1. Introduction
Depression is the second leading cause of disability worldwide and one of the most prevalent psychiatric disorders. According to the WHO report in 2023, symptoms of depression include persistent feelings of sadness, decreased interest, anhedonia, and suicide. While effective treatments for mental disorders are available, more than 75% of patients in low- and middle-income countries do not receive treatment. [1] At the same time, depression is a psychological disorder with a high suicide rate, because the treatment cycle of depression is long, so doctors cannot follow up for a long time, resulting in a huge consumption of financial and material resources to the patient's family, and a heavy burden on the patient's family, family and society. However, the lack of a complete treatment system for depression also leads to the fact that many people do not receive timely treatment for depression in the early stages of its onset. Therefore, prediction, timely diagnosis and treatment of depression are of great significance for the protection of life, health and safety. In recent years, the combination of medicine and multimodal algorithm has been considered as a promising field.
Depression, also known as depressive disorder, is a mental disorder with high morbidity, high clinical cure rate but low treatment acceptance rate and high recurrence rate. Because of these characteristics, the high incidence of depression in clinical treatment, especially among adolescents [1], will lead to increased pressure on medical resources and endanger the safety of public mental health, so it is extremely important to improve the prevention of the disease. Due to the extremely complex pathogenesis of depression, a lot of clinical experience is required to make decisions in the actual diagnosis process, which makes it difficult to diagnose depression, especially psychotic depression [2], and requires more accurate diagnosis to ensure follow-up treatment. In the treatment of depression, due to the long treatment cycle, medical resources are usually insufficient for psychotherapy, and drug and non-drug treatment are the mainstay, and there are differences in the effectiveness and tolerability of individual antidepressant drugs [3], and the current cutting-edge research also focuses on non-drug treatment. When the depressed state has been resolved or released, the prevention of the recurrence of depression is also a major research topic in clinical practice. Therefore, the current research mainly focuses on the following clinical problems: 1. The use of algorithms to predict depression to prevent depression and prevent recurrence after depression treatment ends. 2. Use algorithms to detection depression, including psychotic depressions and assist diagnosis. 3. Use medication and neuromodulation technology to resolve depression.
Electroencephalography (EEG) and functional magnetic magnetic resonance imaging (fMRI) are both commonly used data types in depression research, and there is a complementary relationship between the two. EEG is a research method that collects spontaneous biopotential amplification of the brain by collecting the spontaneous biopotential of the brain with sophisticated electronic instruments, so it is a large-scale data with strong time sensitivity and weak spatial sensitivity. Based on this characteristic, EEG is very suitable for the research of various machine learning and deep learning algorithms. For example, we can use the EEG-based dynamic functional connectivity(DFC)to conduct a classification study of depression, which Hui Chen et al successfully did in their study. [4] FMRI is a technique that can show small changes in the magnetic resonance signal caused by the oxygenation status of blood in the veins and capillaries in various regions of the brain. Nowadays, fMRI technology has developed rapidly, from 1.5T, 3T to the current 7T, which has significantly improved the spatial resolution, can accurately reflect the changes in the cerebral cortex and subcortex, and is suitable for studying the situation of reduced brain state changes for a long time. The functional brain network is a group of neural elements that display related activities, from cell populations to macroscopic brain regions, and is mainly divided into Sensorimotor System (SS), Central Executive Network (CEN), Default Mode Network (DMN), Salience Network (SN), Dorsal Attention Network (DAN), Limbic/Paralimbic System, Visual System (VS). Major depressive disorder (MDD) effects various large-scale functional networks in the brain, and it is considered as a disorder of distributed effects of aberrant interaction in the brain. Abnormalities in CEN, DMN, and SN lead to depression. Based on Bao-Juan Li's research, we can clearly understand the abnormal functional links of the brain network in depression and the direction of neuromodulation therapy, which confirms that the treatment of depression through neuromodulation is promising.[5] At the same time, existing studies have also given the prediction and treatment of depression symptoms through deep brain stimulation, and it has good results. [6][7][8]
In this work, focus on the current clinical issues, we will review the lasted researches to explore the finding and technologies in the field of prediction, detection and neuromodulation in depression, based on the neural signals, including EEG, fMRI and so on, as shown in Fig. 1.
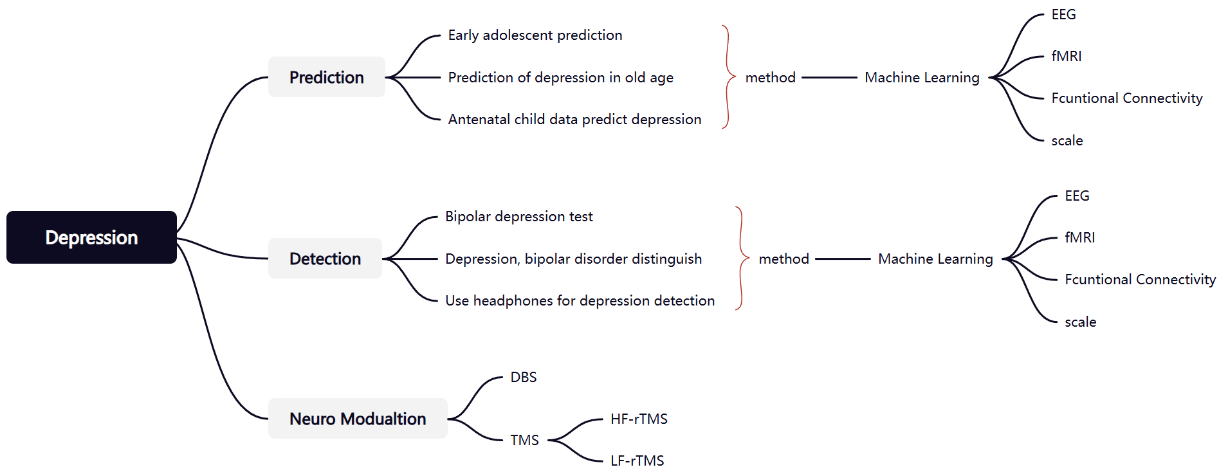
Figure 1: Overview of this review.
2. Prediction
Depression is particularly high in adolescence, which is easy to bring great pressure to patients, families, social and medical resource allocation, so it is of great clinical value to predict depression and achieve early prevention. For the research on the prediction of depression, the main direction and purpose of the research focuses on the early stage of the disease, we can predict the disease through EEG, fMRI or scale data to avoid the onset of the disease. Zhou, X et al. [9] used the Depression Rest dataset, which contains multimodal physical and psychometric data, and proposed a deep learning model with 95% accuracy. The authors used a hybrid CNN-LSTM network, which combines the advantages of convolutional neural network (CNN) and long short-term memory network, which is conducive to processing sequential and temporal data. The disadvantage of CNN is that it is difficult to accurately locate the object, so it will cause the lack of features, which will affect the prediction efficiency and results, which is also a specific problem that CNN is difficult to solve. To solve this problem of CNNs, Yun Su et al [10] used a 3D Multiscale Kernels CNN Model and achieve an accuracy rate of 99.86%. This method expands the one-dimensional features into a two-dimensional electrode matrix to construct the three-dimensional structure of EEG, which can mine the spatiotemporal information between the electrodes, make up for the problem of missing features of CNN, which has stronger performance than traditional CNN. At the same time, they used mental-disorder analysis (MODMA) datasets, which contributed to the early prediction of depression in older adults. Additionally, the number of electrodes required for EEG acquisition can be reduced in this way, which provides ideas for real-time collection of EEG data in the future. In the study of electroencephalograms, researchers have also focused on the functional connections of brain networks. N. Balakrishna et al [11] first used a hybrid machine learning algorithm to extract and compare functional connectivity (FC) and power spectral density (PSD) from EEGs in healthy patients as key features and supplementary information to identify and predict depression. This study demonstrates the potential of machine learning algorithms, reminds us that we should focus on the characteristics of brain networks to achieve stronger model performance, and points out that machine learning is highly robust and makes its clinical application more practical. Pallavi Kaushik et al [12] tried to draw a comparison between the efficacy of using task-based EEG data vs rs-EEG data for predicting the vulnerability to depression in individuals. At the same time, the authors found that for raw rs-EEG data, individuals more prone to depression have, on average, increased activity in the right temporal channel and decreased activity in the left frontal central and right occipital channels. This contributes to the direction of our focus for depression prediction through functional connectivity. When studying the functional connectivity of brain networks, we should not only pay attention to the changes in various regions of the brain network of patients with depression, but also pay attention to their dynamic changes, that is, dynamic functional connectivity. Hui Chen et al [4] proposed a machine learning algorithms based on network manifestations identify dynamic patterns within the spatiotemporal feature space that are specific to nonpsychotic major depression (NPMD), psychotic major depression (PMD), and schizophrenia (SCZ). This paper is different from most studies on deep learning prediction of depression based on EEG signals, focusing on DFC and achieving good results, which indicates that in the field of predicting depression, it is also possible to achieve better results by paying attention to FC while taking into account the spatial characteristics of EEG signals that are insensitive. Clinically, these three diseases often have similar symptoms, which leads to doctors needing more energy to help patients make more accurate diagnoses, so it is easy to cause misdiagnosis. On the basis of solving this problem, this study also inspires us to focus our research on similar diseases that are difficult to diagnose and treat in clinical practice. In addition, EEG and fMRI are two kinds of physiological signals, which can quickly obtain the patient's current disease state, compared to the scale is a clinical tool, although it cannot correspond to brain activity, but the scale can track the patient's disease course changes for a long time, and also contains more clinical medical significance. Priya, A. et al [13] used the Depression, Anxiety and Stress Scale questionnaire (DASS21) as a data source to provide a design idea for us to use data in the form of a scale for depression. At the same time, they proposed a hybrid machine learning algorithm, which put forward methods and improvement ideas for us to process scale data using machine learning. Furthermore, Yoo, A et al. [14] used machine learning to predict adolescent depression from prenatal and child data from the Avon Longitudinal Study of Parents and Children (ALSPAC) which are formal and rigorous scale data that has huge potential for researchers to study in the future. This work allows us to predict the risk of depression in advance early in life, and this study provides valuable ideas for depression, a disease with a high incidence in adolescents, and provides the development direction of early prediction tools for depression in the future.
3. Detection
Depression is a very common psychological disorder, which makes it difficult for patients to make a judgment about seeking medical attention through subjective observation of themselves. The detection of depression can be used for helping doctors to diagnose. For EEG signals, the randomness is strong, and the nonlinear research is limited to a certain extent, resulting in poor recognition results. Therefore, it is particularly important to pre-process and denoise the EEG signal. FM Alneqrat, et al [15] used discrete wavelet transform and Support Vector Machine (SVM), k-nearest neighbor classification (KNN) to detect and diagnose depression, a classical approach that not only achieved 99.51% accuracy, but also told us about the feasibility of these machine learning algorithms. On this basis, M. Shivcharan, K. Boby and V. Sridevi [16] added a notch filter and an independent component analysis module to the study, and extracted time-domain and frequency-domain features from EEG signals and selected meaningful features, which not only reminded us to pay attention to the accuracy of feature extraction in improving the accuracy of the model, but also provided a reference for the feature points that can be paid attention to in subsequent research. In addition to the classical methods mentioned above, there are different ways to process EEG data. Hadeer Mohammed and Mohammed Diykh [17] proposed an MDD intelligent detection model based on the combination of Fourier-Bessel series expansion (FBSE) and domain adaptive (DA), which is a new processing idea and achieves the best accuracy among machine learning algorithms. It provides ideas for the innovation of the subsequent model. In addition, Shor, O. et al [18] focused on the spatio-temporal relationship of EEG electrode signals, reminding us once again that we should pay more attention to the extraction and retention of spatial features when studying EEG signals. At the same time, the data set used by the author is a control for distinguishing schizophrenia and depression, reflecting that in the field of psychiatry, which is difficult to diagnose, it is not only necessary to pay attention to the distinction between healthy and sick, but also to include the distinction of similar conditions to reduce the possibility of misdiagnosis. Moreover, for EEG signals, the researchers focused not only on the signals themselves, but also on emotion recognition, especially for disorders such as depression, which is strongly related to emotion. Y. Anis et al[19] focused on EEG emotion recognition, combined with classical machine learning deep learning algorithms to provide examples for research, and proposed an adaptive method for diagnosing depression using EEG based on machine and deep learning, and achieved considerable results. Wu, C.-T et al [20] mentioned in the study that the ability to use resting state EEG features to distinguish adults with MDD from healthy individuals has reached a bottleneck. We extracted three types of relative EEG power signatures from different frequency bands (δ, θ, α, β, and γ) from healthy adults and patients during emotional tasks and resting states, contributing to our study of depression detection from functional connectivity, and they proposed a conucleate support vector machine (CK-SVM) algorithm. Contributed to the use of classifiers for depression detection. In real life, it is not practical for patients to go to the hospital frequently for EEG tests to monitor potential depression, so it is of great research value to find a convenient way to detect depression through EEG. K. Thulasi et al. [21] discussed to find a solution that enables the acquisition of EEG signals using commercially available headsets, apply machine learning algorithms for processing, and determine mild depression detection. M. Rehman et al [22] proposed a method of detecting mental depression by analyzing the EEG recorded by the Fp1、Fp2, and Fpz electrodes on the headphones, which highlights the need to pay attention to the human brain structure for precise depression detection and uses headphone electrodes for convenience, providing a demonstration for the popularization of EEG-based depression detection.
These existing studies give us some insights that we have developed mature signal processing technology for EEG and fMRI, and used machine learning to distinguish abnormal signals of patients with depression with excellent classification performance of data, carry out auxiliary diagnosis, and contribute to the clinical construction of a depression diagnosis and disease states. At the same time, the use of headphones to detect EEG signals to detect depression status is helpful for public health detection.
4. Neuromodulation
In the current treatment of depression, while antidepressants are effective, one-third to one-half of people with MDD do not respond to multiple antidepressants, or more antidepressants may only achieve a partial response. Therefore, there is a need to develop, test, and understand the effectiveness of new drugs or treatment modalities that, ideally, have a faster onset of action, are better tolerated, and have greater potential for effectiveness than existing antidepressants. [23] This dilemma was turned around with research on the brain computer interface (BCI). At present, the technology is mainly divided into two categories: invasive and non-invasive technologies, including deep brain stimulation (DBS) and transcranial magnetic stimulation (TMS). Zhang C et al. [24] used DBS to treat patients with TRD, and tried multiple therapeutic targets for comparison, which provided valuable insights for the improvement direction of subsequent treatment of DBS, among which it can be seen that subcallosal cingulate gyrus (SCG) and medial forebrain tract (MFB) used as the stimulation targets can achieve better treatment effects without obvious side effects. Fenoy AJ et al. [25] focused on the efficacy of MFB, and the effect was outstanding, especially within 5 minutes of the start of treatment, and it also had a good effect within one week, suggesting that MFB can be used as a key DBS target in the treatment of depression. Cha, J. et al. [26] also showed a significant short-term efficacy of DBS in the treatment of patients with TRD, and pointed out that SCC-DBS has significant time-specific effects in the saliency network (SN) and default mode network (DMN), which reminds us that functional brain network analysis might improve the decision of treatment modalities and targets. For DBS, although the clinical treatment are effective and promising, after all, it is an invasive treatment, and many patients are unwilling or do not have the medical conditions to support this treatment, in which case non-invasive has become a more ideal treatment. Recently, non-invasive treatment studies have also shown some positive results. Abdullah Bolu et al. [27] used high-frequency TMS to stimulate left dorsolateral prefrontal cortex (DLPFC) and 26.1% were evaluated as remission and 29.2% as partial remission. George, Mark S. et al. [28] used the same stimulus target through high frequency repetitive TMS (HF-rTMS) but increased the frequency of stimulation, Of the six subjects, two showed strong mood improvement, and one had complete remission of depressive symptoms for the first time in 3 years. However, at the same time, the research team also found that HF-rTMS may be uncomfortable at higher intensities [29] and is also associated with an increased risk of adverse effects [30], Klein et al. [31] was treated with TMS at 1 Hz, which was well tolerated, with no serious adverse effects reported in any patients, and 17 of 35 patients had a >50% improvement in depression scores. In summary, more attempts are needed to increase the effect of the treatment in the study of LF-rTMS, and a more appropriate frequency of HF-rTMS needs to be found to reduce the discomfort felt by patients during treatment.
5. Conclusion
Depression is a well-known disease with a large number of patients, but it lacks a complete prevention-diagnosis-treatment system, resulting in many patients missing the opportunity to intervene early to alleviate the condition or being misdiagnosed at the time of diagnosis. The powerful performance of machine learning technology in prediction and classification has made significant advances in the prediction and auxiliary diagnosis of depression, providing higher diagnostic accuracy and efficiency for the detection of depression during healthy periods and depression that is easily misdiagnosed, such as bipolar depression. In the future, we should pay more attention to the analysis of brain network functional connectivity to improve the performance and accuracy of machine learning models. DBS and TMS technologies provide treatment options for patients who do not respond well or do not respond to depression medication at present, and in the future, we can try more therapeutic targets or try to find ways to balance the patient's feelings and treatment effects on promising targets.
References
[1]. Evans-Lacko S, Aguilar-Gaxiola S, Al-Hamzawi A, et al. Socio-economic variations in the mental health treatment gap for people with anxiety, mood, and substance use disorders: results from the WHO World Mental Health (WMH) surveys. Psychol Med. 2018;48(9):1560-1571.
[2]. Dubovsky SL, Ghosh BM, Serotte JC, Cranwell V. Psychotic Depression: Diagnosis, Differential Diagnosis, and Treatment. Psychother Psychosom. 2021;90(3):160-177. doi: 10.1159/000511348. Epub 2020 Nov 9. PMID: 33166960.
[3]. Cipriani, A. et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis. The Lancet, Volume 391, Issue 10128, 1357 - 1366
[4]. Chen, H., Lei, Y., Li, R. et al. Resting-state EEG dynamic functional connectivity distinguishes non-psychotic major depression, psychotic major depression and schizophrenia. Mol Psychiatry 29, 1088–1098 (2024). https://doi.org/10.1038/s41380-023-02395-3
[5]. Bao-Juan L., Karl F., Maria M. et al. (2018) A brain network model for depression: From symptom understanding to disease intervention”.https://doi.org/10.1111/cns.12998
[6]. Lynch, C.J., Elbau, I.G., Ng, T. et al. Frontostriatal salience network expansion in individuals in depression. Nature 633, 624–633 (2024). https://doi.org/10.1038/s41586-024-07805-2
[7]. Alagapan, S., Choi, K.S., Heisig, S. et al. Cingulate dynamics track depression recovery with deep brain stimulation. Nature 622, 130–138 (2023). https://doi.org/10.1038/s41586-023-06541-3
[8]. Wang, Z., Jiang, C., Guan, L. et al. Deep brain stimulation of habenula reduces depressive symptoms and modulates brain activities in treatment-resistant depression. Nat. Mental Health 2, 1045–1052 (2024). https://doi.org/10.1038/s44220-024-00286-2
[9]. Zhou, X., Wang, X., Liu, W., & Wang, Z. (2023). Classification Model of Depression Based on the CNN-LSTM Network. Proceedings - 2023 3rd International Conference on Frontiers of Electronics, Information and Computation Technologies, ICFEICT 2023, 210–214. https://doi.org/10.1109/ICFEICT59519.2023.00044
[10]. Yun S., Zhixuan Z., Qi C., Bingtao Z., Xiaohong L.. 3DMKDR: 3D Multiscale Kernels CNN Model for Depression Recognition Based on EEG. 2023. Journal of Beijing Institute of Technology, Vol. 32,No. 2.
[11]. N. Balakrishna, M. B. Mukesh Krishnan and D. Ganesh, Hybrid Machine Learning Approaches for Predicting and Diagnosing Major Depressive Disorder International Journal of Advanced Computer Science and Applications (IJACSA), 15(3), 2024. http://dx.doi.org/10.14569/IJACSA.2024.0150363
[12]. Kaushik, P., Yang, H., Roy, P.P. et al. Comparing resting state and task-based EEG using machine learning to predict vulnerability to depression in a non-clinical population. Sci Rep 13, 7467 (2023). https://doi.org/10.1038/s41598-023-34298-2
[13]. Anu P., Shruti G., Neha Prerna T. Predicting Anxiety, Depression and Stress in Modern Life using Machine Learning Algorithms. Procedia Computer Science, Volume 167, 2020, Pages 1258-1267, ISSN 1877-0509, https://doi.org/10.1016/j.procs.2020.03.442.
[14]. Yoo, A., Li, F., Youn, J. et al. Prediction of adolescent depression from prenatal and childhood data from ALSPAC using machine learning. Sci Rep 14, 23282 (2024). https://doi.org/10.1038/s41598-024-72158-9
[15]. F. M. Alneqrat, A. H. Maamar, A. N. Mohammed and H. A. Aghnaya, Depression Detection Based on Eeg Signals Using Machine Learning Algorithms, 2024 IEEE 4th International Maghreb Meeting of the Conference on Sciences and Techniques of Automatic Control and Computer Engineering (MI-STA), Tripoli, Libya, 2024, pp. 625-630, doi: 10.1109/MI-STA61267.2024.10599680.
[16]. M. Shivcharan, K. Boby and V. Sridevi, EEG Based Machine Learning Models for Automated Depression Detection, 2023 IEEE International Conference on Electronics, Computing and Communication Technologies (CONECCT), Bangalore, India, 2023, pp. 1-6, doi: 10.1109/CONECCT57959.2023.10234686.
[17]. Hadeer M., Mohammed D., Improving EEG major depression disorder classification using FBSE coupled with domain adaptation method based machine learning algorithms, Biomedical Signal Processing and Control, Volume 85, 2023, 104923, ISSN 1746-8094, https://doi.org/10.1016/j.bspc.2023.104923.
[18]. Shor, O., Yaniv-Rosenfeld, A., Valevski, A. et al. EEG-based spatio-temporal relation signatures for the diagnosis of depression and schizophrenia. Sci Rep 13, 776 (2023). https://doi.org/10.1038/s41598-023-28009-0
[19]. Y. Anis, K. Singh and A. Saxena, An Efficient Machine and Deep Learning Classfication Technique for Depression Using EEG, 2023 3rd International Conference on Technological Advancements in Computational Sciences (ICTACS), Tashkent, Uzbekistan, 2023, pp. 404-408, doi: 10.1109/ICTACS59847.2023.10390520.
[20]. Wu, C.-T.; Dillon, D.G.; Hsu, H.-C.; Huang, S.; Barrick, E.; Liu, Y.-H. Depression Detection Using Relative EEG Power Induced by Emotionally Positive Images and a Conformal Kernel Support Vector Machine. Appl. Sci. 2018, 8, 1244. https://doi.org/10.3390/app8081244
[21]. K. Thulasi et al., Detecting Mild Depression from EEG Signal in a Non-Clinical Environment Using Machine Learning Technique, 2023 IEEE 2nd National Biomedical Engineering Conference (NBEC), Melaka, Malaysia, 2023, pp. 100-105, doi: 10.1109/NBEC58134.2023.10352586.
[22]. M. Rehman, S. M. Umar Saeed, S. Khan, S. H. Noorani and U. Rauf, EEG-Based Depression Detection: A Temporal Domain Feature-Centric Machine Learning Approach, 2023 International Conference on Frontiers of Information Technology (FIT), Islamabad, Pakistan, 2023, pp. 208-213, doi: 10.1109/FIT60620.2023.00046.
[23]. Marwaha S, Palmer E, Suppes T, Cons E, Young AH, Upthegrove R. Novel and emerging treatments for major depression. Lancet. 2023 Jan 14;401(10371):141-153. doi: 10.1016/S0140-6736(22)02080-3. Epub 2022 Dec 16. PMID: 36535295.
[24]. Zhang C, Zhang Y, Luo H, Xu X, Yuan TF, Li D, Cai YY, Gong H, Peng DH, Fang YR, Voon V, Sun B. Bilateral Habenula deep brain stimulation for treatment-resistant depression: clinical findings and electrophysiological features. Transl Psychiatry. 2022 Feb 3;12(1):52. doi: 10.1038/s41398-022-01818-z. PMID: 35115488; PMCID: PMC8813927.
[25]. Fenoy AJ, Schulz PE, Selvaraj S, Burrows CL, Zunta-Soares G, Durkin K, Zanotti-Fregonara P, Quevedo J, Soares JC. A longitudinal study on deep brain stimulation of the medial forebrain bundle for treatment-resistant depression. Transl Psychiatry. 2018 Jun 4;8(1):111. doi: 10.1038/s41398-018-0160-4. PMID: 29867109; PMCID: PMC5986795.
[26]. Cha, J., Choi, K.S., Rajendra, J.K. et al. Whole brain network effects of subcallosal cingulate deep brain stimulation for treatment-resistant depression. Mol Psychiatry 29, 112–120 (2024). https://doi.org/10.1038/s41380-023-02306-6
[27]. Abdullah B., İbrahim G., Mehmet S. A., Duygu F., Yasemin E., Özcan U., Ten years' data of Transcranial Magnetic Stimulation (TMS): A naturalistic, observational study outcome in clinical practice, Psychiatry Research, Volume 301, 2021, 113986, ISSN 0165-1781, https://doi.org/10.1016/j.psychres.2021.113986.
[28]. George, Mark S.; Wassermann, Eric M.; Williams, Wendol A.; Callahan, Ann1; Ketter, Terence A.; Basser, Peter; Hallett, Mark; Post, Robert M. Daily repetitive transcranial magnetic stimulation (rTMS) improves mood in depression. NeuroReport 6(14):p 1853-1856, October 2, 1995.
[29]. Janicak PG, O'Reardon JP, Sampson SM, Husain MM, Lisanby SH, Rado JT et al (2008). Transcranial magnetic stimulation in the treatment of major depressive disorder: a comprehensive summary of safety experience from acute exposure, extended exposure, and during reintroduction treatment. J Clin Psychiatry 69: 222–232.
[30]. Loo CK, McFarquhar TF, Mitchell PB (2008). A review of the safety of repetitive transcranial magnetic stimulation as a clinical treatment for depression. Int J Neuropsychopharmacol 11: 131–147.
[31]. Klein E, Kreinin I, Chistyakov A, et al. Therapeutic Efficacy of Right Prefrontal Slow Repetitive Transcranial Magnetic Stimulation in Major Depression: A Double-blind Controlled Study. Arch Gen Psychiatry. 1999;56(4):315–320. doi:10.1001/archpsyc.56.4.315
Cite this article
Bai,C. (2025). Prediction, Diagnosis and Treatment of Depression in Recent Ten Years. Theoretical and Natural Science,89,64-70.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 3rd International Conference on Modern Medicine and Global Health
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Evans-Lacko S, Aguilar-Gaxiola S, Al-Hamzawi A, et al. Socio-economic variations in the mental health treatment gap for people with anxiety, mood, and substance use disorders: results from the WHO World Mental Health (WMH) surveys. Psychol Med. 2018;48(9):1560-1571.
[2]. Dubovsky SL, Ghosh BM, Serotte JC, Cranwell V. Psychotic Depression: Diagnosis, Differential Diagnosis, and Treatment. Psychother Psychosom. 2021;90(3):160-177. doi: 10.1159/000511348. Epub 2020 Nov 9. PMID: 33166960.
[3]. Cipriani, A. et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis. The Lancet, Volume 391, Issue 10128, 1357 - 1366
[4]. Chen, H., Lei, Y., Li, R. et al. Resting-state EEG dynamic functional connectivity distinguishes non-psychotic major depression, psychotic major depression and schizophrenia. Mol Psychiatry 29, 1088–1098 (2024). https://doi.org/10.1038/s41380-023-02395-3
[5]. Bao-Juan L., Karl F., Maria M. et al. (2018) A brain network model for depression: From symptom understanding to disease intervention”.https://doi.org/10.1111/cns.12998
[6]. Lynch, C.J., Elbau, I.G., Ng, T. et al. Frontostriatal salience network expansion in individuals in depression. Nature 633, 624–633 (2024). https://doi.org/10.1038/s41586-024-07805-2
[7]. Alagapan, S., Choi, K.S., Heisig, S. et al. Cingulate dynamics track depression recovery with deep brain stimulation. Nature 622, 130–138 (2023). https://doi.org/10.1038/s41586-023-06541-3
[8]. Wang, Z., Jiang, C., Guan, L. et al. Deep brain stimulation of habenula reduces depressive symptoms and modulates brain activities in treatment-resistant depression. Nat. Mental Health 2, 1045–1052 (2024). https://doi.org/10.1038/s44220-024-00286-2
[9]. Zhou, X., Wang, X., Liu, W., & Wang, Z. (2023). Classification Model of Depression Based on the CNN-LSTM Network. Proceedings - 2023 3rd International Conference on Frontiers of Electronics, Information and Computation Technologies, ICFEICT 2023, 210–214. https://doi.org/10.1109/ICFEICT59519.2023.00044
[10]. Yun S., Zhixuan Z., Qi C., Bingtao Z., Xiaohong L.. 3DMKDR: 3D Multiscale Kernels CNN Model for Depression Recognition Based on EEG. 2023. Journal of Beijing Institute of Technology, Vol. 32,No. 2.
[11]. N. Balakrishna, M. B. Mukesh Krishnan and D. Ganesh, Hybrid Machine Learning Approaches for Predicting and Diagnosing Major Depressive Disorder International Journal of Advanced Computer Science and Applications (IJACSA), 15(3), 2024. http://dx.doi.org/10.14569/IJACSA.2024.0150363
[12]. Kaushik, P., Yang, H., Roy, P.P. et al. Comparing resting state and task-based EEG using machine learning to predict vulnerability to depression in a non-clinical population. Sci Rep 13, 7467 (2023). https://doi.org/10.1038/s41598-023-34298-2
[13]. Anu P., Shruti G., Neha Prerna T. Predicting Anxiety, Depression and Stress in Modern Life using Machine Learning Algorithms. Procedia Computer Science, Volume 167, 2020, Pages 1258-1267, ISSN 1877-0509, https://doi.org/10.1016/j.procs.2020.03.442.
[14]. Yoo, A., Li, F., Youn, J. et al. Prediction of adolescent depression from prenatal and childhood data from ALSPAC using machine learning. Sci Rep 14, 23282 (2024). https://doi.org/10.1038/s41598-024-72158-9
[15]. F. M. Alneqrat, A. H. Maamar, A. N. Mohammed and H. A. Aghnaya, Depression Detection Based on Eeg Signals Using Machine Learning Algorithms, 2024 IEEE 4th International Maghreb Meeting of the Conference on Sciences and Techniques of Automatic Control and Computer Engineering (MI-STA), Tripoli, Libya, 2024, pp. 625-630, doi: 10.1109/MI-STA61267.2024.10599680.
[16]. M. Shivcharan, K. Boby and V. Sridevi, EEG Based Machine Learning Models for Automated Depression Detection, 2023 IEEE International Conference on Electronics, Computing and Communication Technologies (CONECCT), Bangalore, India, 2023, pp. 1-6, doi: 10.1109/CONECCT57959.2023.10234686.
[17]. Hadeer M., Mohammed D., Improving EEG major depression disorder classification using FBSE coupled with domain adaptation method based machine learning algorithms, Biomedical Signal Processing and Control, Volume 85, 2023, 104923, ISSN 1746-8094, https://doi.org/10.1016/j.bspc.2023.104923.
[18]. Shor, O., Yaniv-Rosenfeld, A., Valevski, A. et al. EEG-based spatio-temporal relation signatures for the diagnosis of depression and schizophrenia. Sci Rep 13, 776 (2023). https://doi.org/10.1038/s41598-023-28009-0
[19]. Y. Anis, K. Singh and A. Saxena, An Efficient Machine and Deep Learning Classfication Technique for Depression Using EEG, 2023 3rd International Conference on Technological Advancements in Computational Sciences (ICTACS), Tashkent, Uzbekistan, 2023, pp. 404-408, doi: 10.1109/ICTACS59847.2023.10390520.
[20]. Wu, C.-T.; Dillon, D.G.; Hsu, H.-C.; Huang, S.; Barrick, E.; Liu, Y.-H. Depression Detection Using Relative EEG Power Induced by Emotionally Positive Images and a Conformal Kernel Support Vector Machine. Appl. Sci. 2018, 8, 1244. https://doi.org/10.3390/app8081244
[21]. K. Thulasi et al., Detecting Mild Depression from EEG Signal in a Non-Clinical Environment Using Machine Learning Technique, 2023 IEEE 2nd National Biomedical Engineering Conference (NBEC), Melaka, Malaysia, 2023, pp. 100-105, doi: 10.1109/NBEC58134.2023.10352586.
[22]. M. Rehman, S. M. Umar Saeed, S. Khan, S. H. Noorani and U. Rauf, EEG-Based Depression Detection: A Temporal Domain Feature-Centric Machine Learning Approach, 2023 International Conference on Frontiers of Information Technology (FIT), Islamabad, Pakistan, 2023, pp. 208-213, doi: 10.1109/FIT60620.2023.00046.
[23]. Marwaha S, Palmer E, Suppes T, Cons E, Young AH, Upthegrove R. Novel and emerging treatments for major depression. Lancet. 2023 Jan 14;401(10371):141-153. doi: 10.1016/S0140-6736(22)02080-3. Epub 2022 Dec 16. PMID: 36535295.
[24]. Zhang C, Zhang Y, Luo H, Xu X, Yuan TF, Li D, Cai YY, Gong H, Peng DH, Fang YR, Voon V, Sun B. Bilateral Habenula deep brain stimulation for treatment-resistant depression: clinical findings and electrophysiological features. Transl Psychiatry. 2022 Feb 3;12(1):52. doi: 10.1038/s41398-022-01818-z. PMID: 35115488; PMCID: PMC8813927.
[25]. Fenoy AJ, Schulz PE, Selvaraj S, Burrows CL, Zunta-Soares G, Durkin K, Zanotti-Fregonara P, Quevedo J, Soares JC. A longitudinal study on deep brain stimulation of the medial forebrain bundle for treatment-resistant depression. Transl Psychiatry. 2018 Jun 4;8(1):111. doi: 10.1038/s41398-018-0160-4. PMID: 29867109; PMCID: PMC5986795.
[26]. Cha, J., Choi, K.S., Rajendra, J.K. et al. Whole brain network effects of subcallosal cingulate deep brain stimulation for treatment-resistant depression. Mol Psychiatry 29, 112–120 (2024). https://doi.org/10.1038/s41380-023-02306-6
[27]. Abdullah B., İbrahim G., Mehmet S. A., Duygu F., Yasemin E., Özcan U., Ten years' data of Transcranial Magnetic Stimulation (TMS): A naturalistic, observational study outcome in clinical practice, Psychiatry Research, Volume 301, 2021, 113986, ISSN 0165-1781, https://doi.org/10.1016/j.psychres.2021.113986.
[28]. George, Mark S.; Wassermann, Eric M.; Williams, Wendol A.; Callahan, Ann1; Ketter, Terence A.; Basser, Peter; Hallett, Mark; Post, Robert M. Daily repetitive transcranial magnetic stimulation (rTMS) improves mood in depression. NeuroReport 6(14):p 1853-1856, October 2, 1995.
[29]. Janicak PG, O'Reardon JP, Sampson SM, Husain MM, Lisanby SH, Rado JT et al (2008). Transcranial magnetic stimulation in the treatment of major depressive disorder: a comprehensive summary of safety experience from acute exposure, extended exposure, and during reintroduction treatment. J Clin Psychiatry 69: 222–232.
[30]. Loo CK, McFarquhar TF, Mitchell PB (2008). A review of the safety of repetitive transcranial magnetic stimulation as a clinical treatment for depression. Int J Neuropsychopharmacol 11: 131–147.
[31]. Klein E, Kreinin I, Chistyakov A, et al. Therapeutic Efficacy of Right Prefrontal Slow Repetitive Transcranial Magnetic Stimulation in Major Depression: A Double-blind Controlled Study. Arch Gen Psychiatry. 1999;56(4):315–320. doi:10.1001/archpsyc.56.4.315