1. Introduction
Pneumonia is one of the most common diseases in the world. Many people are suffering from pneumonia. What’s worse, a large amount of people has died because of pneumonia. It’s important for people to find the method of dealing with pneumonia, saving patients’ lives. Fortunately, with the development of medical industry, people have found or invented many antibiotics to kill the pathogens of pneumonia, helping people to recover from pneumonia. However, the pathogens of pneumonia have already generated the resistance against some antibiotics, making these antibiotics become less effective when they are used to kill the pathogens [1]. In addition, although some antibiotics are not strongly resisted by the pathogens, some of them are too expensive, leading to the heavy financial burden for patients and governments. Therefore, how to treat pneumonia with a both effective and economic-friendly way is worth discussing. In this essay, I’ll discuss the therapy of dealing with pneumonia by the combination of Levofloxacin and Cefixime. Levofloxacin and Cefixime are both effective and economic-friendly antibiotics. Additionally, they are absolutely two different kinds of antibiotics, which means the combination therapy can deal with the resistance against antibiotics. Therefore, the combination therapy will be a both effective and economic-friendly way to deal with pneumonia, which can benefit the whole world.
2. Pneumonia
2.1. The Definition and Classification of Pneumonia
Pneumonia refers to inflammation of the terminal airways, alveoli, and pulmonary interstitium. It can be caused by pathogens, physical and chemical factors, immune damage, allergies, and drugs. Pneumonia caused by pathogenic microorganisms is the most common. There are three classification methods for pneumonia caused by pathogens. First of all, according to the pathogen types, pneumonia can be divided into bacterial pneumonia, viral pneumonia, atypical pathogen pneumonia, pulmonary fungal disease, and pulmonary parasitic disease. Secondly, according to the patient’s environment while being infected, pneumonia can be divided into community acquired pneumonia (CAP) and hospital acquired pneumonia (HAP). CAP refers to pneumonia contracted outside of the hospital, including pneumonia that develops during the incubation period after admission due to pathogen infections with a clear incubation period. HAP refers to pneumonia that occurs in the hospital after 48 hours or more of admission, including pneumonia that occurs within 48 hours after being infected in the hospital and discharged from the hospital. Thirdly, according to the anatomical site where pneumonia occurs in the lungs, pneumonia can be divided into lobar pneumonia, lobular pneumonia, and interstitial pneumonia. In clinical situation, doctors always make the diagnosis based on the chest radiograph [2].
2.2. History of Pneumonia
The initial records of pneumonia could be traced back to Hippocratic era. He, like other ancient medical experts, classified diseases with chest pain symptoms as Perioneumonia, and this term had been used for over 2000 years. Hippocratic used blood letting and hot compress to treat patients with Perioneumonia. In the 17th century, Sydenham, a famous Dutch clinical physician, believed that Perioneumonia was the same disease as Pleurisy, but the scope of Perioneumonia’s invasion of lung parenchyma was more extensive. Sydenham reported a case of Perioneumonia Notha, and his student Huxham invented a formula specifically designed to treat it, which was actually a type of alcohol containing cinchona. In 18 century, the famous British clinical physician Boerhaave described two types of peripulmonary inflammation in his book “Proverbs”. One occurs at the end of the pulmonary artery, and the other occurs in the bronchus. This may be the earliest distinction between lobar pneumonia and lobular pneumonia. Italian anatomist Morgagni dissected and observed the bodies of pneumonia patients after death, studying pneumonia pathologically. What’s more, Baillie first described the liver like changes in the lungs of pneumonia patients. The Western medicine percussion method was invented in the 18th century. Auenbrugger used percussion method in 1761 to analyze the percussion sounds of normal lungs and those of pneumonia patients. The invention of percussion method greatly helped doctors diagnose chest diseases. In 19 century, French doctor La ё Nnec invented the Stethoscope. The appearance of Stethoscope makes it possible for doctors to find chest diseases, such as pneumonia, in time. In 1819, La ё Nec published the classic work “On Auscultation”, in which he meticulously described many common auscultation sounds in chest diseases. La ё NEC also noticed that the crepitus heard during chest auscultation is an important indicator for determining the initial stage of pneumonia and a sign of the dissipating stage of pneumonia. Since the invention of percussion and auscultation methods, people’s understanding of pneumonia has become increasingly profound. Most pathogenic bacteria were discovered in the last 30 years of the 19th century, allowing doctors to make etiological diagnosis of pneumonia. In 1895, German physicist Roentgen invented X-ray, which was quickly applied in medicine, especially in the diagnosis of pneumonia. In 1920, Ramsay reported Pneumonilis based on X-ray examination results. In 1938, Reimann further introduced this type of pneumonia, and in 1945, Dingle reported that the pathogen of Pneumonilis may be a virus. The invention of antibiotics in the 20th century created miracles for the treatment of bacterial diseases. In 1928, A. Fleming discovered penicillin; in 1935, G. Domagk invented the sulfa drug Prontosil; in 1944, S. A. Waksmann invented Streptomycin; in 1947, he discovered Chloramphenicol; in 1948, he discovered Chlortetracycline; since then, tetracycline, Oxytetracycline and other antibiotics have been used in clinical practice. Bacterial pneumonia has been beaten by the antibiotics repeatedly [3].
2.3. The Symptoms of Pneumonia
Acute onset, chills, fever. Cough, phlegm, mostly purulent phlegm, occasionally with phlegm and blood. Typically, Streptococcus pneumoniae pneumonia has rust colored sputum, caused by the release of hemoglobin from red blood cells in a fibrous exudate. Mycoplasma pneumoniae pneumonia and viral pneumonia have low sputum volume, mostly white sputum. Phlegm from pulmonary fungal disease is white and thick, with filamentous symptoms, making it difficult to cough up. Physical examination may show signs of lung consolidation or the smell of moist rales. Severe infections can manifest as circulatory failure, respiratory failure, or multiple organ dysfunction [4].
2.4. The Impact and Mortality of Pneumonia
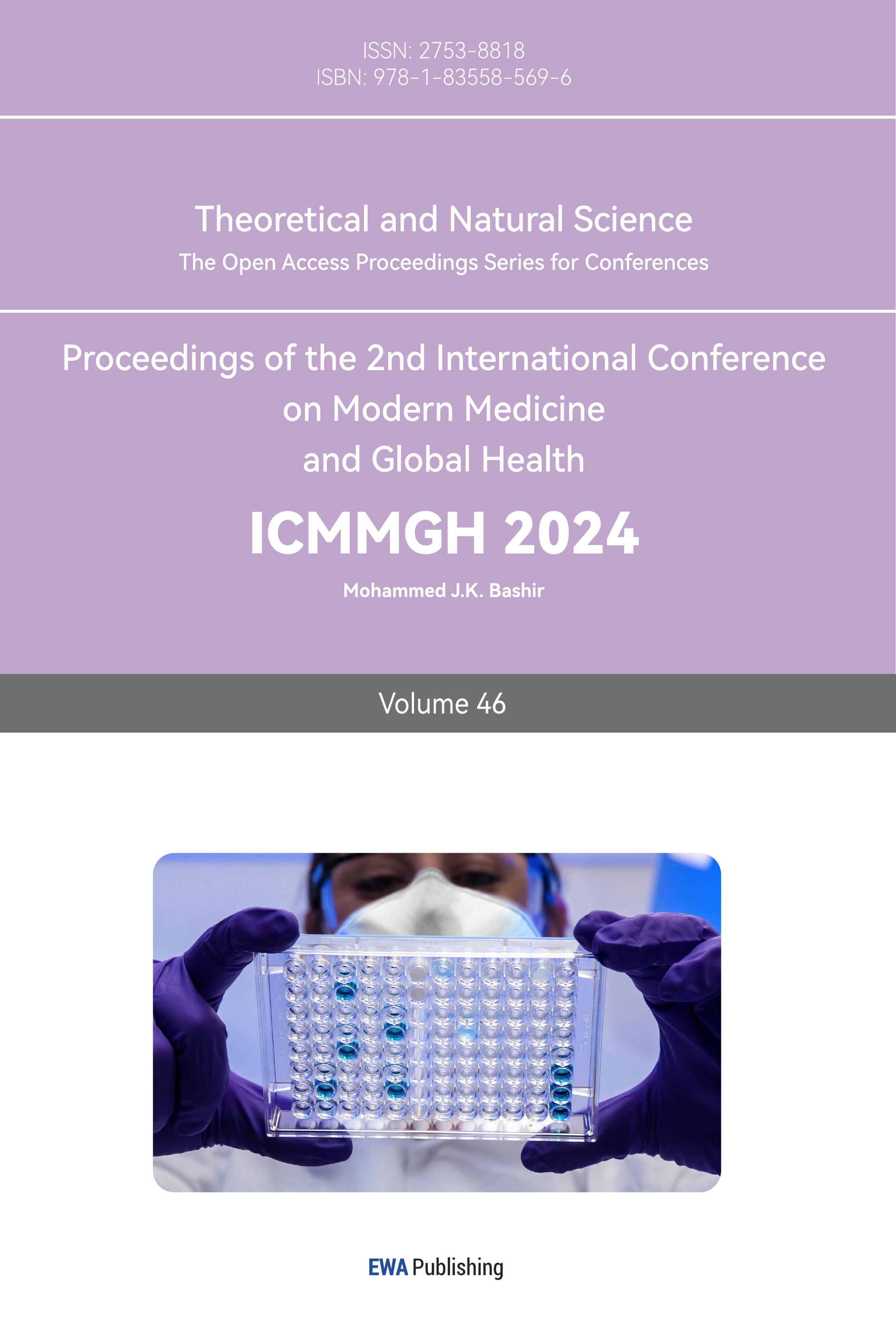
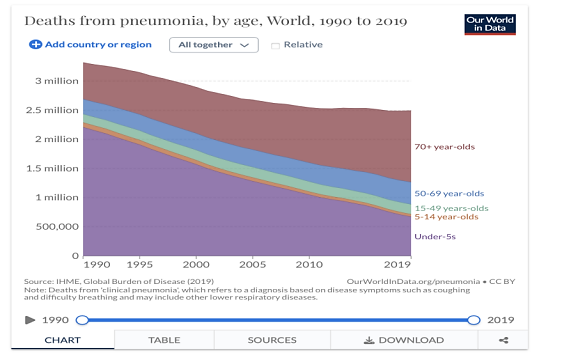
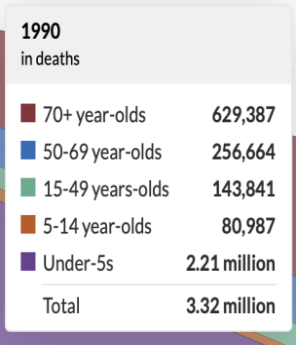
|
|
Figure 1. Deaths from pneumonia, by age, from 1990 to 2019 [5]. | Figure 2. Deaths from pneumonia, by age, in1990 [5]. |
|
|
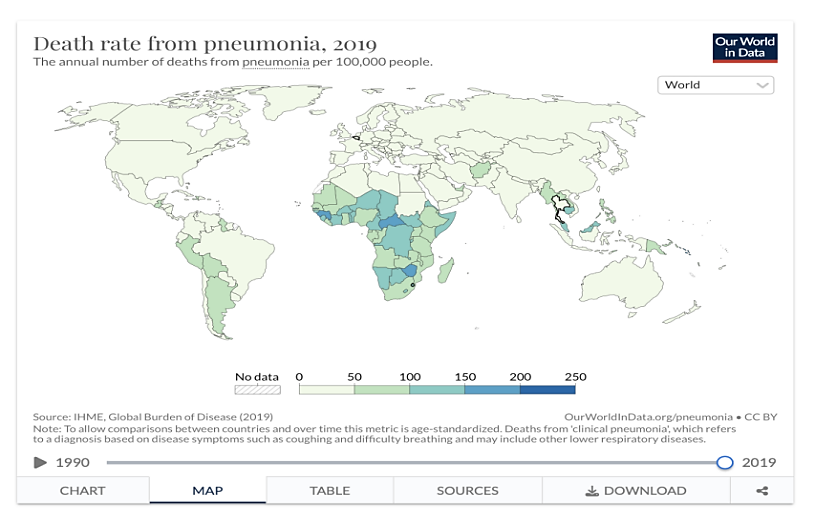
Figure 3. Deaths from pneumonia, by age, in 2019 [5]. | Figure 4. Death rate from pneumonia, 2019 [5]. |
|
|
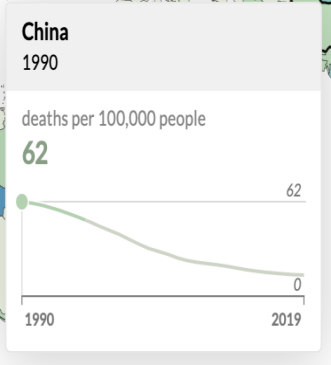
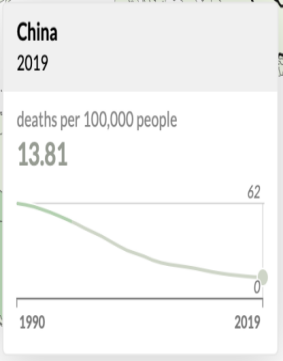
Figure 5. Deaths from pneumonia in China in 1990 [5]. | Figure 6. Deaths from pneumonia in China in 2019 [5]. |
|
|
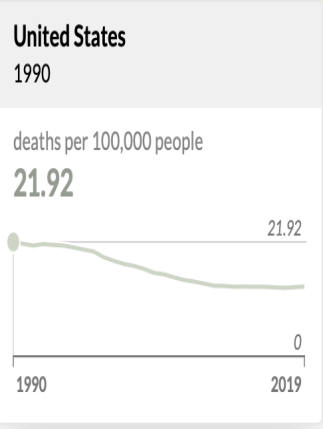
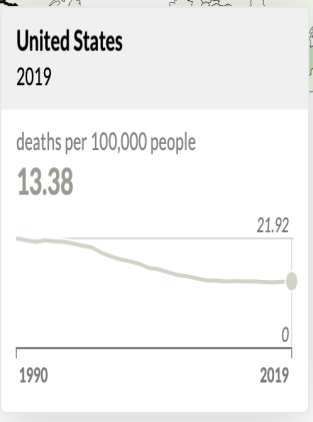
Figure 7. Deaths from pneumonia in the U. S. in 1990 [5]. | Figure 8. Deaths from pneumonia in the U. S. in 2019 [5]. |
In China, as shown in figure 5 and figure 6, the deaths from pneumonia per 100000 people were 62 people in 1990 and 13. 81 people in 2019. In the United States, as shown in Figure 7 and Figure 8, the deaths from pneumonia per 100000 people were 21. 92 people in 1990 and 13. 38 people in 2019 [14].
The death rate of pneumonia differs from region to region. According to figure 4, the death rates from pneumonia in developing countries are highest in the world, especially for the Sub-Sahara Africa, the South-East Asia, and some countries in South America. And the death rates of pneumonia in developed countries are relatively low [15]. This difference is related to the different developing level of medical industry and different economic strength in different countries.
The number of the deaths and death rate from pneumonia have been reduced, but the problem of dealing with pneumonia is still severe and challenging to people. And how to deal with pneumonia with some both economic-friendly and effective approaches is also worth discussing.
3. Streptococcus pneumoniae-- one of the pathogenic bacteria of pneumonia
3.1. Introduction of Streptococcus pneumoniae and how they infect the lung
Streptococcus pneumoniae, also known as pneumococcus, often reside in the nasopharyngeal cavity of normal individuals. Most Streptococcus pneumoniae are not pathogenic or have weak pathogenicity, with only a few having pathogenicity. They are the main pathogens of bacterial pneumonia [16]. In developing countries, 5 million children under the age of 5 die each year from pneumonia caused by Streptococcus pneumoniae. In recent years, 40% to 50% of community acquisition pneumonia in the UK has been caused by Streptococcus pneumoniae [6]. Streptococcus pneumoniae are Gram positive bacteria and anaerobic bacteria with a spearhead like shape, mostly arranged in pairs, with opposite wide ends and outward pointed tips. The bacterial cell is surrounded by a transparent ring, as shown in figure 8. It can also appear as a single or short chain in sputum, pus, and lung tissue lesions. No flagella or spores. capsule can be formed in the body or serum-containing culture medium, and they require special staining to be visible [7]. Streptococcus pneumoniae’s pathogenicity are mainly due to the invasiveness of its capsule containing high molecular weight polysaccharides on tissues, and the bacterial exudate spreads through the Kohn pores to the surrounding alveoli, affecting lung segments or lobes (hence also known as lobar pneumonia). Streptococcus pneumoniae does not produce toxins and generally does not cause lung tissue necrosis or other damage to lung structures [8].

Figure 9. Streptococcus pneumoniae capsule,capsule stain x1500 [9].
3.2. Image of The Infected Lung and The Normal Lung
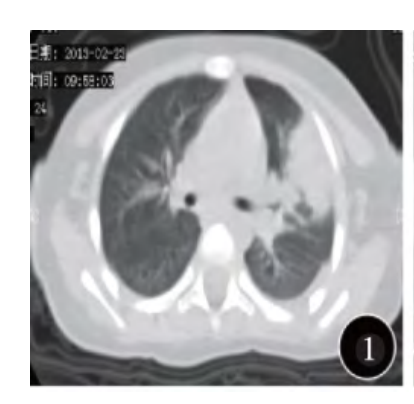
Figure 10. Imaging of Streptococcus pneumoniae pneumonia [8].
The consolidation lesion starts from the periphery of the left upper lobe of the lung, adjacent to the pleura, and spreads towards the center; there is a small amount of pleural effusion on the left side [10].
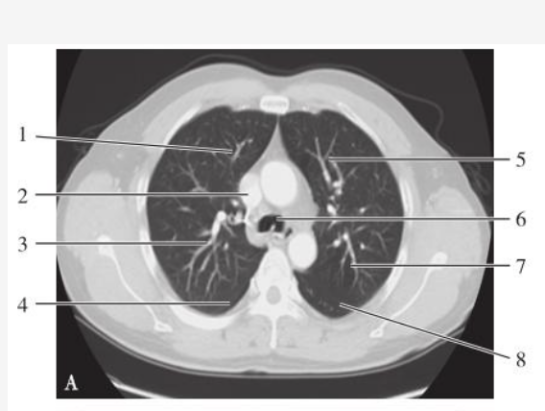
Figure 11. Imaging of the normal lung [10].
4. Drugs used to treat pneumonia
4.1. Brief introduction of other approaches with some crucial disadvantages that people use to deal with pneumonia
Vancomycin:
People use Vancomycin to deal with pneumonia. Vancomycin is a kind of glycopeptide antibiotic, which is extremely good at killing Gram positive and Gram negative bacteria, including the Streptococcus pneumoniae [11]. And the Streptococcus pneumoniae almost hasn’t generated the resistance against Vancomycin. Zhao Xiaoji and others did a research about the rate of resistance against antibiotics generated by streptococcus pneumoniae. They collect specimens from 75201 patients treated at The Third Hospital of Mianyang from January 2017 to December 2020, and a total of 596 strains of Streptococcus pneumoniae were isolated. After conducting bacterial identification, drug sensitivity tests, and statistical analysis of the data, as shown in Table 1, they found that the drug resistance rate of Streptococcus pneumoniae against Vancomycin is 0% in both children group and adult group [12]. However, it rarely metabolizes in human bodies. More than 90% Vancomycin need to excrete through the filtration process of glomerulus. Therefore, in addition to other common side effects, it has a relatively higher Nephrotoxicity. Its adverse effects rate is also relatively high [13]. And its price is also relatively high. I did a survey in Qilu Hospital of Shandong University. I found that the price of Wenkexin Vancomycin Hydrochloride for injection is 103. 99 yuan, and the price of Laikexin Vancomycin Hydrochloride for injection is 78. 00 yuan. And the price of Levofloxacin for injection is 30. 81 yuan; the price of Levofloxacin for oral administration is 24. 00 yuan. And the Cefixime for oral administration is 3. 79 yuan. Obviously, Vancomycin has a relatively high price than Cefixime and Levofloxacin, which means it is not very economic-friendly.
Erythromycin:
People use Erythromycin to deal with pneumonia. Erythromycin is a kind of macrolides antibiotic, which can be used to kill the pathogenic bacteria of pneumonia, including the streptococcus pneumoniae. Its side effects are rare and mild [14]. However, the Streptococcus pneumoniae has generated a strong resistance against Erythromycin, which means its efficiency of killing Streptococcus Pneumoniae is largely reduced. As I mentioned before, Zhao Xiaoji and others did a research about the drug resistance generated by Streptococcus pneumoniae. As shown in Table 1, we can see than the drug resistance rate of Streptococcus pneumoniae against Erythromycin is 94. 7% in the children group; the drug resistance rate of Streptococcus pneumonia against Erythromycin is 98. 6% in the adult group. Therefore, Erythromycin is not a effective way for people to deal with pneumonia [15].
Table 1. Comparison of drug resistance rate of Streptococcus pneumoniae isolated from children group and adult group [strains(%)]. [16].
Antibiotics | Children Group (n=378) | Adults Group (n=218) | The value of x² | The value of P |
Penicillin | 31(8. 2) | 35(16. 1) | 8. 66 | 0. 00 |
Amoxicillin | 73(19. 3) | 58(26. 6) | 4. 29 | 0. 04 |
Ceftriaxone | 21(5. 6) | 34(15. 6) | 16. 64 | 0. 00 |
Cefotaxime | 23(6. 1) | 36(16. 5) | 16. 86 | 0. 00 |
Tetracycline | 342(90. 5) | 206(94. 5) | 3. 02 | 0. 08 |
Erythromycin | 358(94. 7) | 215(98. 6) | 5. 71 | 0. 02 |
Linazolamide | 0 | 0 | —— | —— |
Levofloxacin | 4(1. 1) | 28(13. 2) | 37. 80 | 0. 00 |
Vancomycin | 0 | 0 | —— | —— |
Vancomycin is extremely effective, but it is not very economic-friendly and has many severe adverse effects. Erythromycin is relatively mild and safe, but it is not effective while being used to kill Streptococcus pneumoniae. Therefore, there must be other better antibiotics which can be used to kill Streptococcus pneumoniae and deal with pneumonia.
4.2. The Combination Therapy with Levofloxacin and Cefixime to Deal with Pneumonia
4.2.1. Levofloxacin
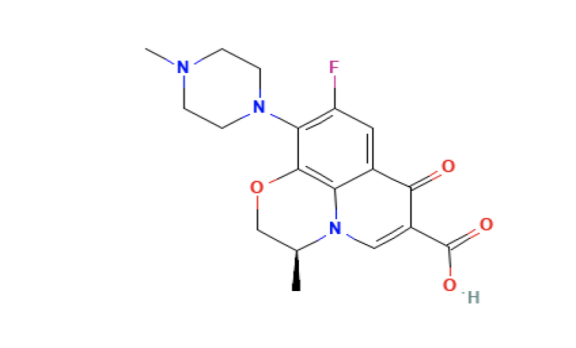
Figure 12. The picture shows the structure of Levofloxacin [16].
(1) Basic Information:
Levofloxacin is a quinolone antibiotic, and it is also the broad-spectrum antibiotic. Its molecular formula is C18H20FN3O4;its IUPAC name is (2S)-7-fluoro-2-methyl-6-(4-methylpiperazin-1-yl)-10-oxo-4-oxa-1-azatricyclo[7. 3. 1. 05, 13]. trideca-5(13), 6, 8, 11-tetraene-11-carboxylic acid. Its molecular weight is 361. 4g/mol. It is freely soluble in glacial acetic acid and chloroform;it is sparingly soluble in water [17]. Its Basic pKa is 8. 12 and its Acidic pKa is 6. 1 [17].
(2) The Mechanism of Action:
As the left-handed isomer of Ofloxacin, Levofloxacin has a good effect on gram-positive bacteria, including Streptococcus pneumoniae. Quinolones can block DNA replication and interfere with the distribution of replicated DNA to offspring cells by inhibiting DNA gyrase and Topoisomerase Ⅳ of bacteria, thus achieving rapid sterilization [18].
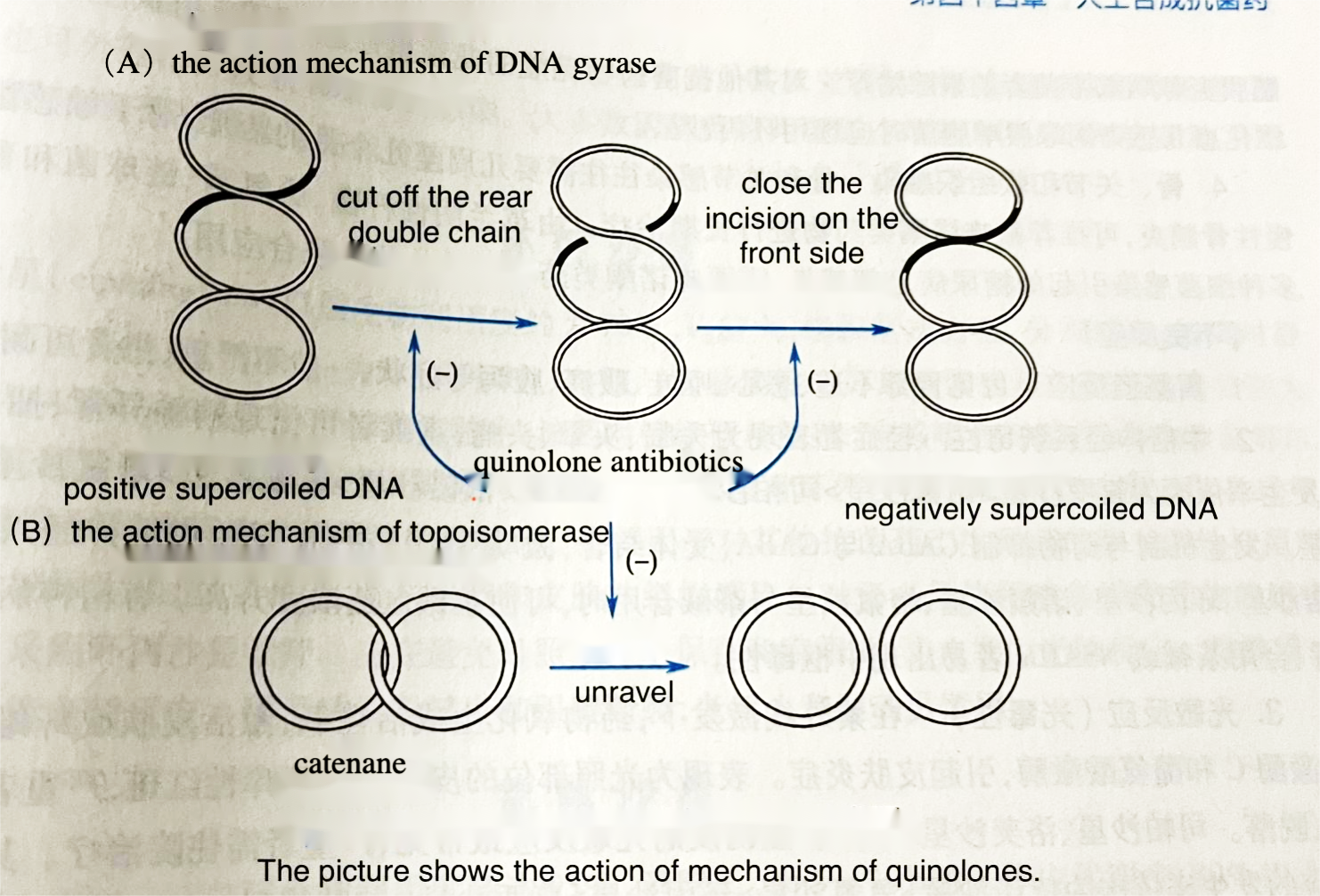
Figure 13. The mechanism of Quinolone antibiotics [19].
(3) Usage, Dosage, and Some of the Precautions
2007 CAP Diagnosis and Treatment Guidelines in the United States pointed out that when Levofloxacin is used to deal with pneumonia, doctors should maintain the plasma concentration above the mutant prevention concentration as long as possible, ensuring the success of treatment and preventing the occurrence of drug-resistant mutants [20]. In China, Levofloxacin can be used by diluting it into 0. 9% sodium chloride injection or 5% glucose injection for intravenous drip. The adults receive 0. 3g-0. 6g Levofloxacin per day, and it should be given once or twice per day by injection. Depending on the type and symptoms of infection, the amount should be modified appropriately. Moreover, it can also be used for oral administration in China. When it is used to deal with community acquired pneumonia, people should be given 0. 4g per day and twice a day; or people can be given 0. 5g per day and once a day; the treatment period is 7days [21]. Like other quinolone antibiotics, Levofloxacin can’t be given to children and pregnant women.
(4) The Efficiency: It’s very good at dealing with the pathogenic bacteria of pneumonia, including Streptococcus pneumoniae. Additionally, the resistance against Levofloxacin generated by Streptococcus Pneumoniae is not very high and serious. As shown in Figure 12, according to the research done by Zhao Xiaoji and others, the drug resistance rate of Streptococcus pneumoniae against Levofloxacin is 1. 1% in children group;the drug resistance rate of Streptococcus pneumoniae against Levofloxacin is 13. 2% in adult group [22]. According to the survey I did in Qilu Hospital of Shandong University, the price of Levofloxacin for injection is 30. 81 yuan. And the price of Levofloxacin for oral administration is 24. 00 yuan. It’s economic-friendly. Tang Jinwen did a research at Daze Health Center, Xinhui District, Jiangmen City, Guangdong Province. He divided 100 patients who had community acquired pneumonia in half into two groups. In addition to some basic therapies, the patients in the experimental group were treated with Levofloxacin. And in the control group, the patients were treated with conventional therapy. The patients in the experimental group were given Levofloxacin for injection 500mg per time and once per day. When the patients in the experimental group got better, the therapy changed into Levofloxacin with oral administration. After conducting the therapies and collecting the data, Tang Jinwen found that the total effective rate of the experimental group (Levofloxacin Treatment) was 98%, and the adverse effects rate of the experimental group(Levofloxacin Treatment)was only 1. 9%. In the control group (Conventional Treatment), the total effective rate was 86%, and the adverse effects rate was 13. 4% [38]. Therefore, even if we use Levofloxacin alone to deal with pneumonia, it will be pretty effective and safe.
(5) Synthesis: This is a relatively new way to synthesize Levofloxacin-- “One Pot” Synthesis. It’s invented by Zhao Feichao, etc. It is more environmental-friendly than traditional approaches;it has low waste and high yield [23].
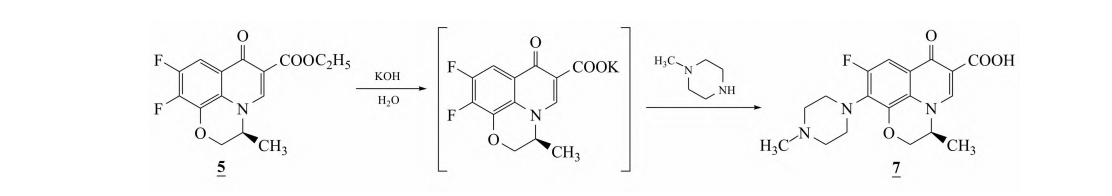
Figure 14. The picture shows the “One Pot” Synthesis of Levofloxacin [40].
The Specific Process of Synthesis:
Add 20. 0g 5, 4. 0g of potassium hydroxide, and 120mL of water to a 500mL three necked bottle, raise the temperature to 60 ℃, and keep it warm until the spots of levofloxacin cyclic ester disappear after TLC detection. Add 105. 0 g of N-methylpiperazine. Continue to raise the temperature to 100 ℃, keep it warm for 9 hours, and then concentrate until dry. Add 100g of water, adjust the pH to 5. 0 with hydrochloric acid, then adjust to neutral with sodium hydroxide, extract with dichloromethane, and concentrate until dry. Add 100 g of anhydrous ethanol to dissolve at high temperature, and decolorize with an appropriate amount of activated carbon. Slowly cool down, crystallize, filter, and dry to obtain 20. 3 g of light yellow solid-Levofloxacin, with a yield of 87. 0% [24].
4.2.2. Cefixime
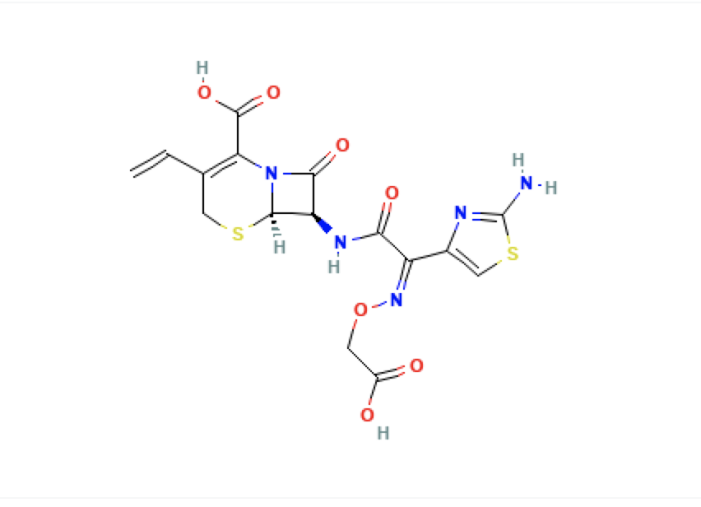
Figure 15. The picture shows the structure of Cefixime [25].
(1) Basic Information:
Cefixime is the Cephalosporin and β Lactam antibiotic, which can be used to kill Streptococcus pneumoniae, etc. Cephalosporin are a kind of antibiotics obtained from natural Cephalosporin C through Semisynthesis [25]. Its molecular formula is C16H15N5O7S2. Its IUPAC name is (6R, 7R)-7-[[(2Z)-2-(2-amino-1, 3-thiazol-4-yl)-2-(carboxymethoxyimino)acetyl]. amino]. -3-ethenyl-8-oxo-5-thia-1-azabicyclo[4. 2. 0]. oct-2-ene-2-carboxylic acid. Its molecular weight is 453. 5 g/mol. This drug was launched in Japan in 1987 and in China in 1994 [25].
(2) The Mechanism of Action
Its antibacterial mechanism is mainly to inhibit the synthesis of mucopeptides in the cell wall of bacteria, thus preventing the cross linking of mucopeptide chains, so that bacteria cannot form a tough wall. In addition, there are special protein molecules that combine with penicillin or Cephalosporin on the cell membrane of bacteria, which is the role of β Lactam antibiotics, namely penicillin binding protein (PBP). Most penicillin or Cephalosporin antibiotics mainly combine with PBP3 and PBP1 to form filamentous and globular bodies, which then cause bacteria to deform and shrink, and gradually dissolve and die [26].
(3) Usage and Dosage
It’s generally Oral administration to deal with pneumonia. For children who weight more than 30kg, they should be given 0. 1g Cefixime per time, twice a day. For children who weight less than 30kg, they should be given 1. 5-3mg per kilogram per time, twice a day. The amount should be modified according to age, weight, and disease circumstance. For the adults, they should be given 0. 1g Cefixime per time, twice a day. The amount should be modified according to the disease circumstance [27].
(4) The Efficiency:
The third generation Cephalosporin(including Cefixime) has strong tissue penetration and is widely distributed in the body. It can reach effective antibacterial concentration in tissue, body cavity and body fluid, and is basically non-toxic to the kidney [28]. Ma Xiaoli did a research in Maternal and Child Health Hospital of Chuanhui, Zhoukou, Henan. She divided 140 patients who had light to moderate community acquired pneumonia in half into two groups. Patients in the control group were treated with Amoxicillin for oral administration, and patients in the experimental group were treated with Cefixime for oral administration. After conducting the research and collecting data, Ma Xiaoli found that the total effective rate in the control group was 72. 86%, and the total effective rate in the experimental group was 90. 00%. And the duration of the recovery and treating process was shorter in the experimental group than which in the control group. The adverse effects rate in the experimental group was 4. 28%, and the adverse effects rate in the control group was 14. 28%. All in all, we can see Cefixime is good at dealing with pneumonia for its efficiency and mildness [29]. Although as the third generation Cephalosporin, which is not so good at killing Gram positive bacteria as the first and second generation Cephalosporin, Cefixime can still be used to kill Streptococcus pneumoniae [30].
(5) The Synthesis:
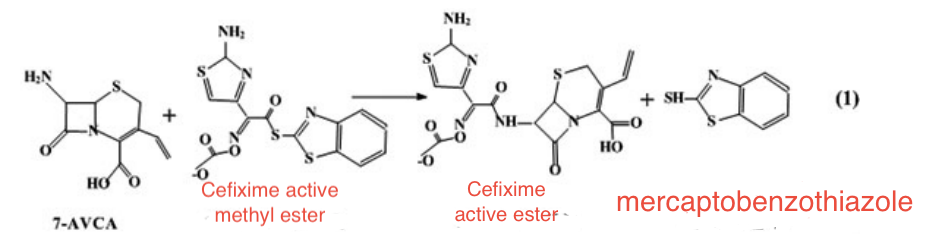
Figure 16. The first step of the synthesis of Cefixime [31].
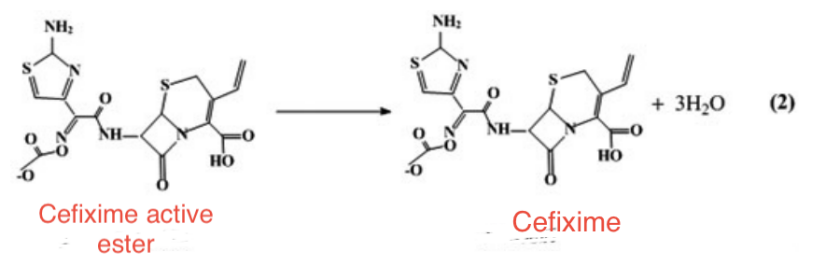
Figure 17. The second step of the synthesis of Cefixime [32].
This approaches replaces traditional tetrahydrofuran, acetone, and other solvents with Cefixime active methyl ester, 7-amino-3-vinyl-cephalanic acid, and ethyl acetate, and undergoes acylation reaction to obtain Cefixime ester. Then, Cefixime is obtained through hydrolysis reaction. The solution is crystallized, filtered, and dried to obtain Cefixime finished product. This method not only reduces the types of solvents used, but also facilitates the recovery and reuse of solvents, which is beneficial for removing reaction by-products such as mercaptobenzothiazole [33].
4.2.3. The combination with Levofloxacin and Cefixime to deal with pneumonia
(1) The Advantages of Combination Therapy
Levofloxacin and Cefixime are two different antibiotics. Levofloxacin is a Quinolone antibiotic, which can block DNA replication and interfere with the distribution of replicated DNA to offspring cells by inhibiting DNA gyrase and Topoisomerase Ⅳ of bacteria, thus achieving rapid sterilization [34]. However, Cefixime is a Cephalosporin antibiotic and has a completely different mechanism. Its antibacterial mechanism is mainly to inhibit the synthesis of mucopeptides in the cell wall of bacteria, thus preventing the cross linking of mucopeptide chains, so that bacteria cannot form a tough wall. In addition, there are special protein molecules that combine with penicillin or Cephalosporin on the cell membrane of bacteria, which is the role of β Lactam antibiotics, namely penicillin binding protein (PBP). Most penicillin or Cephalosporin antibiotics mainly combine with PBP3 and PBP1 to form filamentous and globular bodies, which then cause bacteria to deform and shrink, and gradually dissolve and die [34]. These two antibiotics are both broad-spectrum antibiotics, and both of them can be used to kill Streptococcus pneumoniae, which is one of the main pathogenic bacteria of pneumonia. When they are used alone, their efficiency and safety are both pretty good [34]. [35].
Now, I want to introduce a word-Cross Resistance. Cross Resistance refers to tolerance (as of a bacterium) to a usually toxic substance (such as an antibiotic) that is acquired not as a result of direct exposure but by exposure to a related substance [36]. According to Zhao Xiaoji and other people’s research, Streptococcus pneumonia has generated resistance against both Quinolone antibiotics and Cephalosporin antibiotics [37]. If we just use one antibiotic or a single type of antibiotic, the Streptococcus pneumoniae may generate resistance not only against one specific antibiotic but also against one entire type of antibiotic. The problem of cross resistance will get more serious. And the efficiency of the antibiotics will be largely reduced. The combination of Levofloxacin and Cefixime can resolve this problem well. They have completely different mechanisms and target points. And they are not the same kind. If they can be used together to kill Streptococcus pneumoniae and deal with pneumonia, the problem of Cross Resistance can be avoided, and they can work together to kill Streptococcus pneumoniae from two targets, which is more comprehensively and effectively. According to the survey I did in Qilu Hospital of Shandong University, the price of Levofloxacin for injection is 30. 81 yuan; the price of Levofloxacin for oral administration is 24. 00 yuan. And the Cefixime for oral administration is 3. 79 yuan. They are both economic-friendly. After calculating, we can see that the combination therapy with Levofloxacin and Cefixime is also economic-friendly.
(2) Research Review
Zhang Rongrong did a research in The People’s Hospital of Liuyang. 96 patients with chronic pneumonia treated at The People’s Hospital of Liuyang from October 2019 to October 2020 were selected as the study subjects, and they were randomly divided into a control group and a experimental group, with 48 patients in each group. There was no statistically significant difference in general information between the two groups of patients (P>0. 05). All patients are required to remain quiet, rest in bed, and receive nutritional support, oxygen inhalation, and treatment to maintain respiratory patency. In addition, the patients in the control group were treated by Levofloxacin for intravenous infusion; the amount is 0. 4 g per time and twice a day. The patients in the experimental group were treated by the combination of Levofloxacin and Cefixime. They are treated by both Levofloxacin for intravenous infusion (0. 4 g per time and twice a day) and Cefixime for oral administration (200mg per time and twice a day). The treatment duration period was two weeks. After two weeks, Zhang Rongrong compared the changes in inflammatory factor levels between two groups of patients before and after 2 weeks of treatment. As shown in Table 2, the total effective rate of the control group was 79. 17% and the total effective rate of the experimental group was 93. 75%. And as shown in Table 3, the adverse effects rate of the control group was 35. 41%, and the adverse effects rate of the experimental group was 10. 42%. All in all, the treatment conducted in the experimental group (The combination therapy with Levofloxacin and Cefixime) is more effective than the treatment conducted in the control group (The therapy with only Levofloxacin). And even the adverse effects rate of the combination therapy with Levofloxacin and Cefixime is lower than the adverse effects rate of the mono therapy with Levofloxacin. The difference is statistically significant (P<0. 05). Therefore, the combination therapy with Levofloxacin and Cefixime is both effective and safe [38].
Table 2. The Comparison of Effective Rate[cases(%)]. [39].
Group | Cases | Significant Effect | Normal Effect | No Effect | Total Effective Rate(%) |
Control Group | 48 | 29(60. 41) | 9(18. 75) | 10(20. 83) | 38(79. 17) |
Experimental Group | 48 | 38(79. 17) | 7(14. 58) | 3(6. 25) | 45(93. 75) |
PS:Compare between the groups, x²=5. 537, P<0. 05 | |||||
Table 3. The Comparison of Adverse Effects Rate [Cases(%)]. [40].
Group | Cases | Hepatic Insufficiency | Leukopenia | Gastrointestinal Reaction | Rash | Total Occurrence |
Control Group | 48 | 5(10. 41) | 5(10. 41) | 4(8. 33) | 3(6. 25) | 17(35. 41) |
Experimental Group | 48 | 1(2. 08) | 2(4. 16) | 2(4. 16) | 0 | 5(10. 42) |
PS:Compare between the groups, x²=5. 437, P<0. 05 | ||||||
Zhu Yahong and Tang Xiaoying did a research in Shanghai Pudong Hospital. 106 elderly pneumonia patients who visited the Respiratory Department of Pudong Hospital in Shanghai from February 2014 to February 2015 were randomly divided into an experimental group and a control group, with 53 patients in each group. There was no statistically significant difference in general information such as gender, age, pathological classification, course of disease, and severity between the two groups of patients, indicating comparability. All patients should rest in bed, remain quiet, maintain respiratory patency, inhale oxygen, correct water electrolyte acid-base balance, and receive targeted treatment such as nutritional support. In addition, the patients in the control group were given intravenous infusion of Levofloxacin hydrochloride injection, and the amount was 0. 4g per time, twice a day. The patients in the experimental group were treated by the combination of Levofloxacin and Cefixime. They are treated by both Levofloxacin for intravenous infusion (0. 4 g per time and twice a day) and Cefixime for oral administration (200mg per time and twice a day). The treatment duration period was 14 days. After the treatment, Zhu Yahong and Tang Xiaoying collected the data and did the research. According to Table 4, the total effective rate of the control group (only Levofloxacin treatment) is 84. 91%; the total effective rate of the experimental group (The combination therapy with Levofloxacin and Cefixime) is 96. 23%. The difference is statistically significant (P<0. 05). After treatment, the disappearance time of clinical signs such as fever, cough, and lung rales in the experimental group was significantly shorter than that in the control group, and the difference was statistically significant (P<0. 05). There was no significant difference in the rate of adverse effects between the experimental group (7. 55%) and the control group (9. 43%). The adverse effects which had taken place during the research were mild and insignificant. No other adverse effects were observed during the treatment of both groups. All in all, according to the data and comparison, the combination therapy with Levofloxacin and Cefixime is more effective than the mono therapy with Levofloxacin. And there was no significant difference in the rate of adverse effects rate between the two groups. This research also proves that the combination therapy with Levofloxacin and Cefixime is both effective and safe [41].
Table 4. Comparison on clinical efficacies between two groups[41].
Group | n/cases | Cure/cases | Significant effect/cases | Normal effect/cases | No effect/cases | Total Effective Rate% |
Control Group | 53 | 20 | 14 | 11 | 8 | 84. 91 |
Experimental Group | 53 | 30 | 16 | 5 | 2 | 96. 23 |
PS:Compare between the two groups, P<0. 05 | ||||||
5. Conclusion
All in all, according to the research reviewed before, the combination therapy with Levofloxacin and Cefixime is a very effective approach to deal with pneumonia. Although Levofloxacin is already a very good antibiotic to kill Streptococcus pneumoniae and deal with pneumonia [41]. , the combination therapy is more effective than the mono therapy with Levofloxacin. And its safety and mildness are also pretty good [42]. [43]. Moreover, according to the survey I did in Qilu Hospital of Shandong University, these two antibiotics’ prices are both relatively low. It is also an economic-friendly therapy. It’s worth popularizing this combination therapy clinically, helping an increasing number of people to get better. I believe this combination therapy will be used clinically more frequently in the future.
References
[1]. Zhao Xiaoji, Dang Hao, Zhang Renfei, Zhang Jing, Kang Yuexi, Ma Yushan & Hou Jun. (2023). Analysis of infection distribution characteristics and drug resistance of 596 strains of clinically isolated Streptococcus pneumoniae. Hainan Medical Journal (03), 398-400.
[2]. Zheng Yu, Chen Xia, Ai Jing, Luo Ziqiang&Guo Xuejun. (2015) . Respiratory System . Published by People’s Medical Publishing House
[3]. Zhen Cheng. (2003). Record of Pneumonia. Published by China Medical News in 2003
[4]. Zheng Yu, Chen Xia, Ai Jing, Luo Ziqiang&Guo Xuejun. (2015) . Respiratory System . Published by People’s Medical Publishing House
[5]. Bernadeta Dadonaite and Max Roser (2018) - “Pneumonia”. Published online at OurWorldInData. org.
[6]. Retrieved from: ‘https://ourworldindata. org/pneumonia’ [Online Resource].
[7]. Li Fan, Xu Zhikai, Huang Min, Guo Xiaokui&Peng Yihong. (2018). Medical Microbiology. Published by People’s Medical Publishing House
[8]. Xian Mo& Wu Zhongdao. (2006). Research progress on epidemiology and virulence factors of Streptococcus pneumoniae infection. Journal of Tropical Medicine(06), 740-742+693.
[9]. Li Fan, Xu Zhikai, Huang Min, Guo Xiaokui&Peng Yihong. (2018). Medical Microbiology. Published by People’s Medical Publishing House
[10]. Zheng Yu, Chen Xia, Ai Jing, Luo Ziqiang&Guo Xuejun. (2015) . Respiratory System . Published by People’s Medical Publishing House
[11]. Bi Zhaoyan, Zhou Zhen, Chen Weihong, Yang Liyun & Chen Min. (2016). Correspondence analysis of respiratory pathogens and chest CT images in children with severe pneumonia. Guizhou Medical Journal(08), 874-876.
[12]. Ding Jianping, Wang Xiaoying, Zou Yu&Gao Li. (2017). Medical Imaging Reading Diagnostic Atlas - Chest Volume. Published by People’s Medical Publishing House
[13]. Li Jun, Liu Kexin, Yuan Hong, Du Zhimin&Yan Suying. (2018). Clinical Pharmacology. Published by People’s Medical Publishing House.
[14]. Zhao Xiaoji, Dang Hao, Zhang Renfei, Zhang Jing, Kang Yuexi, Ma Yushan & Hou Jun. (2023). Analysis of infection distribution characteristics and drug resistance of 596 strains of clinically isolated Streptococcus pneumoniae. Hainan Medical Journal(03), 398-400.
[15]. Zheng Yu, Chen Xia, Ai Jing, Luo Ziqiang&Guo Xuejun. (2015) . Respiratory System . Published by People’s Medical Publishing House
[16]. Li Jun, Liu Kexin, Yuan Hong, Du Zhimin&Yan Suying. (2018). Clinical Pharmacology. Published by People’s Medical Publishing House.
[17]. Zhao Xiaoji, Dang Hao, Zhang Renfei, Zhang Jing, Kang Yuexi, Ma Yushan & Hou Jun. (2023). Analysis of infection distribution characteristics and drug resistance of 596 strains of clinically isolated Streptococcus pneumoniae. Hainan Medical Journal(03), 398-400.
[18]. National Center for Biotechnology Information (2023). PubChem Compound Summary for CID 149096, Levofloxacin. Retrieved August 14, 2023 from https://pubchem. ncbi. nlm. nih. gov/compound/Levofloxacin.
[19]. National Center for Biotechnology Information (2023). PubChem Bioassay Record for Bioactivity AID 781329 - SID 103165325, Source: ChEMBL. Retrieved August 14, 2023 from https://pubchem. ncbi. nlm. nih. gov/bioassay/781329#sid=103165325.
[20]. Zheng Yu, Chen Xia, Ai Jing, Luo Ziqiang&Guo Xuejun. (2015) . Respiratory System . Published by People’s Medical Publishing House
[21]. Yang Baofeng, Chen Jianguo, Zang Weijin, Wei Minjie. (2023). Pharmacology. Published by People’s Medical Publishing House
[22]. Li Yi, Hua Xiang, Xiao Heping, Wang Zhuo, Zhou Jia & Huang Yi. (2013). Pharmacokinetics of Levofloxacin in the lungs of rats with pneumococcal pneumonia following intravenous administration studied by microdialysis. Chinese Journal of Infection and Chemotherapy(02), 109-114. doi:10. 16718/j. 1009-7708. 2013. 02. 024.
[23]. The information comes from China National Drug Administration
[24]. Zhao Xiaoji, Dang Hao, Zhang Renfei, Zhang Jing, Kang Yuexi, Ma Yushan & Hou Jun. (2023). Analysis of infection distribution characteristics and drug resistance of 596 strains of clinically isolated Streptococcus pneumoniae. Hainan Medical Journal(03), 398-400.
[25]. Tang Jinwen. (2015). Clinical efficacy analysis of levofloxacin treatment for community acquired pneumonia. China Medical Engineering(12), 48+50.
[26]. Zhao Feichao, He Wenbiao, Jin Jiahua, Pan Kaiming, Zhu Lin, Cao Ruiwei & Gao Haoling . (2021). “One Pot”Synthesis of Levofloxacin. Fine Chemical Intermediates(03), 45-47. doi:10. 19342/j. cnki. issn. 1009-9212. 2021. 03. 012.
[27]. National Center for Biotechnology Information (2023). PubChem Compound Summary for CID 5362065, Cefixime. Retrieved August 14, 2023 from https://pubchem. ncbi. nlm. nih. gov/compound/Cefixime.
[28]. Zheng Yu, Chen Xia, Ai Jing, Luo Ziqiang&Guo Xuejun. (2015) . Respiratory System . Published by People’s Medical Publishing House
[29]. Ma Xianghong, Li Kun, Su Limin, Peng Huan, Ye Congfa, Yang Shuo & Tan Yuelang. (2020). Synthesis and Identification of Related Substances Cefixime. FINE CHEMICAL INTERMEDIATES(06), 53-55+76. doi:10. 19342/j. cnki. issn. 1009-9212. 2020. 06. 013.
[30]. Chen Xinqian&Jin Youyu. (1998). New Materia Medica. Published by People’s Medical Publishing House
[31]. The information is cited from the instruction of Cefixime
[32]. Zheng Yu, Chen Xia, Ai Jing, Luo Ziqiang&Guo Xuejun. (2015) . Respiratory System . Published by People’s Medical Publishing House
[33]. Ma Xiaoli. (2022). Evaluation of the efficacy and safety of cefixime in the treatment of mild to moderate community-acquired pneumonia in children. Medicine and Pharmacy of Yunnan(02), 69-71.
[34]. Zheng Yu, Chen Xia, Ai Jing, Luo Ziqiang&Guo Xuejun. (2015) . Respiratory System . Published by People’s Medical Publishing House
[35]. Chen Yufeng. (2013). Study on the synthesis of Cefixime. Technology Wind(11), 64+68. doi:10. 19392/j. cnki. 1671-7341. 2013. 11. 053.
[36]. The information is cited from Respiratory System, Edited by Zheng Yu and Chen Xia, etc. Published by People’s Medical Publishing House in Nov. 2015
[37]. The information is cited from New Materia Medica, written by Chen Xinqian and Jin Youyu, published by People’s Medical Publishing House in 1998
[38]. Ma Xiaoli. (2022). Evaluation of the efficacy and safety of cefixime in the treatment of mild to moderate community-acquired pneumonia in children. Medicine and Pharmacy of Yunnan(02), 69-71.
[39]. Tang Jinwen. (2015). Clinical efficacy analysis of levofloxacin treatment for community acquired pneumonia. China Medical Engineering(12), 48+50.
[40]. Merriam-Webster. (n. d. ). Cross-resistance. In Merriam-Webster. com dictionary. Retrieved August 14, 2023, from https://www. merriam-webster. com/dictionary/cross-resistance
[41]. Zhao Xiaoji, Dang Hao, Zhang Renfei, Zhang Jing, Kang Yuexi, Ma Yushan & Hou Jun. (2023). Analysis of infection distribution characteristics and drug resistance of 596 strains of clinically isolated Streptococcus pneumoniae. Hainan Medical Journal(03), 398-400.
[42]. Zhang Rongrong. (2021). Clinical efficacy of Cefixime combined with Levofloxacin in the treatment of chronic pneumonia. Chronic Pathematology Journal (04), 614-616. doi:10. 16440/j. cnki. 1674-8166. 2021. 04. 043.
[43]. Zhu Yahong& Tang Xiaoying. (2015). Clinical observation of cefixime combined with levofloxacin in the treatment of senile pneumonia. Modern Pharmacy and Clinic(10), 1229-1233.
[44]. Tang Jinwen. (2015). Clinical efficacy analysis of levofloxacin treatment for community acquired pneumonia. China Medical Engineering(12), 48+50.
Cite this article
Kong,W. (2024). An in-depth review of pneumonia and the combination therapy of pneumonia with Levofloxacin and Cefixime. Theoretical and Natural Science,46,149-162.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 2nd International Conference on Modern Medicine and Global Health
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Zhao Xiaoji, Dang Hao, Zhang Renfei, Zhang Jing, Kang Yuexi, Ma Yushan & Hou Jun. (2023). Analysis of infection distribution characteristics and drug resistance of 596 strains of clinically isolated Streptococcus pneumoniae. Hainan Medical Journal (03), 398-400.
[2]. Zheng Yu, Chen Xia, Ai Jing, Luo Ziqiang&Guo Xuejun. (2015) . Respiratory System . Published by People’s Medical Publishing House
[3]. Zhen Cheng. (2003). Record of Pneumonia. Published by China Medical News in 2003
[4]. Zheng Yu, Chen Xia, Ai Jing, Luo Ziqiang&Guo Xuejun. (2015) . Respiratory System . Published by People’s Medical Publishing House
[5]. Bernadeta Dadonaite and Max Roser (2018) - “Pneumonia”. Published online at OurWorldInData. org.
[6]. Retrieved from: ‘https://ourworldindata. org/pneumonia’ [Online Resource].
[7]. Li Fan, Xu Zhikai, Huang Min, Guo Xiaokui&Peng Yihong. (2018). Medical Microbiology. Published by People’s Medical Publishing House
[8]. Xian Mo& Wu Zhongdao. (2006). Research progress on epidemiology and virulence factors of Streptococcus pneumoniae infection. Journal of Tropical Medicine(06), 740-742+693.
[9]. Li Fan, Xu Zhikai, Huang Min, Guo Xiaokui&Peng Yihong. (2018). Medical Microbiology. Published by People’s Medical Publishing House
[10]. Zheng Yu, Chen Xia, Ai Jing, Luo Ziqiang&Guo Xuejun. (2015) . Respiratory System . Published by People’s Medical Publishing House
[11]. Bi Zhaoyan, Zhou Zhen, Chen Weihong, Yang Liyun & Chen Min. (2016). Correspondence analysis of respiratory pathogens and chest CT images in children with severe pneumonia. Guizhou Medical Journal(08), 874-876.
[12]. Ding Jianping, Wang Xiaoying, Zou Yu&Gao Li. (2017). Medical Imaging Reading Diagnostic Atlas - Chest Volume. Published by People’s Medical Publishing House
[13]. Li Jun, Liu Kexin, Yuan Hong, Du Zhimin&Yan Suying. (2018). Clinical Pharmacology. Published by People’s Medical Publishing House.
[14]. Zhao Xiaoji, Dang Hao, Zhang Renfei, Zhang Jing, Kang Yuexi, Ma Yushan & Hou Jun. (2023). Analysis of infection distribution characteristics and drug resistance of 596 strains of clinically isolated Streptococcus pneumoniae. Hainan Medical Journal(03), 398-400.
[15]. Zheng Yu, Chen Xia, Ai Jing, Luo Ziqiang&Guo Xuejun. (2015) . Respiratory System . Published by People’s Medical Publishing House
[16]. Li Jun, Liu Kexin, Yuan Hong, Du Zhimin&Yan Suying. (2018). Clinical Pharmacology. Published by People’s Medical Publishing House.
[17]. Zhao Xiaoji, Dang Hao, Zhang Renfei, Zhang Jing, Kang Yuexi, Ma Yushan & Hou Jun. (2023). Analysis of infection distribution characteristics and drug resistance of 596 strains of clinically isolated Streptococcus pneumoniae. Hainan Medical Journal(03), 398-400.
[18]. National Center for Biotechnology Information (2023). PubChem Compound Summary for CID 149096, Levofloxacin. Retrieved August 14, 2023 from https://pubchem. ncbi. nlm. nih. gov/compound/Levofloxacin.
[19]. National Center for Biotechnology Information (2023). PubChem Bioassay Record for Bioactivity AID 781329 - SID 103165325, Source: ChEMBL. Retrieved August 14, 2023 from https://pubchem. ncbi. nlm. nih. gov/bioassay/781329#sid=103165325.
[20]. Zheng Yu, Chen Xia, Ai Jing, Luo Ziqiang&Guo Xuejun. (2015) . Respiratory System . Published by People’s Medical Publishing House
[21]. Yang Baofeng, Chen Jianguo, Zang Weijin, Wei Minjie. (2023). Pharmacology. Published by People’s Medical Publishing House
[22]. Li Yi, Hua Xiang, Xiao Heping, Wang Zhuo, Zhou Jia & Huang Yi. (2013). Pharmacokinetics of Levofloxacin in the lungs of rats with pneumococcal pneumonia following intravenous administration studied by microdialysis. Chinese Journal of Infection and Chemotherapy(02), 109-114. doi:10. 16718/j. 1009-7708. 2013. 02. 024.
[23]. The information comes from China National Drug Administration
[24]. Zhao Xiaoji, Dang Hao, Zhang Renfei, Zhang Jing, Kang Yuexi, Ma Yushan & Hou Jun. (2023). Analysis of infection distribution characteristics and drug resistance of 596 strains of clinically isolated Streptococcus pneumoniae. Hainan Medical Journal(03), 398-400.
[25]. Tang Jinwen. (2015). Clinical efficacy analysis of levofloxacin treatment for community acquired pneumonia. China Medical Engineering(12), 48+50.
[26]. Zhao Feichao, He Wenbiao, Jin Jiahua, Pan Kaiming, Zhu Lin, Cao Ruiwei & Gao Haoling . (2021). “One Pot”Synthesis of Levofloxacin. Fine Chemical Intermediates(03), 45-47. doi:10. 19342/j. cnki. issn. 1009-9212. 2021. 03. 012.
[27]. National Center for Biotechnology Information (2023). PubChem Compound Summary for CID 5362065, Cefixime. Retrieved August 14, 2023 from https://pubchem. ncbi. nlm. nih. gov/compound/Cefixime.
[28]. Zheng Yu, Chen Xia, Ai Jing, Luo Ziqiang&Guo Xuejun. (2015) . Respiratory System . Published by People’s Medical Publishing House
[29]. Ma Xianghong, Li Kun, Su Limin, Peng Huan, Ye Congfa, Yang Shuo & Tan Yuelang. (2020). Synthesis and Identification of Related Substances Cefixime. FINE CHEMICAL INTERMEDIATES(06), 53-55+76. doi:10. 19342/j. cnki. issn. 1009-9212. 2020. 06. 013.
[30]. Chen Xinqian&Jin Youyu. (1998). New Materia Medica. Published by People’s Medical Publishing House
[31]. The information is cited from the instruction of Cefixime
[32]. Zheng Yu, Chen Xia, Ai Jing, Luo Ziqiang&Guo Xuejun. (2015) . Respiratory System . Published by People’s Medical Publishing House
[33]. Ma Xiaoli. (2022). Evaluation of the efficacy and safety of cefixime in the treatment of mild to moderate community-acquired pneumonia in children. Medicine and Pharmacy of Yunnan(02), 69-71.
[34]. Zheng Yu, Chen Xia, Ai Jing, Luo Ziqiang&Guo Xuejun. (2015) . Respiratory System . Published by People’s Medical Publishing House
[35]. Chen Yufeng. (2013). Study on the synthesis of Cefixime. Technology Wind(11), 64+68. doi:10. 19392/j. cnki. 1671-7341. 2013. 11. 053.
[36]. The information is cited from Respiratory System, Edited by Zheng Yu and Chen Xia, etc. Published by People’s Medical Publishing House in Nov. 2015
[37]. The information is cited from New Materia Medica, written by Chen Xinqian and Jin Youyu, published by People’s Medical Publishing House in 1998
[38]. Ma Xiaoli. (2022). Evaluation of the efficacy and safety of cefixime in the treatment of mild to moderate community-acquired pneumonia in children. Medicine and Pharmacy of Yunnan(02), 69-71.
[39]. Tang Jinwen. (2015). Clinical efficacy analysis of levofloxacin treatment for community acquired pneumonia. China Medical Engineering(12), 48+50.
[40]. Merriam-Webster. (n. d. ). Cross-resistance. In Merriam-Webster. com dictionary. Retrieved August 14, 2023, from https://www. merriam-webster. com/dictionary/cross-resistance
[41]. Zhao Xiaoji, Dang Hao, Zhang Renfei, Zhang Jing, Kang Yuexi, Ma Yushan & Hou Jun. (2023). Analysis of infection distribution characteristics and drug resistance of 596 strains of clinically isolated Streptococcus pneumoniae. Hainan Medical Journal(03), 398-400.
[42]. Zhang Rongrong. (2021). Clinical efficacy of Cefixime combined with Levofloxacin in the treatment of chronic pneumonia. Chronic Pathematology Journal (04), 614-616. doi:10. 16440/j. cnki. 1674-8166. 2021. 04. 043.
[43]. Zhu Yahong& Tang Xiaoying. (2015). Clinical observation of cefixime combined with levofloxacin in the treatment of senile pneumonia. Modern Pharmacy and Clinic(10), 1229-1233.
[44]. Tang Jinwen. (2015). Clinical efficacy analysis of levofloxacin treatment for community acquired pneumonia. China Medical Engineering(12), 48+50.