1. Introduction
Papillomaviruses are double-stranded DNA viruses that infect mucosal and cutaneous epithelia of a variety of higher vertebrates in a species-specific manner and induce cellular proliferation [1]. Human papillomavirus (HPV) is from the Papillomaviridae family [2]. HPV is one of the common sexually transmitted viruses [3]. It is associated with cervical cancer, the fourth most common cancer among women globally [3]. HPV poses an important public health challenge because of its high infectivity and widespread presence and may cause significant long-term effects [4]. To prevent the development of cancers and reduce the risk of cancers, HPV vaccines have been developed. Vaccines do not contain any live virus or DNA from the virus which means they are safe. The reason is that they do not have ability to cause cancer or other HPV-related disease. HPV vaccines are not used for treating HPV infections or diseases which HPV causes [5]. They are effective in preventing HPV infection and have been routinely offered in many countries worldwide [3]. Low - and middle-income countries exhibit the highest cervical cancer incidence and mortality [5]. This reflects an inequality. People in these countries are exposed to this major inequity due to a lack of access to national HPV vaccination, cervical screening and treatment services, and social and economic determinants [5]. Like any vaccination, HPV vaccination is promoted and applied by healthcare institutions and disease control agencies in countries as a simple and easily implemented means. Despite the benefits of HPV vaccination, HPV vaccination rates are still not meet the target [4]. In this case, how to achieve or even exceed the vaccine coverage target becomes a question worthy of further consideration by researchers in the field of health care. People's attitudes and willingness to receive HPV vaccine are also worthy of exploration. They are influenced by many different factors besides their personal emotions. Identifying these influencing factors can help health care facilities and organizations to better implement vaccination. Since HPV vaccination has been implemented in many different countries around the world, it provides favorable conditions for intercultural research. Intercultural research is conducive to the improvement of global public health policies, global health, and the improvement of human quality of life.
This review will focus on the HPV vaccine coverage in different countries, the public's attitude towards HPV vaccination and the factors influencing their attitude. It will discuss the relationship between public attitudes towards HPV vaccination and vaccination rates in different countries. This review will also explore and try to make recommendations in the field of health in various regions, to spread health knowledge more widely, reduce the prevalence of HPV and improve the level of reproductive health of the population.
2. HPV Vaccination coverage rate
HPV vaccination coverage can be regarded as an objective indicator to assess the status of HPV vaccination. The presentation of WHO's global statistics for 2023 is shown in Figure 1.
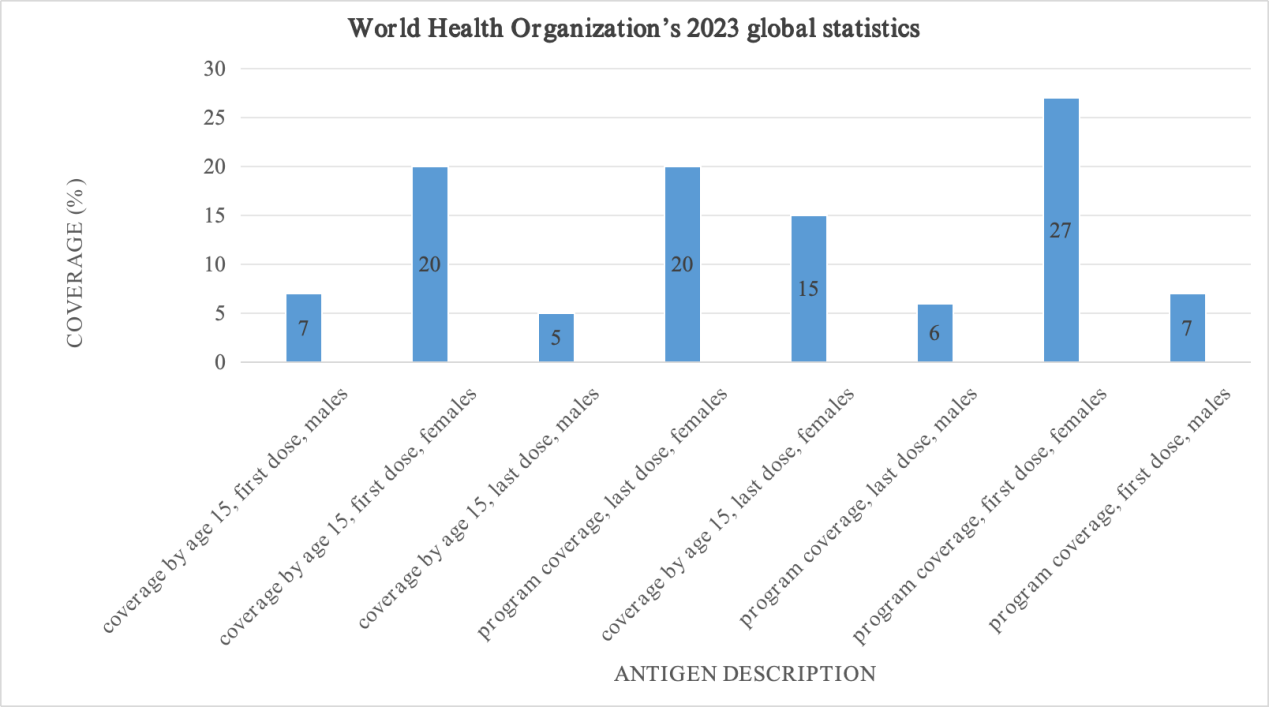
Figure 1: World Health Organization’s 2023 global statistics [6].
Next, HPV vaccination coverage in five geographic regions (Asia, Americas, Europe, Africa, and Australia) will be discussed.
2.1. Asia
The presentation of WHO's 2023 statistics for the Southeast Asia region is shown in Figure 2.
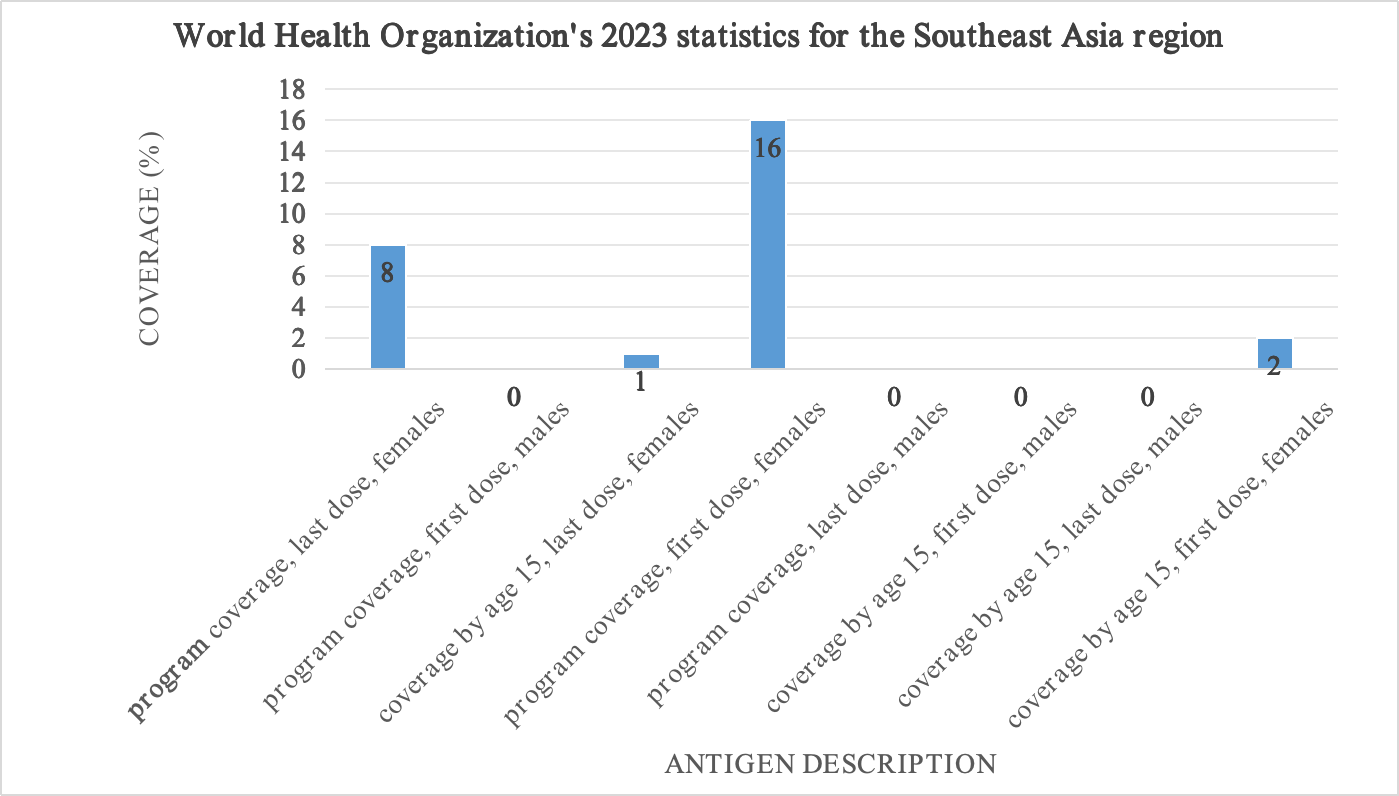
Figure 2: World Health Organization's 2023 statistics for the Southeast Asia region [7].
HPV vaccination coverage in Southeast Asia is lower than global data. This suggests that health professionals need to invest more efforts in promoting HPV vaccine to improve vaccination coverage.
2.2. Americas
The presentation of WHO's 2023 statistics for the Americas region is shown in Figure 3.
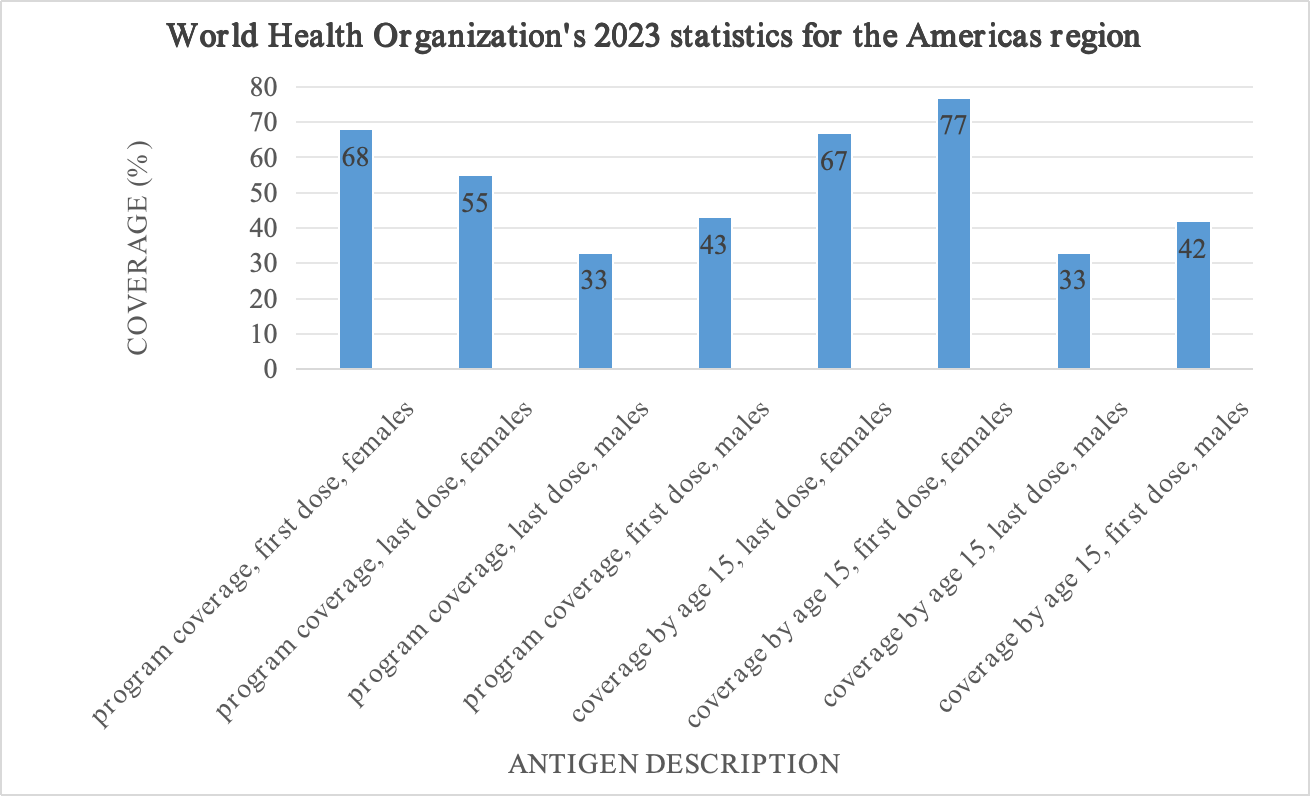
Figure 3: World Health Organization's 2023 statistics for the Americas region [7].
HPV vaccination coverage in the Americas largely exceeds global figures. Compared with the Southeast data, these data suggest that the Americas may have a higher level of livelihood literacy and higher quality health care services for its citizens because of its more developed economic, education and health systems. The reason is that the Americas are more developed than Southeast Asia.
2.3. Europe
HPV vaccination is currently recommended in 23 European Union (EU) and European Economic Area (EEA) member states [8]. The presentation of WHO's 2023 statistics for the European region is shown in Figure 4.
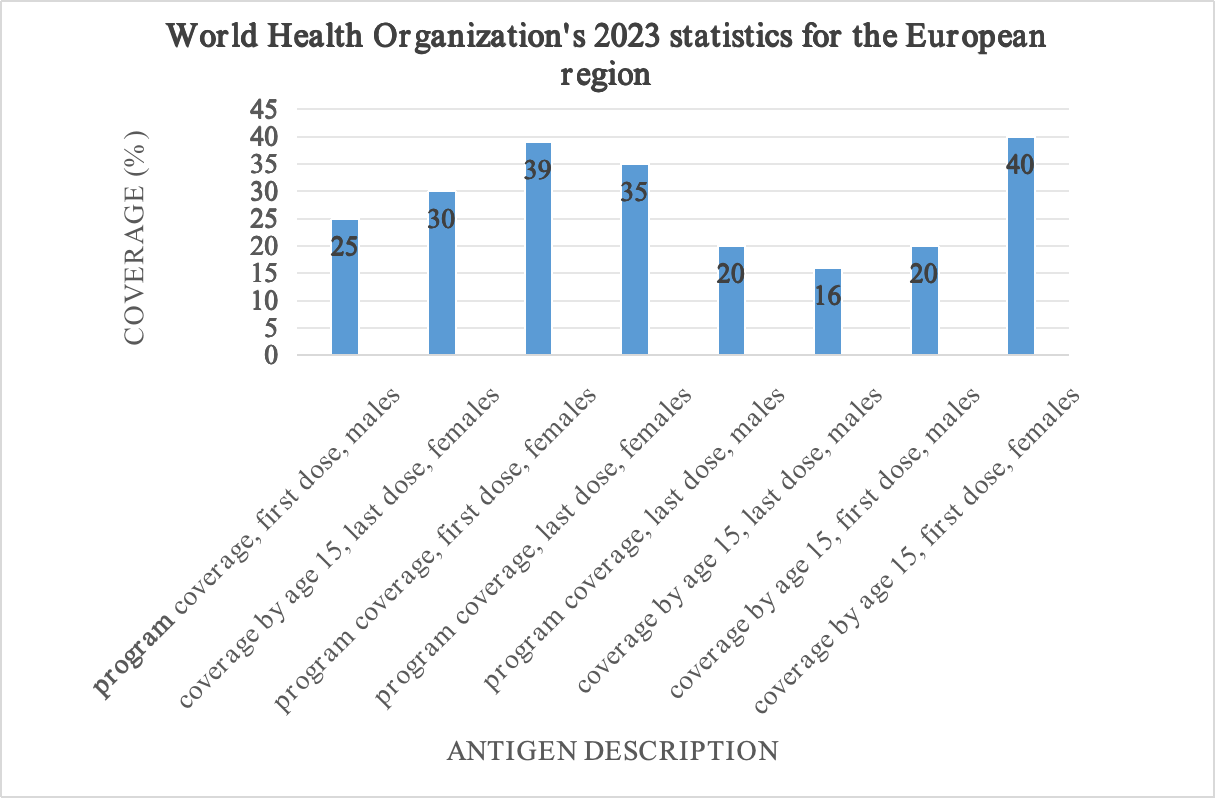
Figure 4: World Health Organization's 2023 statistics for the European region [7].
HPV vaccination coverage in Europe and globally are similar. Virtanen’s study in Finland showed that although the HPV vaccine was introduced into the National Vaccination Programme (NVP) in 2013 and the first vaccination was given in November of that year, the HPV vaccination rate in Finland remained relatively low [8].
2.4. Africa
Thousands of women living in low - and middle-income countries are needlessly dying of cervical cancer [9, 10]. As the third most common cancer among women worldwide, its age-standardized incidence (2008) exceeds 30/100,000/year in Eastern and Western Africa, 26.8/100,000/year in Southern Africa and 23.0/100,000/year in Middle Africa [11]. The comparison of these incidence rates with those in high-income regions reveals a large difference, as Western Asia, North America, and Australia/New Zealand had the significantly lower age-standardized cervical cancer incidence rate in 2008 (less than 6/100,000/year) [11]. The presentation of WHO's 2023 statistics for the African region is shown in Figure 5.
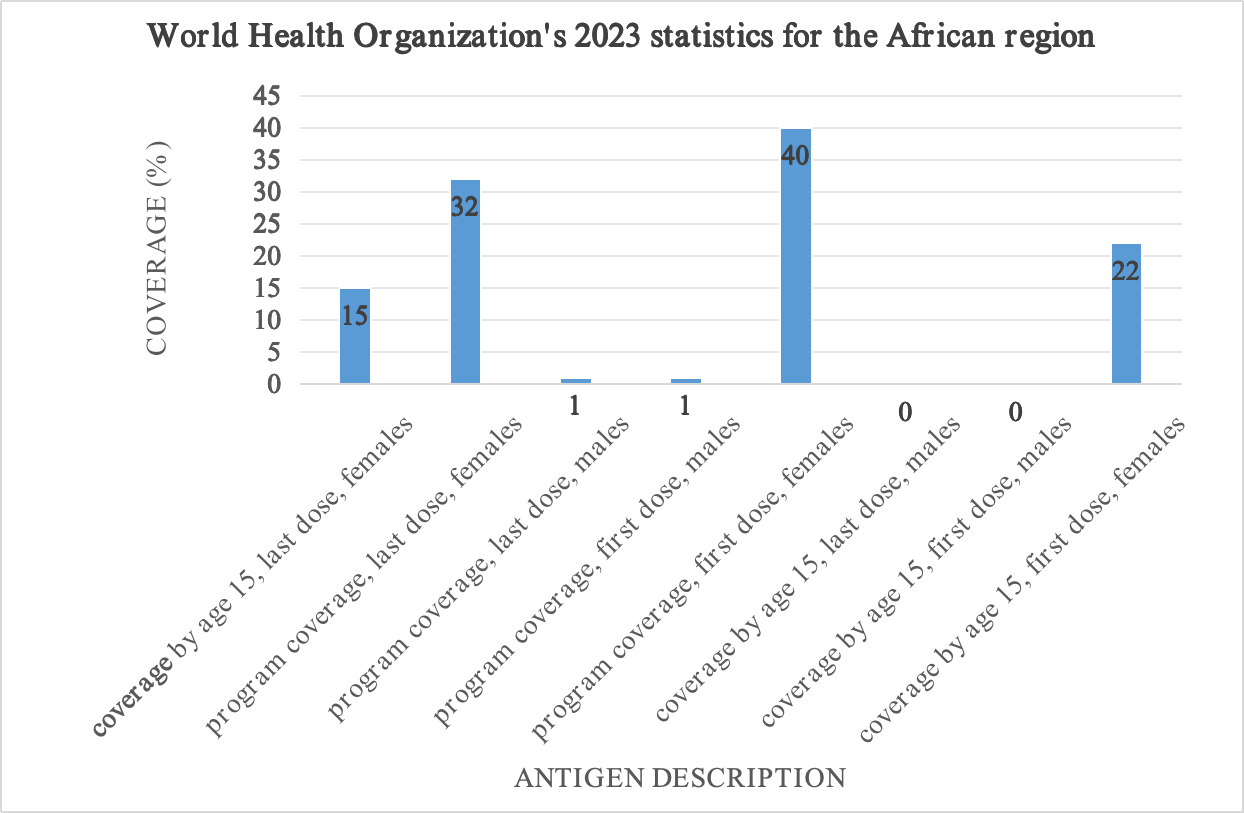
Figure 5: World Health Organization's 2023 statistics for the African region [7].
2.5. Australia
The presentation of WHO's 2023 statistics for Australia is shown in Figure 6.
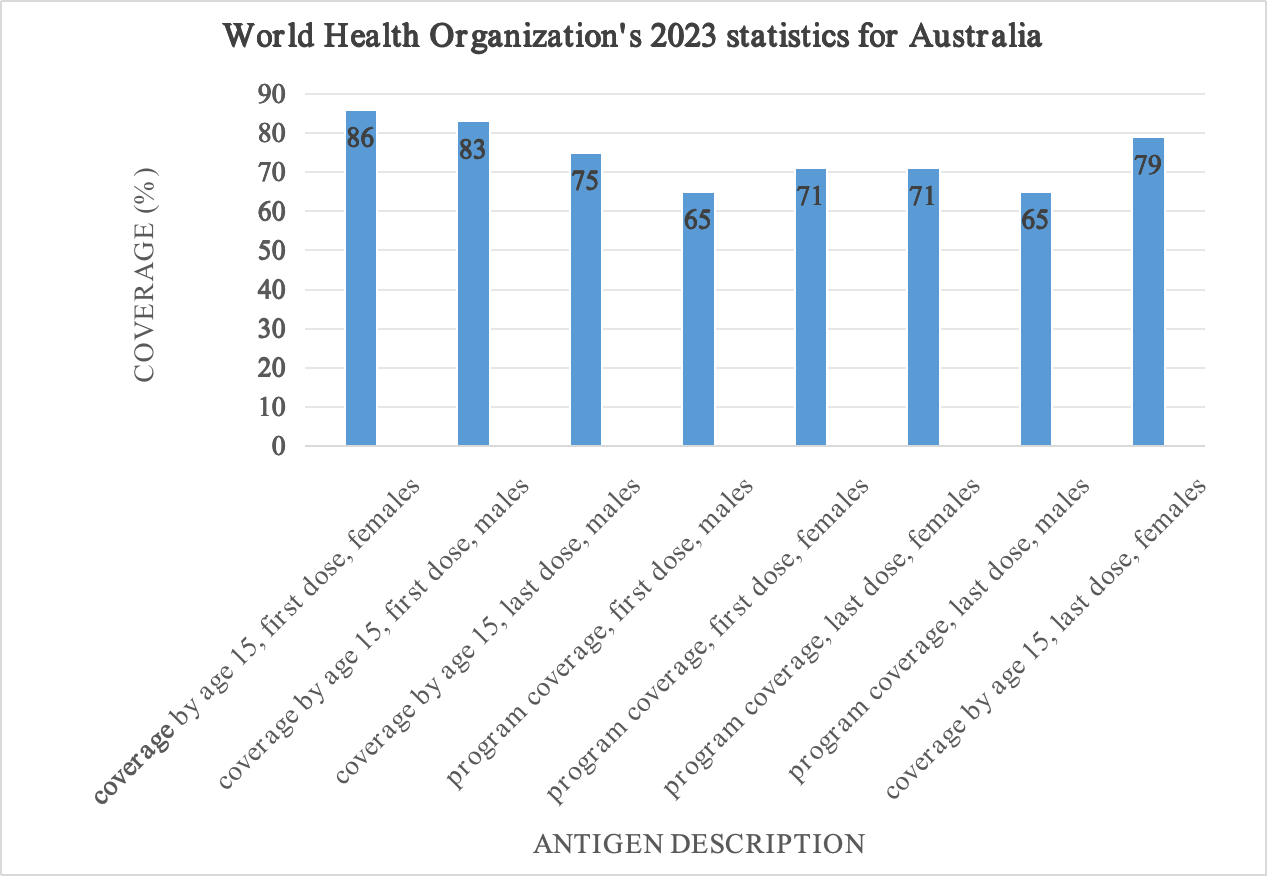
Figure 6: World Health Organization's 2023 statistics for Australia [12].
Vaccination coverage in Australia is not only much higher than in the world, but also substantially higher than in the Americas. They stand in stark contrast to data from Southeast Asia.
3. Public attitudes towards HPV vaccine
Understanding the public's attitude towards HPV vaccine is an important research content. This allows researchers and health professionals to identify specific problems with vaccines and vaccination efforts so they can implement them correctly or take steps to modify public health intervention policies and education campaigns. Public attitudes toward HPV vaccine also help professionals evaluate local healthcare systems and vaccination programs.
3.1. Positive attitude
The public from some regions (e.g., Finland, the rural southern US, Appalachia, and China) have clearly positive attitudes towards HPV vaccine. In the European region, there is a fundamentally positive attitude, rather than an explicitly negative one. In contrast to other European countries such as Austria and the Netherlands [13, 14], and especially to the United States [15], Finland's introduction of the vaccine in its NVP has not generated significant political or public controversy [8]. The public in some parts of the Americas showed more positive attitudes than the Finnish public. In the rural southern United States, positive attitudes were associated with what local women learned about the kinds of diseases that HPV vaccination prevents. Mothers are three times more likely to have their daughters vaccinated by professionals if the vaccine is designed to prevent genital warts rather than HPV infection or cervical cancer [16]. 85.2% of women living in the Appalachia directly expressed a clear positive interest in getting HPV vaccine [17]. In the Asian region, China is a good example. Compared with participants in the United States, participants in China had a strong willingness to receive the vaccine at their own expense and believed in the efficacy of the vaccine [18]. Chinese participants with more knowledge about vaccines were more likely to be vaccinated at cost [18]. Chinese men, young and sexually active Chinese participants, and more educated Chinese participants showed a greater intention to be vaccinated [18]. In China, participants who perceived higher susceptibility and severity of HPV or perceived that HPV vaccine was effective in preventing HPV infection were more likely to receive HPV vaccine regardless of cost [18]. It can be found from the above research that people will hold positive attitudes towards vaccination if they believe that the disease against which the vaccine is given is important to them, their financial situation allows them to be vaccinated, or they have acquired enough knowledge to make them value the vaccine.
3.2. Negative attitude
In Appalachia, college-age women who were sexually active, had a history of sexually transmitted infections, or had an abnormal Pap smear were more likely to express acceptance of HPV vaccine [19], but vaccine acceptance was lower among older women [20]. The 67.6% of women living there were also less receptive to vaccinating little girls [20]. They were concerned about the lack of long-term studies on new vaccines, the potential for the vaccines to harm young women's future fertility, and the suitability of very young girls for HPV vaccination [17]. Their religion teaches abstinence, which also reduces their willingness to vaccinate [17]. Parents of young girls often cultivate the false belief that the HPV vaccine will increase sexual promiscuousness, which also influences their attitudes [17]. In Finland, general public distrust of the new vaccines has also been expressed, along with concerns and anxiety about decreased safe sex after vaccination and inadequate vaccination advice from health care providers [21-24]. Distrust of health officials and suspicion of their true motives are objective [8]. The public shares similar status-biased skepticism about the need for vaccines and a clear belief in their own ability to independently acquire knowledge and make rational decisions [8]. Their trust in their own abilities allowed them to ignore ‘pressure from officials’ [8]. In Asia, although some Chinese participants showed positive attitudes, there were also some Chinese participants with a hierarchical worldview who were skeptical about the efficacy and safety of vaccines [18]. The study found that people have negative attitudes toward vaccination if they are poorly educated, have received different education than vaccination efforts, have misconceptions, or distrust the health community.
3.3. Other attitudes
There are many attitudes beyond the explicit positive attitudes, such as neutral attitudes, ambiguous attitudes, easily changeable attitudes, and so on. This review focuses the discussion on the clear positive and clear negative attitudes towards HPV vaccines. So the review does not discuss attitudes other than these two in much detail. This will be helpful for future studies, as it will be possible to further discuss all public attitudes regarding the HPV vaccine.
4. Influencing factors of HPV vaccine attitude
Many factors influence public attitudes toward the HPV vaccine. People's attitudes may be influenced by their attitudes towards cervical cancer, accessibility to medical services, socioeconomic status, psychological factors, unhealthy behaviours, education level, religious beliefs, and life experiences [17]. Cultural frameworks of luck, fate, and destiny also need to be considered [25, 26]. Cultural, educational, religious, socioeconomic status, psychological, and other influencing factors will be discussed next.
4.1. Culture background and lives
The cultural background of each region means that people born in that region tend to have similar or identical ways of thinking and behaving. People who live in the area but are not born in the area are also influenced by the cultural background of the area. It is important to study a particular culture. Cultural factors influencing attitudes toward HPV vaccination were identified in a subset of participants from a study in Appalachia, Ohio, USA. Where families and communities are close and central [17]. Their care decisions may require multigenerational involvement [17]. This means that they need more time to reach the result of a decision because reaching a common opinion often requires persuading everyone and arguing with different points of view. It can also be seen that decisions are often complicated by differences of opinion among many family members [17]. However, cultures influence each other rather than exist independently. The impact of a culture in which members of society depend on each other on the individual is also worth studying [27].
Individualistic and collectivist cultures also need to be considered. Previous studies [28, 29] have shown that individualistic and collectivist cultures can affect the way and outcome of individuals' choice of benefits and losses. An individualistic culture will make individuals more inclined to gain benefits because it will make individuals attempt to differentiate themselves from others through personal achievement and achievement [17]. Collectivist culture has the opposite effect on individuals, influencing their attempts to "fit in" by fulfilling roles and obligations [17]. However, this does not mean that a collectivist culture will bring losses to individuals. It only means that individuals' choice methods and choice results are more inclined to avoid losses [17].
4.2. Publicity and education
Educational materials and programs on cervical cancer prevention are limited in some areas because they involve women's private parts [17]. This has led to a general lack of knowledge about cervical cancer, HPV, and HPV vaccines. The misunderstanding of the HPV vaccine will have a negative impact on the promotion and vaccination of the HPV vaccine. The false belief that only sexually active girls need vaccines and that vaccines promote promiscuous sex should be dispelled [17]. There is also a misconception that some people think cervical cancer is a genetic disease or that the causative agents are environmental carcinogens in the air and water [17]. There is also skepticism about the idea that it is a dirty disease [17]. Advocacy should inform people about how the vaccine works and whether women with a history of human papillomavirus or other sexually transmitted infections should receive the human HPV vaccine. Large-scale information campaigns are the main source of HPV-related information for parents [30]. Television advertisements and word of mouth were also identified as common sources of information for people to learn about the HPV vaccine [17]. Because of the advertisements on TV, people will try to understand the HPV vaccine and start to think about the benefits and adverse effects that HPV vaccine may bring to them. People also turn to the Internet to find information about the HPV vaccine. This is conducive to increasing public knowledge and dispelling misconceptions.
4.3. Religion
Churches of some religions teach asceticism and preach asceticism and ascetic lifestyles. This leads people who follow these religions to believe that they are not at high risk of contracting the HPV virus and therefore do not receive the HPV vaccine. People also have the idea that the HPV vaccine will increase unhealthy sexual behaviors such as promiscuous sex and promiscuous sex [17].
4.4. Socioeconomic status (SES)
The burden of this falls disproportionately on socially and economically disadvantaged people [31]. These people may lack access to health care, health insurance, and time [17]. People who do not have access to health care will tend to choose not to see a doctor [17]. Moreover, the role of HPV vaccine is not to treat or cure a disease, but only to prevent it, and this non-necessity also allows them to choose not to be vaccinated. The HPV vaccine is a self-funded vaccine in some countries, which means that people need to pay for the full cost of the three doses entirely out of their own money. Their health insurance does nothing to alleviate the financial burden of getting this vaccine. For those who can afford the vaccine, health workers can advise them to get vaccinated and advise on a healthy diet. And for those who are not in a good economic situation or even need to consider food and clothing, it is unreasonable to ask them to get the HPV vaccine. Their money should be spent on more necessary things, such as buying water, food and other necessities to sustain life and subsistence.
4.5. Cognition and psychology
The HPV virus can infect not only women but also men, so for disease prevention and vaccination, both men and women should be recommended to get vaccinated. But only a few countries in the world currently allow men to be vaccinated. In countries where only women are allowed to be vaccinated, the public may focus on women for vaccine-preventable diseases due to inadequate knowledge and other reasons. This creates stress and shame for women, and may give the public the very wrong perception that there is a stigma associated with vaccination [17].
4.6. Others
In addition to cultural, educational, religious, economic, psychological and other reasons, there are many other reasons that affect people's attitudes towards HPV vaccine. Lack of prevention and screening information, lack of access to prevention and screening services, distrust of the medical community, distrust of the health care system, distrust of pharmaceutical companies, distrust of health care providers outside the community, poor doctor-patient communication, short-and long-term side effects of vaccines, poor attitudes towards preventive health, and lack of privacy are all negative factors that exist [17].
5. Discussion
5.1. Relationship between attitudes and vaccination rates
When people see no need for vaccination, they may choose to delay or avoid vaccination. When people do not have access to prevention and screening services, they are unaware of the health status of their bodies. This can make people have a vague attitude toward vaccination and make them hesitant to get the HPV vaccine because they don't know if their vaccination is necessary. People may choose to delay or avoid vaccination when they have more necessary things to do than to get vaccinated or when they perceive vaccination as unnecessary, useless or even affecting their lives.
5.2. Recommendations
In terms of advocacy and education, health workers need to distribute educational materials and conduct awareness campaigns for both sexes. It is recommended that educational materials use images that do not cause discomfort, simple words and grammar, thus allowing people of all ages and education levels to understand the content of the material. While paying attention to the content of educational materials and programs, more attention should be paid to the cultural fields of different regions, so that people can better and truly accept the content of propaganda and education. It is necessary to strengthen the research and promotion of HPV vaccine in men and encourage men to be vaccinated. It's not just a question of economics it's a question of population health and mental health. Developing targeted prevention and intervention measures for different populations [32]. It is recommended to increase the HPV vaccine education for parents, and at least one parent should be invited to participate in the HPV vaccine education activities for minors. Awareness campaigns can be conducted by inviting cervical cancer patients who are positive about treatment or men or women who have been vaccinated to share their stories. In terms of privacy protection during consultations, ensure that the health care worker and the person coming to the client have a one-on-one conversation during the consultation [17]. If there is a need to record or share relevant data about people coming to counselling, research should be conducted in other health departments with the consent of the client.
6. Conclusion
The review begins with a discussion of HPV vaccination rates in most regions of the world. Observing the data in the review, it is not difficult to find that the vaccination rate of men is generally lower than that of women, which may be related to the fact that the HPV vaccine for men has not been widely promoted globally and some countries have not yet implemented the vaccination of men. Health professionals should pay more attention to the role of men in HPV transmission, prevention and vaccination in the future. After exploring people's attitudes towards HPV vaccination and its influencing factors, it can be seen that cultural background, publicity and education, religion, economic status, psychology and other reasons will affect people's attitudes towards HPV vaccination. These factors work together on people's attitudes, rather than just any one factor. However, due to the limitations of the review, it is difficult to compare and rank the impact or importance of these influencing factors. Future research can compare the importance of these influencing factors by collecting data for comparative study. People's attitudes toward vaccines and their vaccination behavior can be seen as positively related. Because positive attitudes lead to positive vaccination behaviors, negative or ambiguous attitudes may lead to non-vaccination or hesitancy.
References
[1]. International Agency for Research on Cancer. (2007). Human papillomaviruses. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, No. 90. Lyon, France: Author.
[2]. Milner, D. A. (2015). Diagnostic pathology: Infectious diseases. Elsevier Health Sciences.
[3]. World Health Organization. (n.d.). Human papillomavirus (HPV). Retrieved from https://www.who.int/europe/news-room/fact-sheets/item/human-papillomavirus-(hpv)
[4]. Montalti, M., Salussolia, A., Capodici, A., Scognamiglio, F., Di Valerio, Z., La Fauci, G., Soldà, G., Fantini, M. P., Odone, A., Costantino, C., Leask, J., Larson, H. J., Lenzi, J., & Gori, D. (2024). Human papillomavirus (HPV) vaccine coverage and confidence in Italy: A nationwide cross-sectional study, the OBVIOUS project. Vaccines, 12(2).
[5]. World Health Organization. (n.d.). Human papillomavirus and cancer. Retrieved from https://www.who.int/zh/news-room/fact-sheets/detail/human-papilloma-virus-and-cancer
[6]. World Health Organization. (n.d.). Human papillomavirus (HPV) vaccination coverage. Retrieved from https://immunizationdata.who.int/global/wiise-detail-page/human-papillomavirus-(hpv)-vaccination-coverage?CODE=Global&YEAR=
[7]. World Health Organization. (n.d.). Human papillomavirus (HPV) vaccination coverage. Retrieved from https://immunizationdata.who.int/global/wiise-detail-page/human-papillomavirus-(hpv)-vaccination-coverage?GROUP=WHO_REGIONS&YEAR=&CODE=
[8]. Virtanen, M. J. (2019). What kind of ‘a girls’ thing’? Frictions and continuities in the framing and taming of the HPV vaccine in Finland. Sociology of Health & Illness, 41(4), 789-805.
[9]. Arrossi, S., Sankaranarayanan, R., & Parkin, D. M. (2003). Incidence and mortality of cervical cancer in Latin America. Salud Pública de México, 45(s306–s314).
[10]. International Atomic Energy Agency. (2011). Inequality in cancer care: A global perspective. Vienna: Author.
[11]. Ferlay, J., Shin, H. R., Bray, F., et al. (2010). GLOBOCAN 2008: Cancer incidence and mortality worldwide: IARC CancerBase No. 10.
[12]. World Health Organization. (n.d.). Human papillomavirus (HPV) vaccination coverage. Retrieved from https://immunizationdata.who.int/global/wiise-detail-page/human-papillomavirus-(hpv)-vaccination-coverage?CODE=AUS&YEAR=
[13]. Paul, K. T. (2016). Saving lives: Adapting and adopting human papilloma virus (HPV) vaccination in Austria. Social Science & Medicine, 153, 193-200.
[14]. Paul, K. T., Wallenberg, I., & Bal, R. (2018). Putting public health infrastructures to the test: Introducing HPV vaccination in Austria and the Netherlands. Sociology of Health & Illness, 40(1), 67-81.
[15]. Gottlieb, S. D. (2018). Not quite a cancer vaccine: Selling HPV and cervical cancer. New Brunswick: Rutgers University Press.
[16]. Sperber, N. R., Brewer, N. T., & Smith, J. S. (2008). Influence of parent characteristics and disease outcome framing on HPV vaccine acceptability among rural Southern women. Cancer Causes & Control, 19(1), 115–118.
[17]. Katz, M.L., Reiter, P.L., Heaner, S., Ruffin, M.T., Post, D.M., & Paskett, E.D. (2009). Acceptance of the HPV vaccine among women, parents, community leaders, and healthcare providers in Ohio Appalachia. Vaccine, 27(30), 3945-3952.
[18]. Liu, S., et al. (2018). Different culture or different mind? Perception and acceptance of HPV vaccine in China and in the U.S. Journal of Health Communication, 23(12), 1008–1016.
[19]. Crosby, R., Schoenberg, N., Hopenhayn, C., Moore, G., & Melhan, W. (2007). Correlates of intent to be vaccinated against human papillomavirus: An exploratory study of college-aged women. Sexual Health, 4(1), 71–73.
[20]. Hopenhayn, C., Christian, A., Christina W.J., & Schoenberg N.E. (2007). Human papillomavirus vaccine: Knowledge and attitudes in two Appalachian Kentucky counties. Cancer Causes & Control, 18(6), 627–634.
[21]. Zimet, G.D., Rosberger, Z., Fisher W.A., Perez S., et al. (2013). Beliefs, behaviors and HPV vaccine: Correcting the myths and the misinformation. Preventive Medicine, 57(5), 414–418.
[22]. Hendry, M., Lewis R., Clements A., Damery S., et al. (2013). “HPV? Never heard of it!”: A systematic review of girls’ and parents’ information needs, views and preferences about human papillomavirus vaccination. Vaccine, 31(45), 5152–5167.
[23]. Larson H.J., Cooper L.Z., Eskola J., Katz S.L.; et al.(2011). Addressing the vaccine confidence gap. The Lancet, 378(9790), 526–535.
[24]. Thomson A., Robinson K., & Vallee-Tourangeau G.(2016). The 5As: A practical taxonomy for the determinants of vaccine uptake.Vaccine,34(8),1018–1024.
[25]. Davison C., Smith G.D., & Frankel S.(1991). Lay epidemiology and the prevention paradox: The implications of coronary candidacy for health education.Sociology of Health & Illness,13(1),1–19.
[26]. Prior L.(2003). Belief knowledge and expertise: The emergence of the lay expert in medical sociology.Sociology of Health & Illness,25(3),41–57.
[27]. Levin I.P., Schneider S.L.& Gaeth G.J.(1998). All frames are not created equal: A typology and critical analysis of framing effects.Organizational Behavior and Human Decision Processes,76(2),149–188.
[28]. Elliot A.J.; Chirkov V.I.; Kim Y.; Sheldon K.M.(2001). A cross-cultural analysis of avoidance relative to approach personal goals.Psychological Science,12(5),505–510.
[29]. Lee A.Y.; Aaker J.L.; Gardner W.L.(2000). The pleasures and pains of distinct self-construals: The role of interdependence in regulatory focus.Journal of Personality and Social Psychology,78(6),1122–1134.
[30]. Hughes J.; Cates J.R.; Liddon N.; Smith J.S.; Gottlieb S.L.; Brewer N.T.(2009). Disparities in how parents are learning about the human papillomavirus vaccine.Cancer Epidemiology Biomarkers & Prevention,18(2),363–372.
[31]. Adimora A.A.; Schoenbach V.(2005). Social context sexual networks and racial disparities in rates of sexually transmitted infections.The Journal of Infectious Diseases,191(Suppl 1),S115-S122.
[32]. Lechuga J.; Swain G.R.; Weinhardt L.S.(2011). Impact of framing on intentions to vaccinate daughters against HPV: A cross-cultural perspective.Annals of Behavioral Medicine,42(2),221–226.
Cite this article
Zhang,J. (2025). HPV Vaccination Rates and Public Attitudes Towards HPV Vaccination in Different Countries: A Review of Cross-Cultural Studies. Theoretical and Natural Science,69,19-29.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 3rd International Conference on Modern Medicine and Global Health
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. International Agency for Research on Cancer. (2007). Human papillomaviruses. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, No. 90. Lyon, France: Author.
[2]. Milner, D. A. (2015). Diagnostic pathology: Infectious diseases. Elsevier Health Sciences.
[3]. World Health Organization. (n.d.). Human papillomavirus (HPV). Retrieved from https://www.who.int/europe/news-room/fact-sheets/item/human-papillomavirus-(hpv)
[4]. Montalti, M., Salussolia, A., Capodici, A., Scognamiglio, F., Di Valerio, Z., La Fauci, G., Soldà, G., Fantini, M. P., Odone, A., Costantino, C., Leask, J., Larson, H. J., Lenzi, J., & Gori, D. (2024). Human papillomavirus (HPV) vaccine coverage and confidence in Italy: A nationwide cross-sectional study, the OBVIOUS project. Vaccines, 12(2).
[5]. World Health Organization. (n.d.). Human papillomavirus and cancer. Retrieved from https://www.who.int/zh/news-room/fact-sheets/detail/human-papilloma-virus-and-cancer
[6]. World Health Organization. (n.d.). Human papillomavirus (HPV) vaccination coverage. Retrieved from https://immunizationdata.who.int/global/wiise-detail-page/human-papillomavirus-(hpv)-vaccination-coverage?CODE=Global&YEAR=
[7]. World Health Organization. (n.d.). Human papillomavirus (HPV) vaccination coverage. Retrieved from https://immunizationdata.who.int/global/wiise-detail-page/human-papillomavirus-(hpv)-vaccination-coverage?GROUP=WHO_REGIONS&YEAR=&CODE=
[8]. Virtanen, M. J. (2019). What kind of ‘a girls’ thing’? Frictions and continuities in the framing and taming of the HPV vaccine in Finland. Sociology of Health & Illness, 41(4), 789-805.
[9]. Arrossi, S., Sankaranarayanan, R., & Parkin, D. M. (2003). Incidence and mortality of cervical cancer in Latin America. Salud Pública de México, 45(s306–s314).
[10]. International Atomic Energy Agency. (2011). Inequality in cancer care: A global perspective. Vienna: Author.
[11]. Ferlay, J., Shin, H. R., Bray, F., et al. (2010). GLOBOCAN 2008: Cancer incidence and mortality worldwide: IARC CancerBase No. 10.
[12]. World Health Organization. (n.d.). Human papillomavirus (HPV) vaccination coverage. Retrieved from https://immunizationdata.who.int/global/wiise-detail-page/human-papillomavirus-(hpv)-vaccination-coverage?CODE=AUS&YEAR=
[13]. Paul, K. T. (2016). Saving lives: Adapting and adopting human papilloma virus (HPV) vaccination in Austria. Social Science & Medicine, 153, 193-200.
[14]. Paul, K. T., Wallenberg, I., & Bal, R. (2018). Putting public health infrastructures to the test: Introducing HPV vaccination in Austria and the Netherlands. Sociology of Health & Illness, 40(1), 67-81.
[15]. Gottlieb, S. D. (2018). Not quite a cancer vaccine: Selling HPV and cervical cancer. New Brunswick: Rutgers University Press.
[16]. Sperber, N. R., Brewer, N. T., & Smith, J. S. (2008). Influence of parent characteristics and disease outcome framing on HPV vaccine acceptability among rural Southern women. Cancer Causes & Control, 19(1), 115–118.
[17]. Katz, M.L., Reiter, P.L., Heaner, S., Ruffin, M.T., Post, D.M., & Paskett, E.D. (2009). Acceptance of the HPV vaccine among women, parents, community leaders, and healthcare providers in Ohio Appalachia. Vaccine, 27(30), 3945-3952.
[18]. Liu, S., et al. (2018). Different culture or different mind? Perception and acceptance of HPV vaccine in China and in the U.S. Journal of Health Communication, 23(12), 1008–1016.
[19]. Crosby, R., Schoenberg, N., Hopenhayn, C., Moore, G., & Melhan, W. (2007). Correlates of intent to be vaccinated against human papillomavirus: An exploratory study of college-aged women. Sexual Health, 4(1), 71–73.
[20]. Hopenhayn, C., Christian, A., Christina W.J., & Schoenberg N.E. (2007). Human papillomavirus vaccine: Knowledge and attitudes in two Appalachian Kentucky counties. Cancer Causes & Control, 18(6), 627–634.
[21]. Zimet, G.D., Rosberger, Z., Fisher W.A., Perez S., et al. (2013). Beliefs, behaviors and HPV vaccine: Correcting the myths and the misinformation. Preventive Medicine, 57(5), 414–418.
[22]. Hendry, M., Lewis R., Clements A., Damery S., et al. (2013). “HPV? Never heard of it!”: A systematic review of girls’ and parents’ information needs, views and preferences about human papillomavirus vaccination. Vaccine, 31(45), 5152–5167.
[23]. Larson H.J., Cooper L.Z., Eskola J., Katz S.L.; et al.(2011). Addressing the vaccine confidence gap. The Lancet, 378(9790), 526–535.
[24]. Thomson A., Robinson K., & Vallee-Tourangeau G.(2016). The 5As: A practical taxonomy for the determinants of vaccine uptake.Vaccine,34(8),1018–1024.
[25]. Davison C., Smith G.D., & Frankel S.(1991). Lay epidemiology and the prevention paradox: The implications of coronary candidacy for health education.Sociology of Health & Illness,13(1),1–19.
[26]. Prior L.(2003). Belief knowledge and expertise: The emergence of the lay expert in medical sociology.Sociology of Health & Illness,25(3),41–57.
[27]. Levin I.P., Schneider S.L.& Gaeth G.J.(1998). All frames are not created equal: A typology and critical analysis of framing effects.Organizational Behavior and Human Decision Processes,76(2),149–188.
[28]. Elliot A.J.; Chirkov V.I.; Kim Y.; Sheldon K.M.(2001). A cross-cultural analysis of avoidance relative to approach personal goals.Psychological Science,12(5),505–510.
[29]. Lee A.Y.; Aaker J.L.; Gardner W.L.(2000). The pleasures and pains of distinct self-construals: The role of interdependence in regulatory focus.Journal of Personality and Social Psychology,78(6),1122–1134.
[30]. Hughes J.; Cates J.R.; Liddon N.; Smith J.S.; Gottlieb S.L.; Brewer N.T.(2009). Disparities in how parents are learning about the human papillomavirus vaccine.Cancer Epidemiology Biomarkers & Prevention,18(2),363–372.
[31]. Adimora A.A.; Schoenbach V.(2005). Social context sexual networks and racial disparities in rates of sexually transmitted infections.The Journal of Infectious Diseases,191(Suppl 1),S115-S122.
[32]. Lechuga J.; Swain G.R.; Weinhardt L.S.(2011). Impact of framing on intentions to vaccinate daughters against HPV: A cross-cultural perspective.Annals of Behavioral Medicine,42(2),221–226.