1. Introduction
A sequence of depressive symptoms known as major depressive disorder (MDD) are primarily brought on by genetic anomalies or abrupt changes in the patient’s environment. MDD in the mother is strongly associated with a wide range of deleterious effects in the kids, including a higher chance of MDD in adolescence, according to earlier research. Researchers have proposed that cognitive vulnerabilities, which are prejudices in processing data and the recollection of mental stimuli (via attention, comprehension, and memory), represent declaring putative mechanisms of risk among kids of depressed mothers, despite the fact that the exact systems of intergenerational risk continue to be insufficiently understood. [1,2] Descendants of depressed female parents have larger extent of cognitive vulnerabilities than their peers.
Overgeneral autobiographical memory (OGM) is the mixed memory of individual complex events that closely related to self-experience. The characteristic of hard to recall specific autobiographical commemorations is frequently seen in depression patients, leading a trend of recollecting fewer exact reminiscences when reply to demonstrative cue words. [3] The risk of cognitive fragility in offspring is increased by parental depression, a type of cognitive vulnerability linked to the intergenerational transmission of depression. Only the expected impacts of maternal depression on children’s OGM are covered in the current study, nevertheless, it is ill-informed about the prospective influence of paternal depression on the development of OGM in offspring. According to previous research, OGM development is affected by elements at the cultural, familial, and individual levels. And there is a lot of proof that mother-child relationships can influence how their children develop OGM. What about father-child interactions?[4] In longitudinal research of 277 experimental subject, Rawal & Rice found that prognosticated standard rank of OGM to pessimistic hints rises in depression symptoms and the emergence of depressive disorders. However, the subsequent period was just one year.[5] For children aged 8 to 14 who resided with their parents, we were able to conduct an evaluation. We looked at the OGM trajectory and conducted assessments every six months for two years. The study was categorized by this, and a thorough evaluation of whether the fathers had MDD history should be done at the start. To assess whether paternal depressive symptoms will be a greater influence factor than MDD history, we should compare the findings with the most recent sociological statistics.
Given that childhood depression and OGM biases are linked, we performed investigative experiments to see if descendants’ OGM would be affected by paternal depressed symptoms at each time point and to figure out whether the impress of father depression on child OGM would be at least partially distinct from the former influencing factor. Increasing severity of paternal depression symptoms, according to our hypothesis, would amplify OGM biases toward unfavorable stimuli. This paper solely provides theoretical experiment design and possible results about how paternal MDD history and depressive symptoms affect offspring OGM, which needs further research in the specific social samples.
This paper aims to show the current gaps in the research data about the history of MDD in fathers and the effect on OGM of offspring by designing theoretical experiments, and to predict the results of theoretical experiments based on the current research data and results. Further research on the influence of parents on OGM in offspring will provide better ideas for the prevention of depression in adolescents.
2. Method
There have 5 ways to assess the father’s history of MDD, the father’s symptoms of depression and the offspring’s MDD, offspring’s symptoms of depression. After analyzing the depression history and symptoms of the father and offspring, all the data were summarized into several formulae to gradually analyze the influence of the father’s history of MDD for the offspring OGM.
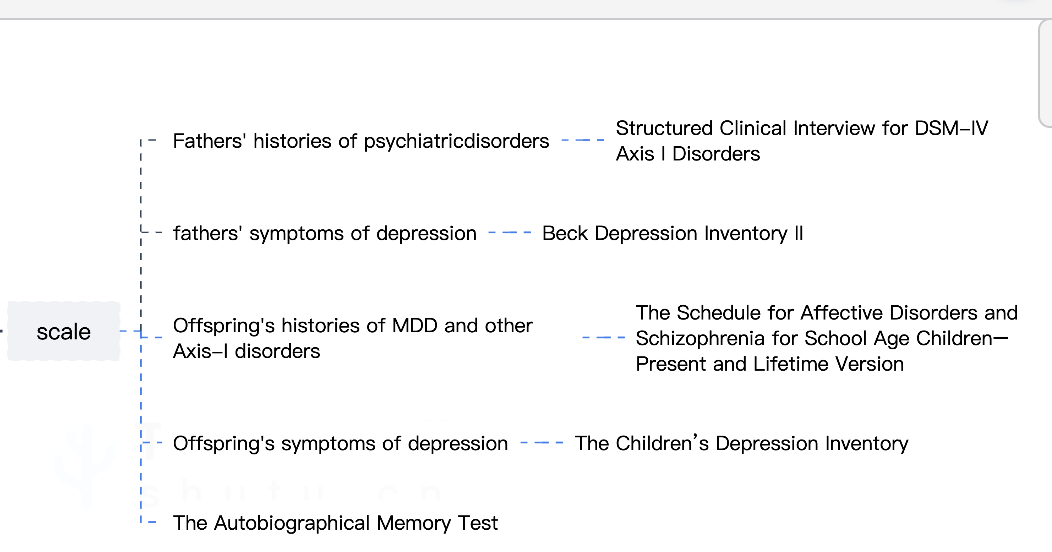
Figure 1. The scale
In the first place, we select the scales shown in fig.1 for our sample (200 fathers with MDD and their offspring aged between 8-14). The Structured Clinical Interview for DSM-IV Axis I Disorders [6] evaluates fathers’ histories of psychiatric disorders. The SCID-I has a displaying type with 24 objects that evaluates the symptoms of several Axis I diseases. Based on the patient’s responses, it directs the interlocutors to “Go To” the particular symptomatic part.[7]
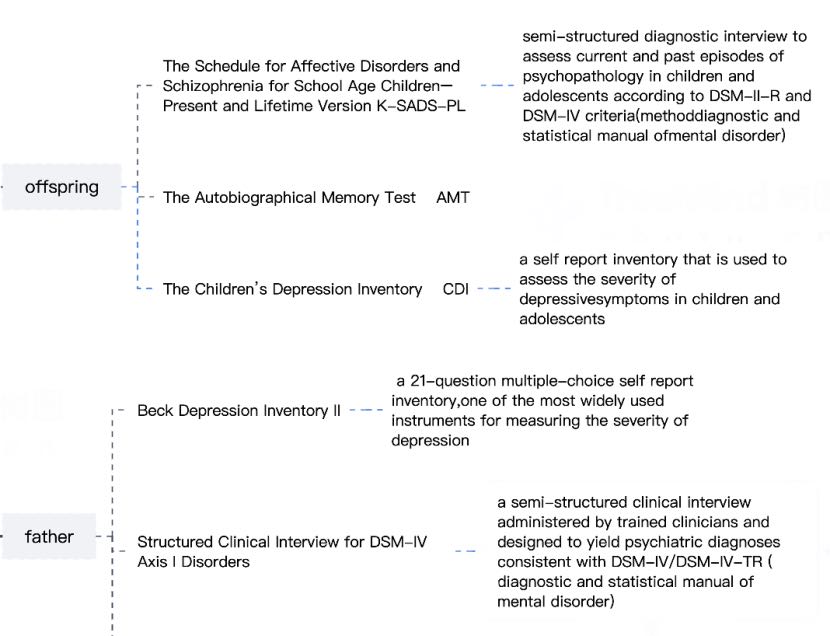
Figure 2. The assess step
2.1. Assess the offspring’s MDD, offspring’s symptoms of depression and offspring’s autobiographical memory
Then we start our assessment with the scales of measuring offspring’s MDD, offspring’s symptoms of depression and their autobiographical memory.
For measuring the severity of depression symptoms in young experimental subject, the Children’s Depression Inventory [8] was adopted.
Involved is the Autobiographical Memory Test [9], which comprising 10 words, half of which are sanguine and the others are pessimistic. Participants have 60 seconds to recollect particular memories according to the words’ emotional connotations. The amount of distinct memories reminisced by each progeny is counted.
The K-SADS-PL [9] is a semi-structured symptomatic interview created to evaluate present and prior instances of psychopathy in kids and teens that comply with DSM-II-R and DSM-IV(diagnostic and mathematical manual of mental disorder), as well as the children’s histories of MDD alongside additional Axis-I disorders. It was developed in 1997.This scale produces accurate and trustworthy psychiatric diagnoses, and it excels at evaluating affective and anxiety disorders.[10]
2.2. Assess the father’s history of MDD, the father’s symptoms of depression
After we obtain the results of offspring’s MDD, offspring’s symptoms of depression and offspring’s autobiographical memory, we assess the father’s history of MDD and the father’s symptoms of depression.
We utilized the 21-question, multiple-choice Beck Depression Inventory II [11], one of the most popular tools for gauging the severity of depression, to measure the father’s depressive symptoms. Three determinants—comprehension, physical symptoms, and impression—were found in the BDI-II component analysis, whereas two determinants—low spirits and uneasiness—were found in the HSCL-10 factor analysis.[12]
The Structured Clinical Interview for DSM-IV Axis I problems [12], a structured clinical conversation carried out by licensed psychiatrists with the goal of generating psychiatric diagnoses congruent with DSM-IV/DSM-IV-TR, is used for estimating the father’s histories of mental problems. (diagnoses and statistical manual of mental disorder).
2.3. The impact of paternal MDD on offspring’s OGM
When all the data are collected, we use the analyzing method called Hierarchical linear modeling [13]to find whether the father’s MDD history is associated with offspring’s memories. The function shows the repercussions of paternal MDD history on formation paths of descendants’ OGM with following 2 years.
The first level of the equation:
\( OGMtij = π0j + π1j (Timeij) + eij \) [14]
The OGMtij represents in this equation the quantity of unique autobiographical memories (positive or negative) produced at time t for evaluation i and participant j by each offspring [14]. The \( π0j \) plays the role of the intercept (OGM score for children) in this equation. \( π1j \) plays the role of slope in this function and it reflects the relation between time period while eij represents the error term.[14]
The second level of the equation:
\( π0j = β00 + β01(MDD) + r0j \) [14]
\( π1j = β10 + β11(MDD) + r1j \) [14]
In those equations,01 is the representation of the cross-level term of interaction showing the impact on the father’s history of MDD, and 11 denotes the cross-level association term demonstrating the repercussion of the father’s history of MDD on the linear variation in the offspring’s OGM over the course of the subsequent two years.
Initially, vaticinatory results at baseline assessment indicates that there is no significant correlation between the offspring OGM for positive clues and the father’s history of major depression, which further shows that father’s history of major depressive disorder does not modulate this trajectory.
Secondarily, vaticinatory results for negative cues suggest that father’s MDD history is expressively relevant to OGM at the standard evaluation and paternal MDD history does not show regulating effect on the slope, meaning that the incipient alteration between OGM and pessimistic prompts is conserved during follow-up.
2.4. The effect of paternal depression symptoms on offspring’s OGM
We also need to evaluate the relationship between paternal depression symptoms and offspring’s OGM, which HLM analyzing method is also involved along with the measuring scales BDI-II and CDI. The level 1 for HLM analyse is:
\( OGMt0ij=γ0j+γ1j(OGMt1ij)+γ2j(BDI-IIt1ij)+ eij \) [14]
For this equation, OGMij stands for the amount of unique autobiographical memories which each offspring was able to recall at temporal point t0 for assessments i and j, γ0j is the intercept of OGMtij, and BDI-IIt1ij represents the rank of depressive symptoms in the male parent at t1 for assessments i and j. Additionally, γ1j represents the gradient of the connection for the quantity of offspring’s OGM during the period from t0 to t1 for participant j, and similarly, γ2j is the inclination that reveals the correlation among paternal depressive symptoms and the magnitude of OGM (i.e., linear correlation), and eij denotes the error term.
Here shows the Level 2 model:
γ 0j = θ00 +θ 01(MDD) + r0j
γ 1j = θ10 + θ11(MDD) + r1j
γ 2j = θ20 + θ21(MDD) + r2j [14]
In the equations above, the cross-level interaction term θ01 shows how a father’s history of MDD affects the OGM intercept at θ00, and the cross-level interaction term θ11 shows how this history affects the gradient of the relationship among the quantity of exact reminiscence each individual (both hysteric and current) generates. Additionally, the cross-level interaction [15] shows how paternal MDD affects the inclination of their depressive symptoms and alterations in descendants’ definite OGM from t1 to t0. lastly, r0j, r1j, and r2j correspond to the error terms, while θ00, θ10 and θ20 are terms of interception for each of their respective equations.
3. Discussion
3.1. Strength and limitation
The present study has covered the OGM deficiency of children of mothers with depressive orders, especially for the negative cue words [14]. OGM biases in adults have also been demonstrated to be reduced by broader cognitive behavioral therapies (CBT), like Mindfulness-Based Cognitive Therapy [16] and CBT for depression [17], which have proven the validity of method.
The large size of sample is the undeniable strength of the experiment [14] Additionally, using HLM gives us multifold benefits over using a regression approach, containing the ability to incorporate [15] the data from all measurement points to calculate gradients for changes and to model individual variations and distinct periods of change with little reliance on the assumption of independent observations. As a result, it is likely to increase the study’s accuracy in determining the relationship between the two variables. On top of that, conceptually, measuring the changes in offspring’s OGM is a gradual process rather than a series of discrete data, and varying path given by HLM is seemed to be more germane as it provides flexibility for the modeling.
The age range of offspring is between 8-14, meaning that they are seem to be affected by the environment (teachers, parents, classmates) and further result in some deviations from what we’ve originally expected. It is recommended for the related studies in the future to use a sample with smaller age group, in order to improve the precision of the results.
3.2. The implication
Paternal MDD history and depressive symptoms may have an impact on their offspring’s OGM, in particular the negative cues. This finding provides some thoughts in the clinical treatment. For instance, in the prevention of future depression in these high-risk youth, we can try to modify the paternal gene [14] to minimize the risk of intergenerational transmission, which requires further extended study and more in-depth research in this field.
4. Conclusion
The underlying intention of the experiment is to appraise the link between paternal MDD history, depression symptoms and offspring’s OGM. We use AMT for children to obtain the data of their specific autobiographical memories for each assessment point with the scale of CDI for the 6 months,12 months followed-up after the initial assessment, and for the fathers they have to complete the BDI-II at the same time point, to ensure the generality of trend and avoid occasional results. In the second place, we used HLM, a method to analyse results to discover the relationships between variables in a more comprehensive way. The expected finding is that descendants of fathers with MDD or depression symptoms are incline to having the vulnerabilities to generate OGM for negative cues, we suppose it is the affected phenotype of memory due to inheritance. However it still needs future research and experiment to proven the hypothesis and find the corresponding gene, then introduce technologies like modifying the relevant gene or developing drugs to control expression of this gene.
Acknowledgement
Baizi Fang, Jiayi Xia and Ruowen Zhu contribute evenly to this work and should be considered co-first authors.
References
[1]. Goodman SH. Depression in mothers. Annu Rev Clin Psychol. 2007;3:107-135. doi:10.1146/annurev.clinpsy.3.022806.091401
[2]. Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal depression and child psychopathology: a meta-analytic review. Clin Child Fam Psychol Rev. 2011;14(1):1-27. doi:10.1007/s10567-010-0080-1
[3]. Champagne K, Burkhouse KL, Woody ML, Feurer C, Sosoo E, Gibb BE. Brief report: Overgeneral autobiographical memory in adolescent major depressive disorder. J Adolesc. 2016;52:72-75. doi:10.1016/j.adolescence.2016.07.008
[4]. Woody ML, Tsypes A, Burkhouse KL, Feurer C, Champagne K, Gibb BE. Development of Overgeneral Autobiographical Memory in Offspring of Depressed Mothers. J Clin Child Adolesc Psychol. 2022;51(1):73-84. doi:10.1080/15374416.2019.1650367
[5]. Rawal A, Rice F. Examining overgeneral autobiographical memory as a risk factor for adolescent depression. J Am Acad Child Adolesc Psychiatry. 2012;51(5):518-527. doi:10.1016/j.jaac.2012.02.025
[6]. First MB, Spitzer RL, Gibbon M, & Williams JB (1994). Structured clinical interview for Axis IDSM-IV disorders. Patient Edition (SCID-I/P).
[7]. Gregory S Chasson , Monnica T Williams , Darlene M Davis , Jessica Y Combs ‘Missed diagnoses in African Americans with obsessive-compulsive disorder: the structured clinical interview for DSM-IV Axis I disorders (SCID-I)’, DOI: 10.1186/s12888-017-1422-z,2017.Jun.17
[8]. Kovacs M (1981). Rating scales to assess depression in school-aged children. Acta Paedopsychiatrica,46, 305–315. [PubMed: 7025571]
[9]. Williams J M G, & Broadbent K (1986). Autobiographical memory in suicide attempters. Journal ofAbnormal Psychology, 95, 144–149. [PubMed: 3711438]
[10]. Joan Kaufman, PH.D., Boris Birmaher, M.D., David Brent, M.D., Uma Rao, M.D., Cynthia Flynn, M.A., Paula Moreci, M.S.W., Douglas Williamson, M.A., and Neal Ryan, M.D. Schedule for Mfective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): Initial Reliability and Validity Data
[11]. Beck A, Steer RA, & Brown GK (1996). Beck Depression Inventory-II. San Antonio, TX, 78204–2498.
[12]. Ingebjørg Aspeland Lien a, Ingeborg Bolstad b c, Lars Lien b c, Jørgen G. Bramness b d eScreening for depression in patients in treatment for alcohol use disorder using the Beck Depression Inventory-II and the Hopkins Symptom Checklist-10
[13]. Raudenbush SW, Bryk AS, Cheong YF, & Congdon RT (2004). HLM 6: Hierarchical linear andnonlinear modeling. Incolnwood, IL: Scientific Software International.
[14]. Mary L. Woody1, Aliona Tsypes2, Katie L. Burkhouse3, Cope Feurer2, Katelynn Champagne4, Brandon E. Gibb2, Development of Overgeneral Autobiographical Memory in Offspring of Depressed Mothers
[15]. Matthew Price, Page Anderson, Christopher C. Henrich, and Barbara Olasov Rothbaum(2013),Greater Expectations: Using Hierarchical Linear Modeling to Examine Expectancy for Treatment Outcome as a Predictor of Treatment Response
[16]. Williams J Mark G, Teasdale JD, Segal ZV, & Soulsby J(2000),Mindfulness-based cognitive therapyreduces overgeneral autobiographical memory in formely depressed patients. Journal of Abnormal Psychology, 109, 150–155. [PubMed: 10740947]
[17]. McBride C, Segal ZV, Kennedy S, & Gemar M(2007) ,Changes in autobiographical memoryspecificity following cognitive behavior therapy and pharmacotherapy for major depression. Psychopathology, 40, 147–152. [PubMed: 17318006]
Cite this article
Fang,B.;Xia,J.;Zhu,R. (2024). How paternal MDD history and depression symptoms affect offspring's OGM. Theoretical and Natural Science,45,33-39.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 2nd International Conference on Modern Medicine and Global Health
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Goodman SH. Depression in mothers. Annu Rev Clin Psychol. 2007;3:107-135. doi:10.1146/annurev.clinpsy.3.022806.091401
[2]. Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal depression and child psychopathology: a meta-analytic review. Clin Child Fam Psychol Rev. 2011;14(1):1-27. doi:10.1007/s10567-010-0080-1
[3]. Champagne K, Burkhouse KL, Woody ML, Feurer C, Sosoo E, Gibb BE. Brief report: Overgeneral autobiographical memory in adolescent major depressive disorder. J Adolesc. 2016;52:72-75. doi:10.1016/j.adolescence.2016.07.008
[4]. Woody ML, Tsypes A, Burkhouse KL, Feurer C, Champagne K, Gibb BE. Development of Overgeneral Autobiographical Memory in Offspring of Depressed Mothers. J Clin Child Adolesc Psychol. 2022;51(1):73-84. doi:10.1080/15374416.2019.1650367
[5]. Rawal A, Rice F. Examining overgeneral autobiographical memory as a risk factor for adolescent depression. J Am Acad Child Adolesc Psychiatry. 2012;51(5):518-527. doi:10.1016/j.jaac.2012.02.025
[6]. First MB, Spitzer RL, Gibbon M, & Williams JB (1994). Structured clinical interview for Axis IDSM-IV disorders. Patient Edition (SCID-I/P).
[7]. Gregory S Chasson , Monnica T Williams , Darlene M Davis , Jessica Y Combs ‘Missed diagnoses in African Americans with obsessive-compulsive disorder: the structured clinical interview for DSM-IV Axis I disorders (SCID-I)’, DOI: 10.1186/s12888-017-1422-z,2017.Jun.17
[8]. Kovacs M (1981). Rating scales to assess depression in school-aged children. Acta Paedopsychiatrica,46, 305–315. [PubMed: 7025571]
[9]. Williams J M G, & Broadbent K (1986). Autobiographical memory in suicide attempters. Journal ofAbnormal Psychology, 95, 144–149. [PubMed: 3711438]
[10]. Joan Kaufman, PH.D., Boris Birmaher, M.D., David Brent, M.D., Uma Rao, M.D., Cynthia Flynn, M.A., Paula Moreci, M.S.W., Douglas Williamson, M.A., and Neal Ryan, M.D. Schedule for Mfective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): Initial Reliability and Validity Data
[11]. Beck A, Steer RA, & Brown GK (1996). Beck Depression Inventory-II. San Antonio, TX, 78204–2498.
[12]. Ingebjørg Aspeland Lien a, Ingeborg Bolstad b c, Lars Lien b c, Jørgen G. Bramness b d eScreening for depression in patients in treatment for alcohol use disorder using the Beck Depression Inventory-II and the Hopkins Symptom Checklist-10
[13]. Raudenbush SW, Bryk AS, Cheong YF, & Congdon RT (2004). HLM 6: Hierarchical linear andnonlinear modeling. Incolnwood, IL: Scientific Software International.
[14]. Mary L. Woody1, Aliona Tsypes2, Katie L. Burkhouse3, Cope Feurer2, Katelynn Champagne4, Brandon E. Gibb2, Development of Overgeneral Autobiographical Memory in Offspring of Depressed Mothers
[15]. Matthew Price, Page Anderson, Christopher C. Henrich, and Barbara Olasov Rothbaum(2013),Greater Expectations: Using Hierarchical Linear Modeling to Examine Expectancy for Treatment Outcome as a Predictor of Treatment Response
[16]. Williams J Mark G, Teasdale JD, Segal ZV, & Soulsby J(2000),Mindfulness-based cognitive therapyreduces overgeneral autobiographical memory in formely depressed patients. Journal of Abnormal Psychology, 109, 150–155. [PubMed: 10740947]
[17]. McBride C, Segal ZV, Kennedy S, & Gemar M(2007) ,Changes in autobiographical memoryspecificity following cognitive behavior therapy and pharmacotherapy for major depression. Psychopathology, 40, 147–152. [PubMed: 17318006]