1. Introduction
Falls represent a major public health concern within China's aging population, ranking as a leading cause of injury-related mortality among older adults [1, 2]. Beyond physical injury, falls can induce a fear of falling, leading to reduced activity, functional decline, and diminished quality of life [3, 4]. Therefore, taking necessary preventive measures to reduce fall risk in middle-aged and older adults is crucial.
Recognized risk factors for falls include gender, impairment in Activities of Daily Living (ADL), gait speed, and chronic conditions such as arthritis [5-7]. However, since cross-sectional gait speed measurement is considered to have low overall predictive value for fall risk, this study primarily investigates the impact of changes in average walking speed on fall risk factors in middle-aged and older adults, while also exploring its interaction with other risk factors on fall risk. Therefore, this study used CHARLS data to explore the impact of ADL, average walking speed, and arthritis history on fall risk among Chinese middle-aged and older adults and to develop a predictive model.
2. Research subjects and methods
2.1. Research subjects
This study utilized data from the nationally representative 2014 China Health and Retirement Longitudinal Study (CHARLS). After excluding participants under 45, over 100 years old, and those with missing data or outliers, 7,367 individuals were included in the analysis
2.2. Research indicators
2.2.1. Exposure factors
This study selected key exposure factors related to physical function and musculoskeletal chronic diseases, including basic six-item ADL (eating, dressing, getting in/out of bed, bathing, using the toilet, and controlling urination/defecation), average walking speed, and arthritis history .The basic six activities of daily living (ADL) were scored according to the standard questionnaire of the China Health and Retirement Longitudinal Study (CHARLS), ranging from 0 (no difficulty in all functions) to 6 (difficulty in all functions). The higher the score, the more functions with difficulty(Table 1).
|
variable |
Description |
|
Age |
Years (range: 45 to 100) |
|
Gender |
Male/Female |
|
Average walking speed |
Meters per second (m/s), average of two 2.5-meter walks |
|
Adlab_c (Activities of Daily Living |
Score from 0 (no difficulty) to 6 (difficulty in all 6 ADLs) |
|
Stroke |
Physician-diagnosed history of stroke (Yes / No) |
|
Arthritis |
Physician-diagnosed history of arthritis (Yes / No) |
|
Drinking |
History of alcohol consumption (Yes / No) |
2.2.2. Outcome factor and covariates
The outcome factor of this study was whether a fall occurred in the past year among middle-aged and older adults aged 45-100. Meanwhile, covariates included age, gender, stroke history, and drinking history. These variables were all identified as potential confounding factors and adjusted for in the models.
2.3. Statistical methods
Statistical analyses were performed using R software. Descriptive data are presented as means ± standard deviations or counts (percentages). We used the t-test to handle continuous variables and the chi-square test to handle categorical variables when comparing the fallers with the non-fallers. To identify independent risk factors, a multivariable logistic regression model was fitted, adjusting for all pre-specified exposure variables and covariates. Furthermore, to assess potential effect modification by age, the analysis was stratified into three groups (45–64, 65–70, and 71–95 years based on tertiles), and the logistic regression model was re-established within each stratum to examine the consistency of the associations.
3. Research results
3.1. Overview of the impact of physical function and musculoskeletal chronic diseases on falls in Chinese older adults
Univariate analysis revealed significant differences in baseline characteristics between the fall and non-fall groups (Table 2). The fall group had a significantly higher proportion of females and individuals with a history of stroke or arthritis. A clear gradient was observed between the degree of ADL impairment and fall incidence. Additionally, the fall group was slightly older and had a slower average walking speed (Table 3). No significant difference was found in drinking habits between the two groups.
|
Total |
outcome |
|||
|
Weighted N (%) |
No N(%) |
YES N(%) |
p-value |
|
|
Total |
7367 |
5900 |
1467 |
|
|
Exposure |
||||
|
Gender |
<0.001 |
|||
|
male |
3,647 (50%) |
3.071(52%) |
576(39%) |
|
|
female |
3,720 (50%) |
2,829 (48%) |
891 (61%) |
|
|
Physical functions |
||||
|
Adlab_c |
<0.001 |
|||
|
Normal |
5,509 (75%) |
4,636 (79% |
873 (60%) |
|
|
Level1 |
956 (13% |
683 (12%) |
273 (19%) |
|
|
Level2 |
429 (5.8%) |
289 (4.9%) |
140 (9.5%) |
|
|
Level3 |
232 (3.1%) |
146 (2.5%) |
86 (5.9%) |
|
|
Level4 |
129 (1.8% |
83 (1.4%) |
46 (3.1%) |
|
|
Level5 |
74 (1.0%) |
41 (0.7%) |
33 (2.2%) |
|
|
Level6 |
38 (0.5%) |
22 (0.4%) |
16 (1.1%) |
|
|
Chronic disease |
||||
|
Stroke |
<0.001 |
|||
|
No |
7,056 (96%) |
5,677 (96%) |
1,379 (94%) |
|
|
Yes |
311 (4.2%) |
223 (3.8%) |
88 (6.0%) |
|
|
Arthritis |
<0.001 |
|||
|
No |
3,842 (52%) |
3,237 (55%) |
605 (41%) |
|
|
Yes |
3,525 (48%) |
2,663 (45%) |
862 (59% |
|
|
Alcohol Drinking |
0.13 |
|||
|
No |
4,980 (68%) |
3,964 (67%) |
1,016 (69%) |
|
|
Yes |
2,387 (32%) |
1,936 (33%) |
451 (31%) |
|
variable |
Total sample (N = 7367) |
The non-fall group (N=5900) |
Fall group (N=1467) |
P value |
|
Age (years) |
67.0 (63.0, 72.0) |
67.0 (63.0, 72.0) |
68.0 (64.0, 73.0) |
0.003 |
|
Average walking speed (meters per second) |
0.77 (0.63, 0.92) |
67.0 (63.0, 72.0) |
0.72 (0.58, 0.87) |
<0.001 |
3.2. Multivariate logistic regression analysis
After adjusting for confounding factors, several factors remained independent predictors of fall risk (Table 4). Female gender was associated with a 62% increased risk of falls (adjusted odds ratio = 1.62, 95% confidence interval: 1.42 - 1.84). There was a clear dose-response relationship between the degree of impairment in activities of daily living and fall risk; even mild impairment (level 1) nearly doubled the risk (adjusted odds ratio = 1.90), and the risk rose sharply with increasing impairment. A history of arthritis and stroke also significantly increased the risk of falls. Conversely, a faster walking speed was a protective factor (adjusted odds ratio = 0.73 for each additional 1 meter/second). After adjustment, age itself was not a significant predictor.
|
Crude OR(95%) |
Full model Adjusted OR(95%) |
Adjusted P-value |
|
|
Gender |
1.68(1.49,1.89) |
1.63 (1.43, 1.86) |
<0.001 |
|
Physical functions |
|||
|
Adlab_c |
|||
|
Normal |
|||
|
Level1 |
2.13 (1.81,2.49) |
1.90 (1.61,2.23) |
<0.001 |
|
Level2 |
2.56 (2.06,.3.17) |
2.22 (1.78, 2.77) |
<0.001 |
|
Level3 |
3.13 (2.36,4.11) |
2.59 (1.95, 3.44) |
<0.001 |
|
Level4 |
2.94 (2.02, 4.23) |
2.38 (1.63, 3.46) |
<0.001 |
|
Level5 |
4.27 (2.67, 6.78) |
3.37 (2.09, 5.41) |
<0.001 |
|
Level6 |
3.86 (1.99, 7.34) |
2.84 (1.47, 5.48) |
0.002 |
|
chronic disease |
|||
|
Stroke |
1.62. (1.25, 2.09) |
1.32 (1.01, 1.72) |
0.047* |
|
Arthritis |
1.73 (1.54, 1.95) |
1.43 (1.27, 1.62) |
<0.001 |
|
Alcohol drinking |
0.91 (0.80, 1.03) |
1.22 (1.06, 1.40) |
0.003 |
|
Age |
1.01(1.00,1.02) |
1.00 (0.99, 1.01) |
0.576 |
|
Average Walk speed |
0.39(0.30,0.51) |
0.73 (0.54, 0.98) |
<.001 |
OR = Odds ratio CI = Confidence interval
3.3. Model for the impact of physical function and musculoskeletal chronic diseases on falls in Chinese older adults
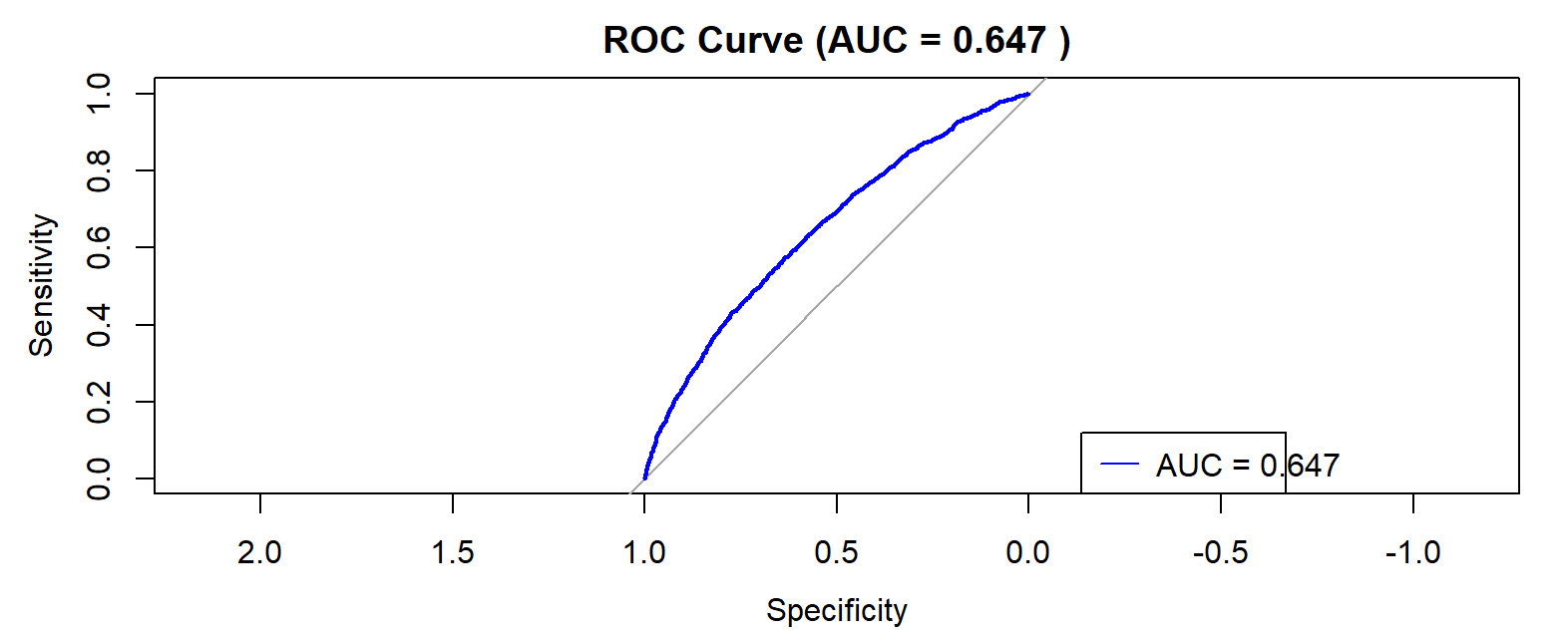
Prior to model interpretation, multicollinearity was assessed and all corrected Generalized Variance Inflation Factor (GVIF) values ranged between 1.01 and 1.11, well below the threshold of 5, indicating no severe multicollinearity. The multivariable logistic regression model demonstrated modest discriminative ability for fall risk, with an area under the ROC curve of 0.647 for the full model (Figure 1).
3.4. Model for the impact of physical function and musculoskeletal chronic diseases on falls in Chinese older adults stratified by age
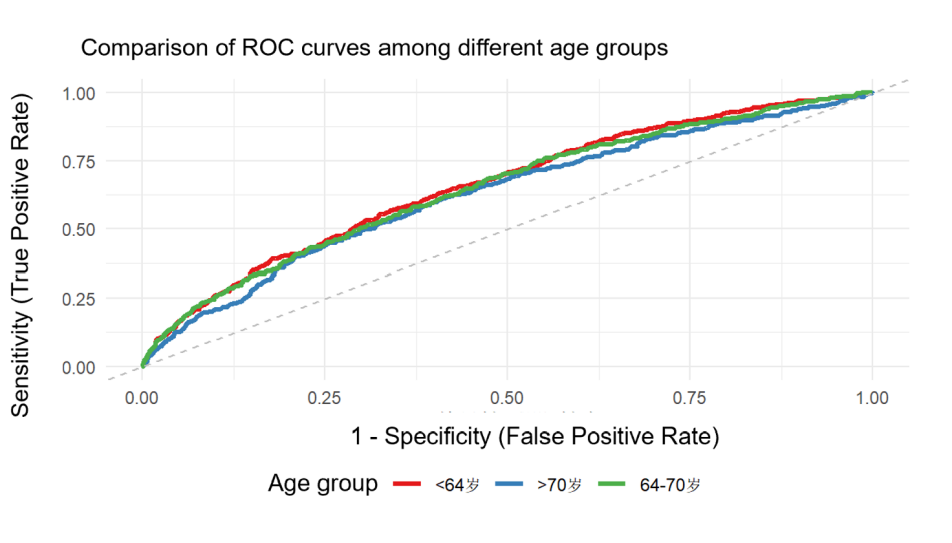
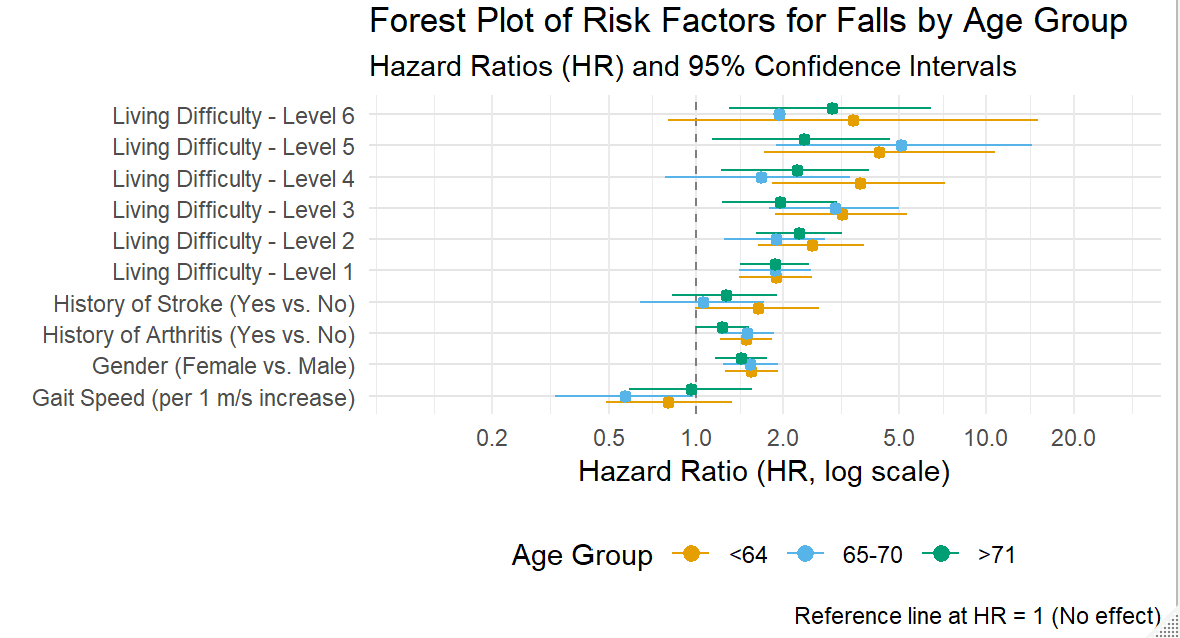
To explore the moderating effect of age, we stratified the analysis into three groups (45–64, 65–70, and 71–95 years). The model maintained stable predictive performance across all age strata, with AUC values ranging between 0.63 and 0.66 (Figure 2).A forest plot clearly shows the extent to which each major risk factor affects the risk of falls among elderly people in China (Figure 3). For instance, being female, having a history of arthritis, and all levels of impaired daily living activities significantly increase the risk of falls, while a faster walking speed provides protection in all groups.
4. Discussion
4.1. The impact of gender and ADL impairment level on fall risk in middle-aged and older adults
Gender, activities of daily living (ADL) ability, and history of fall-related injuries are considered risk factors for fall-related injuries [5-8]. The data analysis of this study indicates that there is a clear dose-response relationship between the degree of physical function impairment and the risk of falling. As the degree of ADL impairment increases, the risk of falling shows a monotonically upward trend. This finding is similar to the research results of Lin Jinlong et al. [9]. In addition, most studies have reported that the fall rate of elderly women is higher than that of elderly men [10-14].
4.2. The impact of arthritis on fall risk in middle-aged and older adults
This study confirmed arthritis as a significant independent risk factor for falls, which aligns with previous meta-analyses [9]. The underlying mechanism likely involves the core features of arthritis pathology: joint pain, muscle weakness, and impaired balance [15]. These factors can lead to adaptive gait patterns, reduced physical activity, and ultimately, a greater risk of falling [16, 17]. The association appears to be particularly pronounced in women [18].
4.3. The impact of average walking speed on fall risk in middle-aged and older adults
Our finding that faster walking speed is a significant protective factor (aOR=0.73 per m/s) is consistent with existing literature that identifies gait speed as a reliable predictor of fall risk [8, 19]. A slower gait may reflect underlying impairments in strength and balance, making it more difficult to recover from a loss of equilibrium [20, 21].
5. Conclusion
This study identified impairment in Activities of Daily Living (ADL), slower average walking speed, and a history of arthritis as significant, independent risk factors for falls among middle-aged and older Chinese adults. A strong graded dose-response relationship was observed between the degree of ADL impairment and fall risk.
The main limitations include the cross-sectional design and the use of self-reported data, which preclude causal inference and may be subject to recall bias. Future longitudinal studies are needed to confirm these associations and elucidate the underlying mechanisms. For clinical and public health practice, incorporating simple assessments of walking speed and ADL into routine evaluations could help identify high-risk individuals for targeted interventions.
References
[1]. Mei, L., Wang, L. N., & Jiang, Q. B. (2022). China's elderly mortality model. Population Journal, 2022, 44 (01): 87-98. DOI: 10.16405/j.cnki.1004-129X.2022.01.007.
[2]. Yang, X. X., Ding, X. B., Mao, D. Q., et al. (2023). Incidence and influencing factors of falls among rural elderly aged 65 and above in Chongqing. Journal of Public Health and Preventive Medicine, 2023, 34 (01): 78-82.
[3]. Schoene D, Heller C, Aung YN, Sieber CC, Kemmler W, Freiberger E. A systematic review on the influence of fear of falling on quality of life in older people: is there a role for falls? Clin Interv Aging. 2019 Apr 24; 14: 701-719. doi: 10.2147/CIA.S197857. PMID: 31190764; PMCID: PMC6514257.
[4]. Zhou, J., Liu, B., & Qin, M. Z. (2021). Research progress on risk assessment and intervention of falls in the elderly Chinese Journal of Geriatrics, 2021, 40(3), 388–392. https: //doi.org/10.3760/cma.j.issn.0254-9026.2021.03.025
[5]. Murphy J, Isaacs B. The post-fall syndrome. A study of 36 elderly patients [ [J]. Gerontology, 1982, 28(4): 265-270.
[6]. Chang VC, Do MT. Risk factors for falls among seniors: implications of gender [J]. Am J Epidemiol, 2015, 181(7): 521-531. DOI: 10.1093/aje/kwu268.
[7]. Gale CR, Cooper C, Sayer AA. Prevalence and risk factors for falls in older men and women: the English longitudinal study of ageing [J]. Age Ageing, 2016, 45(6): 789-794. DOI: 10.1093/ageing/afw129
[8]. Middleton A, Fritz SL, Lusardi M. Walking speed: the functional vital sign. J Aging Phys Act. 2015; 23(2): 314–22.
[9]. Lin Jinlong, Wei Yue, Chen Gong, Lin Shiqi, Pei Lijun. A cohort study on the influence of the chronic diseases on falls among middle-aged and older Chinese. Chinese Journal of Epidemiology, 2022, 43(2): 218-226.
[10]. Stinchcombe A, Kuran N, Powell S. Report summary. Seniors' Falls in Canada: Second Report: key highlights. Chronic Dis Inj Can. 2014 Jul; 34(2-3): 171-4. English, French. PMID: 24991781.
[11]. Peel NM, Kassulke DJ, McClure RJ. Population based study of hospitalised fall related injuries in older people. Inj Prev. 2002; 8(4): 280–283.
[12]. 14 Salvà A, Bolíbar I, Pera G, et al. Incidence and consequences of falls among elderly people living in the community. Med Clin (Barc). 2004; 122(5): 172–176.
[13]. Stevens JA, Sogolow ED. Gender differences for non-fatal unintentional fall related injuries among older adults. Inj Prev. 2005; 11(2): 115–119.
[14]. Schiller JS, Kramarow EA, Dey AN. Fall Injury Episodes Among Noninstitutionalized Older Adults: United States, 2001–2003. Hyattsville, MD: National Center for Health Statistics; 2007. (Advance data from vital and health statistics, no. 392) (DHHS publication no. (PHS) 2007-1250).
[15]. Manlapaz DG, Sole G, Jayakaran P, et al. Risk factors for falls in adults with knee osteoarthritis: a systematic review [J]. PM R, 2019, 11(7): 745-757. DOI: 10.1002/pmrj.12066
[16]. Chen HL, Lu TW, Wang TM, Huang SC. Biomechanical strategies for successful obstacle crossing with the trailing limb in older adults with medial compartment knee osteoarthritis. J Biomech. 2008; 41(4): 753-61. doi: 10.1016/j.jbiomech.2007.11.017. Epub 2008 Jan 4. PMID: 18177877.
[17]. Kornaat PR, Bloem JL, Ceulemans RY et al. Osteoarthritis of the knee: association between clinical features and MR imaging findings. Radiology 2006; 239: 811–7.
[18]. Arden NK, Nevitt MC, Lane NE et al. Osteoarthritis and risk of falls, rates of bone loss, and osteoporotic fractures. Study of Osteoporotic Fractures Research Group. Arthritis Rheum 1999; 42: 1378–85.
[19]. Buehring B, Krueger D, Fidler E, Gangnon R, Heiderscheit B, Binkley N. Reproducibility of jumping mechanography and traditional measures of physical and muscle function in older adults. Osteoporos Int. 2015 Feb; 26(2): 819-25. doi: 10.1007/s00198-014-2983-z. Epub 2014 Dec 9. PMID: 25488806.
[20]. Bergland A, Jarnlo GB, Laake K. Predictors of falls in the elderly by location. Aging Clinical and Experimental Research. 2003; 15(1): 43–50. [PubMed: 12841418]
[21]. Taylor ME, Delbaere K, Mikolaizak AS, Lord SR, Close JCT. Gait parameter risk factors for falls under simple and dual task conditions in cognitively impaired older people. Gait & Posture. 2013; 37(1): 126–130. [PubMed: 22832468]
Cite this article
Lai,Z. (2025). Exploring the Impact of ADL, Average Walking Speed, and Arthritis History on Fall Risk Among Chinese Older Adults. Theoretical and Natural Science,152,17-23.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of ICMMGH 2026 Symposium: Biomedical Imaging and AI Applications in Neurorehabilitation
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Mei, L., Wang, L. N., & Jiang, Q. B. (2022). China's elderly mortality model. Population Journal, 2022, 44 (01): 87-98. DOI: 10.16405/j.cnki.1004-129X.2022.01.007.
[2]. Yang, X. X., Ding, X. B., Mao, D. Q., et al. (2023). Incidence and influencing factors of falls among rural elderly aged 65 and above in Chongqing. Journal of Public Health and Preventive Medicine, 2023, 34 (01): 78-82.
[3]. Schoene D, Heller C, Aung YN, Sieber CC, Kemmler W, Freiberger E. A systematic review on the influence of fear of falling on quality of life in older people: is there a role for falls? Clin Interv Aging. 2019 Apr 24; 14: 701-719. doi: 10.2147/CIA.S197857. PMID: 31190764; PMCID: PMC6514257.
[4]. Zhou, J., Liu, B., & Qin, M. Z. (2021). Research progress on risk assessment and intervention of falls in the elderly Chinese Journal of Geriatrics, 2021, 40(3), 388–392. https: //doi.org/10.3760/cma.j.issn.0254-9026.2021.03.025
[5]. Murphy J, Isaacs B. The post-fall syndrome. A study of 36 elderly patients [ [J]. Gerontology, 1982, 28(4): 265-270.
[6]. Chang VC, Do MT. Risk factors for falls among seniors: implications of gender [J]. Am J Epidemiol, 2015, 181(7): 521-531. DOI: 10.1093/aje/kwu268.
[7]. Gale CR, Cooper C, Sayer AA. Prevalence and risk factors for falls in older men and women: the English longitudinal study of ageing [J]. Age Ageing, 2016, 45(6): 789-794. DOI: 10.1093/ageing/afw129
[8]. Middleton A, Fritz SL, Lusardi M. Walking speed: the functional vital sign. J Aging Phys Act. 2015; 23(2): 314–22.
[9]. Lin Jinlong, Wei Yue, Chen Gong, Lin Shiqi, Pei Lijun. A cohort study on the influence of the chronic diseases on falls among middle-aged and older Chinese. Chinese Journal of Epidemiology, 2022, 43(2): 218-226.
[10]. Stinchcombe A, Kuran N, Powell S. Report summary. Seniors' Falls in Canada: Second Report: key highlights. Chronic Dis Inj Can. 2014 Jul; 34(2-3): 171-4. English, French. PMID: 24991781.
[11]. Peel NM, Kassulke DJ, McClure RJ. Population based study of hospitalised fall related injuries in older people. Inj Prev. 2002; 8(4): 280–283.
[12]. 14 Salvà A, Bolíbar I, Pera G, et al. Incidence and consequences of falls among elderly people living in the community. Med Clin (Barc). 2004; 122(5): 172–176.
[13]. Stevens JA, Sogolow ED. Gender differences for non-fatal unintentional fall related injuries among older adults. Inj Prev. 2005; 11(2): 115–119.
[14]. Schiller JS, Kramarow EA, Dey AN. Fall Injury Episodes Among Noninstitutionalized Older Adults: United States, 2001–2003. Hyattsville, MD: National Center for Health Statistics; 2007. (Advance data from vital and health statistics, no. 392) (DHHS publication no. (PHS) 2007-1250).
[15]. Manlapaz DG, Sole G, Jayakaran P, et al. Risk factors for falls in adults with knee osteoarthritis: a systematic review [J]. PM R, 2019, 11(7): 745-757. DOI: 10.1002/pmrj.12066
[16]. Chen HL, Lu TW, Wang TM, Huang SC. Biomechanical strategies for successful obstacle crossing with the trailing limb in older adults with medial compartment knee osteoarthritis. J Biomech. 2008; 41(4): 753-61. doi: 10.1016/j.jbiomech.2007.11.017. Epub 2008 Jan 4. PMID: 18177877.
[17]. Kornaat PR, Bloem JL, Ceulemans RY et al. Osteoarthritis of the knee: association between clinical features and MR imaging findings. Radiology 2006; 239: 811–7.
[18]. Arden NK, Nevitt MC, Lane NE et al. Osteoarthritis and risk of falls, rates of bone loss, and osteoporotic fractures. Study of Osteoporotic Fractures Research Group. Arthritis Rheum 1999; 42: 1378–85.
[19]. Buehring B, Krueger D, Fidler E, Gangnon R, Heiderscheit B, Binkley N. Reproducibility of jumping mechanography and traditional measures of physical and muscle function in older adults. Osteoporos Int. 2015 Feb; 26(2): 819-25. doi: 10.1007/s00198-014-2983-z. Epub 2014 Dec 9. PMID: 25488806.
[20]. Bergland A, Jarnlo GB, Laake K. Predictors of falls in the elderly by location. Aging Clinical and Experimental Research. 2003; 15(1): 43–50. [PubMed: 12841418]
[21]. Taylor ME, Delbaere K, Mikolaizak AS, Lord SR, Close JCT. Gait parameter risk factors for falls under simple and dual task conditions in cognitively impaired older people. Gait & Posture. 2013; 37(1): 126–130. [PubMed: 22832468]