1. Introduction
Chronic illnesses, particularly CVD, are now the main cause of mortality in both industrialized and emerging nations. CVD includes heart failure (HF), peripheral arterial disease (PAD), coronary heart disease (CHD), stroke, and other illnesses related to the heart. CVD is currently one of the main factors contributing to high death rates worldwide. By 2030, it's predicted that CVD will account for 22.2 million annual fatalities [1]. For instance, 40% of fatalities in China are due to CVD [2], and between 1990 and 2016, the incidence of CVD rose by 14.7% [2]. In the US in 2019, there was a myocardial infarction every 40 seconds and a CVD death every 37 seconds [1]. According to estimates, the yearly overall cost of CVD in the US is $351.2 billion [1].
Numerous risk factors, including obesity, diabetes, hypertension, smoking, and others, are linked to the development of CVD. Research on SB as a modifiable risk factor for CVD has gradually become more evident [3]. SB is defined as having a low energy expenditure and being sedentary or lying down for most of their waking hours. Excessive SB has been linked to CVD risk in more recent cohort studies and meta-analyses. Research has shown a statistically significant increase in the risk of CVD when people engage in SB for more than seven hours per day [1]. Nevertheless, the exact mechanism by which SB causes CVD remains unclear.
There is still controversy about how to reduce the risk of CVD due to SB. PA is classified into numerous exercise groups according to movement pattern, intensity, and duration. It is described as "any physical movement in which the contraction of skeletal muscles causes the expenditure of energy" [2]. PA is gaining ground as a reliable intervention to reduce the incidence of CVD. Longer durations of diverse intensities of PA are associated with a decrease in the incidence of CVD. On the other hand, not much study has been done about the safety and effectiveness of PA treatment. To create a stronger theoretical foundation for the prevention and treatment of CVD in the future, the purpose of this research is to investigate the relationship between CVD and SB as well as the influence of PA on CVD.
2. Epidemiology of cardiovascular disease due to sedentary behavior
In a time of advanced therapeutic techniques, several risk factors can account for the high mortality rate from CVD, including SB. Over 25% of people in a pooled investigation with 1.9 million participants had inadequate PA, with women being more likely to exhibit this condition [4]. Because physical inactivity (PI) affects more than one-third of the population, it has been estimated that leading a sedentary lifestyle kills more people globally than smoking [4].
It has been demonstrated that high SB levels increase the risk of CVD morbidity and death. A study conducted in several countries (China, America, Canada, etc.) found that the average sedentary time for adults between the ages of 18 and 66 was 8.7 hours per day [5]. SB is also very common in Western countries. Adults are sedentary for an average of 9-11 hours a day [5]. Persons with chronic SB had a 34% higher risk of CVD than persons without SB, according to a meta-analysis involving 75,075 samples [5]. An original survey of CVD in Mexico found that the elevated incidence of CVD could be attributed to a 44% increase in PI among adults [6]. A study that included 143,180 individuals found that being physically active and being sedentary for more than eight hours a day increased the risk of stroke [6]. PI and SB among older women in the U.S. are expected to increase to 79 million by 2500 [6]. A study of 80,982 women between the ages of 50 and 79 found that being SB led to a significantly increased risk of hospitalization for HF [6]. A study of 373,026 Europeans with no history of CHD or stroke found that the lower the sedentary television viewing time the lower the incidence of CHD [1].
Studies indicate that the detrimental impacts of SB are more noticeable in groups that are not active [3]. The slope of CVD risk with increasing SB was shown to be significantly correlated with a curvilinear dose-response rise. Several researchers have observed a notable linear dose-response connection [7] between incident CVD fatalities and nonfatal events and TV viewing. Research indicates that there are different correlations between SB and CVD mortality according to how intense a person's moderate-to-vigorous PA (MVPA) is [3]. The impact of SB on CVD mortality is greater in those with low MVPA levels [3]. A harmonized meta-analysis by Ekelund et al. utilizing individual-level data from over a million individuals revealed that the associations between SB and CVD mortality were weakened by rising levels of MVPA [7]. Therefore, every adult should incorporate MVPA into their lifestyle, especially if they spend a significant amount of their time sitting down. The necessity to customize and individualize lifestyle suggestions for each person to maximize their benefits is further demonstrated by these results, which will also have a stronger effect on population health.
3. Influence
Numerous studies on the etiology and risk factors of CVD have been conducted since the mid-1900s. Hypertension, dyslipidemia, smoking, PI, poor diet, obesity, type 2 diabetes mellitus, EF, and inflammation are all risk factors for CVD. SB has a significant influence on some known CVD risk factors. This paper will focus on the discussion around BL, BP, BG, obesity, inflammation, and EF.
3.1. Blood lipids, blood pressure, blood glucose
Prolonged sitting decreases the physiological activity of muscle and chronic muscle fiber contraction significantly reduces the activity of lipoprotein lipase in skeletal muscle. Reduced lipoprotein lipase activity can lower high-density lipoprotein levels, decrease tissue cell absorption of triacylglycerol, and raise the risk of dyslipidemia [8].
Prolonged sitting may also lead to the disturbance of the human renal - angiotensin-aldosterone system, the dysfunction of the sympathetic-parasympathetic nerve, the destruction of endothelial cell function, and eventually lead to increased BP, and then induce CVD [8].
Sitting all the time reduced insulin sensitivity in the skeletal muscles exacerbated BG metabolism problems and encouraged ectopic storage and fat formation, all of which contributed to increased insulin resistance. The pancreas and liver have persistent ectopic fat as peripheral insulin resistance worsens. The build-up aided in the development of metabolic syndrome, and islet beta cell activity steadily declined [9]. At the same time, the phenomenon of excessive intake of energy may occur in video sedentary, which turns the energy balance to excess energy, and eventually leads to the rise of postprandial BG [9]. Meanwhile, most people watch TV in the evening following their major meal. Continuous SB may increase the amount of time spent viewing TV and raise the metabolic risk for CVD by causing recurrent negative effects of postprandial BG and lipid levels on cardiovascular structures.
3.2. Obesity
Elevated body mass index (BMI) greater than 25kg/m2 is recognized as the primary risk factor for CVD and lowers quality of life [10]. In 2015, 603 million persons globally were obese due to an SB and the consumption of meals high in energy, with a 5% global incidence among youngsters [10]. Although risk factors for CVD are already apparent in childhood, CVD is primarily diagnosed in adults [10]. Furthermore, longer periods of inactivity, particularly when it comes to recreational screen usage, are linked to worse health consequences [10]. For instance, longer screen times—which include watching television—are linked to worsening cardio-metabolic health and fitness [10]. When sitting for a long time, the body is immobile for a long time, and lack of exercise, and the muscle strength of the lower limbs are weakened, which is easy to lead to fat accumulation and eventually overweight or obesity. Obesity is a disease, in addition, is also a high-risk factor for CVD, the two cause and affect each other, forming a vicious circle.
3.3. Inflammation and endothelial dysfunction
An early stage of vascular damage known as endothelial dysfunction (ED) reduces vasodilation and encourages the growth of plaque and inflammation in the arterial wall. Prolonged SB causes a fast impairment in EF, according to several laboratory investigations [9]. Reducing extended periods of SB with low energy expenditure activity breaks helps older, sedentary overweight/obese women's EF and immediately reduces EF decrease in young, active individuals. Prolonged sitting-associated ED is a result of decreased lower extremity blood flow and skeletal muscle contractions during prolonged SB, especially in unbroken episodes [9].
Studies reveal that the main organs and tissues in charge of controlling the vascular and metabolic effects of PA are peripheral tissues and cells. Long periods of continuous sitting can harm blood vessels, reduce muscle activity (particularly in the lower limbs' weight-bearing muscles), and lower energy demand because of decreased peripheral blood flow and shear stress [9]. These effects can also increase blood vessel contraction, which can lead to vascular dysfunction, increase venous pressure in the lower limbs, and increase sympathetic nerve activity in the muscles and blood viscosity. This changes blood flow and shear pressure, increasing the risk of thrombosis [9]. Cross-sectional relationships between PA and indicators of low-grade inflammation have been proposed by research [9].
4. Physical activity interventions
To lower the risk of CVD, PA has been suggested as a management option. There is variability in the guidelines for PA from different authorities based on age, gender, physical condition, and purpose. In order to lower the risk of CVD, the American Heart Association (AHA) suggests long-term PA as the first line of therapy for dyslipidemia. For BP control, aerobic exercise of no less than 40 minutes at least three to four times a week needs to be continued for more than 12 weeks, according to the AHA guidelines [11]. When resistance training (RT) is done at the 500–1000 METs weekly exercise intensity advised, it can also lower the risk of CVD [11]. The cardiovascular benefits of PA may be in terms of improving identified risk factors such as dyslipidemia, hypertension, obesity, and ED.
4.1. Improves blood lipids, blood pressure, blood glucose
Long-term PA significantly improves lipids in healthy people. A meta-analysis that included 75,075 participants found that long-term PA lowered triglycerides (TGs), total cholesterol (TC), and LDL and boosted HDL, which in turn lowered the risk of CVD [12]. Several changes were noted in the PA group: reduced TGs (weighted mean difference [WMD] = −7.27; 95% CI: −9.68 ~ −4.87), lower LDL (WMD = -5.80; 95% CI: -8.04 ~ -3.57), lower TC (WMD = −6.84; 95% CI: −9.15 ~ −4.52), and greater HDL (WMD = 2.38; 95% CI: 1.00 ~ 3.76) [12]. In addition, studies have shown that the duration and intensity of PA interventions are equally important. Studies have shown that PA for more than 12 weeks, above and beyond low-intensity PA, is required to significantly raise HDL [12].
PA is known to lower BP in hypertensive patients by decreasing sympathetic excitability. A study involving 1005791 participants found that long-term PA may attenuate the influence of BP associated with SB [5]. Long-term PA was found to significantly reduce BP compared to short and low levels of PA [12]. Extended-duration PA studies involving 3,500 participants showed significantly lower diastolic blood pressure (DBP) (WMD = -2.25; 95% CI: -2.94 ~ -1.56) and significantly lower systolic blood pressure (SBP) (WMD = -3.63; 95% CI: -4.62 ~ -2.64) [12].
PA is equally effective in helping to control BG problems. An analysis of 65 randomized controlled trials (RCT) found that PA significantly improved fasting BG (WMD = -4.40; 95% CI: -5.44 to -3.36) [12].
4.2. Improves body mass index
A set of guidelines has been created to support the health advantages of PA. Children (4–18 years old) should restrict screen time, especially recreational screen time, and participate in moderate–to–intense PA, preferably adding increasingly strenuous activities [13]. Additionally, bone- and muscle-strengthening PA is advised at least three times per week according to these guidelines [13].
PA for up to 60 minutes a day decreased cardiovascular risk variables, including waist circumference and BMI scores, according to research involving 500 Dutch children [10]. Consequently, early infancy should be the starting point for CVD prevention.
A study suggests that running-based HIIT can help obese adolescents in school maintain better physical health and prevent CVD. Forty-five teenage males with an obesity BMI of 24.2 ± 1.0 kg/m2 were randomly assigned to one of three groups: moderate-intensity continuous training (MICT, n = 15), high-intensity interval training (HIIT, n = 15), or a control group (CON, n = 15) [13]. For a duration of 12 weeks, the intervention groups exercised three times a week [13]. The HIIT group ran for 15 seconds at two different intensities: eight sets of high intensity run (90 ~ 100% of maximum aerobic speed; MAS)] and eight sets of low intensity runs (50 % of MAS). The CON group was told to carry on with its normal operations. The MICT group ran for 30 minutes at a moderate intensity (60 ~ 70% MAS) [13]. Each participant had baseline and post-intervention assessments of their body composition indices, cardio-metabolic markers, and cardio-respiratory fitness (CRF). The results showed that although the two treatments did not significantly vary, the BMI and body fat mass dropped in the HIIT and MICT groups (BMI: - 1.8 kg/m2 vs. - 1.2 kg/m2, P < 0.01; FM: - 1.6 kg, P < 0.05 vs. -3.7 kg, P < 0.01) [13].
4.3. Enhance cardiovascular metabolic health
PA is essential for enhancing cardio-metabolic health. According to research, PA guards against damage during the initial phases of myocardial infarction [13]. Above a moderate intensity, PA has been observed by some researchers to reduce or completely abolish the correlation between SB and CVD [13]. While substituting light-intensity PA for SB is expected to have some health advantages for PI people, higher-intensity PA may have even more benefits for all individuals [13].
All forms of PA were significant in improving cardio-metabolic health for people who were overweight. A study took 4331 participants who included five types of exercise as intervention groups and an inactive or sedentary control group (n=1592) [14]. Participants were healthy individuals aged 18 to 64 years with a BMI ≥25. Specifically, continuous endurance training (CET) (n=1424), RT (n=668), combined training (CT) (n=198), interval training (INT) (n=340), hybrid-type training (HYB) (n=109). After converting all results to standard units, the mean difference between pre-and post-training was computed by subtracting the mean. Table 1 shows the definitions of the five exercise types. The mean exercise duration more than 3 weeks. There were an average of 3.5±1.0 sessions each week, with a mean session length of 43±21 minutes. Figure 1 shows that 917, 917, 110, 420, and 2368 people were engaged in the assessment of mean arterial pressure (MAP), CRF, SBP, DBP, and resting heart rate (RHR) efficacy, respectively. Five different exercise modalities on resting vascular function (MAP, RHR, SBP, DBP, and CRF) are depicted in Figure 1 of the research [14]. According to the data shown in Figure 1, CT was the most optimal control programme for decreasing DBP, SBP, and boosting CRF, with scores of -5.58 [-9.18 ~ -1.99]), -4.70 [-8.18 ~ 1.23], and 6.35 [1.46 ~ 11.24], respectively. Additionally, the most successful treatments for lowering MAP and RHR were found to be RT (-6.20 [-10.77 ~ -1.63]) and HYB (-5.63 [-9.94 ~ -1.31]). In summary, CT was found to be the preferred control scheme in improving cardio-metabolic related outcomes in these people, with HYB coming in second [14]. These results suggest that multi-component exercise (MCE) interventions are more effective than single-component modalities, such as CET, INT, and RT [14]. Therefore, the use of MCE interventions is an important way to improve cardiac metabolism and reduce the incidence of CVD.
Table 1. Definition of Exercise Types [14]
HYB | 1-3 times a week, at an intensity of >65% VO2max, >65% HRR, or >75% HRmax. Total workout time: thirty to forty-five minutes each. Any type of intermittent multi-component exercise, such as multi-modal training, integrated neuromuscular training, high-intensity functional training, and cardio RT. |
CT | An amalgam of RT and CET |
CET | Weekly frequency: 3–5×. Intensity: >50% HRR, >65% HRmax, or >45% VO2max. 30 to 60 minutes each session. Aerobic exercises such as walking, running, biking, and rowing. |
INT | Usually, 2-3 times a week. >65% VO2max, >65% HRR, or >75% HRmax deems an intensity. Total workout time: twenty to thirty minutes each. Any intermittent, conventional interval training modality that is intermittent, including single-component HIIT and MIIT (such as walking, jogging, cycling, rowing, and swimming). |
RT | ≥50% 1RM is the intensity. Usually, 2-3 times a week. Total workout time: thirty to sixty minutes each. Any mode of RT. |
HRmax, maximum heart rate; HRR, heart rate reserve; MIIT, moderate-intensity interval training; RM, repetition maximum; VO2max, maximal oxygen uptake.
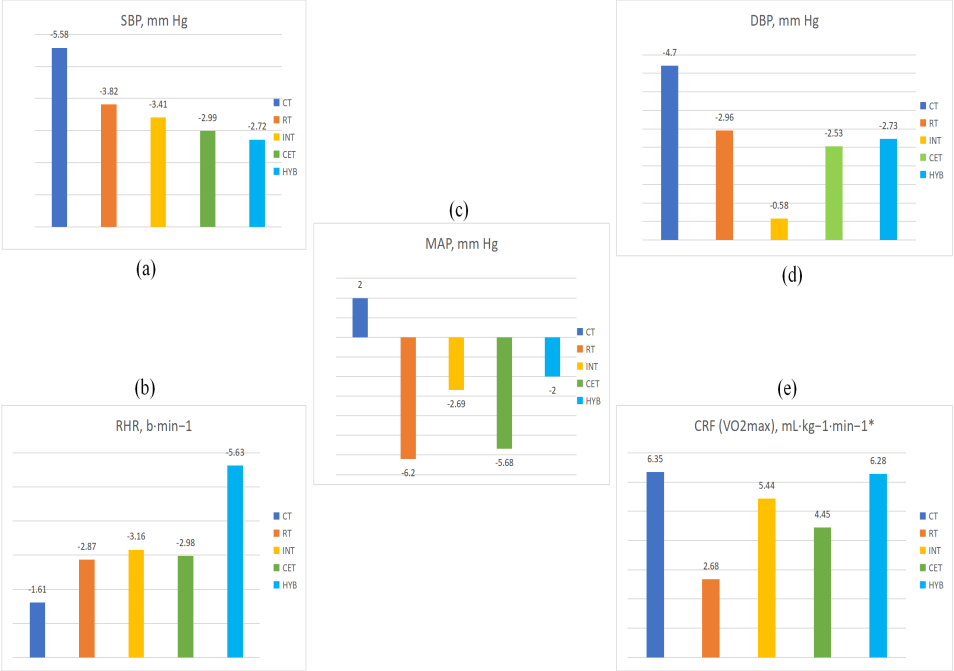
Figure 1. Analyze Bar Graphs Comparing the Efficacy of Exercise Types [14].
(a) change of SBP (mm Hg); (b) change of RHR ( b.min−1); (c) change of MAP (mm Hg); (d) change of DBP (mm Hg); (e) change of CRF (VO2max) (mL.kg-1.min-1);*Clinically desirable outcome is an increase (+).
4.4. Potential mechanism
Research that involved long-term PA in healthy people showed noteworthy changes in BP, BG, and BMI; these findings have been extensively verified. A large RCT [14] found that all individuals had lower blood pressure, weight, and fasting glucose after receiving PA for more than eight weeks. Individuals with different genders, weights, and PA types and intensities experienced the same outcomes. Studies have shown that following PA intervention, there was an improvement in the subjects' BG, body fat, waist circumference, and BMI, as well as an increase in their omentin-1 concentrations [12]. Omentin-1 was discovered in lower concentrations in obese individuals and was negatively correlated with blood pressure, fasting glucose, and BMI [12]. Following the PA intervention, there may have been a rise in the body's concentration of omentin-1, which has improved outcomes associated with CVD.
Furthermore, the efficient use of resources and energy-releasing basic materials in combination with autonomous skeletal muscle contraction, which enhances brain coordination and metabolism, is the mechanism by which PA reduces the risk factor [12]. PA significantly enhances cardiovascular health in healthy adults by improving cardiopulmonary function and a variety of CVD biomarkers, such as lipids [12]. Additionally, long-term aerobic exercisers and endurance athletes have higher levels of HDL and lower total cholesterol [12]. Lipoprotein lipase (LPL) levels may have increased in these individuals, contributing to their better lipid profiles. An increase in LPL concentration causes apolipoprotein-E to be redistributed and changes the composition of lipoprotein in vivo. This alteration lowers the risk of CVD by increasing HDL concentrations and decreasing plasma LDL and HDL ratios [12].
5. Conclusion
With the elevated incidence of CVD, it is clear that SB is an extremely important predisposing factor. Long-term SB increases the risk of CVD in healthy people, possibly because to the several CVD risk factors that SB induces, such as obesity, hypertension, and dyslipidemia. Frequent physical activity lowers the risk of CVD and enhances risk markers. Therefore, to lower the incidence of CVD, people should be encouraged to increase the duration and intensity of their PA and restrict the amount of time they spend inactive each day. It's possible, though, that some other significant effects were left out of this study. More quantifiable indicators of benefits are needed to demonstrate the cardiovascular harm of SB. Increased awareness and education about the dangers of SB are needed to better improve awareness of the need for increased PA. At present, there aren't enough high-quality prospective studies in China, and more research will eventually be required.
Acknowledgment
This work was supported by Guangxi Medical and health key discipline construction project.
References
[1]. Townsend, N., Kazakiewicz, D., Lucy Wright, F., Timmis, A., Huculeci, R., Torbica, A., Gale, C. P., Achenbach, S., Weidinger, F., & Vardas, P. (2022). Epidemiology of cardiovascular disease in Europe. Nature reviews. Cardiology, 19(2), 133–143. https://doi.org/10.1038/s41569-021-00607-3
[2]. Liang, Z. D., Zhang, M., Wang, C. Z., Yuan, Y., & Liang, J. H. (2022). Association between sedentary behavior, physical activity, and cardiovascular disease-related outcomes in adults-A meta-analysis and systematic review. Frontiers in public health, 10, 1018460. https://doi.org/10.3389/fpubh.2022.1018460
[3]. Katzmarzyk, P. T., Powell, K. E., Jakicic, J. M., Troiano, R. P., Piercy, K., Tennant, B., & 2018 PHYSICAL ACTIVITY GUIDELINES ADVISORY COMMITTEE* (2019). Sedentary Behavior and Health: Update from the 2018 Physical Activity Guidelines Advisory Committee. Medicine and science in sports and exercise, 51(6), 1227–1241. https://doi.org/10.1249/MSS.0000000000001935
[4]. Guthold, R., Stevens, G. A., Riley, L. M., & Bull, F. C. (2018). Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1·9 million participants. The Lancet. Global health, 6(10), e1077–e1086. https://doi.org/10.1016/S2214-109X(18)30357-7
[5]. Zhou, W., Yan, W., Wang, T., Zhu, L. J., Xu, Y., Zhao, J., Yu, L. L., Bao, H. H., & Cheng, X. S. (2021). Independent and joint association of physical activity and sedentary behavior on all-cause mortality. Chinese Medical Journal, 134(23), 2857–2864. https://doi.org/10.1097/CM9.0000000000001730
[6]. LaMonte, M. J., Larson, J. C., Manson, J. E., Bellettiere, J., Lewis, C. E., LaCroix, A. Z., Bea, J. W., Johnson, K. C., Klein, L., Noel, C. A., Stefanick, M. L., Wactawski-Wende, J., & Eaton, C. B. (2020). Association of Sedentary Time and Incident Heart Failure Hospitalization in Postmenopausal Women. Circulation. Heart failure, 13(12), e007508. https://doi.org/10.1161/CIRCHEARTFAILURE.120.007508
[7]. Ekelund, U., Steene-Johannessen, J., Brown, W. J., Fagerland, M. W., Owen, N., Powell, K. E., Bauman, A., Lee, I. M., Lancet Physical Activity Series 2 Executive Committe, & Lancet Sedentary Behaviour Working Group (2016). Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet (London, England), 388(10051), 1302–1310. https://doi.org/10.1016/S0140-6736(16)30370-1
[8]. Pinto, A. J., Bergouignan, A., Dempsey, P. C., Roschel, H., Owen, N., Gualano, B., & Dunstan, D. W. (2023). Physiology of sedentary behavior. Physiological reviews, 103(4), 2561–2622. https://doi.org/10.1152/physrev.00022.2022
[9]. Chen, L., You, G., Yang, Z., Shen, R., Zhang, R., Zhu, D., Wang, L., Lin, S., Lv, L., & Huang, K. (2023). Leisure sedentary behaviour increases the risk of venous thromboembolism: a Mendelian randomisation study. BMC cardiovascular disorders, 23(1), 362. https://doi.org/10.1186/s12872-023-03395-5
[10]. Velde, G. T., Plasqui, G., Willeboordse, M., Winkens, B., & Vreugdenhil, A. (2021). Associations between physical activity, sedentary time and cardiovascular risk factors among Dutch children. PloS one, 16(8), e0256448. https://doi.org/10.1371/journal.pone.0256448
[11]. Grundy, S. M., Stone, N. J., Bailey, A. L., Beam, C., Birtcher, K. K., Blumenthal, R. S., Braun, L. T., de Ferranti, S., Faiella-Tommasino, J., Forman, D. E., Goldberg, R., Heidenreich, P. A., Hlatky, M. A., Jones, D. W., Lloyd-Jones, D., Lopez-Pajares, N., Ndumele, C. E., Orringer, C. E., Peralta, C. A., Saseen, J. J., … Yeboah, J. (2019). 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation, 139(25), e1082–e1143. https://doi.org/10.1161/CIR.0000000000000625
[12]. https://doi.org/10.1161/CIR.0000000000000625 Liang, Z. D., Zhang, M., Wang, C. Z., Yuan, Y., & Liang, J. H. (2022). Association between sedentary behavior, physical activity, and cardiovascular disease-related outcomes in adults-A meta-analysis and systematic review. Frontiers in public health, 10, 1018460. https://doi.org/10.3389/fpubh.2022.1018460
[13]. Meng, C., Yucheng, T., Shu, L., & Yu, Z. (2022). Effects of school-based high-intensity interval training on body composition, cardiorespiratory fitness and cardiometabolic markers in adolescent boys with obesity: a randomized controlled trial. BMC pediatrics, 22(1), 112. https://doi.org/10.1186/s12887-021-03079-z
[14]. Batrakoulis, A., Jamurtas, A. Z., Metsios, G. S., Perivoliotis, K., Liguori, G., Feito, Y., Riebe, D., Thompson, W. R., Angelopoulos, T. J., Krustrup, P., Mohr, M., Draganidis, D., Poulios, A., & Fatouros, I. G. (2022). Comparative Efficacy of 5 Exercise Types on Cardiometabolic Health in Overweight and Obese Adults: A Systematic Review and Network Meta-Analysis of 81 Randomized Controlled Trials. Circulation. Cardiovascular quality and outcomes, 15(6), e008243. https://doi.org/10.1161/CIRCOUTCOMES.121.008243
Cite this article
Long,Y. (2024). The cardiovascular risks of sedentary behavior and the progress of physical activity interventions. Theoretical and Natural Science,50,34-41.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of ICBioMed 2024 Workshop: Workshop on Intelligent Medical Data Analysis for Precision Medicine
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Townsend, N., Kazakiewicz, D., Lucy Wright, F., Timmis, A., Huculeci, R., Torbica, A., Gale, C. P., Achenbach, S., Weidinger, F., & Vardas, P. (2022). Epidemiology of cardiovascular disease in Europe. Nature reviews. Cardiology, 19(2), 133–143. https://doi.org/10.1038/s41569-021-00607-3
[2]. Liang, Z. D., Zhang, M., Wang, C. Z., Yuan, Y., & Liang, J. H. (2022). Association between sedentary behavior, physical activity, and cardiovascular disease-related outcomes in adults-A meta-analysis and systematic review. Frontiers in public health, 10, 1018460. https://doi.org/10.3389/fpubh.2022.1018460
[3]. Katzmarzyk, P. T., Powell, K. E., Jakicic, J. M., Troiano, R. P., Piercy, K., Tennant, B., & 2018 PHYSICAL ACTIVITY GUIDELINES ADVISORY COMMITTEE* (2019). Sedentary Behavior and Health: Update from the 2018 Physical Activity Guidelines Advisory Committee. Medicine and science in sports and exercise, 51(6), 1227–1241. https://doi.org/10.1249/MSS.0000000000001935
[4]. Guthold, R., Stevens, G. A., Riley, L. M., & Bull, F. C. (2018). Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1·9 million participants. The Lancet. Global health, 6(10), e1077–e1086. https://doi.org/10.1016/S2214-109X(18)30357-7
[5]. Zhou, W., Yan, W., Wang, T., Zhu, L. J., Xu, Y., Zhao, J., Yu, L. L., Bao, H. H., & Cheng, X. S. (2021). Independent and joint association of physical activity and sedentary behavior on all-cause mortality. Chinese Medical Journal, 134(23), 2857–2864. https://doi.org/10.1097/CM9.0000000000001730
[6]. LaMonte, M. J., Larson, J. C., Manson, J. E., Bellettiere, J., Lewis, C. E., LaCroix, A. Z., Bea, J. W., Johnson, K. C., Klein, L., Noel, C. A., Stefanick, M. L., Wactawski-Wende, J., & Eaton, C. B. (2020). Association of Sedentary Time and Incident Heart Failure Hospitalization in Postmenopausal Women. Circulation. Heart failure, 13(12), e007508. https://doi.org/10.1161/CIRCHEARTFAILURE.120.007508
[7]. Ekelund, U., Steene-Johannessen, J., Brown, W. J., Fagerland, M. W., Owen, N., Powell, K. E., Bauman, A., Lee, I. M., Lancet Physical Activity Series 2 Executive Committe, & Lancet Sedentary Behaviour Working Group (2016). Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet (London, England), 388(10051), 1302–1310. https://doi.org/10.1016/S0140-6736(16)30370-1
[8]. Pinto, A. J., Bergouignan, A., Dempsey, P. C., Roschel, H., Owen, N., Gualano, B., & Dunstan, D. W. (2023). Physiology of sedentary behavior. Physiological reviews, 103(4), 2561–2622. https://doi.org/10.1152/physrev.00022.2022
[9]. Chen, L., You, G., Yang, Z., Shen, R., Zhang, R., Zhu, D., Wang, L., Lin, S., Lv, L., & Huang, K. (2023). Leisure sedentary behaviour increases the risk of venous thromboembolism: a Mendelian randomisation study. BMC cardiovascular disorders, 23(1), 362. https://doi.org/10.1186/s12872-023-03395-5
[10]. Velde, G. T., Plasqui, G., Willeboordse, M., Winkens, B., & Vreugdenhil, A. (2021). Associations between physical activity, sedentary time and cardiovascular risk factors among Dutch children. PloS one, 16(8), e0256448. https://doi.org/10.1371/journal.pone.0256448
[11]. Grundy, S. M., Stone, N. J., Bailey, A. L., Beam, C., Birtcher, K. K., Blumenthal, R. S., Braun, L. T., de Ferranti, S., Faiella-Tommasino, J., Forman, D. E., Goldberg, R., Heidenreich, P. A., Hlatky, M. A., Jones, D. W., Lloyd-Jones, D., Lopez-Pajares, N., Ndumele, C. E., Orringer, C. E., Peralta, C. A., Saseen, J. J., … Yeboah, J. (2019). 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation, 139(25), e1082–e1143. https://doi.org/10.1161/CIR.0000000000000625
[12]. https://doi.org/10.1161/CIR.0000000000000625 Liang, Z. D., Zhang, M., Wang, C. Z., Yuan, Y., & Liang, J. H. (2022). Association between sedentary behavior, physical activity, and cardiovascular disease-related outcomes in adults-A meta-analysis and systematic review. Frontiers in public health, 10, 1018460. https://doi.org/10.3389/fpubh.2022.1018460
[13]. Meng, C., Yucheng, T., Shu, L., & Yu, Z. (2022). Effects of school-based high-intensity interval training on body composition, cardiorespiratory fitness and cardiometabolic markers in adolescent boys with obesity: a randomized controlled trial. BMC pediatrics, 22(1), 112. https://doi.org/10.1186/s12887-021-03079-z
[14]. Batrakoulis, A., Jamurtas, A. Z., Metsios, G. S., Perivoliotis, K., Liguori, G., Feito, Y., Riebe, D., Thompson, W. R., Angelopoulos, T. J., Krustrup, P., Mohr, M., Draganidis, D., Poulios, A., & Fatouros, I. G. (2022). Comparative Efficacy of 5 Exercise Types on Cardiometabolic Health in Overweight and Obese Adults: A Systematic Review and Network Meta-Analysis of 81 Randomized Controlled Trials. Circulation. Cardiovascular quality and outcomes, 15(6), e008243. https://doi.org/10.1161/CIRCOUTCOMES.121.008243