1. Introduction
As a substance obtained by humans from nature, honey is the crystallization of the exquisite craftsmanship of bees. Bees first collect raw materials: nectar (honey) or insect secretions rich in sugar (honeydew honey). The sugar in nectar is first broken down by bee secretions and then modified by other compounds to achieve dehydration. After the nectar matures, it becomes honey, a nutrient rich thick syrup. It mainly contains fructose, glucose, sucrose and water. The skin is the first physical barrier against external sources of infection, consisting of epidermis, dermis, and subcutaneous tissue. A wound refers to skin damage caused by various reasons, put the human body at a disadvantage when fighting against external infectious substances. Once the wound heals, it can restore the skin’s resistance, which is a complex process [1].
Wounds such as burns, ulcers, and postoperative wounds always have a place on the list of common health problems in most countries. The inadequate treatment of these wounds seriously affects normal production, life, and economic development. However, in some countries with limited development, these wounds may cause serious complications because of inadequate treatment measures, and even lead to bacterial infections, requiring treatment with antibiotics. Due to the promotion of antibiotics, many bacteria have developed resistance, resulting in poor treatment outcomes and serious losses [2]. Many technologies and new drugs have been developed to accelerate wound healing and reduce the probability of infection. Therefore, it is important to find an intervention that promotes the healing process and has bactericidal effects. Honey, as a natural product, deserves attention for its antibacterial effect.
Honey has a long history of being used as an antibacterial agent. Some advantages of using honey as a wound healing solution are that it can promote tissue regrowth and has good antibacterial effects [3]. Honey has a penetrating effect, which allows it to form a layer of liquid when used to treat wounds, separating the dressing from the wound bed, which creates a moist environment when using honey to treat burns and helps maintain the integrity of the burn surface, thereby reducing or eliminating pain during the removal and replacement of wound dressings, avoiding damage to newly formed tissue, and shortening the healing time. Because it does not adhere, it can serve as a barrier to reduce the risk of wound infection [4].
In terms of antibacterial effect, for one thing, on the basis of the general antibacterial effect on most bacteria, honey can also eliminate some bacteria that have developed drug resistance. When honey and antibiotics work together, some antibiotics that have lost efficacy due to bacterial resistance can also recover their efficacy [5-7]. As shown in Figure 1, honey contains multiple antibacterial ingredients with different mechanisms of action, making it unlikely for bacteria to develop resistance to honey [8, 9].
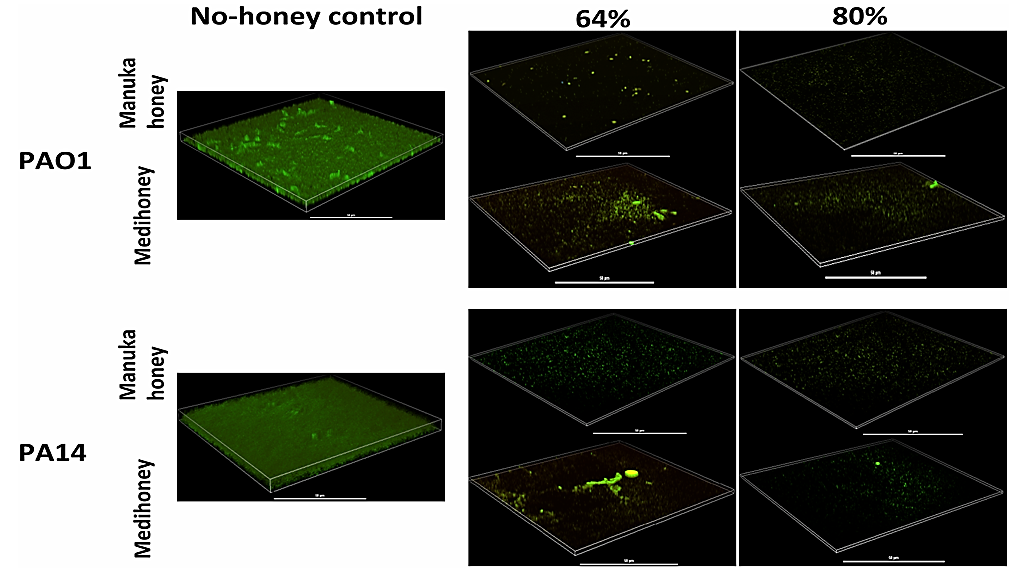
Figure 1. Effects of different concentrations of honey on P. aeruginosa biofilms [8].
At present, there have been many cases in which honey has been used in clinic, such as adding honey to hydrogel dressing, or directly using medical grade honey as wound covering. This research mainly discusses the influence of honey varieties and honey usage methods on treatment effectiveness, the impact of honey treatment on different wounds, and the ability of honey to lighten scars.
2. The role of honey in treating wounds
Honey can be used directly or added to dressings and other substances to participate in the healing process of wounds. Honey mainly exhibits the following effects in the treatment of wounds. Honey has excellent antibacterial properties and is also effective against bacteria that form biofilms and drug-resistant bacteria that are difficult to handle. When using honey with antibiotics, reducing the dosage of antibiotics can also achieve the expected effect. After tissue damage, free radicals are released, which can cause further damage to the tissue. Honey can reduce the damage it causes, while also reducing prostate concentration to alleviate pain and regulating wound exudate through appropriate water balance. The high osmotic pressure brought by honey can automatically discharge the accumulated lymphatic fluid in the wound, and the moist environment it creates is also conducive to wound autolysis and debridement. Honey can stimulate cell growth and repair tissue development, as well as promote angiogenesis [10]. In summary, the physical and chemical properties of honey make it effective in treating wounds.
3. Analysis of therapeutic effect
3.1. Selection of honey types and different application methods in treatment
Most honey can resist bacteria because they release small amounts of hydrogen peroxide and have a mild acidity, but some non-peroxide honey can also disinfection and sterilization bacteria. Manuka honey also has excellent antibacterial effects when blocked from releasing hydrogen peroxide. The methylglyoxal content in Manuka honey gives it excellent antibacterial ability, and its slight acidity and high sugar content may also be involved in the antibacterial process. Many honey products currently available on the market can meet certain antibacterial requirements, with Leptospermum scoparium (L. scoparium) honey being the most famous and effective, as it can inhibit the activity of various bacteria [11].
Medihoney and Manuka honey are mainstream antibacterial honey on the market. Honey from different regions and flower sources also has antibacterial activity comparable to commercially available antibacterial honey against certain bacteria [12]. As the mainstream medical honey for treating wounds, Manuka honey has been widely used in clinical practice. It has undergone extensive research by scientists and has become the first among many types of honey to become medical grade honey. It has also been officially recommended as a substitute for treating wounds. It was approved by the US Food and Drug Administration in 2007 as a recommended alternative for treating wounds. Manuka honey comes from the Leptospermum scoparium plant. It has a high content of methylglyoxal (MGO), making it stand out among many medicinal honeys. MGO is an antioxidant and fungicide that can help Manuka honey enhance its ability to promote healing and better kill bacteria.
The main schemes for applying honey to clinical wound treatment include directly applying medical grade honey, using hydrogel, fiber membrane and ointment added with honey. The use of honey alone still faces some problems in clinical applications, which are gradually improving with the advancement of dressing formulations [10]. Medical grade honey has antibacterial properties and can promote wound healing. Compared with other wound care products, it has multiple advantages and can assist in the treatment of various types of wounds, and is cost-effective. However, directly applying high concentration medical grade honey to the wound can cause a stinging sensation, and attention should be paid when using [13]. There are efficiency issues with using only medical grade honey and gauze for treatment, as multiple dressing changes and the application of new honey are necessary to prevent the honey from leaving the wound due to fluidity [14].
Compared to directly applying honey, the use of wound dressings is more convenient. There are currently various wound dressings related to honey on the market. These products have been approved by the FDA and can be used for medical purposes with different indications. These dressings protect wounds, promote healing, and allow exudate to pass through. Most of them have the effects of creating a moist healing environment, antibacterial, debridement, and reducing odors [14].
3.2. The effect of honey in treating different wounds
Thanks to the non-adhesive properties of medical grade honey, the dressing will not cause any damage to the skin around the wound when removed [13]. Honey and photobiomodulation therapy were found to be most beneficial for burn wound healing and epithelial regrowth compared to any other therapy used alone, and can alleviate inflammation and pain during the healing process [15]. The epithelialization and healing speed of the area treated with honey is significantly faster than that of the area treated with traditional local burn treatment drug sulfamethoxazole silver (SSD). In addition, compared to the area treated with SSD, the possibility of bacterial infection in the honey treated area is lower [16, 17].
Medical grade honey has also played an excellent role in the treatment of vascular leg ulcers (vascular ulcers should be combined with MGH ointment or gel and MGH foam dressing). Manuka honey has also been proved to shorten the time required for wound healing in the treatment of diabetes foot, increase debridement and bacterial clearance rate [18], and will not increase blood glucose level after MGH treatment. MGH has been shown to significantly accelerate the healing of pressure ulcer wounds, while also providing faster pain relief and reducing discomfort during dressing changes. It has the effect of quickly deodorizing and cleaning wounds when treating mushroom shaped wounds [13].
3.3. The effect of honey on scars
Manuka dressings can significantly reduce wound size, shorten healing time, and alleviate pain when used to treat various wounds [19-21]. Honey dressings can not only promote wound healing but also reduce scar width during postoperative recovery in plastic surgery, which is beneficial for the final aesthetic effect after wound recovery. In the comparison of scar conditions at different time points after surgery, the use of honey is more beneficial for reducing scar area compared to traditional dressings [22]. Open thyroidectomy will leave patients with scars about 8 centimeters long, the use of honey resulted in less pigment precipitation in scars, which is more conducive to scar fading. However, in terms of other aspects of scar recovery, the honey group’s effect was not significant [23].
In the healing of eye and face wounds, some patients claimed that honey could accelerate scar fading and relieve wound stiffness in the first week, but after four months, these effects gradually became less apparent. A small number of people believe that honey can alleviate pain during the treatment process. It can be considered that honey has a relatively small impact on the healing of eye and facial wounds, and may have subjective benefits for some patients [24]. In a local wound healing experiment on cats and dogs, researchers compared the therapeutic effects of honey with new medical devices and found that the effect of manuka honey was not significant [25].
4. Conclusion
Honey, as a natural substance containing multiple compounds, can assist in wound healing from both physical and chemical perspectives. It generally has antibacterial activity and potential utilization value, and has promotional value. Research on honey mainly focuses on mainstream medical honey such as manuka honey, while other types of honey also have potential medicinal value that is different from mainstream honey. Subsequent research can further study different types of honey and develop their effectiveness in different aspects. In addition, a widely recognized fact at present is that honey can indeed help wounds heal better in various ways, but there is still limited research on beautifying scars, and the universality of scar repair results is not strong. Further in-depth and larger sample size research is still needed, only in this way can we better confirm the specific repair effect of honey in scar beautification.
References
[1]. Kus KJB, Ruiz ES 2020 Curr. Dermatol. Rep. 9 298-308
[2]. Huang X, Bao X, Liu Y, et al. 2017 Scientific reports 7(1) 1860
[3]. Scepankova H, Combarros-Fuertes P, Fresno J M, et al. 2021 Molecules 26(16) 4784
[4]. Molan PC 2011 Wound Pract. Res. 19 204-220
[5]. Combarros-Fuertes P, Fresno J M, Estevinho M M, et al. 2020 Antibiotics 9(11) 774
[6]. Campeau M E M, Patel R. 2014 International journal of bacteriology 2014(1) 795281
[7]. Hayes G, Wright N, Gardner S L, et al. 2018 Letters in applied microbiology 66(6) 491-495
[8]. Lu J, Cokcetin N N, Burke C M, et al. 2019 Scientific reports 9(1) 18160
[9]. Maddocks S E, Jenkins R E. 2013 Future microbiology 8(11) 1419-1429
[10]. Scepankova H, Combarros-Fuertes P, Fresno J M, et al. 2021 Molecules 26(16) 4784
[11]. Molan P C 1992 Bee world 73(1) 5-28
[12]. Lusby P E, Coombes A L, Wilkinson J M. B 2005 Archives of medical research 36(5) 464-467
[13]. Chrysostomou D, Pokorná A, Cremers N A J, et al. 2024 JAR life 13 51
[14]. Angioi R, Morrin A, White B. 2021 Applied sciences 11(11) 5192
[15]. Yadav A, Verma S, Keshri G K, et al. 2018 Journal of Photochemistry and Photobiology B: Biology 186 152-159
[16]. Malik K I, Malik M A N, Aslam A. 2010 International Wound Journal 7(5) 413-417
[17]. Wijesinghe M, Weatherall M, Perrin K, et al. 2009 Database of Abstracts of Reviews of Effects (DARE): Quality-assessed Reviews [Internet]
[18]. Kamaratos A V, Tzirogiannis K N, Iraklianou S A, et al. 2014 International wound journal 11(3) 259-263
[19]. Biglari B, Simon A, Aytac S, et al. 2012 Spinal cord 50(2) 165-169
[20]. Kamaratos A V, Tzirogiannis K N, Iraklianou S A, et al. 2014 International wound journal 11(3) 259-263
[21]. Jarjis R D, Crewe B T, Matzen S H 2016 International Journal of Surgery Case Reports 20 1-3
[22]. Goharshenasan P, Amini S, Atria A, et al. 2016 Forschende Komplementärmedizin/Research in Complementary Medicine 23(1) 12-15
[23]. Thamboo A, Mulholland G, Matthews K, et al. 2016 World Journal of Otorhinolaryngology-Head and Neck Surgery 2(4) 203-207
[24]. Malhotra R, Ziahosseini K, Poitelea C, et al. 2017 Ophthalmic Plastic & Reconstructive Surgery 33(4) 268-272
[25]. Gouletsou P G, Zacharopoulou T, Skampardonis V, et al. 2024 Veterinary Sciences 11(2) 64
Cite this article
Xiao,Y. (2024). The application of honey in treating wounds. Theoretical and Natural Science,64,143-147.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 4th International Conference on Biological Engineering and Medical Science
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Kus KJB, Ruiz ES 2020 Curr. Dermatol. Rep. 9 298-308
[2]. Huang X, Bao X, Liu Y, et al. 2017 Scientific reports 7(1) 1860
[3]. Scepankova H, Combarros-Fuertes P, Fresno J M, et al. 2021 Molecules 26(16) 4784
[4]. Molan PC 2011 Wound Pract. Res. 19 204-220
[5]. Combarros-Fuertes P, Fresno J M, Estevinho M M, et al. 2020 Antibiotics 9(11) 774
[6]. Campeau M E M, Patel R. 2014 International journal of bacteriology 2014(1) 795281
[7]. Hayes G, Wright N, Gardner S L, et al. 2018 Letters in applied microbiology 66(6) 491-495
[8]. Lu J, Cokcetin N N, Burke C M, et al. 2019 Scientific reports 9(1) 18160
[9]. Maddocks S E, Jenkins R E. 2013 Future microbiology 8(11) 1419-1429
[10]. Scepankova H, Combarros-Fuertes P, Fresno J M, et al. 2021 Molecules 26(16) 4784
[11]. Molan P C 1992 Bee world 73(1) 5-28
[12]. Lusby P E, Coombes A L, Wilkinson J M. B 2005 Archives of medical research 36(5) 464-467
[13]. Chrysostomou D, Pokorná A, Cremers N A J, et al. 2024 JAR life 13 51
[14]. Angioi R, Morrin A, White B. 2021 Applied sciences 11(11) 5192
[15]. Yadav A, Verma S, Keshri G K, et al. 2018 Journal of Photochemistry and Photobiology B: Biology 186 152-159
[16]. Malik K I, Malik M A N, Aslam A. 2010 International Wound Journal 7(5) 413-417
[17]. Wijesinghe M, Weatherall M, Perrin K, et al. 2009 Database of Abstracts of Reviews of Effects (DARE): Quality-assessed Reviews [Internet]
[18]. Kamaratos A V, Tzirogiannis K N, Iraklianou S A, et al. 2014 International wound journal 11(3) 259-263
[19]. Biglari B, Simon A, Aytac S, et al. 2012 Spinal cord 50(2) 165-169
[20]. Kamaratos A V, Tzirogiannis K N, Iraklianou S A, et al. 2014 International wound journal 11(3) 259-263
[21]. Jarjis R D, Crewe B T, Matzen S H 2016 International Journal of Surgery Case Reports 20 1-3
[22]. Goharshenasan P, Amini S, Atria A, et al. 2016 Forschende Komplementärmedizin/Research in Complementary Medicine 23(1) 12-15
[23]. Thamboo A, Mulholland G, Matthews K, et al. 2016 World Journal of Otorhinolaryngology-Head and Neck Surgery 2(4) 203-207
[24]. Malhotra R, Ziahosseini K, Poitelea C, et al. 2017 Ophthalmic Plastic & Reconstructive Surgery 33(4) 268-272
[25]. Gouletsou P G, Zacharopoulou T, Skampardonis V, et al. 2024 Veterinary Sciences 11(2) 64