1. Introduction
Diabetes remains a pressing global health concern, with cardiovascular disease (CVD) remaining a leading cause of death in the diabetic population [1]. From 2009 to 2019, the death rate attributable to high Blood Pressure (BP) increased by 34.2%, with the actual number of deaths rising to 65.3% [2]. CVD is known as the most prominent cause of morbidity and mortality across the world. It is estimated that nearly 18 million global deaths are due to CVD in 2019 by the World Health Organization (WHO) [3].
Diabetes patients have higher risks of developing cardiovascular diseases [4-8], with a risk of 32.2% being affected by CVD [9]. It composed more than half of the mortality causes among diabetes patients [9-12]. Common risk factors of CVD are closely related to diabetes, including dysfunctions in the circulatory, nervous, and urinary systems. Hypertension, as one of the most correlating factors [13,14], inflicts 30% of Type I diabetes and 60% of Type II diabetes patients, increasing the risk of CVD among diabetes patients by damaging the glomerular basement membrane and leading to nephrotic syndromes [15]. Blood pressure is one of the factors for estimating the CVD prevalence risk; regulating blood pressure might lower the risks of CVD.
A meta-analysis of randomized controlled trials suggested that vitamin C supplements significantly decreased the serum level of fasting blood glucose [16], postprandial glycemia, and blood pressure [17]. The observed effect ostensibly attributable to a deficiency in this nutrient but could potentially stemmed from heightened vitamin C requirements among individuals with diabetes [18]. Carter et al. and Mazloom Z mentioned the lower level of vitamin C in the serum of diabetes patients [19,20], but further studies are still required. Vitamin D’s role in normalizing extracellular calcium enabled insulin secretion [21]. Increasing evidence indicates the association between vitamin D deficiency and insulin resistance, leading to higher blood glucose levels [22]. Though some research highlights the potential relationship between the serum level of vitamin D and the complications of diabetes [23], the evidence is still insufficient.
Although the cardiovascular and coronary heart disease mortality of type 2 diabetes patients decreased year by year, the mortality rate was still much higher than that of non-diabetic patients, which highlights the current absence of highly effective clinical strategies to mitigate cardiovascular mortality in diabetes patients [24]. The research on the influence of vitamins on diabetes and CVD remain inadequate, with obscure and inconsistent findings based on different study methods. More significantly, to our best knowledge, there is lack of studies connecting the diabetes and CVD controls when estimating the effects of vitamins. Therefore, an anomaly-detected, population-based study on influential factors is essential to prevent cardiovascular diabetes complications. The study may shed light on the CVD risk control among diabetes patients.
2. Method
2.1. Samples
NHANES (National Health and Nutrition Examination Survey) uses a multistage, probability sampling design to estimate the health and nutritional status of people in the United States. NHANES 2017-2018 data is picked from Center for Disease Control and Prevention’s National Center for Health Statistics site [25]. Diabetic and cardiovascular detection indicators as well as basic physical information are extracted from the datasets. The diabetic health was surveyed with the question “Have you ever been told by a doctor or health professional that you have diabetes or sugar diabetes” and average blood pressure after three readings is calculated for cardiovascular health. The Systolic Blood Pressure (SBP) \( ≥80 \) mm Hg and Diastolic Blood Pressure (DBP) \( ≥120 \) mm Hg is served as a stratifying standard. Age and BMI are potential confounding variables that may contribute to unforeseen outcomes and warrant meticulous consideration such as affecting BG and BP, so they are included in the models as covariates.
2.2. Variables and Outcomes
This study examines serum levels of Vitamin C, Vitamin D (D2 and D3), and their potential correlations with fasting blood glucose (FBG) levels, as well as systolic and diastolic blood pressure (BP). Age and BMI are considered as covariates.
Fasting Blood Glucose (FBG): Quantitatively measured by the UV In vitro test with the Roche/Hitachi cobas c311 system.
Vitamin D2 and D3 (SVD2+D3): Quantitatively measured via high-performance liquid chromatography-tandem mass spectrometry (HPLC-MS/MS).
Vitamin C (SVC): Measured by ultra-high performance liquid chromatography (UPLC) with electrochemical detection.
Systolic and Diastolic BP: Measured three times after 5 minutes of seated rest, with readings taken from the right arm unless contraindicated.
2.3. Shapley Additive Explanations
Shapley Additive Explanation (SHAP) is a method of model post-hoc interpretation, that constructs an additive explanatory model, where all features are treated as “contributors”. The core idea is to calculate the marginal contribution of features to the outputs of the model and explain the model we use from both global and local levels. In this study, Multiple Linear Regression model is put in the black box. A positive SHAP value suggested a positive contribution of the feature values on the predicted outcomes and larger values mean the feature has a greater effect.
2.4. Main Models
Study effects were assessed using Multiple Linear Regression and Logistic Regression methods to evaluate the effects of Vitamin C and Vitamin D on diabetic cardiovascular disease. Besides, Multiple Linear Regression’s kernel function was utilized to illustrate the distribution of feature plots and the SHAP values, where greater SHAP values suggest a more positive contribution of the feature values on the predicted outcomes.
3. Results
3.1. Associations between Vitamins C & D Serum Levels and BP & FBG
Total participants (n=2250) in NHANE cohort have a mean age of 45.10 (SD = 20.64) and a median BMI of 28.93 \( (kg/{m^{2}} \) ) (SD = 7.43). Participants are divided into four groups: Diabetes with CVD Risks, Diabetes Only, CVD Risks Only and No Diabetes nor CVD Risks (see Table 1). Older people have higher risks to develop a diabetes with the mean age of diabetes groups 62.31 (SD = 13.01) and no diabetes groups 42.32 (SD = 20.31). The average BMI levels in four groups all exceeded the standard BMI (18.5-25 \( kg/{m^{2}}) \) by World Health Organization (WHO), and BMI parameters also indicated significance differences between the diabetes with median 32.69(SD = 7.92) and no diabetes groups 28.33(SD = 7.17).
The average SVC among four groups all satisfied to the standard (0.6-1.0 mg/L) made by American Association for Clinical Chemistry (AACC). The average SVC in Diabetes and CVD risk group 0.79 mg/dL was found generally lower than that in other three groups, suggesting that the shortage of SVC may be a key factor that increase the cardiovascular diabetic disease risk. Moreover, the impact of vitamin C on individual symptoms remained to be discussed. For SVD, the average level in four groups all failed to meet the sufficient standard ( \( ≥75 nmol/L \) ) made by American’s Endocrine Society. However, higher SVD was found in diabetes groups with average level of 73.44 (32.41) than that in no diabetes groups 65.61 (30.73).
Table 1. Column with variables of different groups by mean and standard deviation analysis.
Variable | Diabetes and CVD risk (n=158) | Diabetes and No CVD risk (n=157) | No diabetes and CVD risk (n=965) | No diabetes and No CVD risk (n=970) | Total (n=2276) |
Age | 61.29 (12.42) | 63.43(13.33) | 43.05(20.69) | 41.63(20.00) | 45.10(20.64) |
BMI \( (kg/{m^{2}} \) ) | 32.45(8.18) | 32.92(7.70) | 28.48(7.36) | 28.14(6.96) | 28.93(7.43) |
Vitamin D in serum(nmol/L) | 72.52(33.31) | 74.43(31.73) | 66.52(31.21) | 64.77(30.34) | 66.69(31.08) |
Vitamin C in serum(mg/L) | 0.79(0.42) | 0.88(0.67) | 0.90(0.46) | 0.86(0.44) | 0.87(0.46) |
The means and standard deviations of BMI, age, SCV and SCD levels in each group Legend. The number outside the bracket is the mean and the one in the bracket is the standard deviation. Multiple linear regression model was used to the analysis with BMI and age serving as covariates, the results are shown in Table 2. For plasma fasting glucose, SVD was negatively correlated had significant influence \( (p=0.0374) \) . For systolic and diastolic blood pressure, significant effect was both found in SVD \( ({p_{Systolic}} \lt 0.0001, { p_{Diastolic}}=0.0240) \) and SVC \( ({p_{Systolic}} \lt 0.0001, {p_{Diastolic}}=0.0089) \) . Those factors were all negatively correlated with blood pressure. The result suggests that both vitamin D and vitamin C are helpful for Cardiovascular Health while vitamin D is also helpful to lower the risk of diabetes.
Table 2. Relationship between factors and Diabetes and CVD risk.
Factors | Estimate | Spearman correlation coefficient | p-value | Outcome |
BMI \( (kg/{m^{2}} \) ) | 0.7416 | 0.3033 | < 0.0001 | Plasma fasting glucose |
Age | 0.4722 | 0.4281 | < 0.0001 | |
Vitamin D in serum(nmol/L) | -0.0505 | 0.0971 | 0.0374 | |
Vitamin C in serum(mg/L) | -1.7072 | -0.0856 | 0.2596 | |
BMI \( (kg/{m^{2}} \) ) | 0.3074 | 0.2816 | < 0.0001 | Systolic blood pressure |
Age | 0.5031 | 0.5647 | <0.0001 | |
Vitamin D in serum(nmol/L) | -0.0464 | 0.0790 | < 0.0001 | |
Vitamin C in serum(mg/L) | -1.9431 | -0.0953 | 0.0074 | |
BMI \( (kg/{m^{2}} \) ) | 0.2109 | 0.1863 | <0.0001 | Diastolic blood pressure |
Age | 0.1102 | 0.2153 | <0.0001 | |
Vitamin D in serum(nmol/L) | -0.0205 | -0.0005 | 0.0240 | |
Vitamin C in serum (mg/L) | -1.4807 | -0.1012 | 0.0089 |
Using logistic regression, significance impact of SVC and SVD was found on cardiovascular diabetic participants. 75 nmol/L of SVD was discovered as the turning point, which was also the standard threshold for sufficient SVD worldwide. When the SVD was below the sufficient standard, the probability of having diabetic cardiovascular disease would also decrease (0.006%) with the increased SVD (see Figure 1). However, excess content (above standards) may have a negative effect on lowing diabetic and CVD risks, with a forward correlated (0.08%) fitting curve shows in second graph of Figure 1. Furthermore, the logistic regression model shows a high precision of 95% in SVD \( \lt 75 nmol/L \) , 92% in SVD \( ≥75 nmol/L \) , showing the reliability of model results.
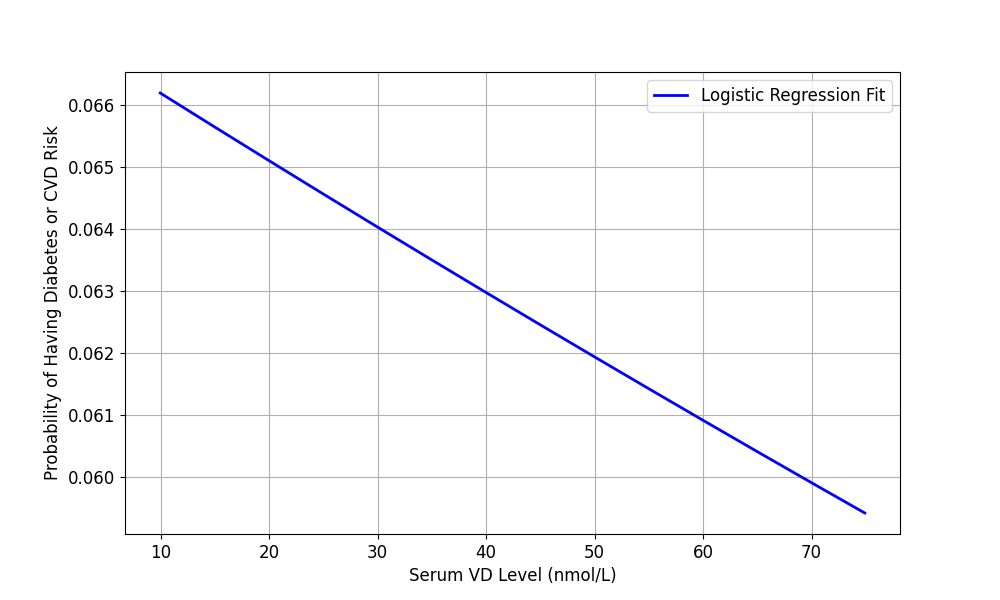
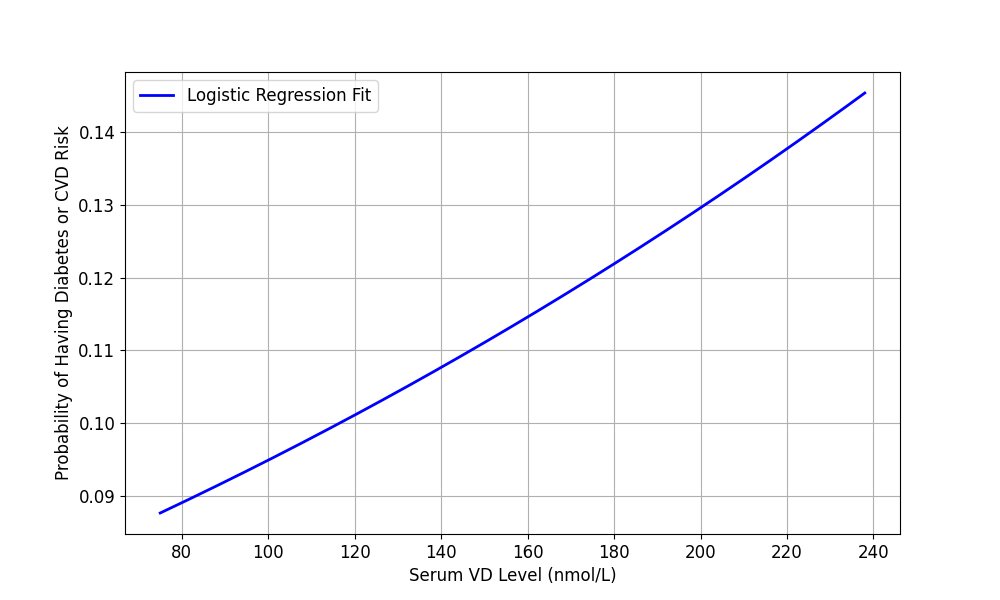
Figure 1. Logistic Regression Fit for Serum VD Level and Health Risks (VD < 75 nmol/L and VD≧75 nmol/L).
3.2. SHAP values
According to the graphs of the visualized SHAP values for the Multiple Linear Regression, bluer dots represent lower feature values and red dots represent higher feature values. Clear contribution coefficients are shown by SHAP values. Since the color of the accumulated dots are bluer when the SHAP values are smaller (see Figure 2), advanced age and higher BMI both contributed to higher FBG (SHAP value of age = 9.75, SHAP value of BMI = 5.51) and BP (SHAP value of age = 10.39 and 2.28, SHAP value of BMI = 2.28 and 1.56), indicating that elder or more obese people are more likely to have higher blood glucose level and blood pressure.
Negative SHAP values observed for higher feature values of SVC implied an inverse relationship with FBG (SHAP value = -1.57) and BP (SHAP value = -1.44 and -0.64) in prediction as shown in Figure 2. Thus, lower SVC may correlate with elevated fasting blood glucose and blood pressure, potentially increasing risks for diabetes and cardiovascular diseases.
The distribution of higher feature values of SVD indicated negative impacts on FBG (SHAP value = -0.80) and BP (SHAP value = -0.91 and -0.69) (see Figure 2), particularly among individuals with higher vitamin D levels. Negative SHAP values for SVD concerning fasting blood glucose and blood pressure suggested that as vitamin D levels rise, fasting blood glucose and blood pressure tend to decrease.

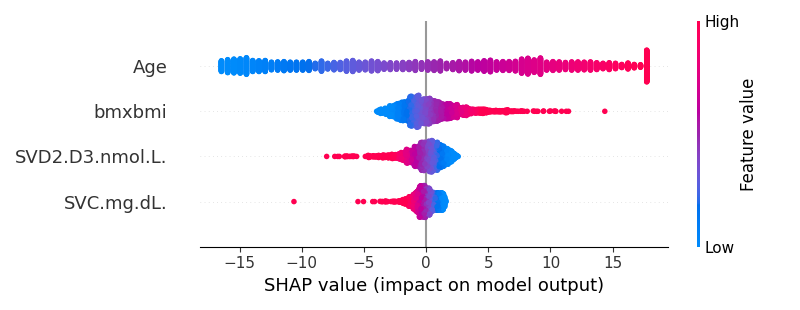
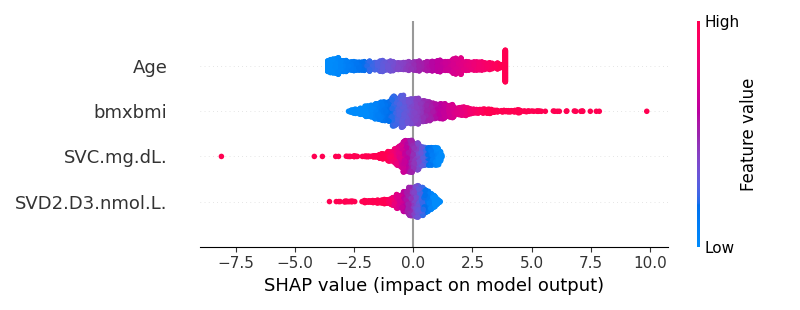
Figure 2. SVR for the Blood Glucose Level, Systolic Blood Pressure and Diastolic Blood Pressure.
4. Discussion
In our research, the serum levels of vitamin C and vitamin D exhibited an inverse correlation with blood pressure, which is consistent with several studies [26-29]. It might because vitamin C mitigate oxidative damage to blood vessels, thereby promoting their elasticity and facilitating glutathione (GSH) synthesis to mitigate hypertension according to the free radical theory [30,31]. Vitamin D functions include vasodilation [32], inhibition of cellular proliferation and myocardial hypertrophy [33], and prevention of vascular calcification through ion balance [34]. Moreover, it was observed in our study that a low serum vitamin D level was associated with elevated blood glucose levels, a relationship potentially elucidated through its effects on pancreatic beta cells and insulin sensitivity [35]. This correlation is substantiated by prior investigations [36,37].
The positive correlation, shown in the logistic regression model, between vitamin D serum level and probability of having cardiovascular diabetic disease when SVD level is greater than the normal. It might be due to the overdose of vitamin D would cause metabolic dysfunctions. Some participants could have imbalanced and unhealthy diets that lead to the abnormally high level of vitamin D, which causes hypercalcemia and other symptoms of toxicity, resulting in negative impacts on blood pressure and blood glucose level.
The relationship between vitamin C levels in serum and blood glucose levels was not significant in this study, which is inconsistent with some studies suggesting a negative association [38,39]. A possible explanation was the effects of other confounding variables excluded from the study. Physical activities and daily diets could affect the metabolism mechanisms, and intake and absorbed amounts of nutrients, which influence the blood glucose level and blood pressure afterwards [40].
The partial definition of CVD risks might also partly cause results deviation. Due to the limited data without a definite diagnosis of CVD, only hypertension was considered as a factor that increases the CVD risk. Besides, the number of samples was marginally inadequate when being divided into the group of having both diabetes and CVD risks. A larger sample size might depict a more pronounced picture of the correlations.
Despite the growing body of research on the roles of vitamins in relieving health issues, there remains a notable lack of comprehensive studies estimating the effects of vitamin C and vitamin D on reducing diabetic cardiovascular disease risks, and the study aims to fill the gap. The significance of this research lies not only in discovering vitamins' potentials but also in their implications for clinical practice. The results suggest that vitamin C and vitamin D levels in serum are vital on preventing CVD in diabetic patients. Thus, to maintain healthy vitamin C and vitamin D levels and prevent the complication, dietary improvements, vitamin supplements control, and medications might be required to facilitate metabolism efficiency.
5. Conclusion
Based on the results and discussions above, the conclusions of this research are listed as follows:
Vitamin D in serum was negatively correlated with plasma fasting glucose with significant influence.
The serum levels of vitamin C and vitamin D present an inverse correlation with systolic and diastolic blood pressure.
It was concluded that higher vitamin C and vitamin D levels in serum might be beneficial in diabetic CVD prevention by lowering both blood glucose levels and blood pressure. The effect of vitamin D has a turning point. When the content level was below that threshold, the probability of having diabetic cardiovascular disease decreases while the serum vitamin levels increased.
Acknowledgement
Nanchen Hu, Fan Xia, Hanna Li contributed equally to this work and should be considered co-first authors.
References
[1]. Yang F, Wang M, Du J, Fu Y, Deng J, Wu J, Zhang Y, Li Y. Predicting life span of type 2 diabetes patients through alkaline phosphatase and vitamin D: Results from NHANES 1999-2018. Atherosclerosis. 2024 Jul;394:117318. doi: 10.1016/j.atherosclerosis.2023.117318. Epub 2023 Oct 5. PMID: 37839936.
[2]. C. W. Tsao et al., “Heart disease and stroke statistics-2022 update: a report from the american heart association, ” Circulation, vol. 145, no. 8, pp. E153–E639, 2022, doi: 10.1161/CIR.0000000000001052
[3]. Zhang H, Dhalla NS. The Role of Pro-Inflammatory Cytokines in the Pathogenesis of Cardiovascular Disease. Int J Mol Sci. 2024 Jan 16;25(2):1082. doi: 10.3390/ijms25021082. PMID: 38256155; PMCID: PMC10817020.
[4]. Glovaci, D., Fan, W., & Wong, N. D. (2019). Epidemiology of Diabetes Mellitus and Cardiovascular Disease. Current Cardiology Reports, 21(4), 1–8. https://doi.org/10.1007/s11886-019-1107-y
[5]. Wilson, P. W. F., D’Agostino, R. B., Levy, D., Belanger, A. M., Silbershatz, H., & Kannel, W. B. (1998). Prediction of Coronary Heart Disease Using Risk Factor Categories. Circulation, 97(18), 1837–1847. https://doi.org/10.1161/01.cir.97.18.1837
[6]. Wilson, P. (1998). Diabetes mellitus and coronary heart disease. American Journal of Kidney Diseases, 32(5), S89–S100. https://doi.org/10.1053/ajkd.1998.v32.pm9820468
[7]. McGill, H. C., & McMahan, C. A. (1998). Determinants of atherosclerosis in the young. The American Journal of Cardiology, 82(10, Supplement 2), 30–36. https://doi.org/10.1016/S0002-9149(98)00720-6
[8]. Selvin, E., Marinopoulos, S., Berkenblit, G., Rami, T., Brancati, F. L., Powe, N. R., & Golden, S. H. (2004). Meta-analysis: glycosylated hemoglobin and cardiovascular disease in diabetes mellitus. Annals of Internal Medicine, 141(6), 421–431. https://doi.org/10.7326/0003-4819-141-6-200409210-00007
[9]. Einarson, T. R., Acs, A., Ludwig, C., & Panton, U. H. (2018). Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovascular Diabetology, 17(1). https://doi.org/10.1186/s12933-018-0728-6
[10]. Matheus, A. S. de M., Tannus, L. R. M., Cobas, R. A., Palma, C. C. S., Negrato, C. A., & Gomes, M. de B. (2013). Impact of Diabetes on Cardiovascular Disease: An Update. International Journal of Hypertension, 2013, 1–15. https://doi.org/10.1155/2013/653789
[11]. Orasanu G. and Plutzky J., (2009). The pathologic continuum of diabetic vascular disease, Journal of the American College of Cardiology. 53, no. 5, S35–S42, 2-s2.0-58549094758, https://doi.org/10.1016/j.jacc.2008.09.055.
[12]. Kemp T. M., Barr E. L. M., Zimmet P. Z., Cameron A. J., Welborn T. A., Colagiuri S., Phillips P., and Shaw J. E., Glucose, lipid, and blood pressure control in Australian adults with type 2 diabetes: the 1999–2000 AusDiab, Diabetes Care. (2005) 28, no. 6, 1490–1492, 2-s2.0-19944387957, https://doi.org/10.2337/diacare.28.6.1490
[13]. Petrie, J. R., Guzik, T. J., & Touyz, R. M. (2018). Diabetes, Hypertension, and Cardiovascular Disease: Clinical Insights and Vascular Mechanisms. The Canadian Journal of Cardiology, 34(5), 575–584. https://doi.org/10.1016/j.cjca.2017.12.005
[14]. Ettehad, D., Emdin, C. A., Kiran, A., Anderson, S. G., Callender, T., Emberson, J., Chalmers, J., Rodgers, A., & Rahimi, K. (2016). Blood pressure lowering for prevention of cardiovascular disease and death: A systematic review and meta-analysis. The Lancet, 387(10022), 957–967. https://doi.org/10.1016/s0140-6736(15)01225-8
[15]. Leon, B. M., & Maddox, T. M. (2015). Diabetes and cardiovascular disease: Epidemiology, biological mechanisms, treatment recommendations and future research. World Journal of Diabetes, 6(13), 1246. https://doi.org/10.4239/wjd.v6.i13.1246
[16]. Saeed Nosratabadi, Damoon Ashtary‐Larky, Fatemeh Hoseini, Zahra Namkhah, Mohammadi, S., Salamat, S., Nadery, M., Sazin Yarmand, Zamani, M., & Omid Asbaghi. (2023). The effects of vitamin C supplementation on glycemic control in patients with type 2 diabetes: A systematic review and meta-analysis. Diabetes & Metabolic Syndrome: Clinical Research and Reviews, 17(8), 102824–102824. https://doi.org/10.1016/j.dsx.2023.102824
[17]. Mason, S. A., Rasmussen, B., van Loon, L. J. C., Salmon, J., & Wadley, G. D. (2018). Ascorbic acid supplementation improves postprandial glycaemic control and blood pressure in individuals with type 2 diabetes: Findings of a randomized cross-over trial. Diabetes, Obesity and Metabolism, 21(3), 674–682. https://doi.org/10.1111/dom.13571
[18]. Dakhale, G. N., Chaudhari, H. V., & Shrivastava, M. (2011). Supplementation of Vitamin C Reduces Blood Glucose and Improves Glycosylated Hemoglobin in Type 2 Diabetes Mellitus: A Randomized, Double-Blind Study. Advances in Pharmacological Sciences, 2011, 1–5. https://doi.org/10.1155/2011/195271
[19]. Carter, P., Gray, L. J., Talbot, D., Morris, D. H., Khunti, K., & Davies, M. J. (2012). Fruit and vegetable intake and the association with glucose parameters: a cross-sectional analysis of the Let’s Prevent Diabetes Study. European Journal of Clinical Nutrition, 67(1), 12–17. https://doi.org/10.1038/ejcn.2012.174
[20]. Mazloom Z, Hejazi N, Dabbaghmanesh MH, Tabatabaei HR, Ahmadi A, Ansar H (2011). Effect of vitamin C supplementation on postprandial oxidative stress and lipid profile in type 2 diabetic patients. Pak J Biol Sci. 2011, 14:900-4. 10.3923/pjbs.2011.900.904
[21]. Martin, T., & Campbell, R. K. (2011). Vitamin D and Diabetes. Diabetes Spectrum, 24(2), 113–118. https://doi.org/10.2337/diaspect.24.2.113
[22]. Glaucia Carneiro, Blandine Laferrère, &Maria Teresa Zanella (2013). Vitamin and mineral deficiency and glucose metabolism – A review
[23]. Raghuvanshi, D. S., Chakole, S., & Kumar, M. (2023). Relationship Between Vitamins and Diabetes. Cureus. https://doi.org/10.7759/cureus.36815
[24]. Deng, W. B., Huang, S. Q., Yu, L. S., & Li, L. H. (2023). Advances in the Study of Cardiovascular Dis-ease Complicated by Diabetes Mellitus[J]. Advances in Clinical Medicine, 13(2), 1302-1307. https://doi.org/10.12677/ACM.2023.132179
[25]. Carr AC, Lunt H, Wareham NJ, Myint PK. Estimating Vitamin C Intake Requirements in Diabetes Mellitus: Analysis of NHANES 2017-2018 and EPIC-Norfolk Cohorts. Antioxidants (Basel). 2023 Oct 15;12(10):1863. doi: 10.3390/antiox12101863. PMID: 37891943; PMCID: PMC10604478.
[26]. Ran, L., Zhao, W., Tan, X., Wang, H., Mizuno, K., Takagi, K., Zhao, Y., & Bu, H. (2020). Association between Serum Vitamin C and the Blood Pressure: A Systematic Review and Meta-Analysis of Observational Studies. Cardiovascular Therapeutics, 2020, 1–11. https://doi.org/10.1155/2020/4940673
[27]. Chen, J., He, J., Hamm, L., Batuman, V., & Whelton, P. K. (2002). Serum Antioxidant Vitamins and Blood Pressure in the United States Population. Hypertension, 40(6), 810–816. https://doi.org/10.1161/01.hyp.0000039962.68332.59
[28]. Mokhtari, E., Hajhashemy, Z., & Saneei, P. (2022). Serum Vitamin D Levels in Relation to Hypertension and Pre-hypertension in Adults: A Systematic Review and Dose–Response Meta-Analysis of Epidemiologic Studies. Frontiers in Nutrition, 9. https://doi.org/10.3389/fnut.2022.829307
[29]. van Ballegooijen, A. J., Cepelis, A., Visser, M., Brouwer, I. A., van Schoor, N. M., & Beulens, J. W. (2017). Joint Association of Low Vitamin D and Vitamin K Status With Blood Pressure and Hypertension. Hypertension, 69(6), 1165–1172. https://doi.org/10.1161/hypertensionaha.116.08869
[30]. Sj, P., A, K., Y, W., P, E., O, K., Jh, L., S, C., C, C., A, D., Sk, D., & M, L. (2003, February 1). Vitamin C as an Antioxidant: Evaluation of Its Role in Disease Prevention. Journal of the American College of Nutrition. https://pubmed.ncbi.nlm.nih.gov/12569111/
[31]. Mihailović, M. B., Avramović, D. M., Jovanović, I. B., Pesut, O. J., Matić, D. P., & Stojanov, V. J. (1998). Blood and plasma selenium levels and GSH-Px activities in patients with arterial hypertension and chronic heart disease. Journal of Environmental Pathology, Toxicology and Oncology: Official Organ of the International Society for Environmental Toxicology and Cancer, 17(3-4), 285–289. https://pubmed.ncbi.nlm.nih.gov/9726804/
[32]. Judd, S. E., & Tangpricha, V. (2009). Vitamin D Deficiency and Risk for Cardiovascular Disease. The American Journal of the Medical Sciences, 338(1), 40–44. https://doi.org/10.1097/maj.0b013e3181aaee91
[33]. Martins, D., Wolf, M., Pan, D., Zadshir, A., Tareen, N., Thadhani, R., Felsenfeld, A., Levine, B., Mehrotra, R., & Norris, K. (2007). Prevalence of Cardiovascular Risk Factors and the Serum Levels of 25-Hydroxyvitamin D in the United States. Archives of Internal Medicine, 167(11), 1159. https://doi.org/10.1001/archinte.167.11.1159
[34]. Zhang, D., Cheng, C., Wang, Y., Sun, H., Yu, S., Xue, Y., Liu, Y., Li, W., & Li, X. (2020). Effect of Vitamin D on Blood Pressure and Hypertension in the General Population: An Update Meta-Analysis of Cohort Studies and Randomized Controlled Trials. Preventing Chronic Disease, 17. https://doi.org/10.5888/pcd17.190307
[35]. Chandler, P. D., Giovannucci, E., Scott, J., Bennett, G. F., Ng, K., Chan, A. T., Hollis, B. W., Rifai, N., Emmons, K. M., Fuchs, C. S., & Drake, B. F. (2015). Effects of Vitamin D Supplementation on C-peptide and 25-hydroxyvitamin D Concentrations at 3 and 6 Months. 5(1). https://doi.org/10.1038/srep10411
[36]. Bhatt, S. P., Misra, A., Gulati, S., Singh, N., & Pandey, R. M. (2018). Lower vitamin D levels are associated with higher blood glucose levels in Asian Indian women with pre-diabetes: a population-based cross-sectional study in North India. BMJ Open Diabetes Research & Care, 6(1), e000501. https://doi.org/10.1136/bmjdrc-2017-000501
[37]. Fondjo, L. A., Sakyi, S. A., Owiredu, W. K. B. A., Laing, E. F., Owiredu, E.-W., Awusi, E. K., Ephraim, R. K. D., & Kantanka, O. S. (2018). Evaluating Vitamin D Status in Pre- and Postmenopausal Type 2 Diabetics and Its Association with Glucose Homeostasis. BioMed Research International, 2018, 1–12. https://doi.org/10.1155/2018/9369282
[38]. Girgis, C., Christie-David, D., & Gunton, J. (2015). Effects of vitamins C and D in type 2 diabetes mellitus. Nutrition and Dietary Supplements, 21. https://doi.org/10.2147/nds.s52022
[39]. Yedjou, C. G., Grigsby, J., Mbemi, A., Nelson, D., Mildort, B., Lekan Latinwo, & Tchounwou, P. B. (2023). The Management of Diabetes Mellitus Using Medicinal Plants and Vitamins. International Journal of Molecular Sciences, 24(10), 9085–9085. https://doi.org/10.3390/ijms24109085
[40]. Yokoyama, T., Date, C., Kokubo, Y., Yoshiike, N., Matsumura, Y., & Tanaka, H. (2000). Serum Vitamin C Concentration Was Inversely Associated With Subsequent 20-Year Incidence of Stroke in a Japanese Rural Community. Stroke, 31(10), 2287–2294. https://doi.org/10.1161/01.str.31.10.2287
Cite this article
Hu,N.;Xia,F.;Li,H. (2025). Potential Effects of Levels of Vitamin C and Vitamin D in Serum on Diabetic Cardiovascular Diseases Prevention. Theoretical and Natural Science,78,195-204.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 4th International Conference on Biological Engineering and Medical Science
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Yang F, Wang M, Du J, Fu Y, Deng J, Wu J, Zhang Y, Li Y. Predicting life span of type 2 diabetes patients through alkaline phosphatase and vitamin D: Results from NHANES 1999-2018. Atherosclerosis. 2024 Jul;394:117318. doi: 10.1016/j.atherosclerosis.2023.117318. Epub 2023 Oct 5. PMID: 37839936.
[2]. C. W. Tsao et al., “Heart disease and stroke statistics-2022 update: a report from the american heart association, ” Circulation, vol. 145, no. 8, pp. E153–E639, 2022, doi: 10.1161/CIR.0000000000001052
[3]. Zhang H, Dhalla NS. The Role of Pro-Inflammatory Cytokines in the Pathogenesis of Cardiovascular Disease. Int J Mol Sci. 2024 Jan 16;25(2):1082. doi: 10.3390/ijms25021082. PMID: 38256155; PMCID: PMC10817020.
[4]. Glovaci, D., Fan, W., & Wong, N. D. (2019). Epidemiology of Diabetes Mellitus and Cardiovascular Disease. Current Cardiology Reports, 21(4), 1–8. https://doi.org/10.1007/s11886-019-1107-y
[5]. Wilson, P. W. F., D’Agostino, R. B., Levy, D., Belanger, A. M., Silbershatz, H., & Kannel, W. B. (1998). Prediction of Coronary Heart Disease Using Risk Factor Categories. Circulation, 97(18), 1837–1847. https://doi.org/10.1161/01.cir.97.18.1837
[6]. Wilson, P. (1998). Diabetes mellitus and coronary heart disease. American Journal of Kidney Diseases, 32(5), S89–S100. https://doi.org/10.1053/ajkd.1998.v32.pm9820468
[7]. McGill, H. C., & McMahan, C. A. (1998). Determinants of atherosclerosis in the young. The American Journal of Cardiology, 82(10, Supplement 2), 30–36. https://doi.org/10.1016/S0002-9149(98)00720-6
[8]. Selvin, E., Marinopoulos, S., Berkenblit, G., Rami, T., Brancati, F. L., Powe, N. R., & Golden, S. H. (2004). Meta-analysis: glycosylated hemoglobin and cardiovascular disease in diabetes mellitus. Annals of Internal Medicine, 141(6), 421–431. https://doi.org/10.7326/0003-4819-141-6-200409210-00007
[9]. Einarson, T. R., Acs, A., Ludwig, C., & Panton, U. H. (2018). Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovascular Diabetology, 17(1). https://doi.org/10.1186/s12933-018-0728-6
[10]. Matheus, A. S. de M., Tannus, L. R. M., Cobas, R. A., Palma, C. C. S., Negrato, C. A., & Gomes, M. de B. (2013). Impact of Diabetes on Cardiovascular Disease: An Update. International Journal of Hypertension, 2013, 1–15. https://doi.org/10.1155/2013/653789
[11]. Orasanu G. and Plutzky J., (2009). The pathologic continuum of diabetic vascular disease, Journal of the American College of Cardiology. 53, no. 5, S35–S42, 2-s2.0-58549094758, https://doi.org/10.1016/j.jacc.2008.09.055.
[12]. Kemp T. M., Barr E. L. M., Zimmet P. Z., Cameron A. J., Welborn T. A., Colagiuri S., Phillips P., and Shaw J. E., Glucose, lipid, and blood pressure control in Australian adults with type 2 diabetes: the 1999–2000 AusDiab, Diabetes Care. (2005) 28, no. 6, 1490–1492, 2-s2.0-19944387957, https://doi.org/10.2337/diacare.28.6.1490
[13]. Petrie, J. R., Guzik, T. J., & Touyz, R. M. (2018). Diabetes, Hypertension, and Cardiovascular Disease: Clinical Insights and Vascular Mechanisms. The Canadian Journal of Cardiology, 34(5), 575–584. https://doi.org/10.1016/j.cjca.2017.12.005
[14]. Ettehad, D., Emdin, C. A., Kiran, A., Anderson, S. G., Callender, T., Emberson, J., Chalmers, J., Rodgers, A., & Rahimi, K. (2016). Blood pressure lowering for prevention of cardiovascular disease and death: A systematic review and meta-analysis. The Lancet, 387(10022), 957–967. https://doi.org/10.1016/s0140-6736(15)01225-8
[15]. Leon, B. M., & Maddox, T. M. (2015). Diabetes and cardiovascular disease: Epidemiology, biological mechanisms, treatment recommendations and future research. World Journal of Diabetes, 6(13), 1246. https://doi.org/10.4239/wjd.v6.i13.1246
[16]. Saeed Nosratabadi, Damoon Ashtary‐Larky, Fatemeh Hoseini, Zahra Namkhah, Mohammadi, S., Salamat, S., Nadery, M., Sazin Yarmand, Zamani, M., & Omid Asbaghi. (2023). The effects of vitamin C supplementation on glycemic control in patients with type 2 diabetes: A systematic review and meta-analysis. Diabetes & Metabolic Syndrome: Clinical Research and Reviews, 17(8), 102824–102824. https://doi.org/10.1016/j.dsx.2023.102824
[17]. Mason, S. A., Rasmussen, B., van Loon, L. J. C., Salmon, J., & Wadley, G. D. (2018). Ascorbic acid supplementation improves postprandial glycaemic control and blood pressure in individuals with type 2 diabetes: Findings of a randomized cross-over trial. Diabetes, Obesity and Metabolism, 21(3), 674–682. https://doi.org/10.1111/dom.13571
[18]. Dakhale, G. N., Chaudhari, H. V., & Shrivastava, M. (2011). Supplementation of Vitamin C Reduces Blood Glucose and Improves Glycosylated Hemoglobin in Type 2 Diabetes Mellitus: A Randomized, Double-Blind Study. Advances in Pharmacological Sciences, 2011, 1–5. https://doi.org/10.1155/2011/195271
[19]. Carter, P., Gray, L. J., Talbot, D., Morris, D. H., Khunti, K., & Davies, M. J. (2012). Fruit and vegetable intake and the association with glucose parameters: a cross-sectional analysis of the Let’s Prevent Diabetes Study. European Journal of Clinical Nutrition, 67(1), 12–17. https://doi.org/10.1038/ejcn.2012.174
[20]. Mazloom Z, Hejazi N, Dabbaghmanesh MH, Tabatabaei HR, Ahmadi A, Ansar H (2011). Effect of vitamin C supplementation on postprandial oxidative stress and lipid profile in type 2 diabetic patients. Pak J Biol Sci. 2011, 14:900-4. 10.3923/pjbs.2011.900.904
[21]. Martin, T., & Campbell, R. K. (2011). Vitamin D and Diabetes. Diabetes Spectrum, 24(2), 113–118. https://doi.org/10.2337/diaspect.24.2.113
[22]. Glaucia Carneiro, Blandine Laferrère, &Maria Teresa Zanella (2013). Vitamin and mineral deficiency and glucose metabolism – A review
[23]. Raghuvanshi, D. S., Chakole, S., & Kumar, M. (2023). Relationship Between Vitamins and Diabetes. Cureus. https://doi.org/10.7759/cureus.36815
[24]. Deng, W. B., Huang, S. Q., Yu, L. S., & Li, L. H. (2023). Advances in the Study of Cardiovascular Dis-ease Complicated by Diabetes Mellitus[J]. Advances in Clinical Medicine, 13(2), 1302-1307. https://doi.org/10.12677/ACM.2023.132179
[25]. Carr AC, Lunt H, Wareham NJ, Myint PK. Estimating Vitamin C Intake Requirements in Diabetes Mellitus: Analysis of NHANES 2017-2018 and EPIC-Norfolk Cohorts. Antioxidants (Basel). 2023 Oct 15;12(10):1863. doi: 10.3390/antiox12101863. PMID: 37891943; PMCID: PMC10604478.
[26]. Ran, L., Zhao, W., Tan, X., Wang, H., Mizuno, K., Takagi, K., Zhao, Y., & Bu, H. (2020). Association between Serum Vitamin C and the Blood Pressure: A Systematic Review and Meta-Analysis of Observational Studies. Cardiovascular Therapeutics, 2020, 1–11. https://doi.org/10.1155/2020/4940673
[27]. Chen, J., He, J., Hamm, L., Batuman, V., & Whelton, P. K. (2002). Serum Antioxidant Vitamins and Blood Pressure in the United States Population. Hypertension, 40(6), 810–816. https://doi.org/10.1161/01.hyp.0000039962.68332.59
[28]. Mokhtari, E., Hajhashemy, Z., & Saneei, P. (2022). Serum Vitamin D Levels in Relation to Hypertension and Pre-hypertension in Adults: A Systematic Review and Dose–Response Meta-Analysis of Epidemiologic Studies. Frontiers in Nutrition, 9. https://doi.org/10.3389/fnut.2022.829307
[29]. van Ballegooijen, A. J., Cepelis, A., Visser, M., Brouwer, I. A., van Schoor, N. M., & Beulens, J. W. (2017). Joint Association of Low Vitamin D and Vitamin K Status With Blood Pressure and Hypertension. Hypertension, 69(6), 1165–1172. https://doi.org/10.1161/hypertensionaha.116.08869
[30]. Sj, P., A, K., Y, W., P, E., O, K., Jh, L., S, C., C, C., A, D., Sk, D., & M, L. (2003, February 1). Vitamin C as an Antioxidant: Evaluation of Its Role in Disease Prevention. Journal of the American College of Nutrition. https://pubmed.ncbi.nlm.nih.gov/12569111/
[31]. Mihailović, M. B., Avramović, D. M., Jovanović, I. B., Pesut, O. J., Matić, D. P., & Stojanov, V. J. (1998). Blood and plasma selenium levels and GSH-Px activities in patients with arterial hypertension and chronic heart disease. Journal of Environmental Pathology, Toxicology and Oncology: Official Organ of the International Society for Environmental Toxicology and Cancer, 17(3-4), 285–289. https://pubmed.ncbi.nlm.nih.gov/9726804/
[32]. Judd, S. E., & Tangpricha, V. (2009). Vitamin D Deficiency and Risk for Cardiovascular Disease. The American Journal of the Medical Sciences, 338(1), 40–44. https://doi.org/10.1097/maj.0b013e3181aaee91
[33]. Martins, D., Wolf, M., Pan, D., Zadshir, A., Tareen, N., Thadhani, R., Felsenfeld, A., Levine, B., Mehrotra, R., & Norris, K. (2007). Prevalence of Cardiovascular Risk Factors and the Serum Levels of 25-Hydroxyvitamin D in the United States. Archives of Internal Medicine, 167(11), 1159. https://doi.org/10.1001/archinte.167.11.1159
[34]. Zhang, D., Cheng, C., Wang, Y., Sun, H., Yu, S., Xue, Y., Liu, Y., Li, W., & Li, X. (2020). Effect of Vitamin D on Blood Pressure and Hypertension in the General Population: An Update Meta-Analysis of Cohort Studies and Randomized Controlled Trials. Preventing Chronic Disease, 17. https://doi.org/10.5888/pcd17.190307
[35]. Chandler, P. D., Giovannucci, E., Scott, J., Bennett, G. F., Ng, K., Chan, A. T., Hollis, B. W., Rifai, N., Emmons, K. M., Fuchs, C. S., & Drake, B. F. (2015). Effects of Vitamin D Supplementation on C-peptide and 25-hydroxyvitamin D Concentrations at 3 and 6 Months. 5(1). https://doi.org/10.1038/srep10411
[36]. Bhatt, S. P., Misra, A., Gulati, S., Singh, N., & Pandey, R. M. (2018). Lower vitamin D levels are associated with higher blood glucose levels in Asian Indian women with pre-diabetes: a population-based cross-sectional study in North India. BMJ Open Diabetes Research & Care, 6(1), e000501. https://doi.org/10.1136/bmjdrc-2017-000501
[37]. Fondjo, L. A., Sakyi, S. A., Owiredu, W. K. B. A., Laing, E. F., Owiredu, E.-W., Awusi, E. K., Ephraim, R. K. D., & Kantanka, O. S. (2018). Evaluating Vitamin D Status in Pre- and Postmenopausal Type 2 Diabetics and Its Association with Glucose Homeostasis. BioMed Research International, 2018, 1–12. https://doi.org/10.1155/2018/9369282
[38]. Girgis, C., Christie-David, D., & Gunton, J. (2015). Effects of vitamins C and D in type 2 diabetes mellitus. Nutrition and Dietary Supplements, 21. https://doi.org/10.2147/nds.s52022
[39]. Yedjou, C. G., Grigsby, J., Mbemi, A., Nelson, D., Mildort, B., Lekan Latinwo, & Tchounwou, P. B. (2023). The Management of Diabetes Mellitus Using Medicinal Plants and Vitamins. International Journal of Molecular Sciences, 24(10), 9085–9085. https://doi.org/10.3390/ijms24109085
[40]. Yokoyama, T., Date, C., Kokubo, Y., Yoshiike, N., Matsumura, Y., & Tanaka, H. (2000). Serum Vitamin C Concentration Was Inversely Associated With Subsequent 20-Year Incidence of Stroke in a Japanese Rural Community. Stroke, 31(10), 2287–2294. https://doi.org/10.1161/01.str.31.10.2287