1. Introduction
Hepatitis virus, a globally prevalent pathogen, poses a significant health risk. As medical research progresses, nowadays the human society understand its complexity and impact on human health. Hepatitis A virus (HAV) is a member of the enteroviridae family, consisting of 20 sided cubic spherical particles without envelope, with a diameter of approximately 27-32nm. Its sedimentation coefficient and floating density are specific, located within the cytoplasmic vacuoles of infected liver cells. The viral nucleocapsid contains four peptides, and the RNA genome is single stranded. HAV is closely related to the family of enteroviruses, mainly transmitted through fecal and oral transmission. The incubation period after infection is about 28 days, which is related to the amount of virus. During infection, there is viremia and detoxification [1]. HBV is currently the smallest DNA virus discovered, with a unique and precise genome structure composed of incomplete circular double stranded DNA. Its negative chain contains approximately 3200 bases and four open reading frameworks (ORFs): S, C, P, and X. The characteristic of hepatitis B virus (HBV) replication is the presence of stable covalent closed circular DNA (cccDNA) in the nucleus of the liver, which involves reverse transcription steps. Under the electron microscope, HBV can present three particle structures: large spherical particles with a diameter of about 42nm are infectious, small spherical particles with a diameter of about 22nm, and tubular particles are not infectious [2]. The infection mechanism of hepatitis B mainly includes the following pathways. Let me explain in detail:
Blood transmission: When blood contaminated by hepatitis B virus enters the human body, it will cause hepatitis B virus infection.
The methods include blood transfusion, blood products, gastroscopy, surgery, hemodialysis, etc. If disinfection is not strict, hepatitis B virus may be transmitted through blood.
Maternal to child transmission: This includes intrauterine infections, perinatal infections, and postpartum infections. Intrauterine infection refers to a baby being infected through the placenta. Perinatal infection means that the damaged skin or mucosa of the baby contacts the mother's blood, amniotic fluid or vaginal secretions, thus infecting hepatitis B virus.Postpartum transmission refers to the infection formed by intimate contact between a baby and its mother after birth.
Sexual contact transmission: If hepatitis B patients or hepatitis B virus carriers, saliva, sweat, semen, vaginal secretions and milk may contain hepatitis B virus.
Sexual organs may be slightly damaged in contact and friction, and hepatitis B B virus can enter the human body from the damaged part and infect hepatitis B virus.
In the family, if one spouse is a hepatitis B patient or a carrier of hepatitis B virus, the other must be vaccinated with hepatitis B vaccine to obtain antibodies [3].
Hepatitis C virus (HCV) is a spherical shell virus with a diameter of about 50 nanometers, and its genes are composed of single stranded positive stranded RNA. The buoyancy density of HCV obtained from patients with acute infection and chimpanzees in sucrose is 1.06g/cm3, while the density after cell culture replication is 1.12g/cm3. The low density of viruses in serum is related to low-density lipoprotein, which is closely related to HCV [4].
2. Pathological characteristics of acute hepatitis caused by HAV
2.1. Hepatocellular damage
Upon invasion of liver cells, the HAV virus triggers a series of damaging reactions in the hepatocytes. The most striking change is ballooning of the hepatocytes, a specialized cytomorphologic change that manifests itself as swelling of the hepatocytes to twice or more the normal diameter. The cytoplasm of swollen hepatocytes becomes hyaline, and the size and shape of the nucleus and cytoplasm change dramatically; these changes are particularly pronounced in the central lobular region of the liver parenchyma. Ballooning of hepatocytes not only affects the normal function of the cells, but may also lead to further damage and necrosis of the hepatocytes.
2.2. Inflammatory cell infiltration
With the initiation of the host immune response, the liver develops a marked infiltration of inflammatory cells. These inflammatory cells consist mainly of lymphocytes, macrophages, and activated endothelial cells. Plasma cells may also be present in large numbers in HAV-infected livers, making hepatitis due to HAV infection histologically similar to autoimmune hepatitis. Infiltration and activation of inflammatory cells exacerbate the inflammatory response in the liver and also promote hepatocyte damage and necrosis.
2.3. Liver histologic changes
As a result of ballooning, apoptotic death, and necrosis of hepatocytes, the organization of the liver undergoes significant changes. The arrangement of the liver plates becomes disorganized, which is referred to as lobular disorder. In addition, inflammation in the portal region may extend beyond the boundaries of the portal bundles into the adjacent parenchymal region, leading to more extensive hepatocellular injury. This process is known as fragmentary necrosis, and it is a typical pathologic feature of acute hepatitis A.
2.4. Immune response and autoimmune hepatitis
A unique feature of acute hepatitis A is that the degree of inflammation in the portal region is usually higher than in other types of viral hepatitis. This may be related to the immune response triggered by HAV infection. In some cases, this strong immune response may lead to inflammation and injury in the liver similar to that seen in autoimmune hepatitis. This similarity between the immune response and autoimmune hepatitis complicates the diagnosis and treatment of acute hepatitis A [5].
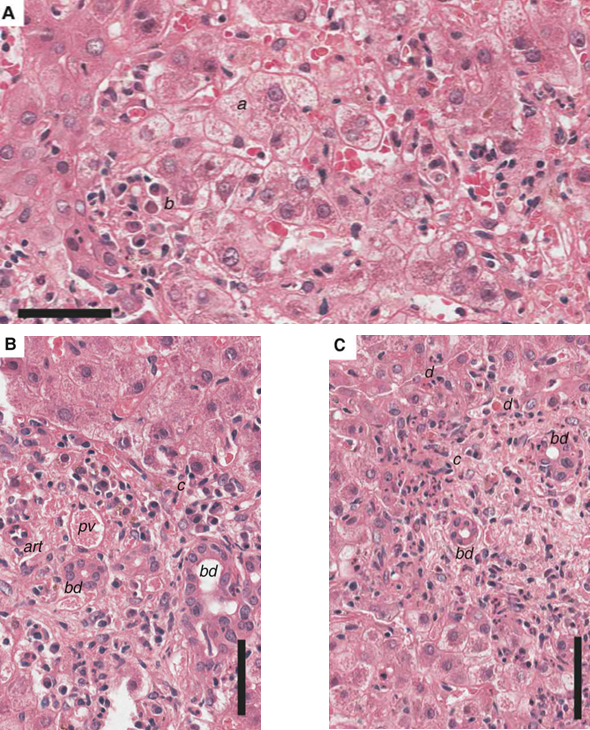
Figure 1. The results of liver tissue sections from a human patient with acute hepatitis A after hematoxylin-eosin (H&E) staining [5].
As shown in figure 1, abnormal hepatic plate arrangement: the normal hepatic plate arrangement (a structure in which hepatocytes are neatly aligned) is disturbed by hepatocellular swelling and inflammatory infiltration within the parenchyma, resulting in disorganized lobular architecture.
Hepatocyte changes: affected hepatocytes (a) are swollen with a reticulated cytoplasmic appearance (lacy appearance), which may be due to cellular edema and/or organelle damage.
Plasma cell infiltrate: the presence of clusters of plasma cells within the parenchyma (b), one of the hallmarks of the inflammatory response.
Inflammatory infiltrate in the portal area: the inflammatory infiltrate around the portal area (including the portal vein, branches of the hepatic artery, and the bile ducts) consists of lymphocytes and macrophages, which cross the border plate and associate with damaged hepatocytes (c), resulting in fragmentary necrosis (piecemeal necrosis).
Fragmentary necrosis: Fragmentary necrosis (c) is one of the characteristic features of acute hepatitis and is manifested by foci of hepatocellular necrosis dispersed within the hepatic lobules and intermingled with surrounding undamaged hepatocytes. This form of necrosis is associated with surrounding residual necrotic or apoptotic hepatocytes (d).
Overall, Figure 1 demonstrates the pathologic changes in the liver of a patient with acute hepatitis A, including swelling of hepatocytes, fragmental necrosis, and inflammatory infiltration in the portal area and parenchyma. These changes are typical pathologic features of acute hepatitis [5].
3. Pathological characteristics of acute hepatitis caused by HBV
hepatocellular degeneration and necrosis with infiltration of inflammatory cells may occur early in the course of the disease in patients with mild acute or chronic hepatitis B. The hepatocellular degeneration and necrosis may occur early in the course of the disease. These inflammatory cells stimulate the fusion zone, leading to destruction of the hepatic lobules and resulting in hepatic impairment. Hepatocellular necrosis with inflammatory cell infiltration occurs in patients with severe acute hepatitis B. Inflammatory necrosis leads to regeneration of liver tissue in the fusion zone with fibrotic changes. Liver function may be impaired by destruction of the hepatic lobules and by the regenerative capacity of hepatocytes. Patients with chronic hepatitis B or acute exacerbation of hepatitis B develop an inflammatory response in hepatocytes during hepatitis activity. This inflammatory response stimulates the hepatic peritoneum, leading to tissue pulling on the hepatic peritoneum, resulting in uneven thickening and increased echogenicity of the hepatic surface, and may even block capillaries and localized thickening of the bile ducts.
4. Stages after HBV infection
4.1. Early stage of infection
In the early stages of HBV infection, the virus enters the body mainly through blood and body fluids and replicates heavily in the liver. At this time, the virus has not yet caused significant damage to the liver cells but has begun to invade the liver. In this stage, the pathological changes in the liver are mainly characterized by mild inflammation and immune response.
4.2. Acute hepatitis stage
As the virus continues to replicate in the liver, hepatocytes begin to be damaged and pathological changes such as hepatocyte degeneration, necrosis and inflammatory cell infiltration occur. These changes lead to impaired liver function and abnormal biochemical indicators such as elevated transaminases. At this point, patients may experience clinical symptoms such as fatigue, loss of appetite, nausea and vomiting.
In the acute hepatitis stage, hepatocyte necrosis is one of the major pathological changes. Due to the double blow of viral replication and immune response, hepatocytes are severely damaged and extensive punctate necrosis or focal necrosis occurs. Hepatocytes around these necrotic areas may show compensatory proliferation, but often cannot fully compensate for the loss of hepatocytes caused by necrosis [6].
4.3. Chronic hepatitis stage
If acute hepatitis is not treated in time or the treatment is incomplete, the condition may change to chronic hepatitis. In the chronic hepatitis stage, the pathological changes in the liver are mainly characterized by persistent hepatocyte inflammation, necrosis and fibrosis. These changes lead to progressive structural changes and gradual functional decline of the liver.
In the chronic hepatitis stage, hepatocyte inflammation and necrosis are one of the major pathologic changes. Due to the continuous replication of the virus in the liver and the persistence of the immune response, hepatocytes will be subject to long-term repeated damage and repair. This continuous process of injury and repair leads to chronic inflammation and necrosis of hepatocytes. At the same time, abnormal proliferation and regeneration of nodules may occur due to the repair process of hepatocytes, and these nodules may gradually evolve into cirrhosis or hepatocellular carcinoma.
4.4. Cirrhosis stage
As chronic hepatitis continues to develop, the pathologic changes in the liver may further deteriorate and progress to cirrhosis. Cirrhosis is a pathological state of severe structural alterations of the liver manifested by hardening of liver tissue, proliferation of fibrous tissue and pseudofollicle formation. In the cirrhotic stage, the normal structure and function of the liver are severely damaged, leading to a serious decline in liver function or even failure.
In the cirrhotic stage, the pathological changes of the liver are mainly characterized by fibrous tissue proliferation and pseudolobule formation. As hepatocytes are subjected to prolonged and repeated injury and repair during chronic hepatitis, a large amount of fibrous tissue proliferates and is deposited in the liver. These fibrous tissues gradually replace normal hepatocyte tissues and form pseudofollicular structures. The pseudofollicular structure loses the characteristics of normal liver functional units, leading to gradual decline or even failure of liver function [7].
Due to the highly infectious nature of HBV and the highly life-threatening nature of infection of the host, the clinical significance and applicability of this virus to almost all blood-borne hepatitis viruses have been developed.
4.5. The clinical significance of HBV
The significance of HBV is in evaluating disease and contagiousness, guiding treatment, evaluating the efficacy, and maternal infant blockade. Hepatitis B DNA detection can judge the virus replication. The higher the quantification level, the more infectious. It guides the treatment choice of hepatitis B patients, especially those with abnormal liver function and elevated HBV DNA. After treatment, evaluate the efficacy through DNA testing to assist doctors in adjusting treatment plans. For mothers with hepatitis B, quantitative detection is used to guide mother infant blocking measures [8].
5. Pathologic changes caused by hepatitis C virus (HCV) infection
5.1. Hepatocellular injury:
The process of HCV replication in hepatocytes leads to direct hepatocellular injury, which is manifested by morphological changes such as hepatocellular swelling, steatosis and necrosis. Hepatocellular necrosis is one of the major pathologic changes in the early stages of hepatitis C virus infection, which may subsequently trigger an inflammatory response.
Inflammatory response: Hepatocellular damage triggers the body's immune response, leading to an inflammatory response by infiltrating the liver with inflammatory cells (e.g., lymphocytes, monocytes, etc.). Inflammatory cell infiltration is often accompanied by hepatocellular edema and fibrous tissue proliferation, further exacerbating the pathological changes in the liver.
Fibrosis and cirrhosis: as the disease progresses, fibrous tissue proliferates in the liver, gradually replacing normal hepatocytes and forming fibrosis. When fibrosis reaches a certain level, it leads to irreversible changes in the structure and function of the liver, resulting in cirrhosis. Cirrhosis is an advanced pathologic manifestation of hepatitis C virus infection that may lead to a number of complications including liver failure and portal hypertension.
In addition, hepatitis C virus infection has some unique pathologic features, such as:
Lymphocytic infiltration in the syncytial area: in acute HCV infection, a large number of lymphocytic infiltration is often seen in the syncytial area, which may be related to the immune response of the body [9].
Bile duct damage and reduced number: HCV infection may lead to bile duct damage and a reduction in the number of interlobular bile ducts, a manifestation similar to autoimmune hepatitis.
Interfacial inflammation: In hepatitis C virus infection, interfacial inflammation is a common pathologic change that occurs mainly between the fusion zone of the liver and the liver parenchyma.
Hepatocellular steatosis: In hepatitis C virus infection, large vesicular steatosis may be present in hepatocytes, which may be caused by impaired fat metabolism due to hepatocellular injury.
5.2. Immune response infected with HCV
The immune response of HCV involves multiple aspects, and the following are some of the main immune response mechanisms: HCV direct killing: HCV replication interferes with the synthesis of large molecules in cells, increases the permeability of lysosomal membranes, and causes cellular lesions. HCV expression products (proteins) have toxic effects on liver cells, such as envelope proteins. Host immune factors: There are HCV specific cytotoxic lymphocytes (CD8+T cells) present in liver tissue, which can attack HCV infected liver cells. The cytokines secreted by CD4+Th cells after allergy can help clear HCV, but may also lead to immune damage [10]. Autoimmunity: HCV infected individuals often have autoimmune changes, such as bile duct pathological damage similar to autoimmune hepatitis. Various autoantibodies, such as antinuclear antibodies, smooth muscle antibodies, and single chain antibodies, can be detected in serum, indicating the involvement of autoimmune mechanisms. Adaptive immune response: CD8+T cells are a type of immune cell whose function is to recognize and kill invaders, including viruses. They find and bind a special shaped viral fragment called an antigenic epitope, allowing them to replicate and produce adaptive immune responses to protect the body from future infections. Interferon signaling pathway and interferon stimulating genes (ISG): During HCV infection, the interferon signaling pathway is activated and ISG is continuously expressed. This is a part of the body's immune response during HCV infection. Please note that the immune response of HCV is a complex process involving interactions between multiple cells and molecules. The above information is for reference only. If necessary, it is recommended to consult a professional doctor or consult relevant literature [11].
6. Conclusion
Hepatitis A, B and C viruses are transmitted by different mechanisms. Hepatitis A is transmitted through the gastrointestinal tract, while hepatitis B and C are transmitted through blood, body fluids, sexual contact and mother-to-child transmission. Pathologically, hepatitis A is mostly acute, while hepatitis B and C tend to become chronic, leading to cirrhosis and even liver cancer. Analyzing the mechanisms of transmission and pathological changes of hepatitis A, B and C viruses is essential for the prevention and control of viral transmission, accurate diagnosis and treatment, development of public health policies and public health education. Understanding this information can help reduce the prevalence of hepatitis, improve treatment outcomes, and promote public health. Among them, there is a lack of research and analysis on the structure of the viruses, and only three typical hepatitis viruses have been extracted, while the remaining two hepatitis viruses have not been mentioned. Future research will deepen our understanding of the hepatitis A, B and C viruses, promote innovations in vaccines and treatments, and provide stronger support for the prevention and treatment of hepatitis.
This paper provides an in-depth analysis of the transmission mechanisms of hepatitis A, B and C viruses, including the processes of virus invasion, replication and release. Taking the three different types of hepatitis A, B and C viruses as research subjects, this study explores in detail the pathological changes caused by the viruses to the liver, such as hepatocellular damage, inflammatory response, liver fibrosis, etc., which reveals the close relationship between the viruses and the health of the liver.
References
[1]. Xie R & Mao J 1989 Study on the Pathogenesis of Hepatitis A Virus Zhejiang Med 11 1 2
[2]. Ding H & Zhuang J 2007 Advances in Research on Hepatitis B Virus Int J Med Health 13 7 5
[3]. Yao Y & Zhang D 2002 Mechanisms of Hepatitis B Virus Infection Replication and Clearance Chin J Hepatol 10 5 3
[4]. Mi Y & Liang S 1998 Advances in Research on Hepatitis C Virus Int J Virol 5 4 105-107
[5]. Cullen J M & Lemon S M 2019 Comparative Pathology of Hepatitis A Virus and Hepatitis E Virus Infection Cold Spring Harb Perspect Med 4
[6]. Chisari F V Isogawa M & Wieland S F 2007 Iconography: Pathogenesis of Hepatitis B Virus Infection World J Gastroenterol 13 13 82-90
[7]. Yan R Q Su J J Huang D R et al 1996 Human Hepatitis B Virus and Hepatocellular Carcinoma I: Experimental Infection of Tree Shrews with Hepatitis B Virus J Cancer Res Clin Oncol 122 5 283-288
[8]. Pawlotsky J M 2004 Pathophysiology of Hepatitis C Virus Infection and Related Liver Disease Trends Microbiol 12 2 96-102
[9]. Corma-Gómez A Macías J Téllez F et al 2024 Liver Stiffness at the Time of Sustained Virological Response Predicts the Clinical Outcome in People Living With Human Immunodeficiency Virus and Hepatitis C Virus With Advanced Fibrosis Treated With Direct-Acting Antivirals Clin Infect Dis 9 9
[10]. Yu-La L 2008 An Investigation and Analysis of the Infection of Human Immunodeficiency Virus Hepatitis B Virus Hepatitis C Virus and Syphilis in Pregnant Women China Pract Med
[11]. Herrscher C Roingeard P & Blanchard E 2020 Hepatitis B Virus Entry into Cells Cells 9 6 1486
Cite this article
Liu,W. (2024). The transmission route of hepatitis A, B, and C virus and its pathological changes on the liver. Theoretical and Natural Science,48,15-21.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 2nd International Conference on Environmental Geoscience and Earth Ecology
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Xie R & Mao J 1989 Study on the Pathogenesis of Hepatitis A Virus Zhejiang Med 11 1 2
[2]. Ding H & Zhuang J 2007 Advances in Research on Hepatitis B Virus Int J Med Health 13 7 5
[3]. Yao Y & Zhang D 2002 Mechanisms of Hepatitis B Virus Infection Replication and Clearance Chin J Hepatol 10 5 3
[4]. Mi Y & Liang S 1998 Advances in Research on Hepatitis C Virus Int J Virol 5 4 105-107
[5]. Cullen J M & Lemon S M 2019 Comparative Pathology of Hepatitis A Virus and Hepatitis E Virus Infection Cold Spring Harb Perspect Med 4
[6]. Chisari F V Isogawa M & Wieland S F 2007 Iconography: Pathogenesis of Hepatitis B Virus Infection World J Gastroenterol 13 13 82-90
[7]. Yan R Q Su J J Huang D R et al 1996 Human Hepatitis B Virus and Hepatocellular Carcinoma I: Experimental Infection of Tree Shrews with Hepatitis B Virus J Cancer Res Clin Oncol 122 5 283-288
[8]. Pawlotsky J M 2004 Pathophysiology of Hepatitis C Virus Infection and Related Liver Disease Trends Microbiol 12 2 96-102
[9]. Corma-Gómez A Macías J Téllez F et al 2024 Liver Stiffness at the Time of Sustained Virological Response Predicts the Clinical Outcome in People Living With Human Immunodeficiency Virus and Hepatitis C Virus With Advanced Fibrosis Treated With Direct-Acting Antivirals Clin Infect Dis 9 9
[10]. Yu-La L 2008 An Investigation and Analysis of the Infection of Human Immunodeficiency Virus Hepatitis B Virus Hepatitis C Virus and Syphilis in Pregnant Women China Pract Med
[11]. Herrscher C Roingeard P & Blanchard E 2020 Hepatitis B Virus Entry into Cells Cells 9 6 1486