1. Introduction
Cephalosomatic Anastomosis (CSA), or head transplantation, is a surgery that involves removing the head of the patient who has a terminal related illness then connecting the blood vessels, trachea, cervical spinal cord, alimentary canal, and other tissues to a doner with no vital signs. Among these, cervical spinal cord be reattached is critical for successful CSA, as well as long-term immunosuppression and postoperative rehabilitation support. Currently, technical and ethical challenges remain major obstacles to its clinical application.
Since the 1900s humankind has investigated the possibility of CSA. Past head transplant experiments have focused on animals, like dogs, rats, and monkeys with varying results. The most famous of these was a human head transplant in human cadavers proposed by Dr. Sergio Canavero, who claimed that a successful operation could restore most of the body’s function. Canavero invented a surgery named GEMINI Spinal Cord Fusion (SCF) to do that.
In terms of immunology, CSA involves complex immune challenges, requiring patients to take immunosuppressive drugs for extended periods. Unlike the immune issues faced in organ transplantation, where the recipient's immune system mounts a response against the donor organ, CSA presents a unique scenario. The head serves as the primary immune control center, while the donor body contains the majority of the immune system components, such as bone marrow and lymph nodes. Consequently, the donor body's immune system may perceive the recipient head as a "foreign object," potentially triggering rejection responses.
Although existing materials suggest that this surgery is theoretically feasible, it may still be prohibited due to its inconsistency with prevailing moral concepts. It brings significant challenges in the field of public health, such as psychological and ethical concerns. To realize this surgery, these challenges need to be anticipated and controlled in the first place. If the surgery succeeds, it will mark a major advancement in human medicine and ignite profound discussions in ethics, potentially reshaping our understanding of life, death, and self-cognition. Even if the surgery fails, the solutions developed during its process can still be adopted and applied in other related branches of medicine.
This literature review builds upon these specific aspects by reviewing the history of the procedure, examining medical barriers and advancements, and exploring the dynamics of ethical implications. Then it discusses the feasibility of the surgery, the broader ethical and societal impacts of CSA, and the application of CSA-related techniques in other branches of medicine. Finally, it summarizes certain limitations and provides recommendations for future improvements.
2. Literature review
2.1. The history of cephalosomatic anastomosis (CSA)
In this section, the past experiments in CSA will be elaborated with a brief introduction to those cases and the problems that they faced.
2.1.1. Dogs
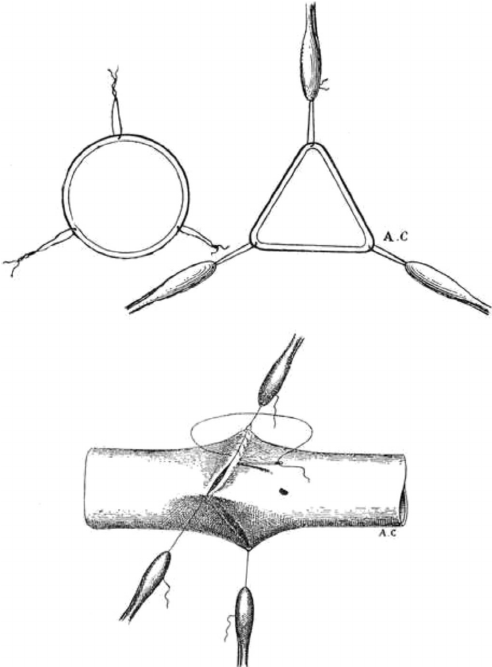
As shown in Figure 1, In 1908, surgeon Dr. Alex Carrel from France and physiologist Dr. Charles Guthrie from America performed the world’s first CSA on dogs. They were granted the Nobel Prize for their contribution to reliable vascular anastomoses in 1912 [1]. By transplanting the head of a dog onto another dog’s neck, using very thin threads and fine needles as sutures to join the artery together, they allowed blood to flow through the transplanted head and then the host’s head. Though the head was without blood flow for twenty minutes and deteriorated rapidly after the surgery, it still exhibited auditory, visual, and cutaneous reflex movements. The surgery also showed that the method they used could effectively prevent hemorrhage and maintain the structure of the anastomoses while ensuring free blood flow at the suture.
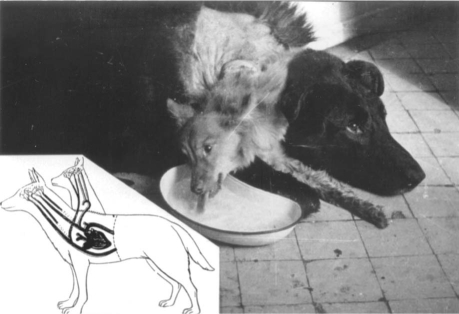
Soviet scientist Dr. Vladimir Demikhov made another milestone in head transplantation. He performed the first successful coronary bypass surgery on a dog model in 1953, which created a new path for blood flow and maintained blood supply during organ transplantation.As shown in Figure 2, Dr. Demikhov also performed a dog head transplant in 1954 [2] (Figure 2). Dr. Demikhov utilized a unique approach by transplanting the head and forelimbs of one dog onto the body of an adult dog, creating a two-headed organism. The key surgical techniques involved precise vascular anastomosis to restore blood circulation and ensure adequate oxygen and nutrient supply to the donor head. His dogs showed more functional capability than Carrel and Guthrie’s experiment; they could move, see, and drink water.
An American neurosurgeon, Dr. Robert White, also tried a head transplant on a dog in 1965. His approach involved transplanting a brain into a separate body, which is very different from the procedures Guthrie and Demikhov performed. This required Dr. White to come up with a brand-new method for the surgery. One of his main challenges was maintaining blood flow to the brain.
He created a vascular loop to preserve the anastomosis of the internal maxillary and internal carotid arteries. This system could still ensure blood flow even if the second cervical vertebral body was severed, which he called “auto-prefusion.” Dr. White successfully transplanted six dog brains, with the longest survival being six days, demonstrating the possibility of short-term brain transplantation [3].
2.1.2. Monkeys
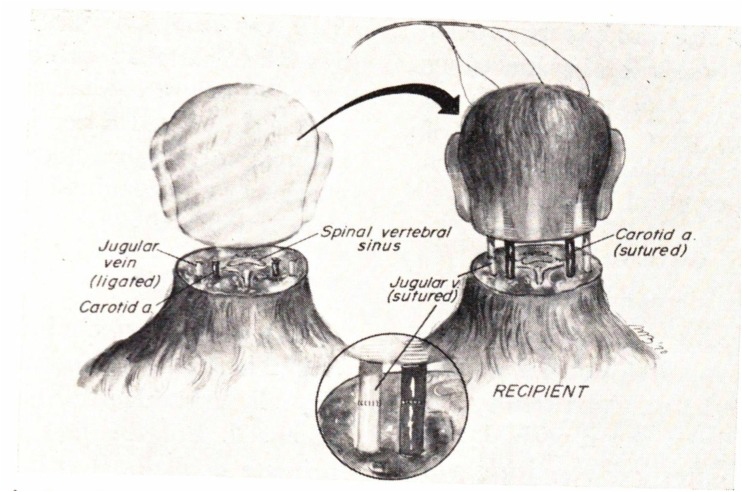
As shown in Figure 3, in 1970, Dr. White also connected isolated monkey heads and bodies to execute the first head transplant on primates. He sutured the jugular vein and carotid artery directly. The fourth to sixth cervical vertebrae were then subjected to a cervical laminectomy. This caused spinal shock and hypotension, so an injection of catecholamines was given to ensure the oxygen supply. Three to four hours after the surgery, the monkeys displayed the ability to chew, bite, swallow, and engage in other behaviors. Dr. White also showed that the monkeys exhibited a pattern of wakefulness through electroencephalogram monitoring. Despite these advancements, revascularization of the brain still remained a challenge [1, 4].
2.1.3. Mice
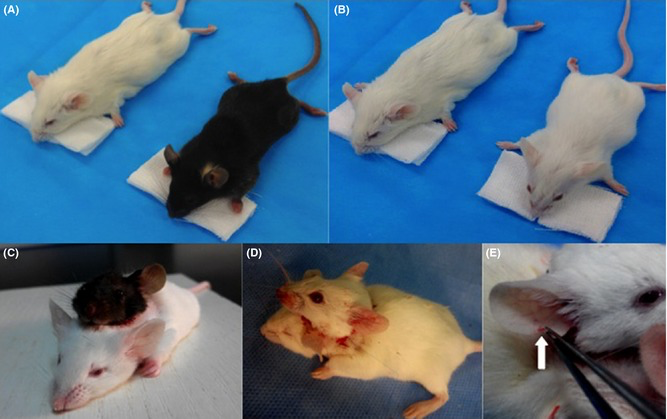
In 2015, further experimentation on CSA was conducted by Chinese surgeon Xiao-Ping Ren [5]. He modified the method of vascular anastomosis, reducing trauma to the test subject and minimizing brain damage. Using electroencephalography and electrocardiography to monitor brain activity and cardiac function during and after surgery ensured the mouse's vital signs were stable. As shown in Figure 4, Dr. Ren surgically anastomosed the mouse body to the blood vessels in the donor's head. The donor and recipient tissues were then sutured together using surgical sutures. His methods resulted in more than half of the mice surviving for over 24 hours, with the longest surviving for six years [6].
2.1.4. Humanoids
As shown in Figure 5, in 2017, society regained interest in this area of research due to an announcement of a possible live human experiment led by Xiao-Ping Ren and Italian surgeon Sergio Canavero. However, the operation was canceled due to the patient’s personal reasons. Instead, the medical team rehearsed the world’s first successful CSA on a dead human being at Harbin Medical University in China. Ren Xiaoping emphasized the correction: "The latest major breakthrough of our team is the completion of the first human head transplant surgical experimental model. We did not perform a head transplant on a live human, nor did we complete an autopsy on a corpse as some reports said" [7].
The surgery took 18 hours and was completed within the planned time limit. This exercise resulted in several advances, including optimizing surgical procedures, preserving major nerves, and assessing spinal stability. One of the most critical steps in the entire surgery was the GEMINI technique, which Canavero planned for a highly controlled cross-sectional resection of the spinal cord to minimize damage to the cortex [8].

2.2. Medical and ethical problems
With the development of medical technology, the scientific community may witness the implementation of CSA. It is undeniable that CSA is an intergenerational surgery; it might even be a key to space travel or other incredible achievements that humankind has never managed to accomplish. However, in 2017, the first CSA planned to operate on a live human was canceled, with no further news about the next opportunity for the operation at present. While the successful development of such surgery is seen as a major medical advance that will change people's lives, it also brings significant challenges, both medical and ethical, which need to be anticipated and addressed.
A leading passage in Surgical Neurology International (SNI) indicated that the plan by Sergio Canavero for CSA is to first cool the head of the patient and the donor’s body, which came from a brain-dead donor, to minimize cell damage from oxygen loss. The patient’s head and donor’s spine would be fused using a method called GEMINI. In this EPQ, I will review this possibility by examining these issues and potential breakthroughs.
2.2.1. Medical
CAS is very complex and involves many difficulties to overcome and consider, such as:
• Ensuring that the head and the body do not reject each other.
• Linking blood vessels and cervical spinal cord together.
• Surgical techniques for the attachment of the head to the body.
• Postoperative recovery.
• How signals from the brain and body are processed and connected.
• Immune responses during transplants, how to prevent rejection, and immunosuppressive therapy.
• Ethical issues of human head transplants, including the patient's identity, rights, and psychological impact [9].
This technology is still in the research stage and, along with regenerative medicine involving stem cell technology and biomaterials, it is hoped to be accomplished as the scientific fields and technical challenges involved are very complex. In the next session, I will review this possibility by examining these issues and potential breakthroughs [10].
2.2.1.1. Immunosuppression
In head transplants, the body is seen as the donor organ and the head as the recipient, as the head is where a person stores all of their personal identity. Consequently, handling the new organ's rejection might be quite difficult. At the time of Guthrie and Carrel's Nobel Prize win in 1912, their research was not applicable to humans, and organs transplanted into different hosts deteriorated. Despite advancements in our knowledge of how to preserve perfusion during transplant surgery, problems like immunosuppression persisted [11].
Following the discovery of immunosuppressants like azathioprine, 6-mercaptopurine, and corticosteroids, medical teams from all around the world started transplanting human kidneys and hearts [9]. In the 1960s and 1970s, White carried out his transplant studies when immunosuppressants were already on the market. Histological analysis of brain tissue after the monkeys passed away indicated that White's use of these medications in his monkey head transplant research prevented super-rejection reactions in the primates [12]. Nevertheless, this came at the expense of incredibly high immunosuppressive drug dosages. Indeed, White's monkey died nine days after the transplant due to the high dosages of immunosuppressants required to avoid rejection [12].
2.2.1.2. Spinal engagement
In 2015, Sergio Canavero published an article titled "The 'Gemini’ Spinal Cord Fusion Protocol: Reloaded" [13]. In this publication, Canavero presented his proposed GEMINI Spinal Cord Fusion (SCF) methodology. The goal of SCF is to cut the spinal cord as sharply as possible while minimizing harm to the white matter axons and neurons in the layers of the cortex. One of the key components of this approach is the use of a nano knife, composed of a thin coating of silicon nitride with an edge that is nanometer sharp, as an alternative to using a specially constructed diamond slicing knife. This method also employs unique materials (fusants/sealants: chitosan, polyethylene glycol [PEG]) that can seal damaged or leaky neurons or fuse broken axons together [13].
It is crucial that the spinal cord stumps not be separated during the procedure. If they are, transplantable tiny neuronal axonal constructs, which are internalized within a designed tube, can be used to fill the gap. However, if the spinal cord is properly linked, the patient may need to take strong immunosuppressive medications, and it remains unclear whether doing so will resolve the issue of rejection [13].
A case study was reported in 2005 of a 24-year-old woman who suffered a complete anatomical transection of the spinal cord at the T6-7 level in a skiing accident. The patient experienced a total loss of T6-7 motor function following the injury. Thirty-nine months after the spinal cord damage, the patient underwent spinal cord reconstruction surgery. A year after the procedure, the patient began to regain strength in her abdominal wall and trunk. As her neurological condition improved, Magnetic Resonance Imaging (MRI) showed significant longitudinal extension of the soft tissue mass. Four years post-surgery, the patient was able to walk long distances with the aid of a walker, although her walking ability was still limited. This case demonstrates that spinal cord transection can be repaired with functional healing; however, the repair is not perfect and can take several years, especially if the gap to be filled is large (8 mm and 4 cm) [9, 13].
In general, the probability of full functional recovery following spinal restoration remains low, and the process of healing can be prolonged and imperfect [13].
2.2.1.3. Brain tissue preservation
A common neuron-protective treatment for patients suffering from hypoxic-ischemic encephalopathy, stroke, and cardiac arrest is induced hypothermia. White et al. [12] used deep hypothermia (less than 25°C) in their early monkey tests to preserve the transplanted brain after surgical ischemia [12].
The ideal cooling time has not yet been established, as acknowledged by Dr. Ren [5] and other members of the group. They do, however, think that hypothermia won't be an issue with the CSA protocol that their team has proposed because the recipient's body (though it might suffer from hypothermia complications like bradycardia, hypotension, and thrombosis) will eventually be discarded, and the donor's brain-dead body won't suffer from hypothermia [5].
2.2.2. Ethical concerns
It is necessary to address some key issues before performing this surgery on live humans, as it will cause controversy in many ethical and philosophical fields. These issues clearly challenge existing moral and ethical concepts. According to a paper by JO BLOGGS, some of the most important ethical challenges facing CSA include:
• Transplants should be determined by the procedure's success rather than the recipient's or donor's income and influence.
• Consider the biological distinctions between the donor and recipient.
• Verify that there is no self-awareness or brain death in the donor's body.
• Take into account the donor's family's sentiments, as they will have to deal with difficult decisions involving living bodies.
• Prevent the wealthy and influential from misusing this transplant technology [14, 15].
Does society need to establish sound norms and guidelines to address these issues? Should we not openly discuss and collect public opinion through a variety of channels, including public forums, print and broadcast media? There is no doubt that such an endeavour would be valuable, as the result would be a more comprehensive and in-depth understanding of the issues and concerns, as well as the benefits of relevant research and new treatments.
Moreover, do we need to carefully assess the balance between risks and benefits? A key question is: 'Is it worth taking the risk of long-term immunosuppression in order to undergo these “non-lifesaving” procedures?’ In the case of head transplants, the risk-benefit trade-off will be more straightforward, as the procedure is intended to be 'life-saving,’ and therefore the risks can be somewhat justified by the benefits. Another difficult and urgent question is: how do we design and implement an 'exit strategy’ if all attempts to reverse rejection fail in the case of chronic rejection and the transplanted head has to be removed?
2.2.3. Social acceptance
Animals are killed in such trials, as demonstrated by earlier research by Drs. White and Demikhov [12, 16]. Even though the outcome of these experiments is more about advancing scientific knowledge, head transplantation is, at its core, a life-extending procedure rather than a therapeutic one. This may influence the decision to have the procedure done. Even if head transplantation becomes technically and scientifically possible in the future, society may still find it difficult to embrace this new treatment.
In this regard, Xiao-Ping Ren stated that the history of human medical development has often been controversial. For example, when the first kidney transplant was performed in 1953, academic circles and society criticized the procedure, believing that people should die naturally and that others should not alter this process. He suggested that new medical techniques often meet opposition, but eventually, societal rules adapt and evolve [17, 18].
In general, any change in physical identity is the biggest challenge faced by a head transplant recipient. The procedure also has the potential to affect identity and lead to psychological disorders such as mood swings, psychosis, and even suicide [17].
2.3. Further considerations
The medical community is on the path of the existence of a long-cherished dream (head transplant surgery), so it should be prepared for possible side effects. The most common challenges are mental wellbeing issues such as psychological, social and ethical. In the field of mental health, it is necessary to consider the increase in psychological disorders caused by confusion about personal identity. In the ethical field, CSA leads to different problems. Therefore, it is necessary to develop ethical guidelines for these advances.
3. Discussion
3.1. Probability of success of CSA experiments
The results of this research tie directly into the broader discourse surrounding CSA, which has been ongoing for over a century. Historical experiments on animals, such as those conducted by Carrel, Demikhov, White, and more recently by Ren and Canavero, have contributed to refining surgical techniques for connecting blood vessels and nerves [11, 12, 16, 19]. This was all done by anastomosing the major blood vessels, including key vessels such as the carotid artery and jugular vein, to ensure that blood circulation was restored between the recipient head and the donor body. But none of the connections to the spinal cord were made, which meant that there was a lack of neurological integration between the host body and the transplanted head, and none of the animal's head was able to control the motor functions of the host body. With the advancement of science and technology, the possibility of physical connectivity and neuro-logical recovery of the spinal cord has been demonstrated through techniques such as Ren's spinal cord fusion and Canavero's GEMINI [20]. Ren's spinal cord fusion uses a special chemical (e.g. Polyethylene Glycol, PEG) that seals and fuses the damaged axon membranes, facilitates the physical connection of the severed nerve fibres, and also encourages the natural regeneration of the nerve fibres to a certain extent. The experiment also applied a specific frequency of electrical stimulation (e.g., 20 Hz continuously) to the damaged area.Ren's spinal cord fusion has been tested in a variety of animal models, including rodents and primates. GEMINI uses special substances that can fuse broken axons together or to seal injured neurons. It is a technology based on a called concept of biological fusion, which could occur both naturally or artificially. In GEMINI, local neurons in the gray matter can reconnect within few days or weeks. Electrical stimulation applied by a spinal cord stimulator across the fusion point accelerates this process. For example, one hour of electrical stimulation at 20 Hz (continuous) applied immediately after severing the severed peripheral nerve remains can reduce the regeneration time from 8-10 weeks to around 3 weeks; similar trends have been observed in humans. However, current experiments have been conducted mainly on animal models and human remains, and complete success has not yet been achieved in living humans.
While earlier experiments faced numerous challenges, including brain revascularization and post-operation survival, recent advancements in immunosuppression therapy and spinal cord fusion technologies have addressed some of these hurdles [19]. However, a major gap remains in overcoming immune rejection, spinal cord integration, and ensuring long-term neurological function, which are all crucial to the success of a head transplant in humans.
By sorting out the existing articles, the results of this study show that although CSA is theoretically possible to be realised in the future, it is still far away from practical application. It is difficult to reattach the donor body to the recipient head while ensuring functional neurological and physiological integration [19, 20]. The limitations of this study include the fact that most animal experiments have focused on vascular anastomoses, with relatively few experiments addressing spinal cord reconnection [21]. Furthermore, there is little proof of long-term usefulness, especially when it comes to sophisticated brain processes like cognition, mobility, and identity retention, even though animal studies indicate short-term survival. The methods employed, like hypothermic brain tissue preservation and the GEMINI spinal fusion protocol, are still in the experimental stage and have not yet been shown to be successful [10].
The results of this review demonstrating the difficulty of achieving CSA. And the cure of spinal cord paralysis remains a great challenge at present. But the scientific community is actively exploring related technologies, such as stem cell therapy technology, which promotes nerve regeneration with stem cells [22]. Reconstruction of damaged spinal cord pathways using some special biomaterials. Combining EEG interface and spinal cord stimulator to stimulate nerve signalling [23].
However, these technologies are still a long way from real clinical application and cure. The ability of neurons to repair spinal cord nerves after damage is extremely limited, especially in the central nervous system (including the spinal cord), where neurons are virtually incapable of regenerating on their own. Even if nerve regeneration is successful, functional connections between the brain and various parts of the body need to be re-established, which involves the correct reconstruction of neural pathways as well as complex functional remodelling [23].
3.2. Ethical issues in CSA
Due to varying legal requirements, societal views, and ethical frameworks, the ramifications of CSA will differ greatly between nations. There would probably be major ethical and legal obstacles for CSA in nations with strong ethical laws, such as the US or the United Kingdom [22]. Public opposition and strict legal restrictions may result from concerns about personal identity, consent, the use of brain-dead donors, and the possibility of psychological trauma .
Although public skepticism and ethical issues would still exist, CSA may be explored more vigorously in nations like China or Russia that have less strict laws on experimental surgery or more lax medical ethics [19]. Although there would probably be ethical and legal issues, the surgery might be seen as a kind of medical breakthrough that could transform the way that severe paralysis or terminal illnesses are treated [9].
In the case of organ transplants, there are not only strict and regulated regulations at the legal level to ensure their legality and fairness. Serious cases of illegal organ transplants are usually punishable by heavy sentences, including imprisonment from three to more than 10 years, and in serious cases, one may even face life imprisonment. At the ethical level, donors will also be required to sign an informed consent form after fully understanding the donation process, the risks of the operation, the possible consequences and the relevant rights. Particular caution will be exercised in the case of organ donation from minors or incapacitated persons, who will need to be assessed by an ethics committee and legally authorised by their guardians. A social monitoring mechanism will also be put in place at the social level, with each organ transplant operation having to be assessed by an independent ethical review committee to ensure that it meets the ethical requirements. At the same time, an open reporting mechanism will be set up to accept social monitoring of illegal transplantation.
So for head transplantation surgery is it also necessary to establish rules and regulations in terms of law, ethics and social supervision to ensure that the head transplantation process is lawful, transparent, open and fair, and to protect the rights and dignity of the donor. The question of the identity of the new individual can also be one of the central controversies. This involves the ability of relatives of both the donor and the recipient to recognise the patient's 'new identity’ and whether the patient will suffer any identity confusion or psychological disorders as a result.
3.3. Future improvements and other application
According to the information above, some further research could be aimed in:
• Improving spinal cord fusion: While GEMINI and other spinal fusion methods have shown promise, long-term success in humans has not been demonstrated. Future research should continue to refine these techniques.
• Neural regeneration: Further research and improved neuroprosthetic techniques are needed to facilitate the repair and reconnection of neurons at the site of spinal cord disruption and to ensure that the spinal cord connections are able to support functional motor and perceptual processing. This requires multidisciplinary collaboration, including the development of better biocompatible materials and related protocols for nerve regeneration [10].
• Ethical and social implications: The psychological, philosophical, and ethical impacts of CSA need to be studied further, especially the effects on personal identity, psychological well-being, and societal acceptance. Ethical guidelines should be developed to navigate the societal and moral questions raised by CSA.
• Long-term survivability: More research is needed into the long-term viability of head transplants, including immune suppression, brain tissue preservation, and the avoidance of organ rejection [20]. The development of personalized immunosuppressant therapies could be critical.
While the concept of CSA may seem far-fetched, the advancements in regenerative medicine, spinal cord repair, and neurobiology offer potential practical applications in treating neurological diseases, spinal cord injuries, and conditions that currently have no effective treatments. Even if CSA itself is not immediately feasible, the technologies and methodologies developed through CSA research could be applied in less extreme surgeries, such as organ transplants, spinal cord injuries, and neurodegenerative diseases like ALS [20]. The benefit of this research lies in its potential to push the boundaries of medical science, exploring the frontiers of neurology, surgery, and organ transplantation. The multidisciplinary approach, combining techniques in immunology, neurology, and bioengineering, has generated new methods that could have applications beyond CSA [19].
For patients with spinal cord injuries, in addition to CSA, a technology that can help patients achieve a cure for spinal cord paralysis, Brain-Computer Interface (BCI), a technology that bypasses the damaged nerves to achieve functional substitution. BCI is a relatively simple technological pathway that has already been applied, and can help fully or partially paralysed patients to control prosthetic limbs, wheelchairs, or other assistive devices to achieve a It can help patients with total or partial paralysis to control prosthetic limbs, wheelchairs or other assistive devices and achieve a degree of independence. Curing spinal paralysis, on the other hand, requires biological regeneration of nerves and functional recovery, which involves a higher degree of scientific complexity and technical difficulty. Therefore, the successful implementation of a Brain-Cell Interface (BCI) far predates a true cure for spinal paralysis. BCI is a direct interaction between the human brain and external devices by capturing and analysing neural signals from the brain and transforming them into executable instructions for external devices. Its core technology lies in analysing neural signals. However, BCI technology still faces challenges such as signal noise, real-time, accuracy and user suitability, and further optimisation of signal analysis algorithms and hardware devices is needed to achieve a wider range of practical applications.
This study makes a substantial contribution to the domains of bioethics, regenerative medicine, and neurosurgery. It necessitates a reevaluation of what is feasible in the fields of human biology and medical ethics and creates new opportunities for curing diseases that were previously incurable [9]. The study's investigation of CSA compels ethicists and medical practitioners to consider difficult questions pertaining to identity, bodily autonomy, and the ethical bounds of medical intervention.
Numerous new gaps in the literature have been identified by the research, especially in relation to the psychological and social effects of undertaking such a radical medical operation. The long-term consequences of spinal cord fusion and the possibility of post-operative rejection or malfunction also require more research. Further studies are also needed to examine the relationship between the brain, neurological system, and immunological response after CSA and to provide uniform guidelines for brain preservation.
4. Conclusion
The main focus of this EPQ is to find out if CSA is possible. After researching I personally feel that is not possible. The journey of CSA has gone through a complicated history of scientific experimentation, technological advancement, and ethical debate. While in the early trials in animals, specifically the ones done by pioneers like Dr. Alex Carrel, Dr. Vladmir Demikhov, and Dr. Robert White, they have provided valuable insights into the feasibility of connecting a head to a donor body, the technical and biological challenges remain significant. Despite the promising developments in spinal cord fusion through the GEMINI protocol and neural regeneration techniques by Sergio Canavero, achieving a fully functional, long-term transplant in humans remains improbable. Immunological rejection, and long-term neurological functionality still need to be addressed. These challenges highlighted the need for more investigation into brain preservation, tailored immunosuppressive treatments, and neuronal regeneration.
Beyond the technical requirements of surgery, there are additional levels of difficulty added by the ethical and psychological ramifications of CSA, which range from issues of personal identity to the possibility of severe psychological distress in recipients. These worries present significant obstacles for CSA's future, as does society's approval of such drastic measures. Because they will influence public opinion and legal frameworks, the ethical, psychological, and sociological ramifications of CSA—particularly those pertaining to identification, consent, and the sanctity of life—must also be thoroughly examined. CSA may be investigated as an experimental procedure in nations with more lax medical ethics, but its development may be constrained by ethical and legal constraints in areas with more stringent laws.
Even though CSA may be a long way from being used in real-world settings, the discoveries and technologies made possible by this research, especially in the fields of regenerative medicine, neurodegenerative disease treatments, and spinal cord injury treatment, have the potential to revolutionize medical care in these fields. In the end, even if CSA may not be practical in the near future, the knowledge gathered from its investigation may result in advances in more practical and moral therapies for a range of neurological disorders.
References
[1]. Borg, J., et al. (2018). "Advancements in Spinal Cord Repair and Regeneration Techniques."Journal of Neurosurgery, 132(5), 1120-1130.
[2]. Canavero, S. (2015). "The 'Gemini’ Spinal Cord Fusion Protocol: Reloaded."Journal of Neurosurgery, 122(4), 1-7.
[3]. Canavero, S. (2016). "Head Transplantation: A Review of the Procedure and Future Perspectives."Journal of Surgical Research, 205(1), 1-15.
[4]. Canavero, S., & Ren, X. (2016). "The GEMINI Protocol: A Revolutionary Approach to Spinal Cord Fusion."Transplantation Proceedings, 48(4), 1185-1190.
[5]. Carrel, A. (1908). "The Technique of Blood Vessel Surgery."Surgical Science, 6(3), 101-105.
[6]. Wang, Y., et al. (2018). "The Use of Stem Cells in Neural Regeneration: A Review of Current Opinion."Current stem cell research & therapy, 13(7), 608–617.
[7]. Yang, B. , et al. (2020). "Strategies and prospects of effective neural circuits reconstruction after spinal cord injury. "Cell death & disease, 11(6), 439.
[8]. Dawson, M. (2017). "The Ethics of Head Transplantation: A Contemporary Debate."Journal of Bioethics, 14(2), 245-256.
[9]. Demikhov, V. (1959). "Experimental Head Transplants in Dogs: A Preliminary Study."Journal of Surgical Research, 34(2), 100-104.
[10]. Digital Paper (2017). "Dr. Xiaoping Ren and Dr. Sergio Canavero’s Head Transplantation Experiments."Science and Technology Daily. Available at: https: //digitalpaper.stdaily.com/http_www.kjrb.com/kjrb/html/2017-11/22/content_382405.htm?div=-1.
[11]. Digital Paper (2017). "The Future of Head Transplantation: Controversy and Social Acceptance."Science and Technology Daily. Available at: https: //digitalpaper.stdaily.com/http_www.kjrb.com/kjrb/html/2017-11/20/content_382294.htm?div=-1.
[12]. Goswami, A. (2021). "The Future of Head Transplantation: Technological, Ethical, and Social Implications."Medical Science and Technology Review, 14(3), 65-80.
[13]. Nobel Prize (1912). "The Nobel Prize in Physiology or Medicine 1912."Nobel Prize. Available at: https: //www.nobelprize.org/prizes/medicine/1912/ceremony-speech/.
[14]. Nobel Prize (1912). Alexis Carrel - Nobel Lecture.Nobel Prize. Available at: https: //www.nobelprize.org/prizes/medicine/1912/carrel/lecture/.
[15]. PMC Article (2009). "Soviet Scientist Vladimir Demikhov’s Contributions to Heart Transplantation and Head Transplantation."National Institutes of Health, PMC. Available at: https: //pmc.ncbi.nlm.nih.gov/articles/PMC2763473/.
[16]. PMC Article (2016). "Head Transplantation in Animals: A Historical Review and Future Directions."National Institutes of Health, PMC. Available at: https: //pmc.ncbi.nlm.nih.gov/articles/PMC5116034/#CR26.
[17]. PMC Article (2017). "The First Human Head Transplant Model and Advancements in Surgical Procedures."National Institutes of Health, PMC. Available at: https: //pmc.ncbi.nlm.nih.gov/articles/PMC5705925/.
[18]. PMC Article (2017). "Psychological and Identity Challenges for Head Transplant Recipients."National Institutes of Health, PMC. Available at: https: //pmc.ncbi.nlm.nih.gov/articles/PMC6174037/#B8.
[19]. PMC Article (2019). "The Path to Head Transplantation in Rodents: Experiments by Dr. Xiao-Ping Ren."National Institutes of Health, PMC. Available at: https: //pmc.ncbi.nlm.nih.gov/articles/PMC6495971/.
[20]. PubMed (1965). "Robert J. White’s Experiments in Brain Transplantation on Dogs."National Institutes of Health, PubMed. Available at: https: //pubmed.ncbi.nlm.nih.gov/5844085/.
[21]. Ren, X. (2015). Personal communication with Dr. Ren's team (referenced inCanavero, 2015).
[22]. Taylor & Francis Online (2017). "Ethical and Social Challenges in Head Transplantation Surgery."Taylor & Francis Online. Available at: https: //www.tandfonline.com/doi/full/10.1080/21507740.2017.1392386#d1e190.
[23]. White, R. J., Wolin, L. R., Massopust, L. C., Taslitz, N., & Verdura, J. (1970). "Cephalic Exchange Transplantation in the Monkey."Surgery, 70(1), 135–139. PMC5116034.
[24]. Xinhua Net (2017). "Head Transplant Experiments in China: Ethical Concerns and Family Consent."Xinhua News. Available at: http: //www.xinhuanet.com//politics/2017-11/23/c_129747301.htm.
Cite this article
Zheng,B. (2025). The development and future usage of head transplantation and related innovations. Journal of Clinical Technology and Theory,3(3),19-28.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Journal:Journal of Clinical Technology and Theory
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Borg, J., et al. (2018). "Advancements in Spinal Cord Repair and Regeneration Techniques."Journal of Neurosurgery, 132(5), 1120-1130.
[2]. Canavero, S. (2015). "The 'Gemini’ Spinal Cord Fusion Protocol: Reloaded."Journal of Neurosurgery, 122(4), 1-7.
[3]. Canavero, S. (2016). "Head Transplantation: A Review of the Procedure and Future Perspectives."Journal of Surgical Research, 205(1), 1-15.
[4]. Canavero, S., & Ren, X. (2016). "The GEMINI Protocol: A Revolutionary Approach to Spinal Cord Fusion."Transplantation Proceedings, 48(4), 1185-1190.
[5]. Carrel, A. (1908). "The Technique of Blood Vessel Surgery."Surgical Science, 6(3), 101-105.
[6]. Wang, Y., et al. (2018). "The Use of Stem Cells in Neural Regeneration: A Review of Current Opinion."Current stem cell research & therapy, 13(7), 608–617.
[7]. Yang, B. , et al. (2020). "Strategies and prospects of effective neural circuits reconstruction after spinal cord injury. "Cell death & disease, 11(6), 439.
[8]. Dawson, M. (2017). "The Ethics of Head Transplantation: A Contemporary Debate."Journal of Bioethics, 14(2), 245-256.
[9]. Demikhov, V. (1959). "Experimental Head Transplants in Dogs: A Preliminary Study."Journal of Surgical Research, 34(2), 100-104.
[10]. Digital Paper (2017). "Dr. Xiaoping Ren and Dr. Sergio Canavero’s Head Transplantation Experiments."Science and Technology Daily. Available at: https: //digitalpaper.stdaily.com/http_www.kjrb.com/kjrb/html/2017-11/22/content_382405.htm?div=-1.
[11]. Digital Paper (2017). "The Future of Head Transplantation: Controversy and Social Acceptance."Science and Technology Daily. Available at: https: //digitalpaper.stdaily.com/http_www.kjrb.com/kjrb/html/2017-11/20/content_382294.htm?div=-1.
[12]. Goswami, A. (2021). "The Future of Head Transplantation: Technological, Ethical, and Social Implications."Medical Science and Technology Review, 14(3), 65-80.
[13]. Nobel Prize (1912). "The Nobel Prize in Physiology or Medicine 1912."Nobel Prize. Available at: https: //www.nobelprize.org/prizes/medicine/1912/ceremony-speech/.
[14]. Nobel Prize (1912). Alexis Carrel - Nobel Lecture.Nobel Prize. Available at: https: //www.nobelprize.org/prizes/medicine/1912/carrel/lecture/.
[15]. PMC Article (2009). "Soviet Scientist Vladimir Demikhov’s Contributions to Heart Transplantation and Head Transplantation."National Institutes of Health, PMC. Available at: https: //pmc.ncbi.nlm.nih.gov/articles/PMC2763473/.
[16]. PMC Article (2016). "Head Transplantation in Animals: A Historical Review and Future Directions."National Institutes of Health, PMC. Available at: https: //pmc.ncbi.nlm.nih.gov/articles/PMC5116034/#CR26.
[17]. PMC Article (2017). "The First Human Head Transplant Model and Advancements in Surgical Procedures."National Institutes of Health, PMC. Available at: https: //pmc.ncbi.nlm.nih.gov/articles/PMC5705925/.
[18]. PMC Article (2017). "Psychological and Identity Challenges for Head Transplant Recipients."National Institutes of Health, PMC. Available at: https: //pmc.ncbi.nlm.nih.gov/articles/PMC6174037/#B8.
[19]. PMC Article (2019). "The Path to Head Transplantation in Rodents: Experiments by Dr. Xiao-Ping Ren."National Institutes of Health, PMC. Available at: https: //pmc.ncbi.nlm.nih.gov/articles/PMC6495971/.
[20]. PubMed (1965). "Robert J. White’s Experiments in Brain Transplantation on Dogs."National Institutes of Health, PubMed. Available at: https: //pubmed.ncbi.nlm.nih.gov/5844085/.
[21]. Ren, X. (2015). Personal communication with Dr. Ren's team (referenced inCanavero, 2015).
[22]. Taylor & Francis Online (2017). "Ethical and Social Challenges in Head Transplantation Surgery."Taylor & Francis Online. Available at: https: //www.tandfonline.com/doi/full/10.1080/21507740.2017.1392386#d1e190.
[23]. White, R. J., Wolin, L. R., Massopust, L. C., Taslitz, N., & Verdura, J. (1970). "Cephalic Exchange Transplantation in the Monkey."Surgery, 70(1), 135–139. PMC5116034.
[24]. Xinhua Net (2017). "Head Transplant Experiments in China: Ethical Concerns and Family Consent."Xinhua News. Available at: http: //www.xinhuanet.com//politics/2017-11/23/c_129747301.htm.









