1. An overview and classification of flexible wearable electrochemical sensors
A flexible wearable electrochemical sensor is a type of sensor that can adhere to the surface of the human body and monitor biological parameters in real time based on electrochemical principles. It utilizes the electrochemical reaction between the electrode and electrolyte to detect target substances. Flexible electrochemical sensors have greater flexibility and adaptability compared to traditional rigid electrochemical sensors, which are not suitable for long-term wear. They can perfectly fit the surface of the human body and better contact the surface of living organisms or irregular objects. This not only improves user comfort but also improves the accuracy and reliability of monitoring data.
Flexible electrochemical sensors can be classified into various types based on their structure and working principles. Among them, the most common is a flexible electrochemical sensor based on a flexible substrate. Its electrodes and sensing elements are integrated into the flexible substrate material, which can achieve high sensitivity detection of target substances, used for monitoring body movement, sensing pressure changes, monitoring body temperature, etc. In addition, there are flexible electrochemical sensors based on nanomaterials, which utilize the high specific surface area and unique electrochemical properties of nanomaterials to improve the detection sensitivity and response speed of the sensors. These sensors can not only maintain stable electrical properties under various bending and stretching conditions, but also effectively detect biomolecules, such as glucose and lactate. In addition, there are flexible electrochemical sensors based on flexible electrodes and electrolytes, which achieve selective detection of different target substances by adjusting the combination of electrolytes and electrode materials.
2. Wearable devices
2.1. Epidermis wearable device
Most of our bodies are covered by epidermis, so epidermis-based wearable devices have unique advantages, such as extensive sampling points, continuity of monitoring, easy placement, and comfort to wear. Some non-invasive monitoring of the skin solves the pain problem and does not cause damage or even infection to the skin.
By fitting flexible sensors on the surface of human skin, physiological indicators such as heart rate, respiratory rate, body temperature, and blood pressure can be monitored in time, providing a scientific basis for exercise and fitness. Compared with the traditional fixed sensor, this monitoring method is more comfortable and convenient, and will not affect the activity and performance of the athletes. Therefore, flexible wearable biosensors are widely used in various sports such as running, swimming and yoga.
Early advances in the epidermal wearable electrochemical sensing platform are mainly based on motor sweating. Sweat is an ideal source of continuous non-invasive measurement biomarkers, commonly used for monitoring multiple biochemical indicators, such as sodium, chloride, potassium, lactate, calcium, ammonia, ethanol, urea, cortisol and various neuropeptides and cytosolic [2]. The detection of external sweat gland biomarkers has great advantages over the biomarkers of urine, blood, tears, and apical urinary sweat glands. Na + and Cl-ions are the most abundant electrolytes in sweat and play a role in promoting hydration [3]. In exercise, the timely recruitment of Na + is essential to accelerate recovery and reduce soft tissue damage caused by dehydration, so it is important to monitor Na + levels in athletes. Bandodkar et al. reported the successful manufacture and analysis of the epidermal tattoo potential sodium sensor, which can be used to continuously non-invasively monitor sodium in sweat, thus highlighting its transformation potential [4] for the sports community.
For example, the Berkeley team developed a motion-based sweat sensor array [5], and in this work, they demonstrated the simultaneous detection of sweat metabolites (glucose and lactate) and electrolytes (sodium and potassium ions) skin temperature by integrating multi-sensor arrays. This pioneering work filled the gap between signal transduction, conditioning, data processing, wireless transmission, and system integration, enabling field data processing and communication, thus driving the field of wearable sensing. The sensing system also extends its presence in Applications in noninvasive pharmacokinetic research, such as researchers trying to use sensing platforms, rely on carbon nanotubes Voltammetry scanning on the pole for direct anode detection of caffeine [6]. The successful practice of this principle shows that the sensing system has great potential for monitoring drugs and drug interactions in the human body, and can be used in future therapeutics (therapy plus diagnosis). Reliable concentration signal response requires efficient sample transmission to provide fresh sweat samples, however, only a few wearable sweat sensors collect and sample sweat by using a microfluidic chamber. Martin et al. produced a wearable microfluidic sensor mounted on a PDMS microfluidic network for dynamic sweat analysis (Fig 1-b) [7], which enables continuous data acquisition and analysis using wireless conversion analysis components. Lee et al. developed a wearable sensor patch, through modification with multiple sweat and waterproof layer equipment components, to achieve effective sweat control and sensing accuracy, to use 1 μ L sweat volume for reliable measurement (figure 1-c) [8], by overcoming the limitation of sample size, can solve a series of problems brought by the skin biosensor. These sensors can accurately capture the physiological signals of the human body, and provide users with data processing and analysis through intelligent algorithms. Personalized exercise monitoring and fitness advice. According to each person's physiological characteristics and exercise habits, the biosensor can automatically adjust the training plan, providing the most suitable training intensity and duration for the athlete. In this way, exercisers can train more efficiently, improve their performance, and reduce the risk of sports injuries.
The simplest and most rapid way to obtain sweat is through exercise, but this method is not suitable for everyone. For the elderly with decreased exercise function, we can take other ways to obtain sweat, such as considering the skin microflow system to collect the natural release of sweat after a hot shower[9]
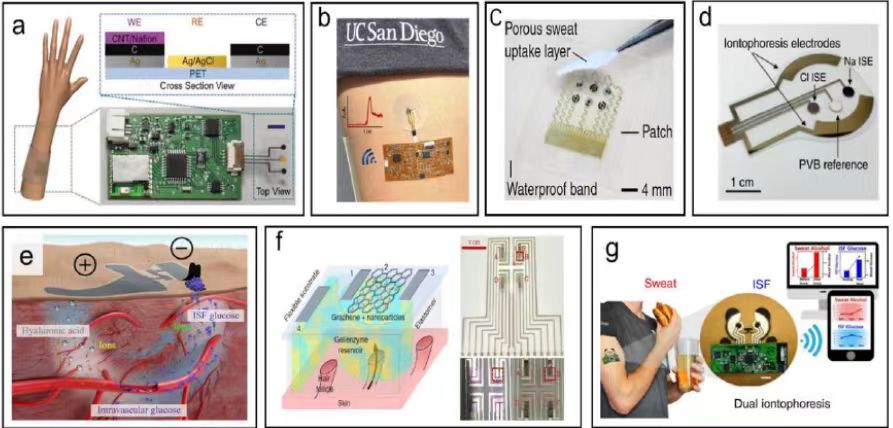
Figure 1. epidermal wearable sensor reported in the literature (a) a wearable watch developed by the Berkeley team for caffeine detection; (b) a wearable microfluidic sensor for dynamic sweat analysis; (c) Lee et al. developed a wearable low sample volume sweat analysis patch; (d) an electrode system for epidermal biofluid; (e) Tsinghua University team developed for the counterion electropermeability patch; (f) a graphene pixel-based path selective glucose monitoring patch developed by researchers; (g) a skin tattoo sensor capable of analyzing both sweat and tissue fluid.
2.2. Oral wearable devices
Currently, sensors using saliva as a sample source are rapidly developing. The disadvantage of saliva for real-time measurement of human performance compared to sweat is that it is limited to exercises that require tooth protection. Furthermore, the concentrations of analytes detected in saliva were much lower than in sweat. In addition, the wearable devices discussed have not demonstrated the continuity of salivary biomarker measurement and also need further verification and exploration for their high sensitivity and stability.
Wang et al. [10] have designed a socket-based oral uric acid biosensor that integrates the equipment needed for sensor operation and signal transmission on the socket circuit board, including a potentiostat, a microcontroller, and a Bluetooth low-energy (BLE) transceiver (Figure 1-17a). Although these braces-based biosensing devices are well suited for fitness or diagnostic applications, more discrete platforms are needed to extend their use, for example, for continuous glucose monitoring in daily life. Subsequently, the oral biosensing device has been further miniaturized as a removable "cavity sensor" device , to measure salivary glucose on the cuff (Figure 1-17b) [11]. Recently, researchers have developed an oral monitoring device to remotely measure sodium intake (Figure 1-17c) [12]. The chemical sensing layer was not tested for toxicity, so the actual oral application still needs to be further evaluated.
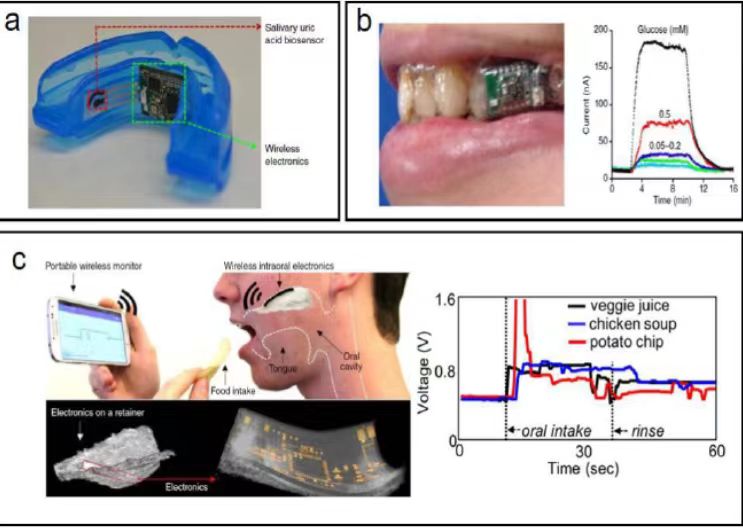
Figure 2. Oral wearable sensor braces sensors designed by Wang et al. for salivary uric acid analysis; (b) detachable " device for measuring sialary glucose on braces; (c) nutrient intake monitoring system using ultra-thin retractable electronics developed by researchers.
3. New technology and advantages of body fluid sampling
Microneedle technique as an emerging method of body fluid sampling has many significant advantages [13]. The size of the microneedle is usually between a few hundred micrometers and a few millimeters, much smaller than the traditional needle, and therefore able to reduce the pain feeling of patients and reduce the risk of bleeding and infection [14].The tip of the microneedle can be very fine, making the sample collection more accurate and controllable [15]. In addition, the use of microneedle sensors can also reduce the number of samples collected, especially for [16] and special groups such as children and the elderly. Another important advantage of microneedle technology is its high compatibility, which can be matched with various analytical instruments and methods to achieve rapid, sensitive and accurate sample detection [17]. Microneedle technology has a wide range of applications, including clinical diagnosis. Traditional blood glucose monitoring usually relies on blood collection from the patient's fingertips, although simple to operate, can cause discomfort and pain during frequent testing. In contrast, the microneedle technique creates tiny puncture points in the skin in a minimally invasive form to effectively obtain glucose in the intertissue fluid for blood glucose monitoring. (The monitoring of drug concentration is an important link to ensure the safe and effective treatment. Microneedle technology can be used to monitor real-time concentration changes of antibiotics, antiviral drugs in the body. This real-time feedback allows doctors to timely adjust medication schedules and improve treatment outcomes.), genetic testing(For some familial genetic diseases, such as cystic fibrosis and Duchenne muscular dystrophy, the application of microneedle technology has improved the convenience of genetic testing. Parents can regularly use microneedle technology to test their children to achieve early intervention and disease management.) and other fields. Therefore, the research and development of microneedle technology has become one of the hot spots in the field of biomedical and medical diagnosis, attracting the attention of a large number of researchers.
4. Problems and challenges
4.1. Beauty
When people buy goods, in addition to practicality, the requirements for their beauty are also constantly improving. Compared to large thick sensors, simple and portable, beautiful sensors are more attractive. However, the existing wearable sensors are still mostly functional, and the appearance design is not good. As the number of functions increases, so does the size of the sensor. How to reduce the sensor unit while ensuring its good sensor is also a topic that needs to be further studied in the future.
4.2. Privacy and Security
Diversification and intelligence are the development trends for wearable sensors. Which can not only monitor basic physiological indicators such as blood pressure and heart rate but also realize functions such as blood glucose monitoring, sleep monitoring and exercise data analysis. At the same time, with the development of artificial intelligence and big data technology, the data processing and analysis capabilities of sensors will be greatly improved to provide users with more accurate and personalized health management services.
However, the challenges facing wearable biosensors mainly come from the information technology and privacy security aspects. The accuracy and stability of the sensor are the most basic requirements, improve the accuracy, stability and anti-interference ability of the sensor, and optimize the algorithm to achieve more accurate data analysis and processing. The privacy and security of user data are also major issues. How to protect user private data and avoid data leakage and abuse is a question that sensor manufacturers and relevant departments need to seriously consider and solve.
5. Conclusion
In terms of sensor information collection, wearable bioelectrochemical sensors can transmit the monitoring information of each sensor element to the wearer in real time, reflecting the physiological health situation of the wearer or the safety situation of the surrounding environment without interruption. Build the sensor information collection and analysis system, and build the personal information level The development trend of wearable sensing devices is to continuously interact the sensor devices with nearby computing devices (such as mobile phones), automatically classify and analyze the monitoring signals, and provide timely intervention (e. g., to provide the health information of the wearer to the remote caregivers). In the future, it should develop in the direction of low cost, multi-parameter integration, low power consumption and high selectivity, and integrate various technologies and demands to promote wearable electrochemical sensors to practical applications. Only by continuously improving the technical level and ensuring data security, can we better promote the development of wearable sensors and provide people with more convenient and effective health management services. It is hoped that in the future, wearable electrochemical sensors can play a role in a wider range of fields and make a greater contribution to the cause of human health.
References
[1]. BANDODKAR A J, JEANG W J, GHAFFARI R, et al.Wearable sensors for biochemical sweat analysis[J].Annual Review of Analytical Chemistry, 2019, 12(1):1-22.
[2]. Kim, J.;Valdés-Ramírez, G.;Bandodkar, A.J.;Jia, W.Z.;Martinez, A.G.;Ramírez, J.;Mercier, P.;Wang, J.Noninvasive mouthguard biosensor for continuous salivary monitoring of metabolites.Analyst, 2014, 139(7), 1632-1636.
[3]. Rivera-Brown, A.M.;Quiñones-González, J.R.Normative data for sweat rate and whole-body sodium concentration in athletes indigenous to tropical climate.Int.J.Sport Nutr.Exerc.Metab., 2020, 30(4), 264-271.
[4]. Bandodkar, A.J.;Molinnus, D.;Mirza, O.;Guinovart, T.;Windmiller, J.R.;Valdés-Ramírez, G.;Andrade, F.J.;Schöning, M.J.;Wang, J.Epidermal tattoo potentiometric sodium sensors with wireless signal transduction for continuous non-invasive sweat monitoring.Biosens.Bioelectron., 2014, 54, 603-609.
[5]. Gao W, Emaminejad S, Nyein H Y Y, et al. Fully integrated wearable sensor arrays for multiplexed in situ perspiration analysis [J]. Nature, 2016, 529(7587): 509-514.
[6]. Tai L-C, Gao W, Chao M, et al. Methylxanthine Drug Monitoring with Wearable Sweat Sensors [J]. Advanced Materials, 2018, 30(23).
[7]. Martin A, Kim J, Kurniawan J F, et al. Epidermal Microfluidic Electrochemical Detection System: Enhanced Sweat Sampling and Metabolite Detection [J]. A Sensors, 2017, 2(12): 1860-1868.
[8]. Lee H, Song C, Hong Y S, et al. Wearable/disposable sweat-based glucose monitoring device with multistage transdermal drug delivery module [J]. Science Advances, 2017, 3(3).
[9]. Zhang Y, Guo H, Kim S B, et al. Passive sweat collection and colorimetric analysis of biomarkers relevant to kidney disorders using a soft microfluidic system [J]. Lab on a Chip, 2019, 19: 1545-1555.
[10]. Kim J, Wang J. Wearable salivary uric acid mouthguard biosensor with integrated wireless electronics [J]. Biosensors and Bioelectronics, 2015: 1061-1068.
[11]. Arakawa T, Kuroki Y, Nitta H, et al. Mouthguard biosensor with telemetry system for monitoring of saliva glucose: A novel cavitas sensor [J]. Biosensors & Bioelectronics, 2016: 106-111.
[12]. Lee Y, Howe C, Mishra S, et al. Wireless, Intraoral Hybrid Electronics for Real-Time Quantification of Sodium Intake Toward Hypertension Management [J]. Proceedings of the National Academy of Sciences, 2018, 115(21): 5377-5382.
[13]. SAMANT P P, PRAUSNITZ M R.Mechanisms of Sampling Interstitial Fluid from Skin Using a Microneedle Patch [J].Proceedings of the National Academy of Sciences of the United States of America, 2018, 115(18):4583-4588.
[14]. MA G J, WU C W.Microneedle, Bio-Microneedle and Bio-Inspired Microneedle:A Review [J].Journal of Controlled Release:Official Journal of the Controlled Release Society, 2017, 251:11-23.
[15]. HSIEH Y C, LIN C Y, LIN H Y, et al.Controllable-Swelling Microneedle-Assisted Ultrasensitive Paper Sensing Platforms for Personal Health Monitoring [J].Advanced Healthcare Materials, 2023, 12(24):e2300321.
[16]. FENG Y X, HU H, WONG Y Y, et al.Microneedles:an Emerging Vaccine Delivery Tool and a Prospective Solution to the Challenges of SARS-CoV-2 Mass Vaccination [J].Pharmaceutics, 2023, 15(5):1349.
[17]. KIM H, LEE J, HEO U, et al.Skin Preparation-Free, Stretchable Microneedle Adhesive Patches for Reliable Electrophysiological Sensing and Exoskeleton Robot Control [J].Science Advances, 2024, 10(3):5260.
Cite this article
Zhu,Z. (2025). Research on Real-time Body Fluid Analysis Based on Flexible Wearable Electrochemical Sensor for Health Monitoring. Theoretical and Natural Science,76,28-33.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 4th International Conference on Biological Engineering and Medical Science
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. BANDODKAR A J, JEANG W J, GHAFFARI R, et al.Wearable sensors for biochemical sweat analysis[J].Annual Review of Analytical Chemistry, 2019, 12(1):1-22.
[2]. Kim, J.;Valdés-Ramírez, G.;Bandodkar, A.J.;Jia, W.Z.;Martinez, A.G.;Ramírez, J.;Mercier, P.;Wang, J.Noninvasive mouthguard biosensor for continuous salivary monitoring of metabolites.Analyst, 2014, 139(7), 1632-1636.
[3]. Rivera-Brown, A.M.;Quiñones-González, J.R.Normative data for sweat rate and whole-body sodium concentration in athletes indigenous to tropical climate.Int.J.Sport Nutr.Exerc.Metab., 2020, 30(4), 264-271.
[4]. Bandodkar, A.J.;Molinnus, D.;Mirza, O.;Guinovart, T.;Windmiller, J.R.;Valdés-Ramírez, G.;Andrade, F.J.;Schöning, M.J.;Wang, J.Epidermal tattoo potentiometric sodium sensors with wireless signal transduction for continuous non-invasive sweat monitoring.Biosens.Bioelectron., 2014, 54, 603-609.
[5]. Gao W, Emaminejad S, Nyein H Y Y, et al. Fully integrated wearable sensor arrays for multiplexed in situ perspiration analysis [J]. Nature, 2016, 529(7587): 509-514.
[6]. Tai L-C, Gao W, Chao M, et al. Methylxanthine Drug Monitoring with Wearable Sweat Sensors [J]. Advanced Materials, 2018, 30(23).
[7]. Martin A, Kim J, Kurniawan J F, et al. Epidermal Microfluidic Electrochemical Detection System: Enhanced Sweat Sampling and Metabolite Detection [J]. A Sensors, 2017, 2(12): 1860-1868.
[8]. Lee H, Song C, Hong Y S, et al. Wearable/disposable sweat-based glucose monitoring device with multistage transdermal drug delivery module [J]. Science Advances, 2017, 3(3).
[9]. Zhang Y, Guo H, Kim S B, et al. Passive sweat collection and colorimetric analysis of biomarkers relevant to kidney disorders using a soft microfluidic system [J]. Lab on a Chip, 2019, 19: 1545-1555.
[10]. Kim J, Wang J. Wearable salivary uric acid mouthguard biosensor with integrated wireless electronics [J]. Biosensors and Bioelectronics, 2015: 1061-1068.
[11]. Arakawa T, Kuroki Y, Nitta H, et al. Mouthguard biosensor with telemetry system for monitoring of saliva glucose: A novel cavitas sensor [J]. Biosensors & Bioelectronics, 2016: 106-111.
[12]. Lee Y, Howe C, Mishra S, et al. Wireless, Intraoral Hybrid Electronics for Real-Time Quantification of Sodium Intake Toward Hypertension Management [J]. Proceedings of the National Academy of Sciences, 2018, 115(21): 5377-5382.
[13]. SAMANT P P, PRAUSNITZ M R.Mechanisms of Sampling Interstitial Fluid from Skin Using a Microneedle Patch [J].Proceedings of the National Academy of Sciences of the United States of America, 2018, 115(18):4583-4588.
[14]. MA G J, WU C W.Microneedle, Bio-Microneedle and Bio-Inspired Microneedle:A Review [J].Journal of Controlled Release:Official Journal of the Controlled Release Society, 2017, 251:11-23.
[15]. HSIEH Y C, LIN C Y, LIN H Y, et al.Controllable-Swelling Microneedle-Assisted Ultrasensitive Paper Sensing Platforms for Personal Health Monitoring [J].Advanced Healthcare Materials, 2023, 12(24):e2300321.
[16]. FENG Y X, HU H, WONG Y Y, et al.Microneedles:an Emerging Vaccine Delivery Tool and a Prospective Solution to the Challenges of SARS-CoV-2 Mass Vaccination [J].Pharmaceutics, 2023, 15(5):1349.
[17]. KIM H, LEE J, HEO U, et al.Skin Preparation-Free, Stretchable Microneedle Adhesive Patches for Reliable Electrophysiological Sensing and Exoskeleton Robot Control [J].Science Advances, 2024, 10(3):5260.