1. Introduction
Brain-computer interface (BCI), or brain-machine interface, is an advanced system which provides direct communications between specific parts of the human brain and a computer [1]. In recent years, this domain has gained huge interests from scientists worldwide, which offers people with the chances of controlling external devices, such as prostheses, through brain activities [2]. To date, BCI has been mainly explored in the field of motor control. For example, a recent study discovered that BCI-based treatment could effectively help the neurorehabilitation of stroke patients with motor deficits [3]. However, the roles of BCI could be explored beyond motor control, as recently BCI has gained focuses from the field of cancer [2]. In specific, scientists have attempted to integrate BCI in the diagnostics, prognostics and treatments of various cancers (e.g., breast and brain cancers), for improving the clinical outcomes of cancer patients [2]. For example, BCI combined with electroencephalogram (EEG) was suggested to increase the speed of cancer diagnosis [2]. In addition, some common side effects from cancer therapies observed in cancer patients or survivors such as motor and language deficits, cognitive impairments and peripheral neuropathy could be effectively reduced with the help of BCI-based systems, as a safer approach compared to traditional therapies [4]. Therefore, this article would briefly summarise how BCI could be applied in oncological settings, according to up-to-date literature, in addition to suggesting the current limitations and challenges of BCI. In specific, the basic components of BCI would be firstly explained, and then how it can be incorporated into the diagnostics, treatments and neurorehabilitation following cancer therapies in patients would be explored, along with some possible concerns or issues such as psychological, technological and ethical ones associated with it.
2. BCI components
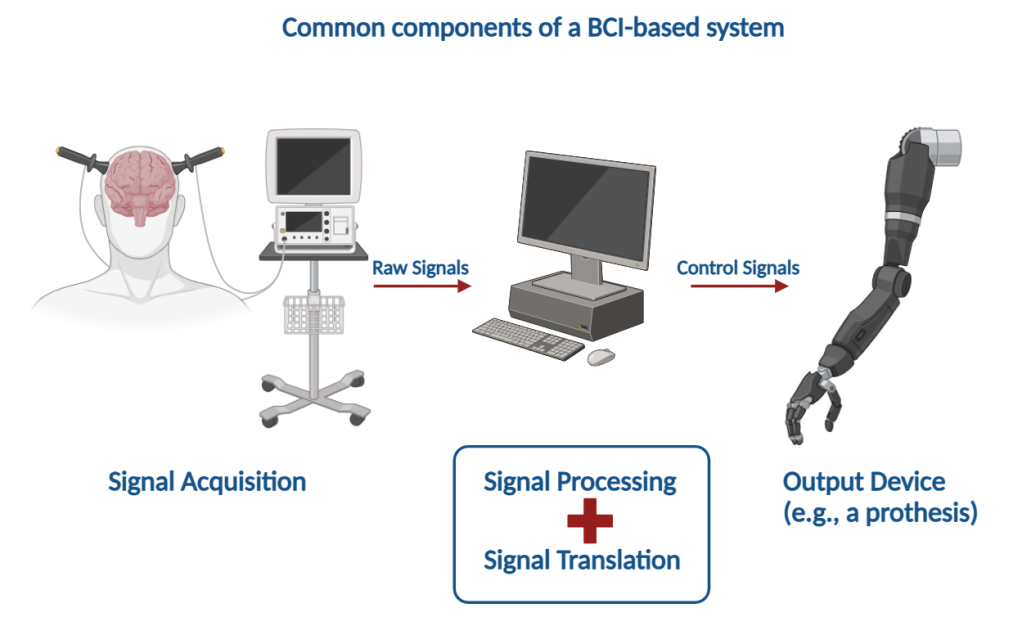
There are currently diverse types of BCIs, such as active, reactive and passive BCIs [5]. In general, a BCI-based system involves four basic components: signal acquisition, signal processing, signal translation, plus an output device (a prosthesis for example) (figure 1).
| |
Figure 1. Common components of a BCI-based system (Photo/Picture credit : Original) . | |
Since brain activities are of paramount importance by reflecting a series of physiological conditions within one’s body, the first component of BCI, signal acquisition, is responsible for receiving brain activity signals and sending these signals for signal processing, which is the second component [6]. There are currently different types of signal-recording devices, which could be roughly divided into two main categories: the invasive ones such as the cortical implants and the non-invasive ones such as the EEG [6]. In general, the invasive ones have higher spatial specificity but less stability, whereas the non-invasive ones lack a high resolution, although being relatively stable. The signal processing and translation steps would minimise the background noises and translate the processed signals into signals that could be read by the output device respectively [5]. For example, background noises would typically be generated in EEG recordings by various factors such as the locations of the electrodes being placed. As these would affect the interpretation of the results recorded, the intended signals would be extracted from the background and being sent to a processing unit. The processing unit contains a series of algorithms which can translate the brain activity signals into signals that can be recognised by the final component of the BCI - the output device, just like a common language translator [5]. Finally, the output device, which is typically a computer or a prothesis, would read the signals translated by the algorithms, follow the instructions given and eventually help the user or patient to achieve their intended tasks such as different movements and communications [5]. Together, the four basic components of BCI would act in an orchestrated way to support the users, offering them the platform for performing a range of complicated tasks.
3. BCI on improving clinical outcomes of cancer patients
As mentioned before, BCI-based robotics have been mainly developed for assisting motor control. In 2006, a groundbreaking study reported the use and control of neuromotor prostheses (robotics) in a tetraplegic patient via intracortical implants [7], which explored the field of BCI within motor controls. Recent studies have also combined the EEG and motor imagery with BCI for assisting rehabilitation of patients, meanwhile being less invasive than previous ones [3,8]. However, besides motor controls, the application of BCI could certainly be expanded further.
3.1. Diagnostics
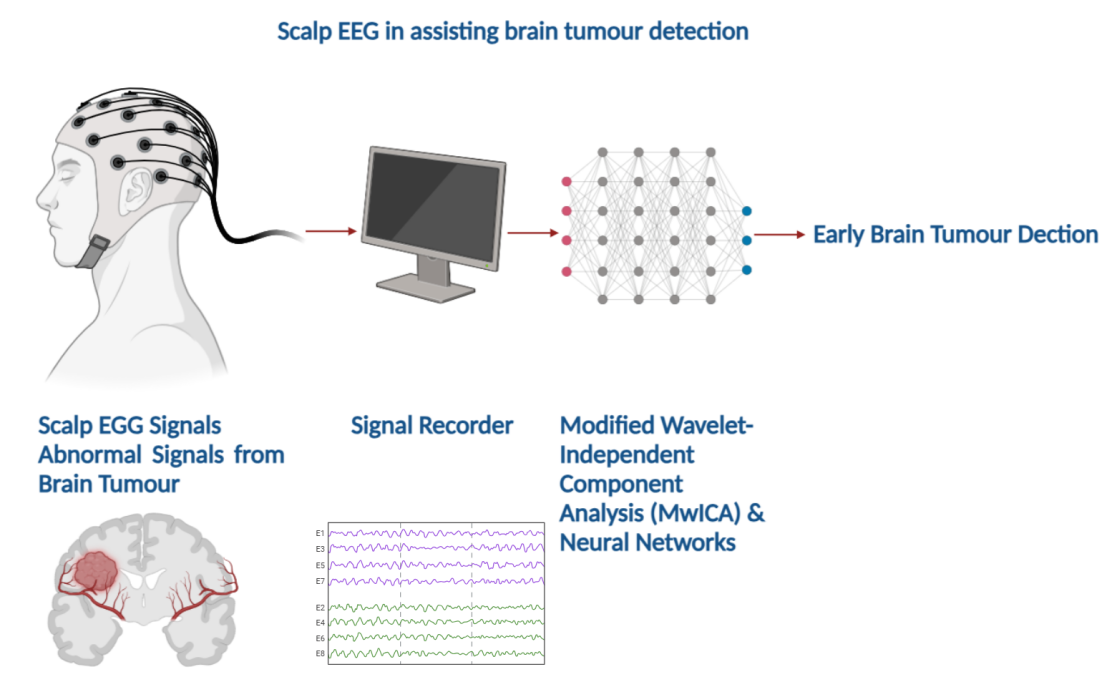
One of the newest BCI approaches has been focused on the diagnosis of cancers [4]. For example, scalp EEG was developed to assist the diagnosis of brain tumours such as glioblastoma [4]. This type of EEG is usually complemented with the modified wavelet-independent component analysis (MwICA) and neural networks, in which signals from the EEG are processed by the MwICA after collection by the EEG electrodes [4]. This approach would enable a relatively accurate detection of abnormal signals resulted from aberrant brain activities, which in turn help the early brain tumour detections. Figure 2 provides a brief illustration of a typical scalp EEG being used to detect abnormal brain signals.
|
Figure 2. Scalp EEG in assisting brain tumour detection (Photo/Picture credit : Original). |
As well as brain tumours, scientists have proposed that EEG-based approaches could provide an avenue for the diagnosis and prognosis of breast cancers [9]. This might be done by assessing aberrant brain activities (e.g., irregular sodium and potassium ion flows), corelating these anomalies to specific gene or protein mutations related to breast cancer. Together, these BCI-based systems combined with EEG may greatly elevate the speed of cancer diagnosis, compared to current approaches which are mainly based on biopsies and other biological tests [6]. However, one current limitation of BCI-based detection methods is that the detected results can only be correlated with a specific disease such as breast cancer, whilst the definite diagnosis is made only when these results are complemented with the corresponding anomalies discovered by medical scans or biopsies.
3.2. Reduction in side effects from cancer therapies
In addition to assisting the cancer diagnostics by using scalp EEG combined with MwICA, the biofeedback, or neurofeedback, of EEG could be applied to monitor and potentially reduce the post-cancer cognitive impairments typically found in cancer survivors [10]. For example, breast cancer survivors might often suffer from fatigue and various degrees of memory function impairments because of surgery, chemotherapy, radiotherapy or other types of clinical interventions [10]. Therefore, how these side effects could be controlled or minimised by BCI applications are of recent concerns from the researchers. In this case, a real-time feedback of EEG signals from brain activities would be recorded, as either visual or auditory information, therefore allowing the brain activities to be modified [10]. This study investigated into 23 female breast cancer survivors aged 40 or over, and found out that the EEG biofeedback potentially reduced the cognitive impairments seen in these survivors as a result of cancer therapies, such as the negative impacts on the quality of life [10]. This suggests that breast cancer survivors could potentially enjoy a better life with the help of the EEG biofeedback.
Another clinical trial also investigated into the effects of EEG biofeedback on chemotherapy-induced peripheral neuropathy observed in cancer survivors [11]. Peripheral neuropathy is a chronic complication which might lead to long-term neuropathic pain in patients, due to the damages to the neurons in the nervous system [11]. This study hence measured several parameters such as pain, sleep quality and fatigue which are typical consequences of neuropathic pain. It was discovered that the participants attending the EEG biofeedback sessions showed reductions in the pain levels perceived, improvements in fatigue values and many other symptoms [11]. Furthermore, when being compared to traditional medications for neuropathic pain relief, such as pregabalin (an anti-seizure drug that prevents the frequent firing of voltage-gated calcium channels), this type of EEG-based system exerts less side effects (e.g., drowsiness) to the users. As a result, the chemotherapy-induced peripheral neuropathy might also be tackled or relieved by BCI-based systems such as the EEG biofeedback.
3.3. Neurorehabilitation
BCI-based technology can as well be applied for the neurorehabilitation in cancer patients. Patients suffering from brain tumours such as glioma often require craniotomy for surgical resection of tumours. This type of highly invasive surgery might lead to a range of neurological side effects such as impaired neural plasticity, language or motor deficits, and psychiatric illnesses [12]. Therefore, it is important for scientists to discover different means to minimise these side effects. Poologaindran et al. [12] in turn suggested that an FDA-approved BCI-based therapy - the repetitive transcranial magnetic stimulation (rTMS) - could be applied to relieve these side effects, providing a chance of neurorehabilitation for those patients. This technique is based on generating different intensities of magnetic fields which target a specific brain area (in this case following the theta burst stimulation (TBS) protocols) [12]. This type of stimulation could consequently control the cortical excitability of one’s brain, potentially reducing the common neurological side effects seen in the post-craniotomy glioma patients. After different rounds of testing, as no seizure cases were observed, they proposed that this method could be safe, and a range of benefits in glioma patients recovering from craniotomy were seen following this treatment (e.g., language and motor functional recoveries. Consequently, although no long-term data were collected, this study provides promising evidence that the BCI-based therapies may in the future be used for neurorehabilitation and other functional recoveries in cancer patients or survivors.
As well as patients with glioma, a study has shown that patients with astrocytoma, another type of brain tumour arising from mutations in astrocytes, could also benefit from BCI interventions [13]: A 32-year-old female patient with astrocytoma suffering from hemiparesis (muscle weakness in half side of her body) participated in this study. The researchers of this study applied EEG to record her motor intention (MI) signals from her paralysed hand following the use of a set of visual cues. The BCI system connected to the EEG was then responsible for decoding and converting these signals, sending them to a robotic hand orthosis which assisted the movements of the patient’s fingers. After 30 sessions of interventions, the patient exhibited various degrees of improvements in motor impairments and recoveries in hand motor functions. Hence, this study further uncovered the potentials of BCI-based applications in terms of assisting the neurorehabilitation in patients suffering from different types of brain tumours.
4. BCI limitations & challenges
4.1. Physical and psychological issues
Although BCI technologies offer revolutionary rehabilitative and enhancement experiences for individuals with disabilities, neurological disorders, and even the general population—such as restoring motor functions, treating mental health conditions, and enhancing human-computer interaction—the health risks associated with their utilization should not be overlooked [5]. Users may experience accumulative physical exhaustion and increased psychological stress as they engage in ongoing BCI training, undergo invasive implantation procedures, and repetitively operate the systems. This is particularly pronounced in the context of invasive BCI technologies, where direct intervention into brain tissue significantly increases the risk of complications such as hemorrhage, brain injury, and post-operative infections, which can be extremely detrimental given the brain's high susceptibility to infection. Furthermore, long-term electrode implantation raises concerns regarding stability and biocompatibility, including inflammation caused by immune reactions and reduced signal transmission efficiency. Consequently, while embracing the conveniences and breakthroughs offered by BCI technologies, it is imperative to prudently evaluate and manage the underlying physiological and psychological risks [5]. Ensuring safety, reliability, and user-friendliness necessitates collaborative efforts from researchers, clinicians, and policymakers to continuously refine BCI technologies, enhancing their safety and practicality, while providing comprehensive education and support to users to help them understand and address potential challenges. This balanced approach will facilitate the healthy and sustainable application of BCI technologies in serving human well-being.
4.2. Technological issues
On top of the physical and psychological issues, technological limitations also exist for current BCI-based systems. One limitation is that, for non-invasive BCI like EEG, the spatial resolution is still relatively low, due to the long distance between the cortexes and electrodes. This also means that a higher current is required to reach the threshold for detection or stimulation, and a higher amount of background noises could present [5]. In addition, for invasive ones such as cortical implants, the electrodes may easily fall off from the set locations in one’s cerebral cortex due to the softness of the tissues. The electrodes sometimes also face the attacks from glial cells such as microglia and astrocytes, which further reduce their stability inside one’s brain [2]. Scientists as well need to ensure that the implants will not cause damages to nearby associated cortexes. Furthermore, although scientists have attempted to reduce the background signals recorded during the signal acquisition step, the background noises are still a relatively major problem in BCI applications, which might interfere with the final interpretation of signals [2].
4.3. Ethical issues
Ethical concerns are also a significant issue in BCI applications. For example, scientists could not predict whether frequent cortical implants and stimulations may result in alterations in personalities, either due to stresses felt or subtle effects on other associated cortexes [5]. These effects could be subtle, whilst scientists should not rule out the possibility that the effects sometimes might be significant. Furthermore, the data collected by the BCI applications are highly private, and this brings about the question of who should be entitled to have the access to these data [5], because unauthorised uses or accesses to one’s personal information significantly breaches one’s privacy. Under extreme circumstances, one’s personal safety could be jeopardised. It is also important for scientists to receive informed consents from people before starting the BCI experiments. This is especially relevant to people who could not express their own opinions such as those suffering from locked-in syndromes [5]: Sometimes people might not wish to undertake the BCI-related experiments, but they cannot express themselves to the scientists due to their impaired health status.
As a result, although BCI could benefit people by offering them the chances for motor control and could assist the diagnosis and treatment of cancer patients, it still poses a relatively large number of problems to current scientists and users. Future studies should aim to minimise these problems so as to increase the safety of BCI-based applications.
5. Conclusion
In conclusion, this article firstly introduced the four main components of a BCI-based system and their corresponding functions, which together help perform one’s desired tasks in an organised way. Then the most widely-explored field of BCI - the motor control - was briefly summarised: It can help patients with motor deficits to control robotics directly via their own brain activities and it also provides a platform for their rehabilitations. In addition, although BCI is a relatively new technology when it comes to oncological settings, it can be applied to either assist the diagnosis of different cancers or reduce side effects from cancer therapies such as language deficits, cognitive impairments and peripheral neuropathy, when being combined with different techniques such as the EEG and its biofeedback. At the same time, a series of example research was given to support these ideas mentioned above. Taken together, the clinical outcomes of cancer patients or survivors could be improved greatly by the use of BCI-based systems. On the other hand, there are also some nonnegligible issues associated with BCI such as physical, mental, technological and ethical concerns. Therefore, in future studies scientists should aim to minimise these issues when advancing novel BCI applications, offering people with a better and safer user experience.
References
[1]. Slutzky, M. W. 2019. Brain-Machine Interfaces: Powerful Tools for Clinical Treatment and Neuroscientific Investigations. Neuroscientist 25(2), 139-154.
[2]. Mridha, M. F., Das, S. C., Kabir, M. M., Lima, A. A., Islam, M. R., & Watanobe, Y. 2021. Brain-Computer Interface: Advancement and Challenges. Sens (Basel) 21(17), 5746.
[3]. Sebastián-Romagosa, M., Cho, W., Ortner, R., Murovec, N., Von Oertzen, T., Kamada, K., Allison, B. Z., & Guger, C. 2020. Brain Computer Interface Treatment for Motor Rehabilitation of Upper Extremity of Stroke Patients-A Feasibility Study. Front Neurosci 14, 591435.
[4]. Awuah, W. A., Ahluwalia, A., Darko, K., Sanker, V., Tan, J. K., Pearl, T. O., & Others. 2024. Bridging Minds and Machines: The Recent Advances of Brain-Computer Interfaces in Neurological and Neurosurgical Applications. World Neurosurg.
[5]. Mudgal, S. K., Sharma, S. K., Chaturvedi, J., & Sharma, A. 2020. Brain computer interface advancement in neurosciences: Applications and issues. Interdiscip Neurosurg 20, 100694.
[6]. Abdulkader, S. N., Atia, A., & Mostafa, M. S. 2015. Brain computer interfacing: Applications and challenges. Egyp Inform J 16(2), 213-230.
[7]. Hochberg, L. R., Serruya, M. D., Friehs, G. M., Mukand, J. A., Saleh, M., Caplan, A. H., & Others. 2006. Neuronal ensemble control of prosthetic devices by a human with tetraplegia. Nat 442(7099), 164-171.
[8]. Cheng, N., Phua, K. S., Lai, H. S., Tam, P. K., Tang, K. Y., Cheng, K. K., & Others. 2020. Brain-Computer Interface-Based Soft Robotic Glove Rehabilitation for Stroke. IEEE Trans Biomed Eng 67(12), 3339-3351.
[9]. Poulos, M., Felekis, T., & Evangelou, A. 2012. Is it possible to extract a fingerprint for early breast cancer via EEG analysis? Med Hypotheses 78(6), 711-716.
[10]. Alvarez, J., Meyer, F. L., Granoff, D. L., & Lundy, A. 2013. The effect of EEG biofeedback on reducing postcancer cognitive impairment. Integr Cancer Ther 12(6), 475-487.
[11]. Prinsloo, S., Novy, D., Driver, L., Lyle, R., Ramondetta, L., Eng, C., & Others. 2018. The Long-Term Impact of Neurofeedback on Symptom Burden and Interference in Patients With Chronic Chemotherapy-Induced Neuropathy: Analysis of a Randomized Controlled Trial. J Pain Symptom Manage 55(5), 1276-1285.
[12]. Poologaindran, A., Profyris, C., Young, I. M., Dadario, N. B., Ahsan, S. A., Chendeb, K., & Others. 2022. Interventional neurorehabilitation for promoting functional recovery post-craniotomy: a proof-of-concept. Sci Rep 12(1), 3039.
[13]. Carino-Escobar, R. I., Rodriguez-Barragan, M. A., Carrillo-Mora, P., & Cantillo-Negrete, J. 2022. Brain-computer interface as complementary therapy for hemiparesis in an astrocytoma patient. Neurol Sci 43(4), 2879-2881.
Cite this article
Chen,Y. (2024). Expanding brain-computer interfaces beyond motor control: improving clinical outcomes of cancer patients. Theoretical and Natural Science,56,40-45.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 2nd International Conference on Applied Physics and Mathematical Modeling
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Slutzky, M. W. 2019. Brain-Machine Interfaces: Powerful Tools for Clinical Treatment and Neuroscientific Investigations. Neuroscientist 25(2), 139-154.
[2]. Mridha, M. F., Das, S. C., Kabir, M. M., Lima, A. A., Islam, M. R., & Watanobe, Y. 2021. Brain-Computer Interface: Advancement and Challenges. Sens (Basel) 21(17), 5746.
[3]. Sebastián-Romagosa, M., Cho, W., Ortner, R., Murovec, N., Von Oertzen, T., Kamada, K., Allison, B. Z., & Guger, C. 2020. Brain Computer Interface Treatment for Motor Rehabilitation of Upper Extremity of Stroke Patients-A Feasibility Study. Front Neurosci 14, 591435.
[4]. Awuah, W. A., Ahluwalia, A., Darko, K., Sanker, V., Tan, J. K., Pearl, T. O., & Others. 2024. Bridging Minds and Machines: The Recent Advances of Brain-Computer Interfaces in Neurological and Neurosurgical Applications. World Neurosurg.
[5]. Mudgal, S. K., Sharma, S. K., Chaturvedi, J., & Sharma, A. 2020. Brain computer interface advancement in neurosciences: Applications and issues. Interdiscip Neurosurg 20, 100694.
[6]. Abdulkader, S. N., Atia, A., & Mostafa, M. S. 2015. Brain computer interfacing: Applications and challenges. Egyp Inform J 16(2), 213-230.
[7]. Hochberg, L. R., Serruya, M. D., Friehs, G. M., Mukand, J. A., Saleh, M., Caplan, A. H., & Others. 2006. Neuronal ensemble control of prosthetic devices by a human with tetraplegia. Nat 442(7099), 164-171.
[8]. Cheng, N., Phua, K. S., Lai, H. S., Tam, P. K., Tang, K. Y., Cheng, K. K., & Others. 2020. Brain-Computer Interface-Based Soft Robotic Glove Rehabilitation for Stroke. IEEE Trans Biomed Eng 67(12), 3339-3351.
[9]. Poulos, M., Felekis, T., & Evangelou, A. 2012. Is it possible to extract a fingerprint for early breast cancer via EEG analysis? Med Hypotheses 78(6), 711-716.
[10]. Alvarez, J., Meyer, F. L., Granoff, D. L., & Lundy, A. 2013. The effect of EEG biofeedback on reducing postcancer cognitive impairment. Integr Cancer Ther 12(6), 475-487.
[11]. Prinsloo, S., Novy, D., Driver, L., Lyle, R., Ramondetta, L., Eng, C., & Others. 2018. The Long-Term Impact of Neurofeedback on Symptom Burden and Interference in Patients With Chronic Chemotherapy-Induced Neuropathy: Analysis of a Randomized Controlled Trial. J Pain Symptom Manage 55(5), 1276-1285.
[12]. Poologaindran, A., Profyris, C., Young, I. M., Dadario, N. B., Ahsan, S. A., Chendeb, K., & Others. 2022. Interventional neurorehabilitation for promoting functional recovery post-craniotomy: a proof-of-concept. Sci Rep 12(1), 3039.
[13]. Carino-Escobar, R. I., Rodriguez-Barragan, M. A., Carrillo-Mora, P., & Cantillo-Negrete, J. 2022. Brain-computer interface as complementary therapy for hemiparesis in an astrocytoma patient. Neurol Sci 43(4), 2879-2881.