1. Introduction
Sleepwalking, a mysterious sleep phenomenon, has long intrigued and been explored by people. Whether it is bloggers sharing their sleepwalking experiences on social media or news reports of sleepwalkers breaking the law, these instances demonstrate that sleepwalking not only affects personal sleep quality but also poses potential threats to the safety of oneself and others [1]. Despite ongoing research into sleepwalking, many mysteries remain unsolved. Understanding sleepwalking is of great significance, not only for the advancement of scientific knowledge, but also for enhancing the quality of life of those affected and their families. By analyzing the differences in sleepwalking between children and adults, this study provides valuable insights into its developmental patterns and underlying mechanisms. This kind of knowledge can direct clinicians to customize age - specific management strategies, thus decreasing the risks related to sleepwalking, like injuries or disruptions to daily life. Furthermore, this paper synthesizes existing research to highlight gaps in the current understanding of sleepwalking, paving the way for future empirical studies. By focusing on genetic factors, brain activity changes, and effective treatments, this study contributes to the development of more precise diagnostic tools and targeted therapies. Ultimately, this research not only deepens our understanding of sleepwalking as a phenomenon but also promotes safer sleep environments and better mental health outcomes for individuals impacted by this condition.
2. Overview of sleepwalking
2.1. Definition and basic concepts of sleepwalking
Sleepwalking, which is known as somnambulism in medical terms, generally refers to the behavior of walking while asleep.. The International Classification of Sleep Disorders defines it as "complex behaviors initiated during partial arousal from slow-wave sleep... Sleepwalkers exhibit disorientation in time and space, slow speech, severely reduced consciousness, and sluggish responses to questions or requests, often accompanied by significant anterograde and retrograde amnesia" [1]. However, not all sleepwalkers fully exhibit these characteristics, and some may demonstrate the ability to interact with the external environment during sleepwalking [2].
2.2. Mechanism of sleepwalking in the sleep cycle
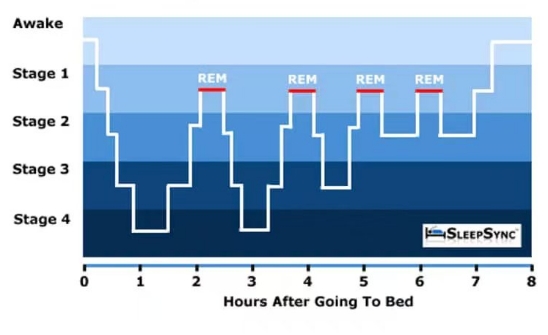
Sleep consists of rapid eye movement (REM) sleep and non-rapid eye movement (NREM) sleep, which can be further divided into N1, N2, and N3 stages (with N3 being slow-wave sleep). Sleepwalking mostly occurs during the N3 stage of slow-wave sleep, where brain activity is relatively slow, and the body is in a deep sleep state, making it difficult to awaken. Under certain influences(as shown in Figure 1), some brain regions awaken prematurely while others remain asleep, leading to a lack of coordination between consciousness and motor functions, thus triggering sleepwalking behavior [3].
2.3. Distinction between sleepwalking and similar disorders
Sleepwalking needs to be distinguished from similar sleep disorders such as night terrors and nightmares. Night terrors also occur during slow-wave sleep, with patients often experiencing sudden awakenings, screaming, and intense fear accompanied by autonomic nervous system responses. However, these episodes are generally short-lived, and patients usually have vague memories of the events [1]. Nightmares, on the other hand, mostly occur during REM sleep and involve frightening dreams that patients can usually recall clearly upon waking, with consciousness quickly returning to full alertness. Compared to sleepwalking, nightmares involve less physical activity and are primarily characterized by psychological fear experiences [3].
3. Clinical manifestations and influencing factors of sleepwalking in children
3.1. Clinical manifestations
Sleepwalking in children is relatively common in clinical settings, with diverse manifestations. Some children exhibit simple actions during sleepwalking, such as sitting up or walking in bed, while others may engage in relatively complex behaviors like dressing or opening doors [1]. These actions often lack a clear purpose and are more mechanical. For instance, observations of numerous children have shown that their behavior during sleepwalking is typically rigid, with weak perception and response abilities to the surrounding environment [1]. They may avoid familiar obstacles during sleepwalking but struggle to respond appropriately to sudden situations. Additionally, children often display a blank expression and vacant gaze during sleepwalking, and even when interacting with others, they may struggle to provide clear responses.
3.2. Influencing factors
The occurrence of sleepwalking in children is influenced by a combination of developmental, genetic, environmental, psychological, and health-related factors.
The prevalence of sleepwalking in children is closely related to age. Multiple studies have shown that the prevalence of sleepwalking in children peaks around the age of 10 [1, 5]. In early childhood, the nervous system is not yet fully developed, and the brain's capacity to regulate the sleep cycle is relatively weak. As a result, sleep is unstable and the risk of sleepwalking is increased. As children grow older, the nervous system matures, and sleep structure stabilizes, resulting in a decrease in sleepwalking incidence. For example, a study on Finnish twin cohorts found significant differences in the prevalence of childhood sleepwalking across different age groups, peaking in mid-childhood and gradually declining thereafter [6].
Genetic factors also have a high correlation with the occurrence of sleepwalking in children. Research indicates that if parents have a history of sleepwalking, the prevalence of sleepwalking in their children significantly increases [1]. Studies show that when both parents have a history of sleepwalking, the prevalence in children is as high as 61.5%, compared to only 22.5% in children whose parents have no such history [1]. Twin studies have found higher concordance rates of sleepwalking in monozygotic twins compared to dizygotic twins, further confirming the influence of genetic factors. This suggests that sleepwalking has a certain genetic susceptibility, possibly involving the combined action of multiple genes [6].
Factors such as sleep deprivation, irregular sleep patterns, and noisy sleep environments can also trigger sleepwalking in children. When children are sleep-deprived, the brain's fatigue state affects the normal regulation of the sleep cycle, altering the proportion and quality of slow-wave sleep, thereby increasing the likelihood of sleepwalking [7]. Additionally, disturbances such as noise and strong light in the sleep environment can disrupt sleep stability and trigger sleepwalking. If children are exposed to a poor sleep environment for a long time, for example, sharing a bed with parents having bad sleep habits or living in a noisy environment, the incidence of sleepwalking will be relatively high [7].
Certain psychological pressures during childhood, such as academic stress and changes in a family environment, may also be related to the occurrence of sleepwalking [1]. When children face excessive psychological pressure, it can affect their sleep quality, leading to sleepwalking. Some children may experience increased frequency of sleepwalking episodes after events such as school transfers or family relocations [1]. Additionally, certain illnesses, such as fever and respiratory infections, may also become triggering factors for sleepwalking, possibly due to physical discomfort affecting sleep stability [7].
4. Clinical manifestations and influencing factors of sleepwalking in adults
Adult sleepwalking is a multifaceted phenomenon influenced by a combination of behavioral, genetic, psychological, physiological, and external factors.
4.1. Clinical manifestations
The behavioral manifestations of sleepwalking in adults are more complex and diverse than in children. In addition to simple walking, adults may engage in complex behaviors such as cooking or driving [2]. These actions may appear purposeful but are actually performed in an unconscious state, and adult sleepwalkers typically lack memory of their actions after an episode [2]. Surveys of adult sleepwalking patients have found that some engage in habitual actions from daily life during sleepwalking, such as opening the refrigerator or using household appliances, and some even drive while sleepwalking. These behaviors pose threats not only to their own safety but also to others [2].
4.2. Influencing factors
Genetic factors also play a significant role in adult sleepwalking. Studies have shown that the prevalence of sleepwalking is significantly higher among first-degree relatives of adult sleepwalkers compared to the general population [6]. The influence of genetic factors on adult sleepwalking is 80% in males and 36% in females [6], indicating a strong association between gender and the neural mechanisms influenced by genetics.
Work-related stress, economic pressure, and social stress in life can lead to excessive psychological burdens, keeping the brain's nerves in a state of tension, which can result in partial awakenings during sleep, reduced sleep quality, and ultimately sleepwalking [3, 8]. This is evidenced by the fact that certain high-intensity professions, such as healthcare workers and financial professionals, experience higher rates of sleepwalking due to high work pressure and fast-paced lifestyles [3].
Common sleep disorders in adults, such as sleep apnea-hypopnea syndrome and periodic limb movement disorder, are closely related to the occurrence of sleepwalking [7, 9]. These sleep disorders cause sleep fragmentation, leading to frequent micro-awakenings in the brain during sleep, increasing the risk of sleepwalking [7, 9]. Studies have shown that some adult sleepwalking patients also suffer from sleep breathing disorders, and treating these disorders can alleviate sleepwalking symptoms [7].
Certain mental illnesses, such as anxiety and depression, are also closely related to the occurrence of sleepwalking. These mental illnesses alter the balance of neurotransmitters in the brain, disrupting sleep regulation mechanisms and increasing the likelihood of sleepwalking [10].
The use and abuse of certain medications can also trigger sleepwalking in adults. For example, sedative-hypnotics and antipsychotics can affect the brain's neural regulation functions and alter sleep structure, increasing the likelihood of sleepwalking [3]. Additionally, alcohol consumption is associated with sleepwalking, as drinking can alter sleep depth and weaken the brain's inhibitory functions, making sleepwalking more likely. Long-term drinkers are more prone to sleepwalking behaviors after drinking, and these behaviors may be more dangerous [3].
5. Coping strategies and recommendations for sleepwalking
Preventing sleepwalking in children involves several proactive measures. Parents should ensure their children get sufficient sleep and follow a consistent sleep schedule to promote healthy sleep patterns. Creating a quiet, comfortable, and safe sleep environment is equally important to minimize disruptions during the night. If a child begins sleepwalking, parents should avoid forcibly waking them, as this can cause confusion or distress. Instead, gently guiding the child back to bed and soothing them can help them resume sleeping peacefully. For children who experience frequent or disruptive episodes, seeking professional medical advice is essential. Healthcare providers may recommend treatments such as scheduled awakening therapy, which involves waking the child shortly before typical sleepwalking episodes to disrupt the cycle [1].
For adults, stress management plays a key role in reducing sleepwalking. Activities such as regular exercise, yoga, and meditation can help alleviate stress and improve sleep quality. Adults should also maintain a regular bedtime routine, avoid staying up late, and limit screen time before sleep to promote relaxation. Safety precautions are crucial for those who sleepwalk frequently. These precautions include removing sharp objects, locking windows and installing barriers to prevent accidents.. Additionally, creating a calming pre-sleep routine, such as reading or listening to soothing music, can help prepare the mind for restful sleep. In severe cases, medical professionals may recommend psychological therapies or medications to address underlying causes and manage symptoms effectively [3].
Furthermore, both children and adults can benefit from avoiding stimulants such as caffeine or alcohol close to bedtime, as these substances can disrupt sleep patterns and increase the likelihood of sleepwalking episodes. Monitoring sleep habits through sleep diaries or wearable devices may also help identify patterns or triggers associated with sleepwalking. By understanding these triggers, families and individuals can work together to implement personalized strategies to reduce occurrences and improve sleep quality [11].
6. Conclusion
This study analyzes the manifestations, causes, and coping strategies of sleepwalking in children and adults, discussing the definition of sleepwalking, its mechanisms in the sleep cycle, and its distinction from similar disorders. Sleepwalking occurs in both children and adults, with differences in clinical manifestations and influencing factors. This paper has limitations due to the lack of empirical research and the limited number of references. Future research is expected to further explore sleepwalking through more empirical studies, focusing on genetic patterns, changes in brain activity during sleepwalking, and treatment methods.
References
[1]. Petit D, Pennestri MH, Paquet J, et al. Childhood Sleepwalking and Sleep Terrors A Longitudinal Study of Prevalence and Familial Aggregation [J]. JAMA Pediatr, 2015, 169(7): 653 - 658.
[2]. Oudiette D, Leu S, Pottier M, et al. Dreamlike Mentations during Sleepwalking and Sleep Terrors in Adults [J]. SLEEP, 2009, 32(12): 1621 - 1627.
[3]. Zadra A, Desautels A, Petit D, et al. Somnambulism: clinical aspects and pathophysiological hypotheses [J]. Lancet Neurol, 2013, 12(3): 285 - 294.
[4]. Doe, J. Catching Zzzs: The Science of Sleep [/OL]. [irunfar.com]. (2025 - 05 - 07). https: //irunfar.com/catching-zzzs-the-science-of-sleep.
[5]. Stallman HM, Kohler M. Prevalence of Sleepwalking: A Systematic Review and Meta - Analysis [J]. PLoS ONE, 2016, 11(11): e0164769.
[6]. Hublin C, Kaprio J, Partinen M, et al. Prevalence and genetics of sleepwalking: A population - based twin study [J]. Neurology, 1997, 48(1): 177 - 181.
[7]. Guilleminault C, Palombini L, Pelayo R, et al. Sleepwalking and Sleep Terrors in Prepubertal Children: What Triggers Them? [J]. Pediatrics, 2003, 111(1): e17 - e25.
[8]. Wang X, et al. The relationship between work - related stress and sleepwalking in adults [J]. Stress and Health, 2018, 34(6): 545 - 552.
[9]. Guilleminault C, Kirisoglu C, da Rosa AC, et al. Sleepwalking, a disorder of NREM sleep instability [J]. Sleep Medicine, 2006, 7(2): 163 - 170.
[10]. Liu Z, et al. Association between sleepwalking and mental disorders in adults: a cross - sectional study [J]. Journal of Affective Disorders, 2019, 252: 10 - 16.
[11]. Arnulf I. Sleepwalking [J]. Current Biology, 2018, 28(22): R1283 - R1295.
Cite this article
Feng,Y. (2025). A Comprehensive Review of Sleepwalking. Theoretical and Natural Science,133,23-28.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of ICBioMed 2025 Symposium: AI for Healthcare: Advanced Medical Data Analytics and Smart Rehabilitation
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Petit D, Pennestri MH, Paquet J, et al. Childhood Sleepwalking and Sleep Terrors A Longitudinal Study of Prevalence and Familial Aggregation [J]. JAMA Pediatr, 2015, 169(7): 653 - 658.
[2]. Oudiette D, Leu S, Pottier M, et al. Dreamlike Mentations during Sleepwalking and Sleep Terrors in Adults [J]. SLEEP, 2009, 32(12): 1621 - 1627.
[3]. Zadra A, Desautels A, Petit D, et al. Somnambulism: clinical aspects and pathophysiological hypotheses [J]. Lancet Neurol, 2013, 12(3): 285 - 294.
[4]. Doe, J. Catching Zzzs: The Science of Sleep [/OL]. [irunfar.com]. (2025 - 05 - 07). https: //irunfar.com/catching-zzzs-the-science-of-sleep.
[5]. Stallman HM, Kohler M. Prevalence of Sleepwalking: A Systematic Review and Meta - Analysis [J]. PLoS ONE, 2016, 11(11): e0164769.
[6]. Hublin C, Kaprio J, Partinen M, et al. Prevalence and genetics of sleepwalking: A population - based twin study [J]. Neurology, 1997, 48(1): 177 - 181.
[7]. Guilleminault C, Palombini L, Pelayo R, et al. Sleepwalking and Sleep Terrors in Prepubertal Children: What Triggers Them? [J]. Pediatrics, 2003, 111(1): e17 - e25.
[8]. Wang X, et al. The relationship between work - related stress and sleepwalking in adults [J]. Stress and Health, 2018, 34(6): 545 - 552.
[9]. Guilleminault C, Kirisoglu C, da Rosa AC, et al. Sleepwalking, a disorder of NREM sleep instability [J]. Sleep Medicine, 2006, 7(2): 163 - 170.
[10]. Liu Z, et al. Association between sleepwalking and mental disorders in adults: a cross - sectional study [J]. Journal of Affective Disorders, 2019, 252: 10 - 16.
[11]. Arnulf I. Sleepwalking [J]. Current Biology, 2018, 28(22): R1283 - R1295.