1. Introduction
It has come to mean that a pandemic declaration is meant to show that there is an infectious pathogen present, can spread easily between individuals, and is likely to cause significant health impacts. The WHO does not declare a pandemic simply because infection rates are high but also to mobilize the entire world into action. It is a call to a unified and efficient response of governments, health organizations, and communities to contain the spread and mitigate the effects of the disease.
Historically, pandemics have invade human societies multiple times, such as the Spanish flu of 1918, which claimed millions of lives from across the world. The COVID-19 pandemic, declared on March 11, 2020, by the WHO, brought to the fore the dire need for timely and coordinated global health responses. This declaration was made in view of the rapid spread of the virus and its serious consequences, including intense mortality and unprecedented strain on healthcare systems [1].
The declaration of COVID-19 as a pandemic outlined the gravity with which international cooperation became highly essential. Such coordination is very important in terms of sharing data, research advantages, and medical resources so that nations can address the health challenge as one. Health leaders from around the world have been thus calling for preparedness and thus a common approach in case of further pandemics after the COVID-19 experience. The same has opened ways for discussion on international treaties for improved global health security. As shown in Figure 1, vaccination of people increased from 0 to 5,000 millions in only one years. International communication and treaties must be stablished in order to achieve the data.
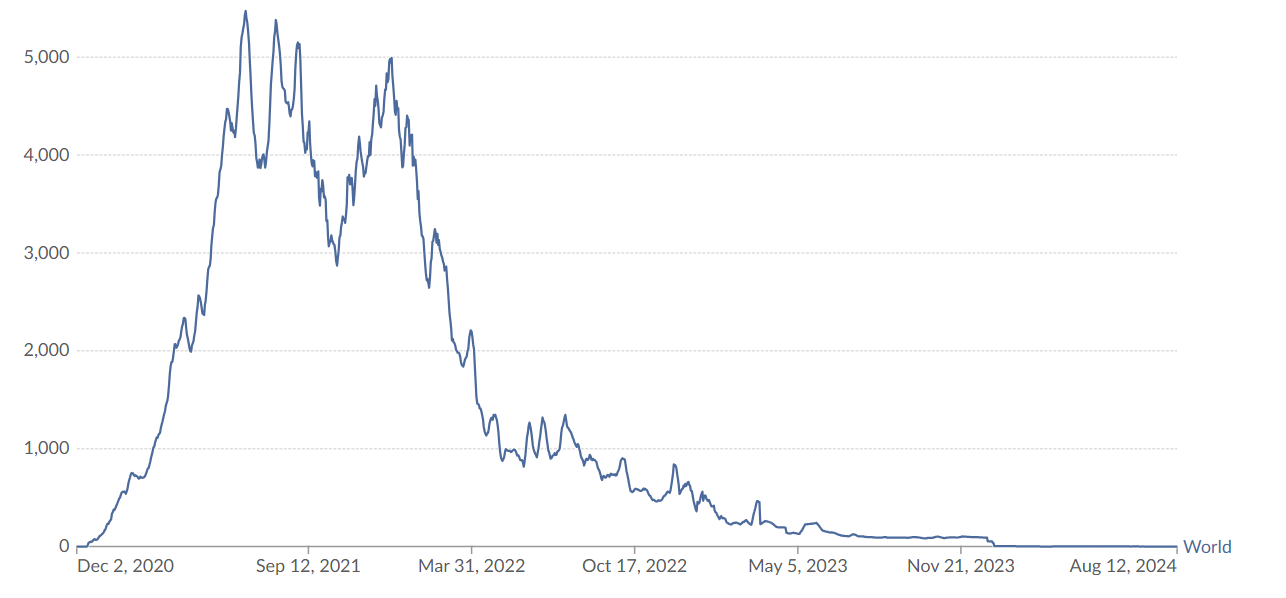
Figure 1: Daily COVID-19 vaccine doses administered per million people [2].
2. Virus characteristics and behaviour
COVID-19 is caused by a new coronavirus, SARS-CoV-2, part of a large family of viruses responsible for conditions ranging from the common cold to severe respiratory syndromes. SARS-CoV-2 virus consists of an RNA genome enveloped with protein shell, whose spike proteins facilitate virus entry into human cells. These spike proteins bind with ACE2 receptors, to be found abundantly in respiratory tract tissues.
SARS-CoV-2 is transmitted person-to-person by respiratory droplets and aerosols produced during talking, coughing, sneezing, or breathing by an infected individual. The virus also spreads, though less frequently, through touching of surfaces contaminated with it, as the virus survives on a number of different types of surfaces for variable periods of time.
Following exposure, incubation of the virus ranges approximately from 2 to 14 days, averaging about 5 days. During this time, a person can be asymptomatic but can spread the virus; hence, complicating containment. The asymptomatic transmission underlines the challenge of identifying and isolating cases-a factor that has contributed to the rapid global spread of the disease [3].
The replication process of SARS-CoV-2 initiates the attachment of the spike protein to ACE2 receptors, hence allowing virus entry. It then hijacks the cell machinery in order to replicate its RNA and form a new viral particle that will eventually cause cell lysis and liberate more virus particles ready to infect more cells.
Mutations are an intrinsic part of viral evolution, and SARS-CoV-2 is no exception to this fact. While many mutations have negligible effects, others may alter the behavior of the virus with regard to transmissibility and immune response [4]. Indeed, several notable variants have had varying impacts, such as Alpha, Delta, and Omicron: Delta was highly transmissible and severe in specific populations, while Omicron had a highly contagious nature but generally resulted in mild symptoms. On the other hand, Omicron also demonstrated partial immune evasion challenging existing vaccines and the need for updated booster doses.
Understanding the biology of SARS-CoV-2 and how it mutates is really key to adapting public health responses, which will help in the development of vaccines, treatments, and prevention methods. Continued evolution simply points to the fact that the virus is a permanent concern for global health, as there will be a need for constant surveillance, flexibility in response strategies, and consistency in the research being carried out. 3. Public Health Strategy: Detection, Protection, and Vaccination
The most effective public health strategies for COVID-19 are multitiered, focusing on detection, protection, and vaccination. These strategies reduce transmission, manage cases, and protect communities from severe disease.
2.1. Detection and testing
Early detection is one of the most important aspects of COVID-19 management. Diagnostic tools involve the use of PCR tests, which usually are regarded as the gold standard because of their high sensitivity and the ability to detect even low viral loads [5]. Rapid antigen tests provide a faster but less sensitive method and thus find wider applications in community settings, including schools and workplaces. Surveillance testing has emerged, especially in high-exposure areas, as an important tool in the identification of asymptomatic carriers of the virus and in the prevention of possible outbreaks.
This is further complemented by contact tracing, whereby health officials get to notify and test people coming in contact with confirmed cases. In many instances, this process is supported by digital tools that ensure speedy isolation and reduce further transmission of the virus, while keeping up the standards of privacy through anonymized tracking.
2.2. Protection measures
The mainstays of protection against COVID-19 include the wearing of masks, physical distancing, and hygiene practices. Masks used initially varied from cloth to surgical, but then N95 and KN95 respirators were introduced as more contagious variants emerged. These masks have better filtration, especially in crowded or indoor environments.
Social distancing has also been one of the cornerstones of policy recommendations, where a minimum distance of six feet is suggested as one of the key ways to contain the spread of the disease via airborne transmission. In addition to all these, the practice of hand hygiene has been advocated continuously, even as the current predominant mode of transmission is through respiratory droplets. Public areas have, likewise, been given added layers of protection through regular disinfection.
Public health communication has played a very important role in reinforcing these protective behaviors. Clear, consistent messaging from health authorities has guided individuals and communities on adopting safety measures while adapting to new scientific findings.
2.3. Vaccination efforts
Vaccination remains the cornerstone of COVID-19 prevention. The rapid development of vaccines has been a scientific milestone that provides substantial protection against severe diseases and mortality. Initial vaccination was reserved for high-risk populations, such as health workers and the elderly, before widening to the general population. Booster doses have been introduced in response to waning immunity and protection against emerging variants [6].
These problems point towards many pitfalls in the global vaccine distribution-access gap between high-income and low-income nations [7]. As long as this situation persists, it will not be easy to build up general immunity and reduce the spread of the viruses. Public health agencies continue to call for equity in distribution and outreach against vaccine hesitancy and misinformation.
While that is a long way of saying it, it has been the COVID-19 pandemic that underlined how imperative a response from public health was, one that had to be duly coordinated and dynamic. The reason continuous detection, protection, and vaccination have become so important for pandemic control and establishment of preparedness against future global health threats.
3. Impact of vaccination and technological integration
Vaccination has dramatically cut instances of severe COVID-19 and spared healthcare systems around the world from undue pressure [7]. This has also been crucial for safer social interactions and supported the gradual reopening of economies. Major protection at the individual level, as seen with vaccines, has also ensured progress toward herd immunity, which is critical for reducing community transmission and shielding the most vulnerable populations from severe illness.
The rapid development and deployment of the COVID-19 vaccine, especially mRNA-based ones, are an unprecedented scientific achievement. Before the pandemic, most vaccines took years of research and trials before they reached people. An accelerated timeline for COVID-19 vaccine development, approved in less than one year, showed what can be accomplished when global collaboration is informed by leading-edge technological innovation. The pace and efficiency of vaccine research have now set new standards under which any future health crisis is being or could be contained. Vaccines based on the mRNA platform, especially those from Pfizer-BioNTech and Moderna, did more than simply show efficacy against COVID-19 but opened doors for therapies and possibly vaccinations against other disorders, such as various forms of cancers, influenza, and even new infectious diseases. The depth of this potential application gives evidence of long-term benefits derived from investment in research and innovation [8].
Outside of vaccine development, technological advancements have significantly enhanced responses to public health. Big data has been available, and strategic utilization has been important in understanding COVID-19 spread and has informed timely decision-making. It further enabled experts to understand infection rates, predict outbreaks, and draft responsive public health policies on a large scale. For instance, case data analysis helped to show hotspots where public health officials distributed resources more appropriately to prevent some healthcare facilities from getting burdened due to the virus. On the one hand, contact tracing has equally been one of the critical tools used in managing the pandemic supported by technologies. Proximity information from contact-tracing apps alerted those who may have been exposed to the virus so they could take matters into their own hands with self-isolation and break chains of transmission. They were invaluable tools in countries where traditional contact tracing would have been well out of scale due to the high volume of cases. Some challenges, such as those dealing with privacy and adoption, were recognized; the deployment of such technology signalled how innovative solutions can serve in emergency situations. International cooperation strengthened the global pandemic response. Systems, like the COVID-19 Dashboard that was developed by WHO, have been very important in facilitating data and strategy sharing in real-time between different countries. By sharing infection statistics, vaccination rates, and effective intervention measures, they were more aptly placed to learn from successes and mistakes of others. This cooperative approach- rather, this sense of cooperation-serve not only to enhance individual national responses but strengthen collective global efforts in combat against the virus. The insights derived from international sharing of data outlined best practices in disease containment, vaccine distribution, and public health communication.
The COVID-19 experience has highlighted the need for continued investment in the public health infrastructure and global health security [9]. It was clear that while technology may hugely enhance the response effort, the bedrock components-the well-resourced health workforce and communication strategies-remain critical. Moving forward from this, leveraging the lessons from the pandemic will be critical to building resilience against future health threats.
Besides that, the pandemic has also revived interest in mRNA technology [10], which led to accelerated research in its use beyond infectious diseases. Adaptability in this technology has paved the way for targeted treatments in the immunotherapy of cancer among many other medical fields. This rapid development of vaccines for COVID-19 proved that collaboration between governments, research institutions, and the private sector could achieve great things. These collaborations underscore the value of public-private partnership, where-if aligned appropriately-acceleration of key scientific discoveries and their delivery can be realized.
The COVID-19 pandemic has been a lesson in how scientific ingenuity and collaboration can change the course of history. The vaccination effort has done much more than contain the most devastating impact of COVID-19; it has provided a bedrock for new technologies with the potential to change the future face of medicine. The role of big data and international collaboration further underpins the fact that collective action and integration of modern tools are basic keys to deal with global health crises. Beyond doubt, lessons in futuro will mold public health policies and technological strategies toward preparedness and responsiveness against emerging threats.
4. Conclusion
Detection, protection, and vaccination are the three main pillars that have underlain all handling of COVID-19, keeping safety concerns about public health in view. Early testing was one way to identify cases in time, which helped reduce the virus's spread. Protection, meaning masking and social distancing, has limited the virus's transmission and outbreaks in terms of severity. Vaccination has provided communities with substantial immunity, reducing serious cases and pressures on healthcare.
The pandemic-driven paradigm shift ranged from big data to rapid vaccine development. The shared response taught the world what is possible when technological innovation and international collaboration transform public health resilience. Indeed, these efforts laid the groundwork for responding to the next infectious disease threat by underlining the need for continued investment in surveillance, prevention, and scientific research in a manner that bolsters global health security.
Going forward, this essay identifies continued investment in global health infrastructure, public health communication, and scientific research as needs in the face of future pandemics. The COVID-19 experience-particularly regarding technological innovation and international cooperation-sets a platform for future responses to emerging health threats.
References
[1]. Pollard, C. A., Morran, M. P., & Nestor-Kalinoski, A. L. (2020). The COVID-19 pandemic: a global health crisis. Physiological genomics, 52(11), 549-557..
[2]. Centers for Disease Control and Prevention (CDC) - COVID-19 Data Tracker, Centers for Disease Control and Prevention. COVID-19 Data Tracker. Centers for Disease Control and Prevention, https://covid.cdc.gov/covid-data-tracker/#datatracker-home. Accessed 14 Nov. 2024.
[3]. Sanjuán, R., Nebot, M. R., Chirico, N., Mansky, L. M., & Belshaw, R. (2010). Viral mutation rates. Journal of virology, 84(19), 9733-9748..
[4]. Ludwig, S., & Zarbock, A. (2020). Coronaviruses and SARS-CoV-2: a brief overview. Anesthesia & Analgesia, 131(1), 93-96.
[5]. Mathuria, J. P., & Yadav, R. (2020). Laboratory diagnosis of SARS-CoV-2-A review of current methods. Journal of infection and public health, 13(7), 901-905..
[6]. Ataguba, O. A., & Ataguba, J. E. (2020). Social determinants of health: the role of effective communication in the COVID-19 pandemic in developing countries. Global health action, 13(1), 1788263.
[7]. Zhao, J., Zhao, S., Ou, J., Zhang, J., Lan, W., Guan, W., ... & Zhang, Q. (2020). COVID-19: coronavirus vaccine development updates. Frontiers in immunology, 11, 602256.
[8]. Rahman, M. M., Masum, M. H. U., Wajed, S., & Talukder, A. (2022). A comprehensive review on COVID-19 vaccines: development, effectiveness, adverse effects, distribution and challenges. Virusdisease, 33(1), 1-22.
[9]. Javed, S., & Chattu, V. K. (2020). Strengthening the COVID-19 pandemic response, global leadership, and international cooperation through global health diplomacy. Health promotion perspectives, 10(4), 300–305.
[10]. Haafza, L. A., Awan, M. J., Abid, A., Yasin, A., Nobanee, H., & Farooq, M. S. (2021). Big data covid-19 systematic literature review: Pandemic crisis. Electronics, 10(24), 3125.
Cite this article
Wang,K. (2025). Global Strategies Against COVID-19: The Role of Public Health Measures, Vaccination, and Technology. Theoretical and Natural Science,69,30-34.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 3rd International Conference on Modern Medicine and Global Health
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Pollard, C. A., Morran, M. P., & Nestor-Kalinoski, A. L. (2020). The COVID-19 pandemic: a global health crisis. Physiological genomics, 52(11), 549-557..
[2]. Centers for Disease Control and Prevention (CDC) - COVID-19 Data Tracker, Centers for Disease Control and Prevention. COVID-19 Data Tracker. Centers for Disease Control and Prevention, https://covid.cdc.gov/covid-data-tracker/#datatracker-home. Accessed 14 Nov. 2024.
[3]. Sanjuán, R., Nebot, M. R., Chirico, N., Mansky, L. M., & Belshaw, R. (2010). Viral mutation rates. Journal of virology, 84(19), 9733-9748..
[4]. Ludwig, S., & Zarbock, A. (2020). Coronaviruses and SARS-CoV-2: a brief overview. Anesthesia & Analgesia, 131(1), 93-96.
[5]. Mathuria, J. P., & Yadav, R. (2020). Laboratory diagnosis of SARS-CoV-2-A review of current methods. Journal of infection and public health, 13(7), 901-905..
[6]. Ataguba, O. A., & Ataguba, J. E. (2020). Social determinants of health: the role of effective communication in the COVID-19 pandemic in developing countries. Global health action, 13(1), 1788263.
[7]. Zhao, J., Zhao, S., Ou, J., Zhang, J., Lan, W., Guan, W., ... & Zhang, Q. (2020). COVID-19: coronavirus vaccine development updates. Frontiers in immunology, 11, 602256.
[8]. Rahman, M. M., Masum, M. H. U., Wajed, S., & Talukder, A. (2022). A comprehensive review on COVID-19 vaccines: development, effectiveness, adverse effects, distribution and challenges. Virusdisease, 33(1), 1-22.
[9]. Javed, S., & Chattu, V. K. (2020). Strengthening the COVID-19 pandemic response, global leadership, and international cooperation through global health diplomacy. Health promotion perspectives, 10(4), 300–305.
[10]. Haafza, L. A., Awan, M. J., Abid, A., Yasin, A., Nobanee, H., & Farooq, M. S. (2021). Big data covid-19 systematic literature review: Pandemic crisis. Electronics, 10(24), 3125.