1. Introduction
Kakuma Refugee Camp is located in the north-western region of Kenya, specifically within Turkana County, close to the borders with Sudan, Ethiopia, and Uganda. The camp was established in 1992 as a children’s encampment to accommodate a group of 20,000 boys of the Nuer and Dinka ethnic groups fleeing from South Sudan due to the Second Sudanese Civil War; they are collectively known as the “Lost Boys of Sudan” [1]. The Kakuma refugee camp is divided into four settlement sectors and covers an area of approximately 15 square kilometres. It is currently the second-largest refugee camp in Kenya. Until March 31, 2023, a total of 201,579 refugees were residing in the Kakuma refugee camp from more than ten countries and all ages, with 73.5% of refugees from South Sudan and 19.5% from Somalia [2]. Due to environmental and man-made factors, the water insecurity issue has dramatically impacted the health of refugees. In order to uphold the human rights of refugees, including the right to have sufficient, safe, and acceptable water for personal and domestic use, this study summarizes the three leading causes of water insecurity and its health impacts through a literature review and incorporates countermeasures from other refugee camps and districts to control and mitigate the effects of water insecurity in Kakuma camp.
2. Reasons for water insecurity
2.1. Sharply increased number of refugees
Initially, the Kakuma refugee camp was designed only to accept 70,000 refugees. However, in 2013, due to conflicts erupting again in South Sudan, the massive influx of refugees into the Kakuma refugee camp resulted in the camp housing 183,000 refugees in 2015, which is more than twice the capacity of the camp [3]. Currently, the number of refugees in the refugee camp is still increasing steadily, which puts pressure on the water supply since the facilities are built for only seventy thousand refugees [4].
2.2. Water scarcity
Kakuma refugee camp is facing water supply shortages due to water scarcity in Turkana County since it is an arid area. The demand for water prompts humanitarian agencies such as the Lutheran World Federation to organise the digging of wells to try to meet the needs of the refugees [5], but the possibility of digging dry holes and brackish groundwater is common [6]. In addition, the local community and the refugee population continue to gather unpurified river water from the Tarach River for household purposes. The main reason for the refugees to continue using the river water is that the well water supported by humanitarian agencies is not enough for usage [7], and given that the past monthly temperatures in Turkana County range from 20 to 40°C historically [8], which is a year-round warmer climate, leading to higher water consumption by refugees.
2.3. Wells with excessive fluoride concentrations
Currently, the primary water source for refugees in the Kakuma refugee camp is still well water. However, research reveals that in July 2016, a survey of 15 pumping wells within the Kakuma refugee camp displayed fluoride concentrations ranging from 1.5 mg/l to 8.4 mg/l [6]. According to the World Health Organization’s (WHO) guideline for the quality of drinking water, the suggested fluoride concentration should not surpass 1.5 mg/L [9]. This indicates that all the pumping wells tested had excessive fluoride concentrations in water. Fluoride is an element naturally found in all water sources of natural origin and is linked to geological environments that contain volcanic rocks. Kakuma refugee camp is situated within the East African Rift Valley, an area geologically comprises volcanic rock aquifers, which inherently possess excessive levels of fluoride in the groundwater [10]. Due to a shortage of water resources, refugees continue to use water from these wells today.
3. Results of water insecurity
3.1. Cholera
According to the WHO, cholera is an acute diarrheal illness caused by the bacteria Vibrio cholerae through consuming food or water that has been contaminated by the bacteria [11]. Kenya has had many widespread outbreaks of cholera throughout its history and continues to have cholera cases every year [12,13]. Due to water scarcity and the sharp increase in the number of refugees, many refugees use unpurified river water for cooking or drinking, reducing the frequency of bathing. This has made cholera likely to occur in the Kakuma refugee camp, especially in the context of the continued cholera outbreak in Kenya.
In 2009, an outbreak of cholera in the Kakuma refugee camp resulted in 224 cases and four deaths of refugees [14]. This outbreak of cholera was caused by the moving in of 12000 new refugees from the Dabaab refugee camp in August 2009 due to overcrowding, where water consumption is increasing rapidly, but the water supply is facing a shortage. The water supply shortage not only causes refugees to consume polluted water but also obstructs the implementation of response measures focusing on improving hygiene and sanitation, thus contributing to the rapid spread of cholera in the Kakuma refugee camp.
3.2. Skeletal fluorosis
Skeletal fluorosis is a chronic metabolic bone and joint disease induced by the consumption of high doses of fluoride, primarily through water ingestion. Fluoride is a cumulative toxin that alters bone tissue accretion and resorption. The primary factor influencing the progression of the medical condition, characterised by the immobilisation of axial skeleton joints and the main joints of the extremities, is the overall quantity of fluoride ingested [15]. A notable correlation exists between the fluoride concentrations in water and the occurrence of skeletal fluorosis in regions where the condition is prevalent. A study conducted in Poldasht County, Iran, suggested that skeletal fluorosis is 18.1% higher in people living in a high-fluoride village (10.15mg/l) than in a low-fluoride village (0.68mg/l) [16].
In the Kakuma refugee camp, a case study mentioned that a Somali man who settled in Canada from the Kakuma refugee camp was found to be suffering from severe skeletal fluorosis with 6.73 g/kg fluoride in his body, where the normal range is 0.5-1.2 g/kg. This person lived in the area supplied with well water from well No. 5 between 2009 and 2015. This well was measured to contain 8.4 mg/L of fluoride in July 2016, which significantly exceeded the guideline [10]. This study suggests that skeletal fluorosis in the Kakuma refugee camp may be highly underestimated due to the challenging clinical diagnosis of fluorosis and the fact that the refugees depend on naturally occurring well water with excessive fluoride concentrations for their livelihoods.
4. Countermeasures
4.1. Oral cholera vaccine
Since cholera is directly caused by water scarcity, which is difficult to improve in the short term, providing two doses of oral cholera vaccine (OCV) will be the most efficient way of controlling cholera. The utilisation of OCV has been witnessed in more than a hundred vaccination initiatives, during which nearly 73 million doses of the vaccine were dispatched to 23 countries to address urgent situations [17,18]. Currently, three types of OCV are WHO pre-qualified, among which ShanChol and Euvichol are killed whole-cell bivalent (O1 and O139) vaccines and are used for mass vaccination as they do not require a buffer [11,19–21]. These two types of OCV are given to all people over one year and should be given at least two weeks apart. The data between 2013 and 2018 shows that complete vaccination with the OCV protects for at least three years with an effectiveness of 76%, and one dose provides short-term protection with a pooled effectiveness of 69% in one year [18].
OCV has been tested worldwide in the past ten years with remarkable results, bringing effective control of cholera outbreaks in various regions. It is tested to be safe with only minor adverse events following immunisation [18,19,21,22]. OCV has also been tested in the refugee camp setting in 1997 and 2013, with 2013 taking place at the Maela refugee camp in Thailand, where a total of 43,485 refugees were infected with ShanChol OCV [23,24]. Among these refugees, 81% of refugees obtained a minimum of one vaccine dose, with 64% having received two doses [24]. The results demonstrate that conducting widespread vaccination within the refugee camps using the OCV is readily attainable and has proven successful in managing cholera within the camp.
4.2. Reverse Osmosis
In rural areas commonly affected by skeletal fluorosis, existing treatment programmes are either inaccessible or unaffordable. Therefore, prevention is one of the safest and most effective ways to combat skeletal fluorosis. To reduce the fluoride in well water, reverse osmosis (RO) could be applied to purify water. RO is a water purification technique employed to eliminate a vast majority of impurities from water. This is achieved by utilising pressure to push unpurified water through a semi-permeable membrane to effectively separate fluoride and transfer water into purified water that meets the guideline [25].
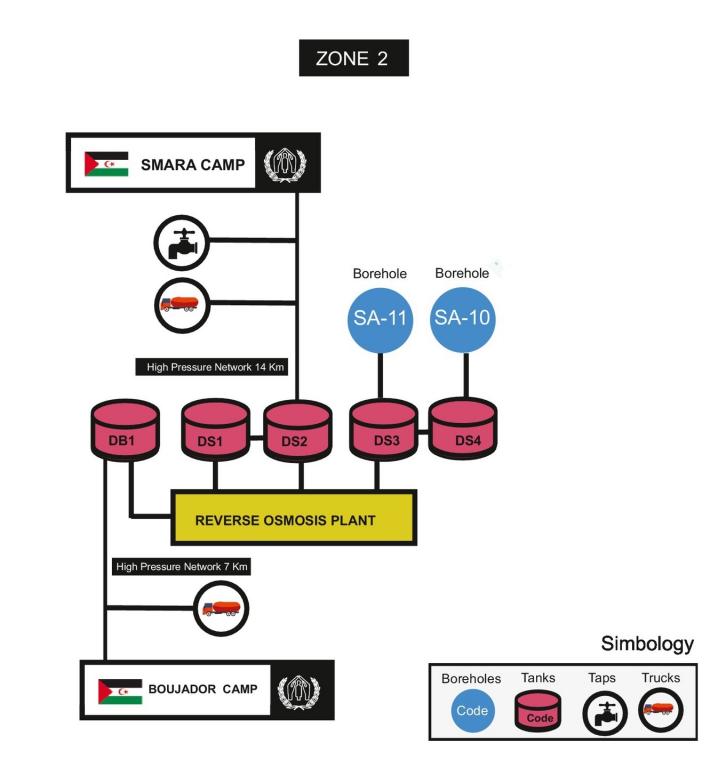
Figure 1. Process of RO in the Sahara refugee camp [26].
RO has been tested in the Sahara refugee camp in Algeria, which has very similar environmental conditions to the Kakuma refugee camp, both of which are arid areas. In order to reduce fluoride in water, two reverse osmosis plants were set up in Zone 2 of the Sahara refugee camp between 2004 and 2007. Figure 1 shows that raw water will be transferred from the borehole to two tanks and then purified in the RO plant. The purified water is stored in three other tanks and transferred to the refugee via pipes or trucks. Raw water from boreholes SA-11 and SA-10 in 2006 reached 1.68mg/l and 1.76mg/l, but after purification through RO, the fluoride decreased to 0.23mg/l, which meets the guideline for drinking water quality [26]. Therefore, RO has been tested to reduce fluoride in well water and can be used effectively in conditions such as refugee camps with large populations.
5. Conclusion
In conclusion, the water insecurity issue caused by a sharp increase in the number of refugees, water scarcity, and excessive fluoride concentration in well water is a multifaceted challenge intricately intertwined with several interrelated factors and poses a significant health risk to the refugees. Diseases known to occur in Kakuma refugee camps as a result of water insecurity include cholera and skeletal fluorosis, an outbreak of which has already occurred several times in the refugee camp and caused the deaths of refugees. Besides, long-term consumption of water with a high fluoride concentration puts refugees at a high probability of developing skeletal fluorosis, and due to clinical diagnosis difficulties, the number of refugees with skeletal fluorosis is greatly underestimated. To control and reduce these diseases, implementing OCV and RO emerges as a viable countermeasure. OCV could provide refugees with three years of protection against cholera, and it can be established within a relatively brief implementation period. RO stands out as an effective method for purifying well water and diminishing fluoride concentrations, thereby lowering the risk of refugees developing skeletal fluorosis. Both countermeasures have been shown to be effective in other refugee camps with similar situations.
However, it’s noteworthy that the cessation of Shanchol OCV production by the end of 2023 raises concerns about future supplies, although there have been reports that Euvichol OCV has increased its production. Further research endeavours could delve into the development of sustainable, long-term countermeasures for solving water insecurity and its associated health impacts within the refugee camp setting.
References
[1]. IRC (2014). The Lost Boys of Sudan. https://www.rescue.org/uk/article/lost-boys-sudan
[2]. UNHCR. (2023). Refugees and Asylum-seekers in Turkana. https://data.unhcr.org/ en/country/ken/796
[3]. UNHCR Kenya. (n.d.). Kalobeyei Settlement – UNHCR Kenya. Retrieved August 28, 2023, from https://www.unhcr.org/ke/kalobeyei-settlement
[4]. REACH Initiative. (2022). Actor and Service Mapping in Kakuma Refugee Camps, July 2022—Kenya. https://reliefweb.int/report/kenya/actor-and-service-mapping-kakuma-refugee-camps-july-2022
[5]. Mahamud, A. S., Ahmed, J. A., Nyoka, R., Auko, E., Kahi, V., Ndirangu, J., Nguhi, M., Burton, J. W., Muhindo, B. Z., Breiman, R. F., & Eidex, R. B. (2012). Epidemic cholera in Kakuma Refugee Camp, Kenya, 2009: The importance of sanitation and soap. The Journal of Infection in Developing Countries, 6(03), Article 03. https://doi.org/10.3855/jidc.1966
[6]. Bauman, P., Ernst, E., & Woods, L. (2017). Surface Geophysical Exploration for Groundwater at the Kakuma Refugee Camp in Turkana County, Kenya.
[7]. Anomat Ali, J., Imana, D. K., & Ocha, W. (2017). The Refugee Crisis in Kenya: Exploring Refugee-Host Community Causes of Tensions and Conflicts in Kakuma Refugee Camp. Journal of International Relations and Foreign Policy, 5(2). https://doi.org/ 10.15640/jirfp.v5n2a4
[8]. CGIAR. (2021, September 22). Kenya County Climate Risk Profile Series: Climate Risk Profile - Turkana County - Kenya | ReliefWeb. https://reliefweb.int/report/kenya/kenya-county-climate-risk-profile-series-climate-risk-profile-turkana-county
[9]. WHO. (2017). Guidelines for drinking-water quality, 4th edition, incorporating the 1st addendum. https://www.who.int/publications-detail-redirect/9789241549950
[10]. Fabreau, G. E., Bauman, P., Coakley, A. L., Johnston, K., Kennel, K. A., Gifford, J. L., Sadrzadeh, H. M., Whitford, G. M., Whyte, M. P., & Kline, G. A. (2019). Skeletal fluorosis in a resettled refugee from Kakuma refugee camp. The Lancet, 393(10168), 223–225. https://doi.org/10.1016/S0140-6736(18)32842-3
[11]. WHO. (2022). Cholera. https://www.who.int/news-room/fact-sheets/detail/cholera
[12]. Cowman, G., Otipo, S., Njeru, I., Achia, T., Thirumurthy, H., Bartram, J., & Kioko, J. (2017). Factors associated with cholera in Kenya, 2008-2013. Pan African Medical Journal, 28(1), Article 1. https://doi.org/10.4314/pamj.v28i1
[13]. WHO. (2023). Cholera in the WHO African Region. https://apps.who.int/iris/ bitstream/handle/10665/366482/AFRO%20Cholera%20Bulletin.03_Final.pdf
[14]. Weinberg, M., Ochieng, J. B., Breiman, R. F., Omollo, J. O., Feikin, D. R., Shultz, A., Qassim, M., & Burke, H. (2009). Cholera Outbreak in Kenyan Refugee Camp: Risk Factors for Illness and Importance of Sanitation. The American Journal of Tropical Medicine and Hygiene, 80(4), 640–645. https://doi.org/10.4269/ajtmh.2009.80.640
[15]. Krishnamachari, K. A. (1986). Skeletal fluorosis in humans: A review of recent progress in the understanding of the disease. Progress in Food & Nutrition Science, 10(3–4), 279–314.
[16]. Mohammadi, A. A., Yousefi, M., Yaseri, M., Jalilzadeh, M., & Mahvi, A. H. (2017). Skeletal fluorosis in relation to drinking water in rural areas of West Azerbaijan, Iran. Scientific Reports, 7(1), Article 1. https://doi.org/10.1038/s41598-017-17328-8
[17]. WHO. (n.d.). Cholera vaccine stockpiles. Retrieved August 28, 2023, from https://www.who.int/groups/icg/cholera/stockpiles
[18]. Pezzoli, L. (2020). Global oral cholera vaccine use, 2013–2018. Vaccine, 38, A132–A140. https://doi.org/10.1016/j.vaccine.2019.08.086
[19]. Calain, P., Chaine, J.-P., Johnson, E., Hawley, M.-L., O’Leary, M. J., Oshitani, H., & Chaignat, C.-L. (2004). Can oral cholera vaccination play a role in controlling a cholera outbreak? Vaccine, 22(19), 2444–2451. https://doi.org/10.1016/j.vaccine.2003.11.070
[20]. CDC. (2023, August 7). Cholera—Vibrio cholerae infection. https://www.cdc.gov/ cholera/vaccines.html
[21]. Song, K. R., Lim, J. K., Park, S. E., Saluja, T., Cho, S.-I., Wartel, T. A., & Lynch, J. (2021). Oral Cholera Vaccine Efficacy and Effectiveness. Vaccines, 9(12), Article 12. https://doi.org/10.3390/vaccines9121482
[22]. Lucas, M. E. S., Deen, J. L., von Seidlein, L., Wang, X.-Y., Ampuero, J., Puri, M., Ali, M., Ansaruzzaman, M., Amos, J., Macuamule, A., Cavailler, P., Guerin, P. J., Mahoudeau, C., Kahozi-Sangwa, P., Chaignat, C.-L., Barreto, A., Songane, F. F., & Clemens, J. D. (2005). Effectiveness of Mass Oral Cholera Vaccination in Beira, Mozambique. New England Journal of Medicine, 352(8), 757–767. https://doi.org/10.1056/NEJMoa043323
[23]. Legros, D., Paquet, C., Perea, W., Marty, I., Mugisha, N. K., Royer, H., Neira, M., & Ivanoff, B. (1999). Mass vaccination with a two-dose oral cholera vaccine in a refugee camp. Bulletin of the World Health Organization, 77(10), 837–842.
[24]. Phares, C. R., Date, K., Travers, P., Déglise, C., Wongjindanon, N., Ortega, L., & Bhuket, P. R. N. (2016). Mass vaccination with a two-dose oral cholera vaccine in a long-standing refugee camp, Thailand. Vaccine, 34(1), 128–133. https://doi.org/10.1016/j.vaccine.2015.10.112
[25]. Mavukkandy, M. O., Chabib, C. M., Mustafa, I., Al Ghaferi, A., & AlMarzooqi, F. (2019). Brine management in desalination industry: From waste to resources generation. Desalination, 472, 114187. https://doi.org/10.1016/j.desal.2019.114187
[26]. García, R., Naves, A., Anta, J., Ron, M., & Molinero, J. (2021). Drinking water provision and quality at the Sahrawi refugee camps in Tindouf (Algeria) from 2006 to 2016. Science of The Total Environment, 780, 146504. https://doi.org/10.1016/j.scitotenv.2021.146504
Cite this article
Xu,Q. (2023). Research on the causes, impacts and measures of water safety - Taking Kakuma refugee camp as an example. Theoretical and Natural Science,8,140-145.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 2nd International Conference on Modern Medicine and Global Health
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. IRC (2014). The Lost Boys of Sudan. https://www.rescue.org/uk/article/lost-boys-sudan
[2]. UNHCR. (2023). Refugees and Asylum-seekers in Turkana. https://data.unhcr.org/ en/country/ken/796
[3]. UNHCR Kenya. (n.d.). Kalobeyei Settlement – UNHCR Kenya. Retrieved August 28, 2023, from https://www.unhcr.org/ke/kalobeyei-settlement
[4]. REACH Initiative. (2022). Actor and Service Mapping in Kakuma Refugee Camps, July 2022—Kenya. https://reliefweb.int/report/kenya/actor-and-service-mapping-kakuma-refugee-camps-july-2022
[5]. Mahamud, A. S., Ahmed, J. A., Nyoka, R., Auko, E., Kahi, V., Ndirangu, J., Nguhi, M., Burton, J. W., Muhindo, B. Z., Breiman, R. F., & Eidex, R. B. (2012). Epidemic cholera in Kakuma Refugee Camp, Kenya, 2009: The importance of sanitation and soap. The Journal of Infection in Developing Countries, 6(03), Article 03. https://doi.org/10.3855/jidc.1966
[6]. Bauman, P., Ernst, E., & Woods, L. (2017). Surface Geophysical Exploration for Groundwater at the Kakuma Refugee Camp in Turkana County, Kenya.
[7]. Anomat Ali, J., Imana, D. K., & Ocha, W. (2017). The Refugee Crisis in Kenya: Exploring Refugee-Host Community Causes of Tensions and Conflicts in Kakuma Refugee Camp. Journal of International Relations and Foreign Policy, 5(2). https://doi.org/ 10.15640/jirfp.v5n2a4
[8]. CGIAR. (2021, September 22). Kenya County Climate Risk Profile Series: Climate Risk Profile - Turkana County - Kenya | ReliefWeb. https://reliefweb.int/report/kenya/kenya-county-climate-risk-profile-series-climate-risk-profile-turkana-county
[9]. WHO. (2017). Guidelines for drinking-water quality, 4th edition, incorporating the 1st addendum. https://www.who.int/publications-detail-redirect/9789241549950
[10]. Fabreau, G. E., Bauman, P., Coakley, A. L., Johnston, K., Kennel, K. A., Gifford, J. L., Sadrzadeh, H. M., Whitford, G. M., Whyte, M. P., & Kline, G. A. (2019). Skeletal fluorosis in a resettled refugee from Kakuma refugee camp. The Lancet, 393(10168), 223–225. https://doi.org/10.1016/S0140-6736(18)32842-3
[11]. WHO. (2022). Cholera. https://www.who.int/news-room/fact-sheets/detail/cholera
[12]. Cowman, G., Otipo, S., Njeru, I., Achia, T., Thirumurthy, H., Bartram, J., & Kioko, J. (2017). Factors associated with cholera in Kenya, 2008-2013. Pan African Medical Journal, 28(1), Article 1. https://doi.org/10.4314/pamj.v28i1
[13]. WHO. (2023). Cholera in the WHO African Region. https://apps.who.int/iris/ bitstream/handle/10665/366482/AFRO%20Cholera%20Bulletin.03_Final.pdf
[14]. Weinberg, M., Ochieng, J. B., Breiman, R. F., Omollo, J. O., Feikin, D. R., Shultz, A., Qassim, M., & Burke, H. (2009). Cholera Outbreak in Kenyan Refugee Camp: Risk Factors for Illness and Importance of Sanitation. The American Journal of Tropical Medicine and Hygiene, 80(4), 640–645. https://doi.org/10.4269/ajtmh.2009.80.640
[15]. Krishnamachari, K. A. (1986). Skeletal fluorosis in humans: A review of recent progress in the understanding of the disease. Progress in Food & Nutrition Science, 10(3–4), 279–314.
[16]. Mohammadi, A. A., Yousefi, M., Yaseri, M., Jalilzadeh, M., & Mahvi, A. H. (2017). Skeletal fluorosis in relation to drinking water in rural areas of West Azerbaijan, Iran. Scientific Reports, 7(1), Article 1. https://doi.org/10.1038/s41598-017-17328-8
[17]. WHO. (n.d.). Cholera vaccine stockpiles. Retrieved August 28, 2023, from https://www.who.int/groups/icg/cholera/stockpiles
[18]. Pezzoli, L. (2020). Global oral cholera vaccine use, 2013–2018. Vaccine, 38, A132–A140. https://doi.org/10.1016/j.vaccine.2019.08.086
[19]. Calain, P., Chaine, J.-P., Johnson, E., Hawley, M.-L., O’Leary, M. J., Oshitani, H., & Chaignat, C.-L. (2004). Can oral cholera vaccination play a role in controlling a cholera outbreak? Vaccine, 22(19), 2444–2451. https://doi.org/10.1016/j.vaccine.2003.11.070
[20]. CDC. (2023, August 7). Cholera—Vibrio cholerae infection. https://www.cdc.gov/ cholera/vaccines.html
[21]. Song, K. R., Lim, J. K., Park, S. E., Saluja, T., Cho, S.-I., Wartel, T. A., & Lynch, J. (2021). Oral Cholera Vaccine Efficacy and Effectiveness. Vaccines, 9(12), Article 12. https://doi.org/10.3390/vaccines9121482
[22]. Lucas, M. E. S., Deen, J. L., von Seidlein, L., Wang, X.-Y., Ampuero, J., Puri, M., Ali, M., Ansaruzzaman, M., Amos, J., Macuamule, A., Cavailler, P., Guerin, P. J., Mahoudeau, C., Kahozi-Sangwa, P., Chaignat, C.-L., Barreto, A., Songane, F. F., & Clemens, J. D. (2005). Effectiveness of Mass Oral Cholera Vaccination in Beira, Mozambique. New England Journal of Medicine, 352(8), 757–767. https://doi.org/10.1056/NEJMoa043323
[23]. Legros, D., Paquet, C., Perea, W., Marty, I., Mugisha, N. K., Royer, H., Neira, M., & Ivanoff, B. (1999). Mass vaccination with a two-dose oral cholera vaccine in a refugee camp. Bulletin of the World Health Organization, 77(10), 837–842.
[24]. Phares, C. R., Date, K., Travers, P., Déglise, C., Wongjindanon, N., Ortega, L., & Bhuket, P. R. N. (2016). Mass vaccination with a two-dose oral cholera vaccine in a long-standing refugee camp, Thailand. Vaccine, 34(1), 128–133. https://doi.org/10.1016/j.vaccine.2015.10.112
[25]. Mavukkandy, M. O., Chabib, C. M., Mustafa, I., Al Ghaferi, A., & AlMarzooqi, F. (2019). Brine management in desalination industry: From waste to resources generation. Desalination, 472, 114187. https://doi.org/10.1016/j.desal.2019.114187
[26]. García, R., Naves, A., Anta, J., Ron, M., & Molinero, J. (2021). Drinking water provision and quality at the Sahrawi refugee camps in Tindouf (Algeria) from 2006 to 2016. Science of The Total Environment, 780, 146504. https://doi.org/10.1016/j.scitotenv.2021.146504