molecular transmission network analysis
The HIV-TRACE program was used on a CentOS 7 platform to construct the molecular transmission network of HIV-infected individuals. Pairwise genetic distances between sequences were calculated using the Tamura-Nei 93 (TN93) model. The optimal genetic distance threshold was determined based on the distance that identified the largest number of transmission clusters. Epidemiological information was assigned to all nodes in the molecular network, and visualization and presentation were conducted using the web-based HIV-TRACE platform (https://veg.github.io/hivtrace-viz).
2.2.5. Statistical analysis
SAS 9.4 software was used to perform statistical descriptions of the basic demographic characteristics of the study population. Categorical variables were expressed as n (%). Differences in network composition were analyzed using the χ² test or Fisher’s exact test, with a P-value < 0.05 considered statistically significant.
3. Results
3.1. Basic information of the study population
A total of 111 subjects were surveyed in this study, with successful amplification of pol gene sequences obtained from 83 individuals (amplification rate: 74.8%). Among them, males accounted for 89.16% (74/83), individuals aged 50 years and above accounted for 59.04% (49/83), and those with an education level of junior high school or below accounted for 65.06% (54/83). Regarding marital status, the majority were either married or had a spouse (45.78%, 38/83) or unmarried (38.55%, 32/83). The main occupations were housework and unemployment (36.14%, 30/83) and commercial services (34.94%, 29/83). The predominant transmission route was heterosexual contact, accounting for 65.06% (54/83). See Table 1.
|
Variable |
Number of Cases (n=83) |
Included in Network (n=18) |
Not Included in Network (n=65) |
χ2 Value |
P Value |
|
|
Gender |
Male |
74(89.16%) |
15(20.27%) |
59(79.73%) |
0.3995* |
|
|
Female |
9(10.84%) |
3(33.33%) |
6(66.67%) |
|||
|
Age |
<50 |
34(40.96%) |
2(5.88%) |
32(94.12%) |
8.4701 |
0.0036 |
|
≥50 |
49(59.04%) |
16(32.65%) |
33(67.35%) |
|||
|
Education Level |
Junior high school or below |
54(65.06%) |
16(29.63%) |
38(70.37%) |
5.7412 |
0.0166 |
|
High school or above |
29(34.94%) |
2(6.90%) |
27(93.10%) |
|||
|
Occupation |
Housework/Unemployed |
30(36.14%) |
12(40.00%) |
18(60.00%) |
0.0142* |
|
|
Commercial Services |
29(34.94%) |
3(10.34%) |
26(89.66%) |
|||
|
Retired/Withdrawn |
8(9.64%) |
2(25.00%) |
6(75.00%) |
|||
|
Others |
16(19.28%) |
1(6.25%) |
15(93.75%) |
|||
|
Marital Status |
Unmarried |
32(38.55%) |
5(15.63%) |
27(84.38%) |
4.3809 |
0.1119 |
|
Married/With Spouse |
38(45.78%) |
12(31.58%) |
26(68.42%) |
|||
|
Divorced/Widowed |
13(15.66%) |
1(7.69%) |
12(92.31%) |
|||
|
Transmission Route |
Heterosexual |
54(65.06%) |
18(33.33%) |
36(66.67%) |
12.3436 |
0.0004 |
|
Homosexual |
29(34.94%) |
0(0.00%) |
29(100.00%) |
|||
|
Commercial Sexual Behavior |
Present |
38(45.78%) |
14(36.84%) |
24(63.16%) |
9.4788 |
0.0021 |
|
Absent |
45(54.22%) |
4(8.89%) |
41(91.11%) |
|||
|
Gene Subtype |
CRF07_BC |
41(49.40%) |
4(9.76%) |
37(90.24%) |
<0.0001* |
|
|
CRF01_AE |
20(24.10%) |
12(60.00%) |
8(40.00%) |
|||
|
CRF08_BC |
11(13.25%) |
0(0.00%) |
11(100.00%) |
|||
|
CRF105_0108 |
3(3.61%) |
2(66.67%) |
1(33.33%) |
|||
|
Others |
8(9.64%) |
0(0.00%) |
8(100.00%) |
|||
|
* Fisher’s exact test |
||||||
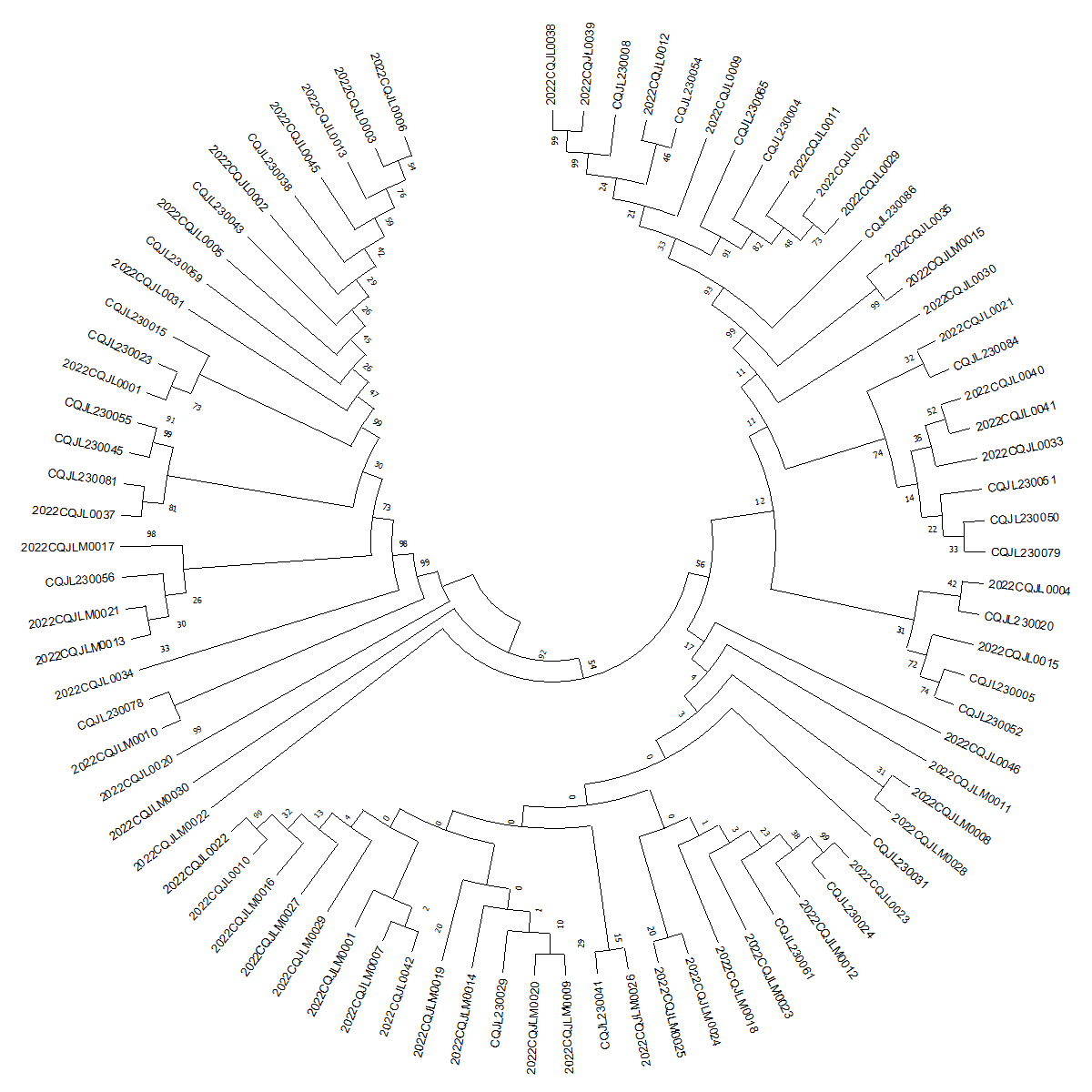
3.2. HIV subtype analysis
Among the 83 successfully amplified gene sequences, 49.40% (41/83) were identified as subtype CRF07_BC, 24.10% (20/83) as CRF01_AE, 13.25% (11/83) as CRF08_BC, and 3.61% (3/83) as CRF105_0108. Additionally, there were 2 cases each of subtypes CRF55_01B and CRF80_0107, and one case each of subtype B, CRF104_0107, CRF114_0155, and CRF79_0107. Phylogenetic analysis based on the constructed evolutionary tree showed that the sequences clustered into distinct clades, with several clusters exhibiting bootstrap values exceeding 90%, forming numerous short-branch evolutionary clusters. See Figure 1.
3.3. Molecular network characteristics analysis
At a genetic distance threshold of 1.5%, the number of clusters reached its maximum. The constructed molecular network had a network inclusion rate of 21.69% (18/83), forming a total of 6 molecular clusters. Among these, one cluster consisted of 8 nodes, while the remaining clusters each consisted of 2 nodes. The total number of links among all nodes in the network was 38, with the highest number of links for a single node being 6. Significant differences in network inclusion rates were observed across different age groups, gene subtypes, educational levels, commercial sexual behavior, and occupations (P < 0.05). See Table 1.
3.4. Characteristics analysis of networked individuals
Among the individuals included in the molecular network, the gene subtypes were CRF01_AE (12 cases), CRF07_BC (4 cases), and CRF105_0108 (2 cases). The largest molecular cluster was composed of the CRF01_AE subtype, all of whom were male, with five nodes having link counts of four or more. All networked individuals were infected through heterosexual transmission, with males accounting for 83.33% (15/18), those aged 50 and above comprising 88.89% (16/18), and 88.89% (16/18) having an educational level of junior high school or below. Additionally, 77.78% (14/18) reported engaging in commercial sexual behavior, and 66.67% (12/18) were houseworkers or unemployed. See Table 1 and Figure 2.
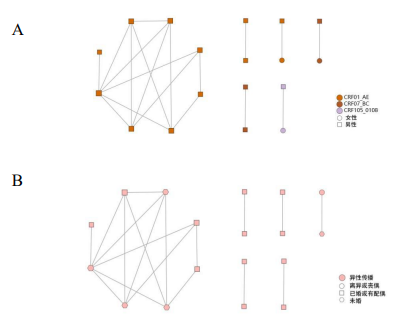
A: Molecular transmission network diagram by gene subtype and gender
B: Molecular transmission network diagram by transmission route and marital status
Figure 2. Distribution characteristics of the molecular transmission network
4. Conclusion and discussion
The results of this study indicate that CRF07_BC and CRF01_AE are the predominant HIV strains currently circulating in the key sub-districts and towns, consistent with findings from other regions [5]. The subtype analysis also revealed the presence of multiple recombinant forms, reflecting a complex genetic composition that aligns with the overall epidemic trends in China [8]. Molecular network analysis showed that all nodes with link counts ≥4 were included in the largest CRF01_AE molecular cluster, and all these individuals were male. According to information inquiries, the current residences of infected individuals within this cluster are located within the studied sub-district or adjacent sub-districts, suggesting the possible existence of hidden commercial sex venues in the area, which warrants focused attention.
The study results show that among the individuals included in the molecular network, those aged 50 and above accounted for as high as 88.89%. In recent years, the number and proportion of middle-aged and elderly HIV/AIDS patients newly reported in China have shown a significant upward trend, highlighting the urgent need to address HIV infection among this demographic [11]. From January to October 2020, the proportion of newly reported HIV/AIDS cases aged 50 and above in Chongqing increased from 35.10% in 2015 to 60.60%, making this group one of the key targets for public health education and intervention in Chongqing [12]. On one hand, rapid socioeconomic development and continuous improvements in healthcare have led to a rising proportion of middle-aged and elderly populations; on the other hand, this group generally has lower educational levels, with relatively limited knowledge and risk perception regarding HIV/AIDS. Moreover, due to declining labor capacity, many face financial difficulties, and a large portion reside in towns and rural areas, where relatively monotonous daily activities and potential feelings of social isolation prevail. Under such circumstances, these individuals may be more likely to frequent low-tier commercial sex venues to meet certain social or emotional needs [13]. Therefore, subsequent prevention and control efforts should prioritize tailored interventions for the middle-aged and elderly population to promote the integration of knowledge, belief, and behavior regarding HIV prevention.
Furthermore, subsequent information inquiry revealed that among the CRF01_AE infected individuals included in the network, there was one couple in which the female spouse was newly infected, indicating potential shortcomings in intervention efforts targeting serodiscordant couples. Due to the unique nature of the spousal relationship, serodiscordant couples represent a high-risk group for sexual transmission of HIV [14]. However, intervention implementation faces significant challenges owing to confidentiality concerns, marital dynamics, family factors, sexual behavior patterns, and reproductive intentions, often resulting in suboptimal outcomes [15]. Therefore, ongoing efforts should focus on strengthening communication between patients and their spouses and encouraging consistent condom use during sexual activity within HIV-affected families to effectively reduce transmission risk.
This study has several limitations. Due to constraints in project duration and funding, the number of collected gene sequences was relatively small. Additionally, given the sensitive nature of HIV/AIDS patient status, selection bias may have occurred in choosing study participants. Future research should aim to include a larger number of sequences and integrate clinical and epidemiological data to more comprehensively evaluate the molecular network characteristics and potential transmission relationships among infected individuals.
In summary, this study constructed an HIV molecular transmission network to elucidate the transmission characteristics of newly reported HIV/AIDS cases in key streets and towns of Jiulongpo District, Chongqing City, from 2021 to 2023. By integrating demographic and epidemiological data, the results revealed a diverse range of viral genotypes among the infected individuals, who were predominantly older adults with lower educational levels and mainly infected through sexual transmission. The findings highlight the need to prioritize targeted interventions for middle-aged and elderly populations as well as the spouses of HIV-positive patients.
Funding project
Key Public Health Specialty (Discipline) Development Project of Chongqing (YWBF2022072); Jiulongpo District Science and Technology Program (2022-02-017-Y)
References
[1]. China CDC STD and AIDS Prevention and Control Center. (2024). National HIV/AIDS and STD epidemic report, December 2023.Chinese Journal of AIDS & STD, 30(3), 225.
[2]. Wang, Z. H., Wu, S. L., Zhang, C. Y., et al. (2023). Epidemiological characteristics of HIV in Fujian Province based on molecular transmission network analysis.Chinese Journal of Public Health, 39(12), 1526–1529.
[3]. Cheng, P., Liu, J. F., Wang, J. L., et al. (2024). Molecular transmission network analysis of HIV-1 CRF01_AE strain epidemic characteristics in Kunming City.Chinese Journal of Disease Control, 28(5), 574–580.
[4]. Guo, Q., Wang, H., Qi, X. C., et al. (2023). Study on transmission clusters and molecular network characteristics of HIV-1 infected individuals in Jilin Province.Chinese Journal of Health Engineering, 22(6), 732–736.
[5]. Gou, Z., Ai, Y., Xu, W. P., et al. (2024). Genetic subtypes and molecular transmission characteristics of newly reported HIV-1 infected individuals in Luzhou City.Modern Preventive Medicine, 51(7), 1302–1307, 1319.
[6]. Fang, Q., Shen, Y. L., Liu, G. Z., et al. (2024). Study on drug resistance and molecular transmission network of newly reported HIV infections in Bengbu City, 2021–2022.Anhui Journal of Preventive Medicine, 30(1), 23–27.
[7]. Duan, X., Liang, X. Y., Wang, J. B., et al. (2023). Molecular transmission network analysis of HIV viral gene subtypes among newly reported men who have sex with men in Dehong Prefecture, Yunnan Province, 2010–2019.Shanghai Journal of Preventive Medicine, 35(12), 1168–1174.
[8]. Hemelaar, J., Ramyiadarsini, E., Jason, Y., et al. (2019). Global and regional molecular epidemiology of HIV-1, 1990–2015: A systematic review, global survey, and trend analysis.The Lancet Infectious Diseases, 19(2), 143–155. https: //doi.org/10.1016/S1473-3099(18)30665-6
[9]. Qiao, R. J., Zhang, L. C., Feng, Y., et al. (2023). Analysis of pretreatment drug resistance and molecular transmission network characteristics among newly reported HIV/AIDS patients in parts of Gansu Province, 2020–2021.Chinese Journal of AIDS & STD, 29(8), 860–865.
[10]. Feng, Y., Wang, D., & Xing, H. (2023). Molecular transmission networks facilitate precise HIV/AIDS prevention and control in China.Chinese Journal of AIDS & STD, 29(1), 1–8.
[11]. Wei, H., Li, B., & Lan, G. H. (2021). Progress in research on the epidemiological characteristics of AIDS among elderly populations in China.Applied Preventive Medicine, 27(2), 189–193.
[12]. Qin, F., Duan, X. J., Yuan, R. H., et al. (2023). Epidemiological characteristics and trend analysis of HIV/AIDS among individuals aged 50 and above in the county of Chongqing City.Modern Medical and Health, 39(21), 3647–3651.
[13]. Qin, C., Huang, Z. B., Huang, Z. K., et al. (2023). Molecular transmission network characteristics and influencing factors of HIV-1 in Longzhou County.Chinese Journal of AIDS & STD, 29(2), 136–141.
[14]. Liu, H., Gong, Z., Yan, X., et al. (2024). Principal component analysis of risk factors for spousal seroconversion due to unsafe sexual behaviors among HIV-discordant couples.Chinese Journal of Preventive Medicine, 25(3), 357–361.
[15]. Chen, X. Y., Song, L., Jiang, A., et al. (2024). Analysis of factors affecting sexual transmission between spouses among HIV-positive couples.Ningxia Medical Journal, 46(4), 314–317.
Cite this article
He,W.;Chen,H.;Liu,Y.;He,J. (2025). Molecular network analysis of HIV infections in key sub-districts and towns of one district, Chongqing, 2021-2023. Journal of Clinical Technology and Theory,3(2),46-51.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Journal:Journal of Clinical Technology and Theory
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. China CDC STD and AIDS Prevention and Control Center. (2024). National HIV/AIDS and STD epidemic report, December 2023.Chinese Journal of AIDS & STD, 30(3), 225.
[2]. Wang, Z. H., Wu, S. L., Zhang, C. Y., et al. (2023). Epidemiological characteristics of HIV in Fujian Province based on molecular transmission network analysis.Chinese Journal of Public Health, 39(12), 1526–1529.
[3]. Cheng, P., Liu, J. F., Wang, J. L., et al. (2024). Molecular transmission network analysis of HIV-1 CRF01_AE strain epidemic characteristics in Kunming City.Chinese Journal of Disease Control, 28(5), 574–580.
[4]. Guo, Q., Wang, H., Qi, X. C., et al. (2023). Study on transmission clusters and molecular network characteristics of HIV-1 infected individuals in Jilin Province.Chinese Journal of Health Engineering, 22(6), 732–736.
[5]. Gou, Z., Ai, Y., Xu, W. P., et al. (2024). Genetic subtypes and molecular transmission characteristics of newly reported HIV-1 infected individuals in Luzhou City.Modern Preventive Medicine, 51(7), 1302–1307, 1319.
[6]. Fang, Q., Shen, Y. L., Liu, G. Z., et al. (2024). Study on drug resistance and molecular transmission network of newly reported HIV infections in Bengbu City, 2021–2022.Anhui Journal of Preventive Medicine, 30(1), 23–27.
[7]. Duan, X., Liang, X. Y., Wang, J. B., et al. (2023). Molecular transmission network analysis of HIV viral gene subtypes among newly reported men who have sex with men in Dehong Prefecture, Yunnan Province, 2010–2019.Shanghai Journal of Preventive Medicine, 35(12), 1168–1174.
[8]. Hemelaar, J., Ramyiadarsini, E., Jason, Y., et al. (2019). Global and regional molecular epidemiology of HIV-1, 1990–2015: A systematic review, global survey, and trend analysis.The Lancet Infectious Diseases, 19(2), 143–155. https: //doi.org/10.1016/S1473-3099(18)30665-6
[9]. Qiao, R. J., Zhang, L. C., Feng, Y., et al. (2023). Analysis of pretreatment drug resistance and molecular transmission network characteristics among newly reported HIV/AIDS patients in parts of Gansu Province, 2020–2021.Chinese Journal of AIDS & STD, 29(8), 860–865.
[10]. Feng, Y., Wang, D., & Xing, H. (2023). Molecular transmission networks facilitate precise HIV/AIDS prevention and control in China.Chinese Journal of AIDS & STD, 29(1), 1–8.
[11]. Wei, H., Li, B., & Lan, G. H. (2021). Progress in research on the epidemiological characteristics of AIDS among elderly populations in China.Applied Preventive Medicine, 27(2), 189–193.
[12]. Qin, F., Duan, X. J., Yuan, R. H., et al. (2023). Epidemiological characteristics and trend analysis of HIV/AIDS among individuals aged 50 and above in the county of Chongqing City.Modern Medical and Health, 39(21), 3647–3651.
[13]. Qin, C., Huang, Z. B., Huang, Z. K., et al. (2023). Molecular transmission network characteristics and influencing factors of HIV-1 in Longzhou County.Chinese Journal of AIDS & STD, 29(2), 136–141.
[14]. Liu, H., Gong, Z., Yan, X., et al. (2024). Principal component analysis of risk factors for spousal seroconversion due to unsafe sexual behaviors among HIV-discordant couples.Chinese Journal of Preventive Medicine, 25(3), 357–361.
[15]. Chen, X. Y., Song, L., Jiang, A., et al. (2024). Analysis of factors affecting sexual transmission between spouses among HIV-positive couples.Ningxia Medical Journal, 46(4), 314–317.