1. Introduction
Hypertension is a significant risk factor for the development of cardiovascular disease, and there exists a robust correlation between hypertension and the likelihood of mortality resulting from cardiovascular disease [1]. The emotional burden of hypertension can manifest itself in psychological distress [2]. In turn, psychological distress represents an additional risk factor for the development of hypertension [3]. Psychological distress is usually defined as a state of emotional distress characterized by nonspecific mental health problems, including symptoms associated with depression and anxiety [4]. Non-adherence to antihypertensive treatment represents a significant contributing factor to uncontrolled hypertension [5]. As reported by the World Health Organization, approximately 50-70% of hypertensive patients are non-adherent to their treatment [6]. Psychological distress was associated with non-adherence among individuals with hypertension [7]. Additionally, several studies have suggested a close link between employment status and both physical and mental health [8]. However, none of the studies on medication adherence have explored the association between employment status and psychological distress. The paper aims to explore whether employment status affects the association between psychological distress and medication adherence in hypertensive patients. The results are expected to emphasize the importance of mental health in chronic disease management and provide insights for targeted interventions or psychological therapies to improve medication adherence in specific employment groups.
2. Literature Review
Psychological distress is a critical factor in discussions about medical adherence, particularly related to anxiety and depression symptoms. Doubova et al. studied 487 adults with hypertension and found that increased levels of psychological distress adversely affected patient self-care and led to decreased medication adherence [9]. Furthermore, individuals with slight symptoms of anxiety or depression had a 1.59-fold and 2.48-fold higher likelihood, respectively, of becoming non-compliant within the next 3 months compared to those with minimal symptoms [10]. Also, as societal psychological conditions deteriorated, increased anxiety levels had a substantial negative impact on the adherence to medication among older persons [11]. However, several studies have not demonstrated a significant association between mental health and adherence. For example, a systematic review selected 18 studies from 2002 to 2020 and found that 9 of them did not show a significant association between depressive symptoms and medication adherence [12]. The lack of consensus may be attributed to differences in study design, psychological and adherence measurements, and criteria for defining depressive and hypertensive conditions. This lack of agreement highlights the complexity of the association between psychological factors and hypertension medication adherence, suggesting this association may be influenced by other factors. Therefore, it is necessary to test additional factors that may influence this association.
There exists a strong correlation between employment status and both psychological distress and medication adherence. Specifically, a meta-analysis revealed that the occurrence of psychological disorders among those who are unemployed is 18% greater than among those who are employed [13]. Additionally, a study conducted in Sweden including 51,118 persons revealed that unemployment and temporary employment were linked to greater levels of psychological distress in comparison to permanent and self-employment [14]. Few studies have tested the association between employment status and medication adherence, with one study suggesting that unemployed individuals typically have poorer medication adherence [15][16]. Nevertheless, a later study found that unemployed or retired hypertensive participants in China had 1.5 times higher odds of adhering to their medication compared to employed participants [15]. This positive association may be due to the characteristics of the sample and the region, where access to medical services is relatively easier in Hong Kong [15]. In view of these inconsistencies, this study aimed to revisit the association between employment status and medication adherence using a sample from Northern Ghana, where access to healthcare facilities is more limited [17].
Moreover, while employment is a fundamental determinant of health status [18], it has received less attention in terms of psychological distress and medication adherence than other demographic factors such as age, gender, race, and education level. This secondary data analysis aims to address gaps in the literature by testing the effect of employment status on the association between psychological distress and medication adherence in hypertensive patients. In addition, this paper analyzes specific aspects of psychological distress, including anxiety and depressive symptoms, to test this association. It is hypothesized that employment status may influence the association between psychological distress (including anxiety and depressive symptoms) and medication adherence. This can be demonstrated if the interaction term between psychological distress and employment status significantly influenced medication adherence. The main predictors were psychological distress, anxiety, depressive symptoms, and employment status, while the outcome variable was medication adherence.
3. Methodology
3.1. Research Design and Data Sources
This secondary data analysis used Kwakye data from a cross-sectional survey of adult patients in the Northern Region of Ghana, West Africa [19]. A total of 306 adults participated in the survey. They had been diagnosed with hypertension for at least six months, and were currently taking medication. The majority are aged between 40-60 years (46.73%), followed by 60-80 years (35.93%), 18-40 years (10.13%) and 80-100 years (7.19%). The majority of participants were female (64.38%), while males constituted 35.62% of the sample. In terms of employment status, 73.86% (226) of the participants were employed, 19.93% (61) were unemployed and 6.20% (19) were retired.
3.2. Variable Control
Demographic information collected included age, sex, religion, location, ethnicity, marital status, education, occupation, employment status, family history of hypertension, and co-morbidities.
Ten-item Kessler Psychological Distress Scale (K10) was used to measure psychological distress [20]. Participants reported the frequency of experiencing symptoms such as nervousness, hopelessness, sadness, worthlessness, and fatigue over the past month. Responses were rated on a 5-point Likert scale ranging from “none of the time” (1 point) to “all of the time” (5 points). The total score ranged from 10 to 50, with higher scores indicating greater psychological distress. The K10 scale can be divided into two subscales: a 4-item anxiety subscale (scoring 4-20) and a 6-item depression subscale (scoring 6-30), both of which were summed to assess specific symptoms of anxiety and depression. Previous studies have demonstrated strong internal consistency for the K10 (Cronbach’s \( α \) > 0.88). In this study, Cronbach’s \( α \) greater than 0.64, indicating acceptable internal consistency.
Five-item Medication Adherence Report Scale (MARS-5) was used to assess medication adherence [21], which includes questions about behaviors such as forgetting doses, altering dosages, stopping medication, skipping doses, and taking less than the prescribed amount. Participants rated the frequency of these non-adherent behaviors on a 5-point scale from “never” (1 point) to “always” (5 points). The total score ranged from 5 to 25; with higher scores indicating better adherence. Prior research has shown good internal consistency for the MARS-5 across various chronic illness patient groups (Cronbach’s \( α \) : 0.67 to 0.89) [21]. In the present study, the MARS-5 demonstrated good internal consistency as well, with Cronbach’s \( α \) greater than 0.75.
3.3. Statistical Analysis
Data were analyzed in R using RStudio. Three multiple linear regression models were built to predict medication adherence. The predictors of the first model included psychological distress, employment status (with levels: employed, unemployed, and retired), and their interaction term. The second and third models included employment status, either the depression symptom score or anxiety symptom score, along with their respective interaction terms with employment status. All models controlled for age, sex, religion, location, marital status, education, disease duration, number of medications taken per day, number of antihypertensive medications taken per day, and blood pressure. ANOVA was performed to evaluate whether the inclusion of interaction terms significantly improved the model fit.
4. Results
As shown in Table 1, using a cutoff of 24, participants generally reported relatively low medication adherence [22]. Additionally, the participants reported generally well psychological distress according to the Kessler Psychological Distress Scale [20].
Table 1. Descriptive Statistics
Variable | Mean | Sd | Maximum | Minimum |
Medication Adherence (5-25) | 22.39 | 2.73 | 25 | 14 |
Psychological Distress (10-50) | 14.96 | 3.61 | 32 | 10 |
Anxiety Symptom (4-20) | 5.37 | 1.54 | 14 | 4 |
Depression Symptom (6-30) | 9.59 | 2.51 | 20 | 6 |
The assumptions for the three linear regression models were generally met. Diagnostic checks showed that points 243, 149, and 122 were influential points with high leverage and high standardized residual. Therefore, they were excluded from later analysis.
4.1. Association between Psychological Distress, Employment Status and Medication Adherence
Table 2. Model Summary
Predictors | Estimates | Ci | P-Value |
(Intercept) | 25.46 | 22.53- 28.39 | <0.001 |
Age | 0.05 | 0.02- 0.08 | 0.001 |
Systolic Blood Pressure | -0.04 | -0.06- -0.02 | 0.001 |
Diastolic Blood Pressure | -0.01 | -0.04- 0.02 | 0.567 |
Psychological Distress | -0.01 | -0.10- 0.09 | 0.910 |
Employment Status (Retired) | -0.54 | -5.01- 3.93 | 0.813 |
Employment Status (Unemployed) | 4.04 | 0.43- 7.65 | 0.028 |
Psychological Distress ×Employment Status (Retired) | 0.03 | -0.27- 0.33 | 0.841 |
Psychological Distress ×Employment Status (Unemployed) | -0.30 | -0.55- -0.06 | 0.015 |
The model that included psychological distress, employment status, and their interaction was significant (F(18, 284) = 4.66, p < .05). This model accounted for 22.78% of the variance in medication adherence, with an adjusted R-squared value of 0.16. The association between psychological distress and medication adherence was slightly negative but not statistically significant (see Table 2, \( β \) = 0.006, SE = 0.05, p > .05; 95% CI [-0.10, 0.09]). Unemployed participants showed 4.04 higher medication adherence scores by compared to employed participants (see Table 2, p < .05; 95% CI [0.43, 7.65]). However, retirees did not differ significantly from employed individuals in terms of medication adherence (see Table 2, \( β \) = -0.54, p > .05; 95% CI [-5.01, 3.93]). The interaction term indicated that for each unit increase in psychological distress, medication adherence decreased by an additional 0.30 units in unemployed patients compared to employed patients (p < .05; 95% CI [-0.55, -0.06]). Figure 1 illustrates a sharper decrease in medication adherence for unemployed individuals, indicating that the negative effect of psychological distress is stronger for them compared to employed individuals. Retired individuals did not show a significant difference in medication adherence compared to employed individuals (see Table 2, \( β \) = 0.03, SE = 0.15, p > .05; 95% CI [-0.27, 0.33]). ANOVA comparing the models with and without the interaction term indicated that including the interaction term significantly improved model fit (p < .05). Additionally, age and systolic blood pressure were significant predictors of medication adherence (see Table 2, \( β \) = 0.05, SE = 0.01, p < .05; 95% CI [0.02, 0.08]; \( β \) = -0.04, SE = 0.01, p < .05; 95% CI [-0.06, -0.02]).
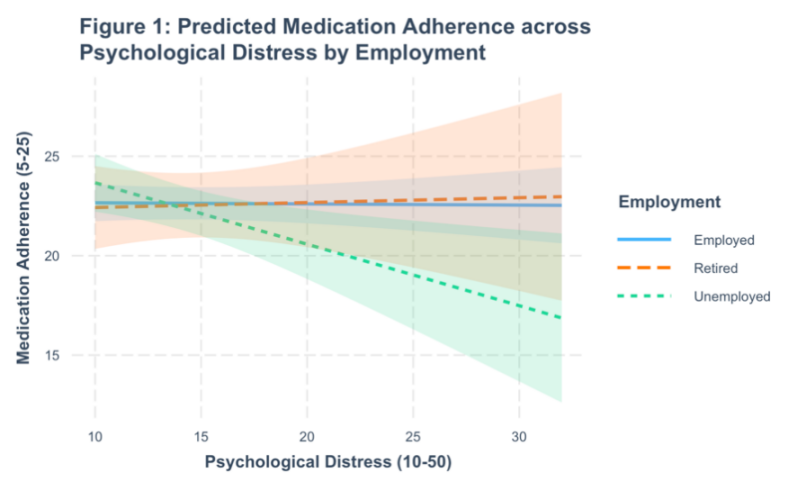
Figure 1. Predicted Medication Adherence Across Psychological Distress by Employment
4.2. Association between Anxiety symptoms/Depression symptoms, Employment Status and Medication Adherence
The model including anxiety symptoms, employment status, and their interaction was significant (F(18, 284) = 4.51, p < 0.05). This model explained 22.24% of the variance in medication adherence, with an adjusted R2 value of 0.17. Only age ( \( β \) = 0.05, SE = 0.01, p < 0.05) and systolic blood pressure ( \( β \) = -0.04, SE = 0.01, p < 0.05) were significant predictors, indicating that younger patients and those with higher systolic blood pressure tend to have poorer medication adherence. The model with depression symptoms, employment status, and their interaction was also significant (F(18, 284) = 4.51, p < 0.05). This model explained 22.24% of the variance in medication adherence, with an adjusted R² value of 0.17. Similarly, only age ( \( β \) = 0.05, SE = 0.01, p < 0.05) and systolic blood pressure ( \( β \) = -0.04, SE = 0.01, p < 0.05) were significant predictors. Older participants and higher systolic blood pressure associated with lower medication adherence.
5. Discussion
In this study, employed participants, younger participants, and participants with higher systolic bold tend to have poor medication adherence. Current research and clinical findings suggest that effective interventions can be achieved through patient health education, management of medication, reminders and providing feedback on blood pressure monitoring [23]. The effectiveness of these interventions can be further improved by focusing more on specific populations during implementation. In addition, psychotherapies are also effective interventions for improving low adherence, such as Motivational Interviewing (MI) [24]. This study found that unemployment exacerbates the negative impact of psychological problems on medication adherence. Therefore, employment status should be considered an important factor in consulting. Targeting the negative psychological effects of unemployment in the intervention can help to improve patients’ medication adherence.
However, there were limitations, one of which was the uneven distribution of participants' employment status, with a larger number of employed participants compared to unemployed and retired participants. Thus, generalizability of the results may be limited because of the small size and limited variability in the unemployed and retired groups. Future research could include a more balanced sample to confirm these results. In addition, testing medication adherence using self-report may be subject to social desirability bias. Participants may underreport the attitudes and behaviors that are socially unexpected or undesirable [25]. As a result, they may less frequently and inaccurately report their non-adherence to medication and thus overestimate their medication adherence [26]. Therefore, the validity and reliability of the findings may be compromised. Further studies could use pharmacy records to measure medication adherence and re-examine this association.
6. Conclusion
This study aimed to test whether employment status influences the association between psychological distress (including anxiety symptom and depression symptom) and medication adherence for patients with hypertension. Through a secondary data analysis, we found the unemployed individuals showed better medication adherence compared to employed individuals. Significantly, the correlation between psychological distress and medicine adherence is contingent upon the employment status of the individual. This correlation is particularly pronounced for individuals who are without jobs, since unemployment amplifies the adverse effects of psychological stress on compliance with therapy. Moreover, there was a positive correlation between age and medication adherence, while a negative correlation was observed between systolic blood pressure and medication adherence. Nevertheless, the applicability of the results may be restricted partly because of the unequal distribution of the three employment categories. Furthermore, the validity and reliability of results may be influenced by social desirability bias arising from self-report measures. Notwithstanding these constraints, the research emphasizes the need of taking into account work position while developing interventions to enhance persons’ adherence to medication, especially in the setting of psychological therapies.
References
[1]. Stanaway, J. D., et al. (2018) Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet, 392(10159), 1923–1994.
[2]. Kretchy, I. A., et al. (2014) Mental health in hypertension: assessing symptoms of anxiety, depression and stress on anti-hypertensive medication adherence. International Journal of Mental Health Systems, 8(1).
[3]. Qiu, T., et al. (2023) Comorbidity of Anxiety and Hypertension: Common Risk Factors and Potential Mechanisms. International Journal of Hypertension, 2023, 1–14Belay,
[4]. Guangul, A.S., (2021) Prevalence and Associated Factors of Psychological Distress among Nurses in Public Hospitals, Southwest, Ethiopia: a cross-sectional Study. Ethiopian Journal of Health Science, 31(6), 1247–1256.
[5]. Hamrahian, S.M., et al. (2022) A Critical Review of Medication Adherence in Hypertension: Barriers and Facilitators Clinicians Should Consider. Patient Preference and Adherence, 16(16), 2749–2757.
[6]. Pristianty, L., et al. (2023) Association between knowledge and adherence to hypertension treatment. Journal of Public Health in Africa.
[7]. Eghbali, M., et al.. (2022) Evaluation of Psychological Distress, Self-Care, and Medication Adherence in Association with Hypertension Control. International Journal of Hypertension, 2022, 1–7.
[8]. Nasrin, N. (2023) Does Employment Status Associate with Physical and Mental Health Status? A Cross-Sectional Study on Working-age Population. Asia Pacific Journal of Health Management.
[9]. Doubova, S.V., et al. (2017) Association of hypertension-related distress with lack of self-care among hypertensive patients. Psychology, Health & Medicine, 22(1), 51–64.
[10]. Bautista, L.E., et al. (2012) Symptoms of depression and anxiety and adherence to antihypertensive medication. American Journal of Hypertension, 25(4), 505–511.
[11]. Affandy, H. (2022) ASSOCIATION BETWEEN ANXIETY LEVEL IN PANDEMIC AND MEDICAL ADHERENCE IN HYPERTENSIVE ELDERLY. Diponegoro International Medical Journal, 3(2), 42–48.
[12]. Stamoulis, T., et al. (2024) Unveiling the Nexus: Depressive Symptoms and Medication Adherence in Hypertensive Patients’ Self-care: A Systematic Review. Materia Socio Medica, 36(1), 65–65.
[13]. Paul, K.I. and Moser, K. (2009) Unemployment impairs mental health: Meta-analyses. Journal of Vocational Behavior, 74(3), 264–282.
[14]. Sidorchuk, A., et al. (2017) Employment status and psychological distress in a population-based cross-sectional study in Sweden: the impact of migration. BMJ Open, 7(4), e014698.
[15]. Lee, G.K.Y., et al. (2013). Determinants of Medication Adherence to Antihypertensive Medications among a Chinese Population Using Morisky Medication Adherence Scale. PLoS ONE, 8(4), e62775.
[16]. Zyczynski, T.M. and Coyne, K.S. (2000). Hypertension and current issues in compliance and patient outcomes. Current Hypertension Reports, 2(6), 510–514.
[17]. Xu, Y., et al. (2019) Poverty and Health Issues in the Northern Part of Ghana.
[18]. Armenti, K., et al. (2023) Work: A Social Determinant of Health Worth Capturing. International Journal of Environmental Research and Public Health, 20(2), 1199.
[19]. Kwakye, Adwoa Oforiwaa (2024) Medication adherence among Adult hypertensive patient, Mendeley Data, V1, doi: 10.17632/zdhnnf6knb.1
[20]. Kessler, R.C., et al.. (2003) Screening for Serious Mental Illness in the General Population. Archives of General Psychiatry, 60(2), 184–189.
[21]. Chan, A.H.Y., et al. (2020) The Medication Adherence Report Scale: A measurement tool for eliciting patients’ reports of nonadherence. British Journal of Clinical Pharmacology, 86(7), 1281–1288.
[22]. Spetz, K., et al. (2024) Using the 5-Item Medication Adherence Report Scale (MARS-5) to Screen for Non-adherence to Vitamin and Mineral Supplementation After Bariatric Surgery. Obesity Surgery, 34(2), 576–582.
[23]. Conn, V.S., et al. (2015) Interventions to Improve Medication Adherence in Hypertensive Patients: Systematic Review and Meta-analysis. Current Hypertension Reports, 17(12).
[24]. Spoelstra, S.L.,et al. (2014). Interventions combining motivational interviewing and cognitive behaviour to promote medication adherence: a literature review. Journal of Clinical Nursing, 24(9-10).
[25]. Latkin, C.A., et al. (2017) The association between social desirability bias and self-reports of health, substance use, and social network factors among urban substance users in Baltimore, Maryland. Addictive Behaviors, 73(1), 133–136.
[26]. Stirratt, M.J., et al. (2015) Self-report measures of medication adherence behavior: recommendations on optimal use. Translational Behavioral Medicine, 5(4), 470–482
Cite this article
Li,R. (2024). Association between Psychological Distress, Employment Status and Medication Adherence among Adult Hypertensive Patient. Theoretical and Natural Science,64,50-56.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 4th International Conference on Biological Engineering and Medical Science
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Stanaway, J. D., et al. (2018) Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet, 392(10159), 1923–1994.
[2]. Kretchy, I. A., et al. (2014) Mental health in hypertension: assessing symptoms of anxiety, depression and stress on anti-hypertensive medication adherence. International Journal of Mental Health Systems, 8(1).
[3]. Qiu, T., et al. (2023) Comorbidity of Anxiety and Hypertension: Common Risk Factors and Potential Mechanisms. International Journal of Hypertension, 2023, 1–14Belay,
[4]. Guangul, A.S., (2021) Prevalence and Associated Factors of Psychological Distress among Nurses in Public Hospitals, Southwest, Ethiopia: a cross-sectional Study. Ethiopian Journal of Health Science, 31(6), 1247–1256.
[5]. Hamrahian, S.M., et al. (2022) A Critical Review of Medication Adherence in Hypertension: Barriers and Facilitators Clinicians Should Consider. Patient Preference and Adherence, 16(16), 2749–2757.
[6]. Pristianty, L., et al. (2023) Association between knowledge and adherence to hypertension treatment. Journal of Public Health in Africa.
[7]. Eghbali, M., et al.. (2022) Evaluation of Psychological Distress, Self-Care, and Medication Adherence in Association with Hypertension Control. International Journal of Hypertension, 2022, 1–7.
[8]. Nasrin, N. (2023) Does Employment Status Associate with Physical and Mental Health Status? A Cross-Sectional Study on Working-age Population. Asia Pacific Journal of Health Management.
[9]. Doubova, S.V., et al. (2017) Association of hypertension-related distress with lack of self-care among hypertensive patients. Psychology, Health & Medicine, 22(1), 51–64.
[10]. Bautista, L.E., et al. (2012) Symptoms of depression and anxiety and adherence to antihypertensive medication. American Journal of Hypertension, 25(4), 505–511.
[11]. Affandy, H. (2022) ASSOCIATION BETWEEN ANXIETY LEVEL IN PANDEMIC AND MEDICAL ADHERENCE IN HYPERTENSIVE ELDERLY. Diponegoro International Medical Journal, 3(2), 42–48.
[12]. Stamoulis, T., et al. (2024) Unveiling the Nexus: Depressive Symptoms and Medication Adherence in Hypertensive Patients’ Self-care: A Systematic Review. Materia Socio Medica, 36(1), 65–65.
[13]. Paul, K.I. and Moser, K. (2009) Unemployment impairs mental health: Meta-analyses. Journal of Vocational Behavior, 74(3), 264–282.
[14]. Sidorchuk, A., et al. (2017) Employment status and psychological distress in a population-based cross-sectional study in Sweden: the impact of migration. BMJ Open, 7(4), e014698.
[15]. Lee, G.K.Y., et al. (2013). Determinants of Medication Adherence to Antihypertensive Medications among a Chinese Population Using Morisky Medication Adherence Scale. PLoS ONE, 8(4), e62775.
[16]. Zyczynski, T.M. and Coyne, K.S. (2000). Hypertension and current issues in compliance and patient outcomes. Current Hypertension Reports, 2(6), 510–514.
[17]. Xu, Y., et al. (2019) Poverty and Health Issues in the Northern Part of Ghana.
[18]. Armenti, K., et al. (2023) Work: A Social Determinant of Health Worth Capturing. International Journal of Environmental Research and Public Health, 20(2), 1199.
[19]. Kwakye, Adwoa Oforiwaa (2024) Medication adherence among Adult hypertensive patient, Mendeley Data, V1, doi: 10.17632/zdhnnf6knb.1
[20]. Kessler, R.C., et al.. (2003) Screening for Serious Mental Illness in the General Population. Archives of General Psychiatry, 60(2), 184–189.
[21]. Chan, A.H.Y., et al. (2020) The Medication Adherence Report Scale: A measurement tool for eliciting patients’ reports of nonadherence. British Journal of Clinical Pharmacology, 86(7), 1281–1288.
[22]. Spetz, K., et al. (2024) Using the 5-Item Medication Adherence Report Scale (MARS-5) to Screen for Non-adherence to Vitamin and Mineral Supplementation After Bariatric Surgery. Obesity Surgery, 34(2), 576–582.
[23]. Conn, V.S., et al. (2015) Interventions to Improve Medication Adherence in Hypertensive Patients: Systematic Review and Meta-analysis. Current Hypertension Reports, 17(12).
[24]. Spoelstra, S.L.,et al. (2014). Interventions combining motivational interviewing and cognitive behaviour to promote medication adherence: a literature review. Journal of Clinical Nursing, 24(9-10).
[25]. Latkin, C.A., et al. (2017) The association between social desirability bias and self-reports of health, substance use, and social network factors among urban substance users in Baltimore, Maryland. Addictive Behaviors, 73(1), 133–136.
[26]. Stirratt, M.J., et al. (2015) Self-report measures of medication adherence behavior: recommendations on optimal use. Translational Behavioral Medicine, 5(4), 470–482