1. Introduction
ONFH is a type of aseptic necrosis, its course will last several years or longer, and most patients need to replace their total hip arthroplasties (THA) at the advanced stage. AVN’s pathogenesis can be classified as two kinds:traumatic pathogeny and non-traumatic pathogeny. Common non-traumatic pathogenies including using glucocorticoids, intemperance and some immune diseases or blood diseases. Traumatic pathogeny usually are several special kinds fracture.
For these two kinds of ONFH, there is not many difference for therapeutic schedule. The non- operative treatments involving extracorporeal shock wave, medical treatment and hyperbaric oxygen therapy, while operative therapies cover core decompression (CD), steam cell treatment, bone-grafting, tantalum rods, osteotomy and THA. But some methods may only be helpful for early patients. Comparing with the 20century, doctor and patient has paid more attention to early diagnosis and different therapeutic methods. Even though these therapies methods only can control the course of disease, they can improve prognosis in patients and delay the time to receive THA. Although ONFH has caught people’s attention for hundreds of years, there is still many questions haven’t been solved: how can the high-risk group prevent it? how to reduce its treatment cost? is nowadays’ therapeutic schedule really useful?
This article will mainly focus on high-risk factors, pathological diagnosis and stage, different treatment methods and sequelae.
2. High-risk factors
2.1. Traumatic pathogeny
2.1.1. Femoral neck freactures. The most common reason for traumatic pathogeny is fractures happening in the sub-capital region of the femoral neck [1]. According to fracture classification, it can be divided into Graden 1, Graden 2, Garden 3, Garden 4 four types. Among them Garden 3 and Garden types are more easily to get ONFH. The blood supply to the femoral head will be limited by injuries in this region, as it damages the anastomosis between the lateral epiphyseal vessels[1].According to a research, displaced fractures can make the risk of ONFH grown increase 7.1%,comparing with undisplaced freactures [1].Aim to recover the vascular supply to the femoral head and its functionality, doctors tend to choose femoral neck fixation and try to retain original joint. However, using some kinds of metal screws may lead to insufficiency of blood supply, makes a reverse effect.
2.1.2. Legg-Calvé-Perthes disease (LCPD). LCPD is a kind of complex disease affecting the epiphysis of the femoral head in children [2]. It is symbolized by bilateral or unilateral necrosis of the femoral head, limit the joint ROM of hip, this problem, specific gait and pain are the most common reason prompting children to see doctors [2]. Considered as an osteochondrosis in the past, now it is recognized as an idiopathic ONFH mainly happened in children and teenager. It is set to be between 0.4~ 29.0/100000 children under 15, mostly happened in children 4-8 years old, while the morbidity of male is four times higher than female, however, for all ONFH patients, male is only one time more than female [2].
2.2. Non-traumatic pathogeny
The common reasons for non-traumatic pathogeny including glucocorticoid, Intemperance, hyperlipidemia, sickle cell disease (SCD), systemic lupus erythematosus and Gaucher disease. For non-traumatic ONFH, it doesn’t have an explicit pathogenesis till now. But affected blood supply through different ways have has been approved.
2.2.1. Glucocorticoid. In China, glucocorticoid has been abused for several decades, it used be thought as a medicine can treat diseases from simple flue to SARS, and now it has become the second source of increasing number for ONFH. According to a research involved 1884 ONFH patients from China, there were 495 induced by steroid and 685 were Glucocorticoids can affect lipid metabolism [3]. As is known to all, corticosteroids can induce osteoporosis from several ways, including osteocyte apoptosis, inhibit osteoblastogenesis and promote osteoblast. At the same time, they also will enhance lifespan, maturation, and osteoclast differentiation. That is why glucocorticoid can cause chaemic necrosis of the bone tissue in the vascular supply area. It is reported that Japanese peak age for non-traumatic ONFH is 40, and using steroid is the most common reason (51%) [4].
2.2.2. Intemperance. Some researches show that ethanol will inhibit osteoblast proliferation and differentiation, accelerate osteoblast apoptosis. Meanwhile, it may induce precursors to adipogenic differentiation, which leads to the imbalance of bone homeostasis [3]. For example, bone marrow-derived mesenchymal stem cells (BM-MSCs) play a crucial part in bone formation, but they are vulnerable to ethanol (EtOH).About 31% patients is habitual alcohol use[3]. In the meantime, ethanol can increase intraosseous pressureblood, cause lipid metabolism disorder and promote fat production, all of these together will end up to the obstruction of blood supply in the femoral head.
2.2.3. Hyperlipemia. According to a retrospective study about how can the abnormal lipids metabolism induce AVNFH, there are several main pathogenesis. Hyperlipemia will damage vascular endothelial cells, providing conditions for generating thrombus; meanwhile, this illness will reduce the ability to compound nitric oxide (NO) of vascular endothelial cells, causes disfunction of vascular contraction and relaxation, finally influences bone microcirculation [5].At the same time, hyperlipemia can create fat embolism in the peripheral blood, obstructing bone microvascular, increasing the intraosseous pressure, and makes the dysfunction of bone microcirculation exacerbated ulteriorly[5].Besides, some other abnormities in the femoral head will increasing bone marrow microcirculation pressure, such as fat accumulation, fatty marrow and adipocyte hypertrophy, finally cause hypoxia, ischemia, edema observed and metabolic disorders in bone marrow tissue. These problems increase secondary intracranial pressure, make original ischemia and anoxia more seriously. All of these together contribute a vicious circle, leading to consequences like bone necrosis or bone dystrophy in the end [5]. This study also has a statistically significant discovery (P < 0.05): after the reduction of femoral neck fracture, patients with hyperlipemia are much easier to experience AVNFH than normal patients [5].
2.2.4. Sickle cell disease (SCD). SCD is a kind of multisystem disease which affect the kidneys, brain, bones, lungs and cardiovascular systems. This is a genetic hemoglobinopathy, inherited as an autosomal recessive trait with difficulty in hemoglobin synthesis. The symbol of this disease is the distortion of red blood cells (RBCs) due to deoxygenation, leading to both extracellular and intracellular hemolysis, cause erythrocyte rigidity and vaso-occlusion. And finally, organs including bone will be progressively damaged because of the recurrent episodes of inflammation and vaso-occlusion. Over 30% of SCD patients will experience osteonecrosis, and half of them happened in femoral head region [6]. Considering about the population of SCD patients and their growing life expectancy, ONFH risk shouldn’t be ignore.
2.2.5. Systemic lupus erythematosus (SLE). SLE is an autoimmune disease will influence multisystem and multiple organs. Osteonecrosis is one of the most common complications for SLE, and femoral head is the easiest to get involved. For how can SLE cause osteonecrosis, several hypotheses have been mentioned, including SLE itself, using Glucocorticoid and other medicine [6]. Between them, only using Glucocorticoid this reason has already got clinical verifications [6]. It can be proved by a clinical experiment. According to a study that divided 127 patients into two group, one received Glucocorticoid every day, and another group received every two days [7]. Finally, researchers found that patients without AVN are more frequently to use corticosteroid once in two days [7].
2.2.6. Gaucher disease (GD). GD is a genetic, rare, lysosomal disease can cause dysfunction and lipid accumulation in multiple organs. Skeleton involvement (usually include hip joint) is one of the most common problems for GD, and this is the main reason for disability, pain an reduce of ADL scores [8].Be exposured to excess bioactive glycosphingolipids seems will influence hematopoiesis and the balance of osteoclast and osteoblast numbers and activity. Several problems like cortical bone thinning, osteolytic lesions, disordered trabecular and cortical bone modeling, and fragility fractures, can be caused by the unbalance between bone formation and breakdown. [8]. According to a study involved 2004 patients from 1991 to 2000, between 76% and 94% of GD type1 patients has at least one osteonecrosis region [9]. Considering about their age of onset, probably some patients need to face ONFH even before adult.
2.2.7. Other diseases. Some other diseases like leukemia, autoimmune disease and organ grafting also have a higher risk to get ONFH. However, this situation mainly caused by Glucocorticoid therapy regimen instead of illnesses themselves.
3. Pathological diagnosis and stage
The first ARCO (the Committee on Nomenclature and Staging of the Association Research Circulation Osseous) staging system for ONFH was set up in1991 and revised it in 2019.The 2019 edition made two changes: stage 0 was deleted and stage III was divided into early stage (IIIA) and late stage (IIIB)two parts [9].
The location and size of necrosis both can indicate the long-term progression of ONFH, that’s why they are recognized as the major determinant in the therapy [9].
The widely used classification systems are Steinberg classification and Japanese Investigation Committee (JIC) classification. The first one categorized the extent of involvement into 3 subsets: mild degree (< 15% of articular surface or head affected), moderate degree (15–30%), and severe degree (> 30%) [10].The second divided ONFH into 4 kinds: A, B, C1 and C2. Type A lesion < medial 1/3 of the weight-bearing portion; type B lesion < medial 2/3; both type C1and C2 lesion > medial 2/3 but C1 not extending laterally to the acetabular edge. The prevalence of collapse was < 10% in the type A, 40% in the type B, 80% in type the C1, and > 90% in the type C2 (as shown in figure1). The classification is 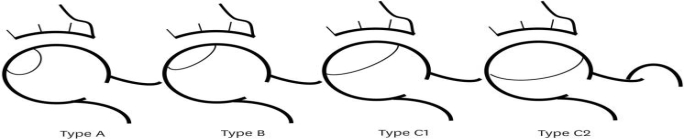 based on the central coronal section of the femoral head on a T1-weighted MRI.
based on the central coronal section of the femoral head on a T1-weighted MRI.
Figure 1. Japanese Investigation Committee (JIC) classification [10].
4. Common treatment
Common treatments include non-surgical and surgical therapy. Before deciding the therapeutic schedule, stage of methods, age, underlying disease all should be mentioned as they can affect the prognosis. Usually non-surgical therapies including drug, extracorporeal shock wave, Hyperbaric oxygen (HBO) therapy and long-term observation; surgical therapies including core decompression, bone grafting, cellular therapy, osteotomies and THA. Some methods are doubtful about their effectiveness even though they have been wildly used around the world, and doctors in different regions have their own deviation about the therapeutic schedules.
4.1. Non-surgical therapies
4.1.1. Pharmacological treatments. Most wildly used drugs are bisphosphonates, iloprost, enoxaparin, statins and acetylsalicylic acid. However, there aren’t enough research about their effective rate and most have adverse reaction report.
Bisphosphonates is a class of drug can reduce osteoclast activity, considered Alendronate has some potential protective effects of in ONFH early stage. A research using alendronate treat rat model (n=12) show it some function for the early stage of ONFH [10]. However, aisphosphonate didn’t prevent femoral head collapse, improve Harris hip score, and reduce the rate of THA according to a series of human researches and it has established adverse effect like esophageal or gastric irritation [11].
Other medicines have similar problem. According to recently 10 years researches published in Pubmed, these medicines didn’t have enough clinical manifestation to prove their effectiveness, especially for patients at middle or advanced stage. As a result, doctors only use them as adjuvant therapy and need to monitor adverse reaction strictly.
4.1.2. Extracorporeal shock wave. Extracorporeal shock wave (ESWT) has been widely used since the end of the 20th Century. It has been reported that ESWT can lower pain degree, improving function and survival time of the hip.
A study involving 39 consecutive patients (53 hips) underwent ESWT lasting 18 months can improve this idea [12]. In this research, the Harris hip score improved significantly, before receiving ESWT, it is 77.4, grow up to 86.9 points finally (p < 0.001). At the same time, the mean VAS score signally decreased for 1.6 point (p < 0.001) [12]. The therapeutic effect for ARCO1 and ARCO2 is obviously better that that for other stages. However, most of the research about ESWT only include less than 100 hips, probably this method needs more clinical data in the future.
4.1.3. Hyperbaric oxygen therapy (HBOT). HBOT has many effects including enhance the reactive nitrogen species (RNS) and also the reactive oxygen species (ROS) production, modulating inflammatory and response promoting cell growth. That is how does HBOT help to improve vascularization and the survival rate of ischemic tissue. Due to its high security and special effect for cardiovascular system, it has been widely used to treat cerebral infarction and myocardial infarction. Now it is also considered as an economical and effective way to treat early ONFH.
According to a systematic review for evidence-Supported HBOT in ONFH, this method can significantly bring improvement to patients’ symptoms and quality of life. This article mentions 10 studies (n control =353; n HBO-treated cases=368), 8 of them was conducted on Asian population [13]. Subgroup analyses suggested that the therapy was statistically significant in the Asian (OR = 3.53, 95% CI (1.87, 6.64), p < 0.00001), while the effect in other area is not significant, may due to number is not enough (OR = 7.41, (0.73, 75.71), p = 0.09) [13]. Meanwhile, HBOT can hardly cause adverse reaction and is economical, all these advantages let it become a popular choice.
4.1.4. Long-term observation. This method is only suitable for some suspected case and high-risk group with no clinical symptom. Long-term observation usually will last 1 or 2 years, during this period, patients need to take X-ray regularly, and none can make sure whether the state of illness will get worse or not.
4.2. Surgical therapies
4.2.1. Core decompression. CD have some main curative effects. It can decrease intraosseous pressure, improve the blood supply for femoral head and alleviate bone marrow edema. These made it widely used among early ONFH patients. However, the surgery result can be influenced by many elements, including male sex, etiology, whether the patient has a seated occupation problem or not, age, hemoglobin level, disease duration and the combined necrosis angle [14]. For example, it is reported that the survival rate of hips therapied by CD was 50% (about 6 years of follow-up period), while the survival rate is 30% higher for patients at Ficat stage I-II ONFH [14].
However, CD therapy also has some terrible influence on the later treatment. It is suggested that if the CD surgery fail, patients’ risk to experience periprosthetic femoral fractures will grow up to about 4-fold. The possible reason for failure is the filling of the decompression tunnel of the femoral neck with sclerotic bone, and result in the increasing of bone fragility and the reduce of the bone strength [14]. All of these bring huge problem to further treatment.
4.2.2. Bone grafting. Bone grafting is mainly divided into four kinds: bone graft combined with bone marrow graft (BG+BM), autologous bone graft (ABG), free vascular bone graft and biomaterial bone graft (BBG). This surgery recovers the biological stability, promoting the repair of necrotic areas, preserving the femoral head and a majority of the hip function indirectly, which is really helpful.
4.2.3. Cellular therapy. This therapy has been used to treat ONFH for over 20 years, and gained a fine curative effect.It including the combining stem cells with CD, the autologous bone graft, the platelet-rich plasma and supporting biomaterial implantation. According to a meta-analysis involving 13 RCTs (n=619), stem cells could observably postpone the progression of disease, increase the long-term survival rate of hip. It will effectively reduce the probability of collapse of femoral head (no less than 5 years) (RR, 0.37; 95% CI, 0.28~0.49) and THA (more than 3 years) (0.32; 0.23~0.44), both of them have statistical significance and is more beneficial for patients aged ≤40 [15].
Till now, the mechanism is still unclear. Stem cells can self-renew and proliferation, and also secrete multiple biological factors, these functions probably help it to treat ONFH. Meanwhile, due to the age may effects the cell function, older people may not gain ideal curative effect.
4.2.4. Osteotomies. Osteotomies is a surgery using to preserve joint for patients, mainly used in Japan, with moving necrotic area away from the loading surface. The adjustment is triaxial, involving the flexion‐extension, and anterior–posterior rotation, and the proximal femoral osteotomy can be divided into two parts: intertrochanteric curved osteotomy and transtrochanteric rotational osteotomy (preferred choice), they are both developed in Japan [16]. However, this surgery takes a much longer convalescence than CD, and make it more difficult for patients to receive THA.
4.2.5. Total hip arthroplasty (THA). THA has been considered as the optimal therapy for final‐stage ONFH since the 20th century. Only patients with below conditions can take this surgery as it can’t be reversed: pain could not be controlled by other treatments, collapsed femoral head, ONFH with moderate-severe persistent pain [17].
In the past, this surgery usually taken for people around 75, as the service life of the prosthesis is about 10 years. But the newest prosthesis can be used for over 25 years and cause less complications, that is why younger patients consider about receiving this surgery.
However, there may be some complication after THA, involving infection, periprosthetic fracture, dislocation, fracture of the prosthesis, wear of the implantation materials and loosing [17].
5. Conclusion
ONFH has been studied for about one hundred years. Although the etiology and pathogenesis of the disease have been understood to a certain extent, further research is still needed to solve its unresolved problems. For treatment, there are still many problems about its therapeutic schedule. On the one hand, some traditional methods like medicine therapy and steotomies’ effectiveness didn’t have enough evidence; on the other hand, HBO therapy is really economical and convenience, but its studies mainly taken in Asian. CD, BG and cellular therapy have good reverberations, but they all cost tens of thousands of dollars, requires a much longer convalescence than other methods. Meanwhile, before taking invasive therapies like CD and THA, doctors and patients should think twice. There is a risk behind them, isn’t there any other way and does the patients really can bear them? Treatment guidelines shouldn’t be indiscriminately imitated as each methods have its own problem, patients and doctors should work together to find a suitably personal plan.
References
[1]. Konarski W, Poboży T, Śliwc ,zyński A, Kotela I, Krakowiak J, Hordowicz M, Kotela A. Avascular Necrosis of Femoral Head-Overview and Current State of the Art. Int J Environ Res Public Health. 2022 Jun 15;19(12):7348. doi: 10.3390/ijerph19127348. PMID: 35742595; PMCID: PMC9223442.
[2]. Pavone V, Chisari E, Vescio A, Lizzio C, Sessa G, Testa G. Aetiology of Legg-Calvé-Perthes disease: A systematic review. World J Orthop. 2019 Mar 18;10(3):145-165. doi: 10.5312/wjo.v10.i3.145. PMID: 30918798; PMCID: PMC6429000.
[3]. Tan B, Li W, Zeng P, Guo H, Huang Z, Fu F, Gao H, Wang R, Chen W. Epidemiological Study Based on China Osteonecrosis of the Femoral Head Database. Orthop Surg. 2021 Feb;13(1):153-160. doi: 10.1111/os.12857. Epub 2020 Dec 21. PMID: 33347709; PMCID: PMC7862166.
[4]. Fukushima W, Fujioka M, Kubo T, Tamakoshi A, Nagai M, Hirota Y. Nationwide epidemiologic survey of idiopathic osteonecrosis of the femoral head. Clin Orthop Relat Res. 2010 Oct;468(10):2715-24. doi: 10.1007/s11999-010-1292-x. Epub 2010 Mar 12. PMID: 20224959; PMCID: PMC2939331.
[5]. Zeng X, Zhan K, Zhang L, Zeng D, Yu W, Zhang X, Zhao M, Lai Z, Chen R. The impact of high total cholesterol and high low-density lipoprotein on avascular necrosis of the femoral head in low-energy femoral neck fractures. J Orthop Surg Res. 2017 Feb 17;12(1):30. doi: 10.1186/s13018-017-0532-0. PMID: 28212664; PMCID: PMC5316144.
[6]. Xu Y, Chen S, Cai Q, Zhang C. [Analysis of incidence and clinical characteristics of osteonecrosis of femoral head in patients with systemic lupus erythematosus treated with glucocorticoid: A descriptive study based on a prospective cohort]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2023 May 15;37(5):605-614. Chinese. doi: 10.7507/1002-1892.202302026. PMID: 37190840; PMCID: PMC10196977..
[7]. Doğan I, Kalyoncu U, Kiliç L, Akdoğan A, Karadağ Ö, Kiraz S, Bilgen ŞA, Ertenli I. Avascular necrosis less frequently found in systemic lupus erythematosus patients with the use of alternate day corticosteroid. Turk J Med Sci. 2020 Feb 13;50(1):219-224. doi: 10.3906/sag-1908-182. PMID: 31905492; PMCID: PMC7080371.
[8]. Hughes D, Mikosch P, Belmatoug N, Carubbi F, Cox T, Goker-Alpan O, Kindmark A, Mistry P, Poll L, Weinreb N, Deegan P. Gaucher Disease in Bone: From Pathophysiology to Practice. J Bone Miner Res. 2019 Jun;34(6):996-1013. doi: 10.1002/jbmr.3734. Epub 2019 Jun 24. PMID: 31233632; PMCID: PMC6852006.
[9]. Hines JT, Jo WL, Cui Q, Mont MA, Koo KH, Cheng EY, Goodman SB, Ha YC, Hernigou P, Jones LC, Kim SY, Sakai T, Sugano N, Yamamoto T, Lee MS, Zhao D, Drescher W, Kim TY, Lee YK, Yoon BH, Baek SH, Ando W, Kim HS, Park JW. Osteonecrosis of the Femoral Head: an Updated Review of ARCO on Pathogenesis, Staging and Treatment. J Korean Med Sci. 2021 Jun 21;36(24): e177. doi: 10.3346/jkms.2021.36.e177. PMID: 34155839; PMCID: PMC8216992.
[10]. Rong K, Li X, Jiang W, Wu X, Xia Q, Chen J, Yin X. Alendronate Alleviated Femoral Head Necrosis and Upregulated BMP2/EIF2AK3/EIF2A/ATF4 Pathway in Liquid Nitrogen Treated Rats. Drug Des Devel Ther. 2021 Apr 23;15:1717-1724. doi: 10.2147/DDDT.S286610. PMID: 33935494; PMCID: PMC8079257.
[11]. Lee YJ, Cui Q, Koo KH. Is There a Role of Pharmacological Treatments in the Prevention or Treatment of Osteonecrosis of the Femoral Head?: A Systematic Review. J Bone Metab. 2019 Feb;26(1):13-18. doi: 10.11005/jbm.2019.26.1.13. Epub 2019 Feb 28. PMID: 30899719; PMCID: PMC6416144.
[12]. Xie K, Mao Y, Qu X, Dai K, Jia Q, Zhu Z, Yan M. High-energy extracorporeal shock wave therapy for nontraumatic osteonecrosis of the femoral head. J Orthop Surg Res. 2018 Feb 2;13(1):25. doi: 10.1186/s13018-017-0705-x. PMID: 29394948; PMCID: PMC5797389.
[13]. Paderno E, Zanon V, Vezzani G, Giacon TA, Bernasek TL, Camporesi EM, Bosco G. Evidence-Supported HBO Therapy in Femoral Head Necrosis: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2021 Mar 12;18(6):2888. doi: 10.3390/ijerph18062888. PMID: 33808951; PMCID: PMC7999152.
[14]. Wei C, Yang M, Chu K, Huo J, Chen X, Liu B, Li H. The indications for core decompression surgery in patients with ARCO stage I-II osteonecrosis of the femoral head: a new, comprehensive prediction system. BMC Musculoskelet Disord. 2023 Mar 30;24(1):242. doi: 10.1186/s12891-023-06321-0. PMID: 36997998; PMCID: PMC10061868.
[15]. Mao L, Jiang P, Lei X, Ni C, Zhang Y, Zhang B, Zheng Q, Li D. Efficacy and safety of stem cell therapy for the early-stage osteonecrosis of femoral head: a systematic review and meta-analysis of randomized controlled trials. Stem Cell Res Ther. 2020 Oct 19;11(1):445. doi: 10.1186/s13287-020-01956-5. PMID: 33076978; PMCID: PMC7574494.
[16]. Kuroda Y, Okuzu Y, Kawai T, Goto K, Matsuda S. Difference in Therapeutic Strategies for Joint-Preserving Surgery for Non-Traumatic Osteonecrosis of the Femoral Head between the United States and Japan: A Review of the Literature. Orthop Surg. 2021 May;13(3):742-748. doi: 10.1111/os.12979. Epub 2021 Apr 5. PMID: 33821555; PMCID: PMC8126904.
[17]. Yang M, Li X, Chu K, Li Z, Wei C, Yao M, Li H. Comparison of Outcomes Following Total Hip Arthroplasty Between Patients Diagnosed with Association Research Circulation Osseous (ARCO) Stage III and Stage IV Osteonecrosis of the Femoral Head: A Retrospective Study of 302 Patients. Med Sci Monit. 2023 Jan 17;29:e938991. doi: 10.12659/MSM.938991. PMID: 36647319; PMCID: PMC9864440.
Cite this article
He,Q. (2024). High risk factors and exsit therapies for Osteonecrosis of the Femoral Head (ONFH). Theoretical and Natural Science,50,16-23.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of ICBioMed 2024 Workshop: Workshop on Intelligent Medical Data Analysis for Precision Medicine
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Konarski W, Poboży T, Śliwc ,zyński A, Kotela I, Krakowiak J, Hordowicz M, Kotela A. Avascular Necrosis of Femoral Head-Overview and Current State of the Art. Int J Environ Res Public Health. 2022 Jun 15;19(12):7348. doi: 10.3390/ijerph19127348. PMID: 35742595; PMCID: PMC9223442.
[2]. Pavone V, Chisari E, Vescio A, Lizzio C, Sessa G, Testa G. Aetiology of Legg-Calvé-Perthes disease: A systematic review. World J Orthop. 2019 Mar 18;10(3):145-165. doi: 10.5312/wjo.v10.i3.145. PMID: 30918798; PMCID: PMC6429000.
[3]. Tan B, Li W, Zeng P, Guo H, Huang Z, Fu F, Gao H, Wang R, Chen W. Epidemiological Study Based on China Osteonecrosis of the Femoral Head Database. Orthop Surg. 2021 Feb;13(1):153-160. doi: 10.1111/os.12857. Epub 2020 Dec 21. PMID: 33347709; PMCID: PMC7862166.
[4]. Fukushima W, Fujioka M, Kubo T, Tamakoshi A, Nagai M, Hirota Y. Nationwide epidemiologic survey of idiopathic osteonecrosis of the femoral head. Clin Orthop Relat Res. 2010 Oct;468(10):2715-24. doi: 10.1007/s11999-010-1292-x. Epub 2010 Mar 12. PMID: 20224959; PMCID: PMC2939331.
[5]. Zeng X, Zhan K, Zhang L, Zeng D, Yu W, Zhang X, Zhao M, Lai Z, Chen R. The impact of high total cholesterol and high low-density lipoprotein on avascular necrosis of the femoral head in low-energy femoral neck fractures. J Orthop Surg Res. 2017 Feb 17;12(1):30. doi: 10.1186/s13018-017-0532-0. PMID: 28212664; PMCID: PMC5316144.
[6]. Xu Y, Chen S, Cai Q, Zhang C. [Analysis of incidence and clinical characteristics of osteonecrosis of femoral head in patients with systemic lupus erythematosus treated with glucocorticoid: A descriptive study based on a prospective cohort]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2023 May 15;37(5):605-614. Chinese. doi: 10.7507/1002-1892.202302026. PMID: 37190840; PMCID: PMC10196977..
[7]. Doğan I, Kalyoncu U, Kiliç L, Akdoğan A, Karadağ Ö, Kiraz S, Bilgen ŞA, Ertenli I. Avascular necrosis less frequently found in systemic lupus erythematosus patients with the use of alternate day corticosteroid. Turk J Med Sci. 2020 Feb 13;50(1):219-224. doi: 10.3906/sag-1908-182. PMID: 31905492; PMCID: PMC7080371.
[8]. Hughes D, Mikosch P, Belmatoug N, Carubbi F, Cox T, Goker-Alpan O, Kindmark A, Mistry P, Poll L, Weinreb N, Deegan P. Gaucher Disease in Bone: From Pathophysiology to Practice. J Bone Miner Res. 2019 Jun;34(6):996-1013. doi: 10.1002/jbmr.3734. Epub 2019 Jun 24. PMID: 31233632; PMCID: PMC6852006.
[9]. Hines JT, Jo WL, Cui Q, Mont MA, Koo KH, Cheng EY, Goodman SB, Ha YC, Hernigou P, Jones LC, Kim SY, Sakai T, Sugano N, Yamamoto T, Lee MS, Zhao D, Drescher W, Kim TY, Lee YK, Yoon BH, Baek SH, Ando W, Kim HS, Park JW. Osteonecrosis of the Femoral Head: an Updated Review of ARCO on Pathogenesis, Staging and Treatment. J Korean Med Sci. 2021 Jun 21;36(24): e177. doi: 10.3346/jkms.2021.36.e177. PMID: 34155839; PMCID: PMC8216992.
[10]. Rong K, Li X, Jiang W, Wu X, Xia Q, Chen J, Yin X. Alendronate Alleviated Femoral Head Necrosis and Upregulated BMP2/EIF2AK3/EIF2A/ATF4 Pathway in Liquid Nitrogen Treated Rats. Drug Des Devel Ther. 2021 Apr 23;15:1717-1724. doi: 10.2147/DDDT.S286610. PMID: 33935494; PMCID: PMC8079257.
[11]. Lee YJ, Cui Q, Koo KH. Is There a Role of Pharmacological Treatments in the Prevention or Treatment of Osteonecrosis of the Femoral Head?: A Systematic Review. J Bone Metab. 2019 Feb;26(1):13-18. doi: 10.11005/jbm.2019.26.1.13. Epub 2019 Feb 28. PMID: 30899719; PMCID: PMC6416144.
[12]. Xie K, Mao Y, Qu X, Dai K, Jia Q, Zhu Z, Yan M. High-energy extracorporeal shock wave therapy for nontraumatic osteonecrosis of the femoral head. J Orthop Surg Res. 2018 Feb 2;13(1):25. doi: 10.1186/s13018-017-0705-x. PMID: 29394948; PMCID: PMC5797389.
[13]. Paderno E, Zanon V, Vezzani G, Giacon TA, Bernasek TL, Camporesi EM, Bosco G. Evidence-Supported HBO Therapy in Femoral Head Necrosis: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2021 Mar 12;18(6):2888. doi: 10.3390/ijerph18062888. PMID: 33808951; PMCID: PMC7999152.
[14]. Wei C, Yang M, Chu K, Huo J, Chen X, Liu B, Li H. The indications for core decompression surgery in patients with ARCO stage I-II osteonecrosis of the femoral head: a new, comprehensive prediction system. BMC Musculoskelet Disord. 2023 Mar 30;24(1):242. doi: 10.1186/s12891-023-06321-0. PMID: 36997998; PMCID: PMC10061868.
[15]. Mao L, Jiang P, Lei X, Ni C, Zhang Y, Zhang B, Zheng Q, Li D. Efficacy and safety of stem cell therapy for the early-stage osteonecrosis of femoral head: a systematic review and meta-analysis of randomized controlled trials. Stem Cell Res Ther. 2020 Oct 19;11(1):445. doi: 10.1186/s13287-020-01956-5. PMID: 33076978; PMCID: PMC7574494.
[16]. Kuroda Y, Okuzu Y, Kawai T, Goto K, Matsuda S. Difference in Therapeutic Strategies for Joint-Preserving Surgery for Non-Traumatic Osteonecrosis of the Femoral Head between the United States and Japan: A Review of the Literature. Orthop Surg. 2021 May;13(3):742-748. doi: 10.1111/os.12979. Epub 2021 Apr 5. PMID: 33821555; PMCID: PMC8126904.
[17]. Yang M, Li X, Chu K, Li Z, Wei C, Yao M, Li H. Comparison of Outcomes Following Total Hip Arthroplasty Between Patients Diagnosed with Association Research Circulation Osseous (ARCO) Stage III and Stage IV Osteonecrosis of the Femoral Head: A Retrospective Study of 302 Patients. Med Sci Monit. 2023 Jan 17;29:e938991. doi: 10.12659/MSM.938991. PMID: 36647319; PMCID: PMC9864440.