1. Introduction
Osteoarthritis (OA) is a costly inflammatory joint degenerative disease that affects millions of patients around the globe. Patients with OA are characterized by the breakdown of cartilage in the joints, and it incurs common symptoms such as progressively increasing pain and results in decreased quality of life due to the side effects of this disease and the expensive medical bills that come alongside [1]. Cartilage is an important structure that cushions bone to bone impact during joint movement. Damaging of this tissue could lead to clinical pathologies. Cartilage tissue exhibits several unique characteristics such as a less abundant blood supply, lack of lymphatic drainage, and sparse nerve distribution, which limit cartilage's ability to self-repair, making treatment difficult for diseases that involve the breakdown of natural cartilage, such as OA. Therefore, the fabrication of tissue-engineered cartilage in a laboratory to replace the damaged cartilage in OA patients has become an increasingly popular therapy that has been investigated by scientists [2].
Current therapies include palliative treatments, which only alleviate symptoms and cannot prevent further cartilage degeneration, surgical therapies, which have some effective effects yet limited in ways depending on the specific type, and tissue engineering, which is efficient in regenerating cartilage, yet face some ethical tissues [2]. Therefore, a major focus in treating these diseases is the attempt to regenerate new cartilage to replace the degenerated, diseased cartilage. Conservative treatments for osteoarthritis (OA), including hyaluronic acid injections, analgesics, and non-steroidal anti-inflammatory drugs (NSAIDs), are commonly recommended in treatment guidelines. However, their actual therapeutic effects are minor [2]. Tissue engineering through surgical therapies is a primary focus in treating OA. Cartilage regeneration techniques, according to the latest scientific advancements, encompass several methods. These include the microfracture method, which stimulates the body's natural healing process, osteochondral transplantation, where healthy bone and cartilage are transplanted to the defect site, and autologous chondrocyte implantation, where lab-grown chondrocytes are implanted to repair damaged cartilage and cell-Scaffold Construct Strategies, which utilize stem cells or chondrocytes, with or without in vitro expansion, to facilitate cartilage repair. iPSCs is promising to apply on cartilage regeneration because it is an effective cell source for the regeneration for the regeneration of cartilage [2].
This review summarizes current technological advancements in cartilage regeneration, with a focus on the application of induced pluripotent stem cells and its potential in OA therapy. This review aims to cover various methods employed for cartilage repair, including Cell-Scaffold Construct Strategies, microfracture, osteochondral transplantation, and chondrocyte implantation. Additionally, this review summarizes the latest research on in vitro and in vivo studies and evaluates the outcomes of clinical trials related to cartilage regeneration. Finally, it will highlight future directions and emerging trends in the field.
2. Technology
2.1. Cartilage regeneration
Cartilage is a specialized tissue that is found in various joints and structures throughout the body, and it plays a crucial role in regulating joint function and pain. Due to its avascular and aneural nature, the ability of cartilage tissue to naturally repair and regenerate itself when damaged is greatly restricted. This means that cartilage tissue receives fewer nutrients and has less access to the body's natural healing processes [2]. Therefore, when cartilage tissue is damaged, the body's response to the wound is less robust than it would be for other tissues. If the damage is not addressed properly, this special quality of cartilage makes it prone to developing long-term functional impairments such as osteoarthritis.
Over the past three decades, numerous treatment techniques and commercial products have been developed to promote the repair and regeneration of defective cartilage. Before the advent of regenerative medicine and tissue engineering as mainstream therapies for OA and other joint diseases, palliative treatment was the most common treatment to manage OA and its symptoms. However, in contrast to the regenerative medicine approach, palliative treatments focused on relieving symptoms rather than addressing the underlying cause of the disease. These treatments included non-steroidal anti-inflammatory drugs, analgesics therapy, corticosteroid injection and injection lubricants, such as hyaluronic acid. After demonstrating the regenerative ability of cartilage in an experiment where cow chondrocytes were seeded into a biodegradable ear-shaped scaffold and successfully implanted in mice, there was a significant shift in a significant shift towards the application of tissue engineering in regenerative medicine [2]. Various cell types, scaffolds, and specific microenvironments were used and manipulated to create biologically compatible cartilage constructs. Cell engineering technology has been continuously evolving.
Starting with Pridie’s Drilling Method in 1959, where holes were drilled in the articular cartilage to stimulate repair, it was later refined to the microfracture method by Steadman in 1980. The goal of the microfracture method (MF) is to create holes in the subchondral bone which will release bone marrow and form a mesenchymal stem cell and growth factor dense clot. These stem cells will later differentiate into chondrocytes and repair the cartilage. Another common method that utilizing tissue engineering principles is called Osteochondral Transplantation and it utilizes a surgical procedure called transplanting osteochondral plugs [2]. This method is divided into autologous, which is using the patient's own tissue and allogeneic, which is using donor tissue, transplantation. Autologous transplantation is limited by the availability of healthy cartilage various issues that comes with integration while allogeneic transplantation is able larger defects comes with risks of disease transmission and limited donor supply. Osteochondral Transplantation includes various subgroup techniques [2]. Table 1 summarizes the advantages and limitations of current surgical therapies. For instance, Particulated Articular Cartilage Implantation is a variation that involves implanting crushed cartilage particles into defects. It requires less donor cartilage and results in less donor site damage compared to Autologous Chondrocyte Implantation (ACI), which involves harvesting chondrocytes, expanding them in vitro, and implanting them into the defects. ACI has undergone various technical updates since its appearance in 1994. The third generation, Matrix-Induced Autologous Chondrocyte Implantation (MACI), is an advanced tissue engineering technique that uses a scaffold to support cell implantation MACI has shown better therapeutic effects for larger defects, but it requires two surgeries, so it elongates the recovery time, and is more costly [2].
Table 1. The limitations and advantages of surgical therapies.
Types | Limitation | Advantages |
Microfracture (MF) | Limited repaired defect size | Easy to operate Low cost |
Osteochondral Transplantation (OCT) | Transplant cartilage has difficulty integrating into surrounding cartilage | Rapid healing No immune rejection |
Autologous Chondrocyte Implantation (ACI) | Long recovery time (6-12months) | No risk of disease transmission Less trauma formation |
2.2. Induced pluripotent stem cells (iPSCs)
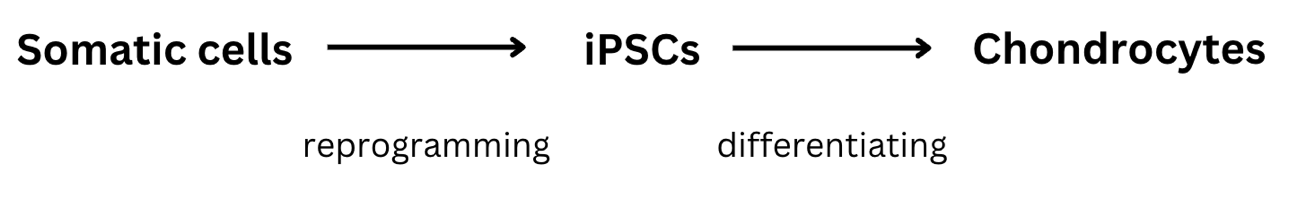
As the field of tissue engineering continues to advance, the focus of therapy for cartilage repair has again shifted toward more innovative and effective treatments. This breakthrough is made possible by the use and introduction of Induced Pluripotent Stem Cells (iPSCs). In the process of looking for better approaches, it has been observed that there has been an exponential increase in the use of stem cells. They are unspecialized cells that can proliferate and differentiate into any kind of functional cell. In the context of OA treatment, stem cells could be utilized to differentiate into chondrocytes (Figure 1). There are a few types of stem cells available for consideration in therapy. For instance, mesenchymal stem cells (MSCs) are cells that are easily acquired and yield some promising results for cartilage repair, yet they leave some questions about their suitability for cartilage tissue engineering due to issues such as cell ossification and fibrocartilage formation. Alternatively, embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs) are additional options worth considering. Both are pluripotent stem cells with the ability to differentiate into many kinds of cell types. However, the use of ESCs is often restricted due to the ethical dilemmas they present [3]. As a result, iPSCs have become an increasing point of interest for investigation as it offers a promising therapeutic application in cartilage repair.
|
Figure 1. Schematic representation of somatic cell reprogramming to iPSCs and subsequent chondrogenic differentiation. Figure credit: original. |
iPSCs are generated by reprogramming non-nucleated somatic cells to revert to their pluripotent state. This process restores their capacity to differentiate into various cell types, including chondrocytes for cartilage repair [4]. These cells can be generated from a patient's own somatic cells, which is a significant advantage as it eliminates the risk of immune rejection that is typically associated with allogeneic cell therapies. Moreover, the use of iPSCs alleviates the ethical concerns associated with embryonic stem cells, as their derivation does not require the destruction of embryos [5]. The potential of iPSCs in cartilage repair has been demonstrated through various studies. In preclinical models, iPSCs that have been predifferentiated towards the chondrogenic lineage have effectively repaired cartilage defects. For example, when human iPSC-induced mesenchymal stem cells were plated onto a PLGA scaffold and transplanted into cartilage defects in animal models, cartilage-like tissue formation was observed [6].
Moreover, the use of nanofiber-based polyether sulfone scaffolds for culturing undifferentiated iPSCs has shown to enhance their chondrogenic differentiation, suggesting that such scaffolds could provide an optimal microenvironment for iPSCs to develop into chondrocyte-like cells. This approach has shown promising results in animal models, with higher expression of chondrogenic markers and improved restoration of cartilage defects compared the control groups [7]. Though offers the potential for a patient specific ethically uncomplicated solution for cartilage repair, iPSCs in tissue engineering comes a crucial safety concern: the potential risk of teratoma formation, tumours that can arise from pluripotent stem cells if they are not fully differentiated [8].
3. Applications
3.1. In vitro and in vivo
The use of iPSCs for cartilage regeneration has been thoroughly researched in both in vitro and in vivo. Under in vitro conditions, efforts have been made to guide the differentiation of iPSCs into lineages that produce cartilage-like tissues. This procedure incorporates specific growth factors and culture conditions designed to replicate chondrocytes' natural developmental processes. The in vitro environment allows for precise control over cellular differentiation and the opportunity to study the early stages of cartilage formation in a controlled setting. In vitro, iPSCs are manipulated to differentiate into specific cell lineages, such as mesodermal and ectomesodermal lineages, which give rise to chondrocytes responsible for cartilage formation. After comparing the performance of differentiation and functional capabilities of mesodermal cell-derived chondrocytes (MC-Chs) and neural crest cell-derived chondrocytes (NCC-Chs), it was found that the NCC-Chs exhibit a closer resemblance to native articular chondrocytes in terms of morphology and gene expression, indicating the superior level of NCC-Chs in cartilage tissue engineering [9].
On the other hand, in vivo studies have aimed to assess the potential of iPSC-derived chondrocytes to integrate and function within living organisms. Animal models, particularly rodents and primates, have been used to implant these cells and evaluate their ability to repair or regenerate damaged cartilage. The in vivo environment provides a more complex and dynamic context, closely resembling the conditions that the regenerated cartilage would face in clinical applications. In vivo, these stem cells are implanted into animal models and assessed for their ability to regenerate cartilage. It is shown that NCC-Ch implants lead to increased matrix production and stiffness, suggesting that they are more effective in forming hyaline cartilage-like tissue compared to MC-Ch implants [9].
3.2. Clinical trials
The translation of iPSC-based cartilage regeneration into clinical practice is a burgeoning field. Ongoing clinical trials are focused on determining the safety and effectiveness of iPSC-derived chondrocytes for cartilage repair. These trials aim to assess the potential of iPSCs to restore cartilage tissue in patients with joint diseases, such as OA. MSCs have demonstrated potential in iPSC generation, showing promise for differentiating into a variety of cell types, particularly those involved in tissue regeneration. However, there are concerns about the transmission of etiological abnormalities from source cells to iPSCs and their derivatives, which could, in turn, affect the therapeutic efficacy of these cells. Some current data suggest that there is no difference between iPSCs from healthy and sick donors, while other studies suggest otherwise. For example, in an experiment where iPSCs were created using fibroblast from a patient who has sever skeletal dysplasia, it was found that when the iPSCs were promoted to differentiate into cartilage cells, they secreted extracellular matrix that was both reduced in quantity and abnormal in quality compared to what is typically observed in healthy cartilage development. This suggest that source of iPSCs can affect their potential use in therapies. In the same experiment, it was also noted that iPSCs derived from patient responded differently to certain growth factors such as BMP2 and TPDβ, which usually would encourage differentiation of stem cells into cartilage cells. For example, it is current known that obtaining autologous iPSCs lines enable the possibility of making chondrogenic constructs that is specific to every patient. Currently there has been successful transplantations of differentiated iPSC cells into autologous cells. For these cases, no serious health consequences were noted, signifying a successful transplantation [10]. The discrepancies between studies indicate the need for further research and suggest that clinical trials must carefully consider the source of MSCs and the potential impact of epigenetic memory on iPSC differentiation and functionality.
4. Conclusion
Osteoarthritis poses significant challenges for the health of citizens around the globe. Its degenerative impact on joint cartilage leads to diminished quality of life for millions of people. Though traditional treatments, such as palliative care, offer symptomatic relief, they often fall short when addressing the underlying cartilage regeneration. The emergence of tissue regeneration in the field of regenerative medicine, particularly the appearance of induced pluripotent stem cells, has shed light on the potential for creating personalized and effective therapies for this joint disease. This specific stem cell source, while possessing the unique potential to differentiate into chondrocytes, also bypasses the ethical and immunological dilemmas associated with other stem cell sources such as ESCs. Preclinical studies have shown the potential for integrating iPSCs-derived chondrocytes within living organisms, with results such as restored cartilage tissue and improved matrix production and stiffness. However, even though iPSCs hold significant potential in advancing the field of regenerative medicine, they come with several safety hazards, such as the risk of teratoma formation and impacting epigenetic memory during iPSC differentiation. Currently, clinical trials are still in their beginning stages. Despite the challenges and safety hazards associated with iPSCs, their potential therapeutic value in revolutionizing the field is undeniable. Therefore, ongoing research, clinical trials, and a deeper understanding of these tools are crucial in developing personalized and effective therapies that will, in turn, enhance the quality of life for those suffering from degenerative joint diseases.
References
[1]. Abramoff B and Caldera FE 2020 Med. Clin. North Am. 104 293-311
[2]. Guo X, Ma Y, Min Y, Sun J, Shi X, Gao G, Sun L and Wang J 2022 Bioact. Mater. 20 501-518
[3]. Reina-Mahecha A, Beers MJ, van der Veen HC, Zuhorn IS, van Kooten TG and Sharma PK 2023 Tissue Eng. Regen. Med. 20 1041-1052
[4]. Ali EAM et al. 2024 Stem Cell. Res. Ther. 26 15 185
[5]. Liu X, Li W, Fu X and Xu Y. 2017 Front. Immunol. 2 8 645
[6]. Bai HY, Chen GA, Mao GH, Song TR and Wang YX 2010 J. Biomed. Mater. Res. A. 94 539-46
[7]. Liu J et al. 2014 PLoS One. 10 1371
[8]. Castro-Viñuelas R et al. 2018 Eur. Cell. Mater. 36 96-109
[9]. Zujur D et al. 2023 Front. Cell. Dev. Biol. 11 1140717
[10]. Eremeev A and Pikina A and Ruchko Yand Bogomazova 2023 Int. J. Mol. Sci. 24 14408.
Cite this article
Sekely,C.A. (2024). Applications of iPSCs on Cartilage Regeneration. Theoretical and Natural Science,71,6-10.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of ICBioMed 2024 Workshop: Computational Proteomics in Drug Discovery and Development from Medicinal Plants
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Abramoff B and Caldera FE 2020 Med. Clin. North Am. 104 293-311
[2]. Guo X, Ma Y, Min Y, Sun J, Shi X, Gao G, Sun L and Wang J 2022 Bioact. Mater. 20 501-518
[3]. Reina-Mahecha A, Beers MJ, van der Veen HC, Zuhorn IS, van Kooten TG and Sharma PK 2023 Tissue Eng. Regen. Med. 20 1041-1052
[4]. Ali EAM et al. 2024 Stem Cell. Res. Ther. 26 15 185
[5]. Liu X, Li W, Fu X and Xu Y. 2017 Front. Immunol. 2 8 645
[6]. Bai HY, Chen GA, Mao GH, Song TR and Wang YX 2010 J. Biomed. Mater. Res. A. 94 539-46
[7]. Liu J et al. 2014 PLoS One. 10 1371
[8]. Castro-Viñuelas R et al. 2018 Eur. Cell. Mater. 36 96-109
[9]. Zujur D et al. 2023 Front. Cell. Dev. Biol. 11 1140717
[10]. Eremeev A and Pikina A and Ruchko Yand Bogomazova 2023 Int. J. Mol. Sci. 24 14408.