1. Introduction
Terahertz (0.1-10 THz) imaging is a potent answer to the increasing need for advanced imaging tools. THz imaging is comprehensively noninvasive and sensitive compared to traditional imaging tools such as X-ray, CT, and MRI. With its low photon energy (0.4 to 41 meV) [1], THz is unable to ionize the atoms or damage the DNA, making it suitable for in vivo detection. THz can detect the subtle difference of polar molecules. From a biomedical perspective, THz highlights the deviance of water content in body tissues [2], which is used to distinguish abnormal parts like cancerous cells. Although the limited penetration depth of in vivo tissues limits the diagnostic precision, enhancements such as nanoparticles and hybrid detection [3] could improve the range and specificity of detection.
This paper aims to find the application of terahertz imaging and its limitations. The imaging method has disadvantages of high response to disturbance, low resolution, slow acquisition speed, small sample size, and lack of standardization. This paper helps reveal the current advantages of terahertz imaging and its future target. If the use of terahertz imaging in clinical practice is popularized, it would gain more experimental data and doctors’ attention to improve this technology in the future.
2. Principle
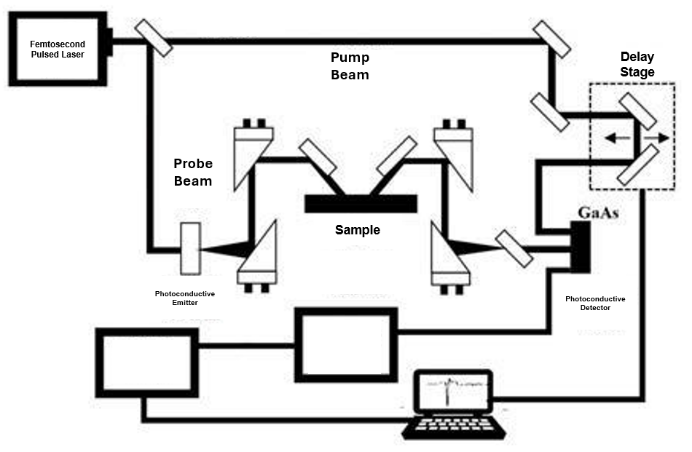
Figure 1: Pulsed wave THz imaging system using photoconductive antennas in a reflection-based geometry
THz imaging has two detection systems: the continuous wave system (CW) and the terahertz pulsed imaging system (TPI). CW maintains certain (one to several) frequencies and analyzes the difference in absorption between healthy and cancerous cells, while TPI detects the boundaries between tissues through transmission or reflection of the surface and the change of the pulse (delay, amplitude, and phase). Both act as the base of the THz imaging. Figure 1 indicates the pulsed wave THz imaging system, which is more widespread in experiments for its high spatial resolution [3]. For clinical applications, continuous wave THz has more potential. Their performance advantages are mentioned in Table 1 [3].
Table 1: Comparison of terahertz imaging technology performance
Performance | Pulse wave THz imaging system | Continuous wave THz imaging system |
Penetration depth | Relatively weak | Relatively strong |
Spatial resolution | Higher, up to about 1.0mm | Limited, approximately 2.5mm-2.6mm |
Acquisition speed | Slower | Faster and capable of real-time imaging |
THz imaging detects the motion (vibration, rotation, oscillation) of molecules and hydrogen bonds. The longer the wavelength, the less scattering and noise [4]. The higher the frequency of THz bandwidth, the clearer the molecular interstices of DNA and proteins [5]. THz imaging is perfect balance. Water molecules, which are abundant in bio tissues, absorb the THz radiation drastically, causing both its high sensitivity and limited penetration.
As most cancer starts on soft surfaces in the body, they have loose structures, higher water content, and more united vibrational properties(~1.65THz) than normal tissues [6]. These properties distinguish the health cells from the cancerous cells, acting as a biomarker of cancer. The penetration depth fluctuates from microns to millimeters, depending on the percentage of fat, water, and proteins [7].
3. Application
3.1. Breast cancer (invasive ductal carcinoma, IDC)
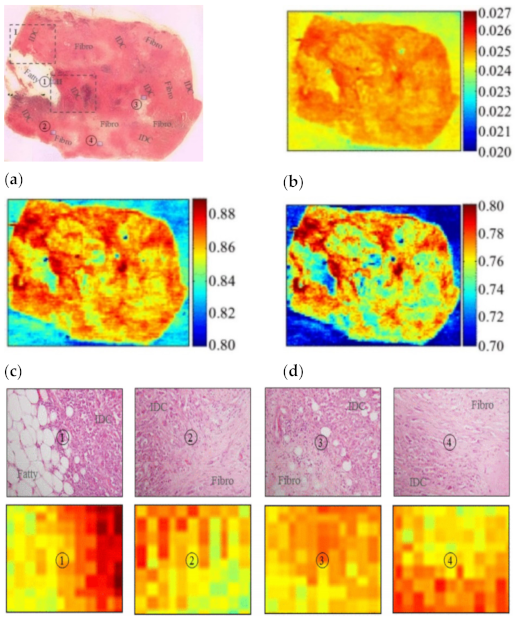 For breast cancer, operations are required to remove the cancerous tissue with high precision to ensure safety and preserve healthy tissues. THz are used to identify the magnitude and frame of the tumor area with different refractive indices, and it is clear enough to distinguish the fat, fibrosis, and cancer in the breast [8]. Figure 2 shows different transition areas of a sample between normal breast cells and cancerous cells. The breast cancer is named triple-negative invasive ductal carcinoma, labeled IDC. There is consistency between the upper images (ex vivo) labeled IDC and the lower images (in vivo) that are orange to dark red. This THz imaging can successfully distinguish normal breast tissue from cancerous tissue.
For breast cancer, operations are required to remove the cancerous tissue with high precision to ensure safety and preserve healthy tissues. THz are used to identify the magnitude and frame of the tumor area with different refractive indices, and it is clear enough to distinguish the fat, fibrosis, and cancer in the breast [8]. Figure 2 shows different transition areas of a sample between normal breast cells and cancerous cells. The breast cancer is named triple-negative invasive ductal carcinoma, labeled IDC. There is consistency between the upper images (ex vivo) labeled IDC and the lower images (in vivo) that are orange to dark red. This THz imaging can successfully distinguish normal breast tissue from cancerous tissue.
Figure 2: The THz reflection imaging of different parts of a sample with triple-negative invasive ductal carcinoma (IDC), a type of breast cancer. Upper ①: The transition areas between IDC and normal tissues (Fatty); Upper ②, ③, ④: The transition areas between IDC and normal tissues (Fibro); Lower①, ②, ③, ④: THz reflection images of the sample parts above
3.2. Epidermoid carcinoma
For epidermoid carcinoma, gold nanorods are used in THz imaging. The specificity of THz imaging is raised by the difference in heat. The near-infrared laser (NIR) emits electromagnetic waves, penetrating through the target area. Gold nanorods block the waves and absorb the radiated energy to raise the temperature. Gold nanorods are distributed linearly with the water content, while cancerous tissues contain higher percentages of water. Thus, the temperature of cancerous tissues is higher than normal tissues under THz imaging. A minute change in temperature is enough to intensify THz signals, which improves the comparison and clarifies the THz imaging [9].
3.3. Gastric cancer
For gastric cancer, Gadolinium Oxide Nanoparticles (GONPs) improve diagnosis by targeting the cancer cells with antigens and antibodies. Gadolinium absorbs electromagnetic waves up to 3 times more than water molecules. GONPs delay pulses in phase and decrease the peak intensity [10]. These traits exemplify the distinction between gastric cancer with the presence of GONPs and normal tissue, which resolves the tumor margins in THz imaging.
3.4. Diabetes
For diabetes using ex vivo method, THz effectively analyzes the gas content from the dried blood and kidney samples [11]. For in vivo application, THz noninvasively detects the skin structure, subsurface blood flow, and the glucose concentration with 95% accuracy [12].
3.5. Skin cancer (melanoma)
3.5.1. Freezing method
Researchers can freeze the tissue to improve the quality of THz detection for skin cancer, especially melanoma. The change in states increases the depth of penetration in THz, as ice is more permeable compared to water. The contrast between melanoma and non-melanoma skin cells is also increased, in the density of cells and percentage of water content, in refractive index and absorption coefficient. This helps increase the sensitivity and precision of early melanoma diagnosis [13].
3.5.2. Methylation method
Methylation can also be used for improving THz detection quality of melanoma, which is a competitive and noninvasive method. The methylation causes water molecules to reorganize around the methyl groups, changing the rigidity and the shell dynamics of hydration. Hypermethylation patterns were detected under THz spectroscopy for the methylated DNA from melanoma cells. These amplify the contrast of the THz signal between methylated melanoma tissues and methylated normal tissues. The differentiation between methylated and non-methylated DNA regions has more than 90% accuracy. It bypasses the penetration limits mentioned above and aids the surgeries that excise the melanoma [14].
4. Challenges and future directions
4.1. Tradeoffs of overall THz imaging quality
THz imaging faces many challenges that prevent it from biomedical applications. First, for every extra requirement in resolution, there is an increase in destabilization. These two limitations restrict the overall imaging quality in biomedical practice.
4.1.1. Destabilization
One of the main challenges of THz imaging is the high response to disturbance. Not only does the previously mentioned limited penetration depth contribute to destabilization, but the THz radiation also has significant absorption and scattering in biological tissues, causing high signal loss and reduced image quality. The existence of water vapor absorption in the THz spectrum decreases the quality of the signal, and a small fluctuation in temperature offers a magnificent change in the imaging result [15].
4.1.2. Low resolution
The other challenge is low resolution. The signal attenuation hinders clinical diagnosis applications [16]. The latest studies exceed the traditional diffraction limits of THz and have achieved sub-wavelength resolution (~40 nm), but it is still hindered by a high ratio of signal to noise in water-abundant tissues [17].
4.2. Low acquisition speed
The acquisition speed of THz imaging is relatively slow compared to traditional imaging techniques such as CT and MRI. The imaging system depends on the mechanical delay lines with pulsed imaging, resulting in around 10 seconds per image [16]. For improved ratio of signal to noise by averaging multiple scans, the acquisition speed is as low as 30 seconds for more advanced images [18]. It makes THz imaging hard to detect dynamic tissues, such as tissues with blood flow. This limits its use in real-time imaging applications and makes it challenging to present dynamic processes in biological tissues.
4.3. Lack of enough experimental data
The main challenges that block the THz application of clinical diagnosis are the lack of comparable experimental data. It can be seen through the small sample size and the lack of standardization of THz imaging.
Many THz studies are cutting-edge and experimental, rely more on ex vivo and animal tissues, and are thus limited in sample size. Therefore, the findings may not generalize to in vivo experiments and broader populations. 72% of THz studies use fewer than 30 patient samples, while most MRIs have more than 100 participants (90% of MRI studies of breast cancer had more than 500 participants) [19].
The lack of standardization also hinders application. There are 14 proprietary software tools in 62 studies of THz imaging. These tools have disparate data formats, which create barriers to resampling validation and clinical applications [20].
4.4. Future directions
Despite these challenges, THz imaging is promising for biomedical applications. Advances in THz technology, such as detection with metallic tips. single-pixel cameras and hybrid systems [18], have the potential to improve the acquisition speed and enable real-time imaging. Integrating THz imaging with other imaging methods can offer a more comprehensive view of biological tissues. Further research in nanoparticles and near THz waves is also essential for balancing between sensitivity and robustness, improving THz imaging technology, and expanding its applications in biomedicine.
5. Conclusion
Terahertz imaging is a rapidly evolving technology with great potential for biomedical applications. Its unique advantages, being sensitive and non-invasive, make it suitable for its medical applications, especially in cancer detection. Although there are still some limitations to overcome, including high response to disturbance, low resolution, slow acquisition speed, small sample size, and the lack of standardization, recent advances in terahertz technology show great promise in addressing these challenges.
The future of terahertz imaging lies in the continued development of new sources, detectors, and imaging technologies, as well as the future popularized clinical practice. The standardization of terahertz imaging technology is also crucial for its wide application in clinical practice. With further research and development, terahertz imaging has the potential to become an important tool for biomedical diagnosis and treatment, improving patient outcomes and quality of life.
References
[1]. Yang, X., Zhao, X., et al. (2016). Biomedical applications of terahertz spectroscopy and imaging. Trends Biotechnol. 34, 810–824. doi:10.1016/j.tibtech.2016.04.008
[2]. Z. Yan, L.G. Zhu, et al, THz medical imaging: from in vitro to in vivo, Trends Biotechnol. (2022).
[3]. Gezimati, Mavis, and Ghanshyam Singh. "Advances in Terahertz Technology for Cancer Detection Applications." Optical and Quantum Electronics, vol. 55, no. 151, 2023. Springer, doi:10.1007/s11082-022-04340-0.
[4]. Mittleman DM, Jacobsen RH, et al. T-ray imaging. IEEE J Sel Top Quantum Electron. 1996;2(3):679-92. doi:10.1109/2944.571768
[5]. Brucher Seifer M, Nagel M, et al. Label-free probing of the binding state of DNA by time-domain terahertz sensing. Appl Phys Lett.2000;77(24):4049-51. doi: 10.1063/1.1332415.
[6]. Cheon H, Yang HJ, et al. Terahertz molecular resonance of cancer DNA. Sci Rep. 2016;6:37103. doi: 10.1038/srep37103.
[7]. Fitzgerald A, Pickwell E, et al. Medical applications of broadband terahertz pulsed radiation. In: 2005 IEEE LEOS Annual Meeting Conference Proceedings. Sydney, NSW: IEEE; 2005. p. 120-1. doi: 10.1109/leos.2005.1547899.
[8]. Bowman, T.C.; El-Shenawee, M.; Campbell, L.K. Terahertz imaging of excised breast tumor tissue on paraffin sections. IEEE Trans. Antennas Propag. 2015, 63, 2088–2097.
[9]. S.J. Oh, J. Choi, et al., Molecular imaging with terahertz waves, Opt. Express 19 (5) (2011) 4009–4016.
[10]. D.K. Lee, H. Kim, et al. Characteristics of gadolinium oxide nanoparticles as contrast agents for terahertz imaging, J. Infrared Millim. Terahertz Waves 32 (4) (2011) 506–512.
[11]. Lykina AA, Anfertev VA, et al. Terahertz high-resolution spectroscopy of thermal decomposition gas products of diabetic and non-diabetic blood plasma and kidney tissue pellets. J Biomed Opt. 2021;26(4):043008. doi: 10.1117/1.jbo.26.4.043008. 61. Kulya MS, Odlyanits
[12]. Mittleman, D. M., et al. (1996). "Terahertz imaging." *IEEE Transactions on Microwave Theory and Techniques*, 44(12), 2249-2256.
[13]. Sim, Y.C., Ahn, K.M., Park, J.Y., Park, C.S., Son, J.H.: Temperature-dependent terahertz imaging of excised oral malignant melanoma. IEEE Transact. Terahertz Sci. Technol. 3(4), 368–373 (2013)
[14]. Cheon, H., Yang, H.J., Lee, S.H., Kim, Y.A., Son, J.H. Terahertz molecular resonance of cancer DNA methylation. Sci. Rep. 2019, 9, 13832. doi:10.1038/s41598-019-50256-3.
[15]. Mittleman, D. M., et al. (1996). "Terahertz imaging." *IEEE Transactions on Microwave Theory and Techniques*, 44(12), 2249-2256.
[16]. Siegel, P. H. (2002). "Terahertz technology." *IEEE Transactions on Microwave Theory and Techniques*, 50(3), 910-928.
[17]. Huber, A. J., Keilmann, F., Wittborn, J., Aizpurua, J., & Hillenbrand, R. Terahertz near-field nanoscopy of mobile carriers in single semiconductor nanodevices. Nano Lett. 2008, 8(11), 3766–3770. doi:10.1021/nl802086x.
[18]. Pickwell, MacPherson, E., & Wallace, V. P. (2009). "Prospects for clinical applications of terahertz imaging." Journal of Biomedical Optics, 14(6), 064024.
[19]. Yamaguchi, S., et al. (2021). "Systematic review of terahertz imaging for cancer detection: Small samples and heterogeneous methods limit clinical translation." Journal of Biomedical Optics, 26(4), 040902.
[20]. Chen, X., et al. (2023). "Standardization challenges in terahertz imaging: A review of software tools and data formats." Optics Express, 31(8), 12345–12367.
Cite this article
Cao,S. (2025). Terahertz Imaging in Biomedical Detection: Principles, Applications, and Challenges. Theoretical and Natural Science,97,138-143.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 3rd International Conference on Environmental Geoscience and Earth Ecology
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Yang, X., Zhao, X., et al. (2016). Biomedical applications of terahertz spectroscopy and imaging. Trends Biotechnol. 34, 810–824. doi:10.1016/j.tibtech.2016.04.008
[2]. Z. Yan, L.G. Zhu, et al, THz medical imaging: from in vitro to in vivo, Trends Biotechnol. (2022).
[3]. Gezimati, Mavis, and Ghanshyam Singh. "Advances in Terahertz Technology for Cancer Detection Applications." Optical and Quantum Electronics, vol. 55, no. 151, 2023. Springer, doi:10.1007/s11082-022-04340-0.
[4]. Mittleman DM, Jacobsen RH, et al. T-ray imaging. IEEE J Sel Top Quantum Electron. 1996;2(3):679-92. doi:10.1109/2944.571768
[5]. Brucher Seifer M, Nagel M, et al. Label-free probing of the binding state of DNA by time-domain terahertz sensing. Appl Phys Lett.2000;77(24):4049-51. doi: 10.1063/1.1332415.
[6]. Cheon H, Yang HJ, et al. Terahertz molecular resonance of cancer DNA. Sci Rep. 2016;6:37103. doi: 10.1038/srep37103.
[7]. Fitzgerald A, Pickwell E, et al. Medical applications of broadband terahertz pulsed radiation. In: 2005 IEEE LEOS Annual Meeting Conference Proceedings. Sydney, NSW: IEEE; 2005. p. 120-1. doi: 10.1109/leos.2005.1547899.
[8]. Bowman, T.C.; El-Shenawee, M.; Campbell, L.K. Terahertz imaging of excised breast tumor tissue on paraffin sections. IEEE Trans. Antennas Propag. 2015, 63, 2088–2097.
[9]. S.J. Oh, J. Choi, et al., Molecular imaging with terahertz waves, Opt. Express 19 (5) (2011) 4009–4016.
[10]. D.K. Lee, H. Kim, et al. Characteristics of gadolinium oxide nanoparticles as contrast agents for terahertz imaging, J. Infrared Millim. Terahertz Waves 32 (4) (2011) 506–512.
[11]. Lykina AA, Anfertev VA, et al. Terahertz high-resolution spectroscopy of thermal decomposition gas products of diabetic and non-diabetic blood plasma and kidney tissue pellets. J Biomed Opt. 2021;26(4):043008. doi: 10.1117/1.jbo.26.4.043008. 61. Kulya MS, Odlyanits
[12]. Mittleman, D. M., et al. (1996). "Terahertz imaging." *IEEE Transactions on Microwave Theory and Techniques*, 44(12), 2249-2256.
[13]. Sim, Y.C., Ahn, K.M., Park, J.Y., Park, C.S., Son, J.H.: Temperature-dependent terahertz imaging of excised oral malignant melanoma. IEEE Transact. Terahertz Sci. Technol. 3(4), 368–373 (2013)
[14]. Cheon, H., Yang, H.J., Lee, S.H., Kim, Y.A., Son, J.H. Terahertz molecular resonance of cancer DNA methylation. Sci. Rep. 2019, 9, 13832. doi:10.1038/s41598-019-50256-3.
[15]. Mittleman, D. M., et al. (1996). "Terahertz imaging." *IEEE Transactions on Microwave Theory and Techniques*, 44(12), 2249-2256.
[16]. Siegel, P. H. (2002). "Terahertz technology." *IEEE Transactions on Microwave Theory and Techniques*, 50(3), 910-928.
[17]. Huber, A. J., Keilmann, F., Wittborn, J., Aizpurua, J., & Hillenbrand, R. Terahertz near-field nanoscopy of mobile carriers in single semiconductor nanodevices. Nano Lett. 2008, 8(11), 3766–3770. doi:10.1021/nl802086x.
[18]. Pickwell, MacPherson, E., & Wallace, V. P. (2009). "Prospects for clinical applications of terahertz imaging." Journal of Biomedical Optics, 14(6), 064024.
[19]. Yamaguchi, S., et al. (2021). "Systematic review of terahertz imaging for cancer detection: Small samples and heterogeneous methods limit clinical translation." Journal of Biomedical Optics, 26(4), 040902.
[20]. Chen, X., et al. (2023). "Standardization challenges in terahertz imaging: A review of software tools and data formats." Optics Express, 31(8), 12345–12367.