1. Introduction
Obesity has been an emerging risk factor for various diseases, including diabetes, cardiovascular diseases, and cancer. Obesity has become prevalent reaching 41.9% in 2017 in the United States (US) alone [1]. According to World Health Organization (WHO), a body mass index (BMI) over 25 kg/m2 is considered overweight, while BMI over 30 kg/m2 is considered obese [2]. Obesity has turned into an epidemic with 4 million mortalities in 2017 from obesity-related disorders [2]. From 1975 - 2016, the prevalence of overweight or obese children from the age of 5-19 years increased from 4% to 18% [2]. According to the Centers for Disease Control and Prevention (CDC), 1 in 5 children in the US struggle with obesity [3]. The World Obesity Federation estimates that by 2020, around 770 million individuals will be affected by obesity, with numbers likely to reach one billion by 2023 [4]. Each year, obesity imposes a financial burden on society costing the US health system an estimated 173 billion dollars [3]. Obesity can lead to all causes of mortality, including type 2 diabetes, hypertension (high blood pressure), sleep apnea, breathing problems, coronary heart disease [5], and potential causes of cancer. Multiple factors, including easy access to high-calorie and low-nutrient food, a sedentary lifestyle, and an irregular sleep schedule have contributed to the higher prevalence of obesity worldwide [6]. Previously, obesity was considered a “rich people's disease” due to the excessive food available for people with higher income; however, as high-calorie products, such as fast foods and junk foods have become more widely available in recent years, obesity does not necessarily relate to social status; instead, it has become an epidemic proportion for all. Multiple factors, such as education and socioeconomic status can influence the prevalence of obesity as it has been shown individuals with college-level education tend to have a lower prevalence of obesity than people without a college-level education [1]. This may be influenced by financial resources and time available to afford a healthier lifestyle.
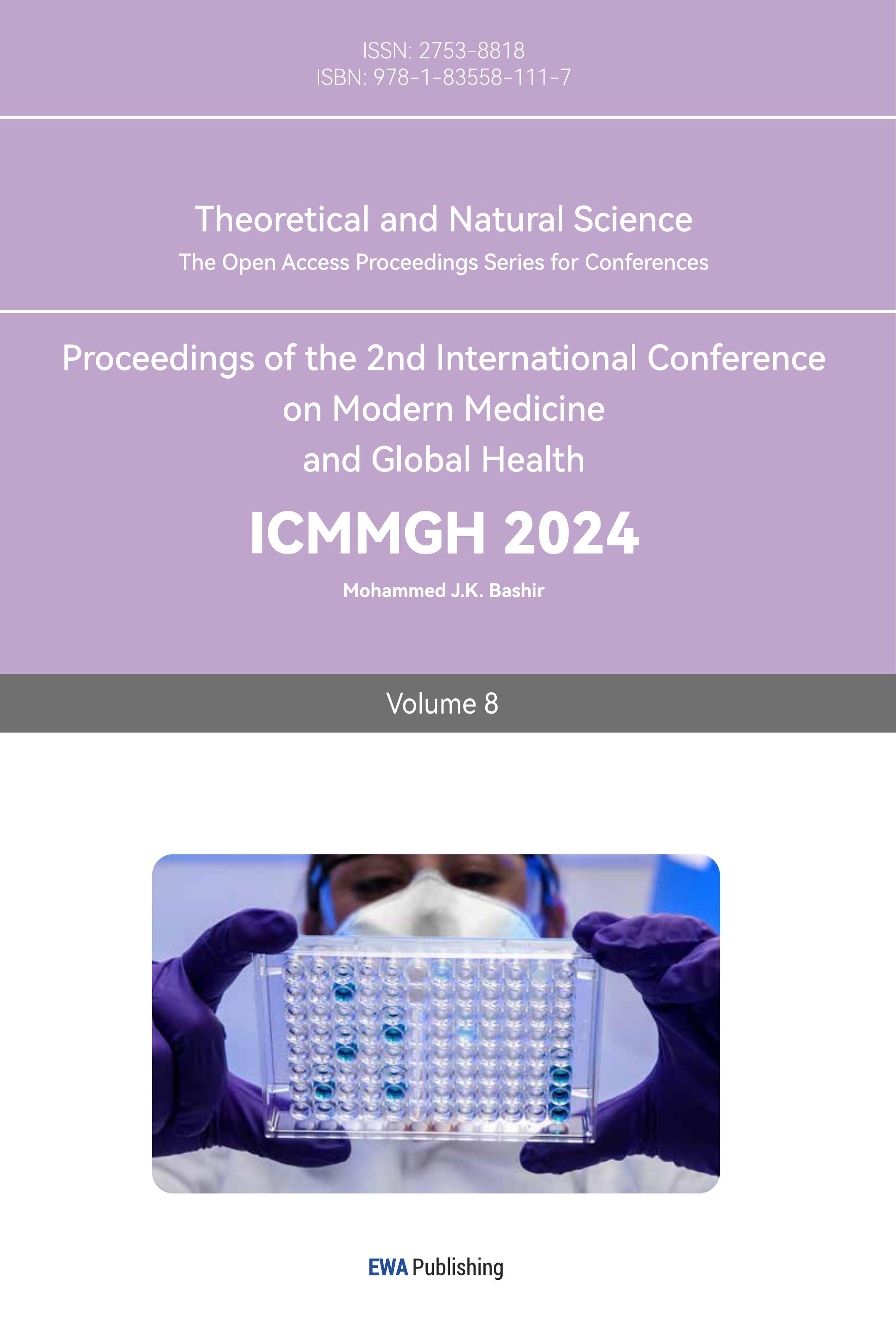
Cancer is the second leading cause of death worldwide leading to roughly 10 million deaths yearly [7]. Obesity consists in about 4-8% of cancer patients, including breast, colorectal, esophageal, kidney, gallbladder, uterine, pancreatic, and liver cancer (Figure 1) [8].
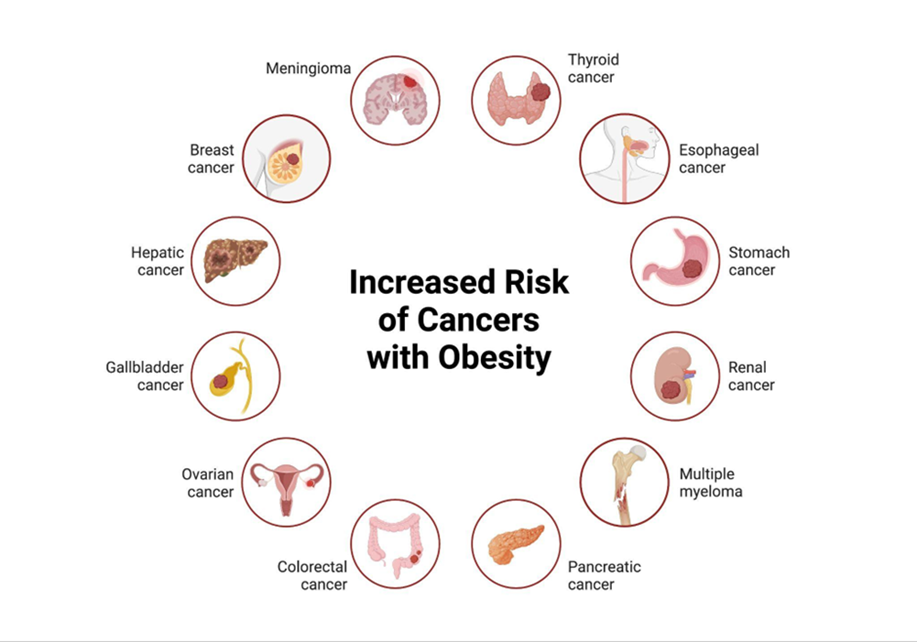
Figure 1. Different types of cancer have a higher risk of occurring from obesity.
In a prospective study focusing on the 57,145 deaths caused by cancer among 900,000 adults in the US who were free of cancer in 1982, the death rates from all cancers combined were 52% higher for men and 62% higher for women in those with a BMI equal to or exceeding 40, compared to individuals of normal weight [9].
Cancer is a disease caused by uncontrolled and abnormal cell division. Cancer cells grow independently from the growing signal, ignore the stop signal, evade apoptosis, trigger angiogenesis, and undergo metastasis allowing them to move to other blood vessels causing damage to the whole body [10]. The newly formed cancer cells divide abnormally which means that they do not function as normal cells, and they compete with normal cells for nutrients. While the mechanism of obesity causing cancer has not yet been well understood, obesity increases mortality rates and influences treatment choices [10].
This paper explores the relationship between cancer and obesity, providing an overview of the characterization of cancer, and investigating the role of obesity as a risk factor for cancer, strategies to reduce the obesity burden, and its future impact on healthcare.
2. Methods
The research was conducted from scholarly sources including Google scholars, the National Center for Biotechnology Information (NCBI), the Centers for Disease Control and Prevention (CDC), the World Health Organization (WHO), and the National Institutes of Health (NIH). The search was mostly limited to papers published in English over the past 20 years that were focused on the following keywords for research: “Obesity”, “Cancer”, “Diabetes”, “Diet”, “Nutrition”, “Oncogene”, “Growth factor”, “Receptor protein”, “Metabolism”. Studies were included within the following criteria: (a) focused on the epidemiology of obesity and cancer, (b) were published in peer-reviewed journals or conference proceedings. Studies with a primary focus on specific populations (e.g., individuals with obesity and cancer) were also included if they provided relevant insights for the research topic. The figures were created using Biorender.
3. Results and discussion
Obesity has become one of the major epidemic issues in the world causing health challenges and leading to a higher chance of having diseases such as cancer. Adiposity, chronic low-grade inflammation, and hyperinsulinemia are essential factors of obesity that play a crucial role in tumor onset [11]. Even though some levels of fat are required for normal body function, patients with obesity tend to have an abundance of visceral fat [12] and excessive fat can lead to serious health problems including long-lasting inflammation. Additionally, obesity can also lead to elevated levels of insulin, insulin-like growth factor, and sex hormones, which contribute to the development of cancer [13]. The risk of cancer increases with the more excess weight a person gains and the longer a person is overweight.
Obesity can be classified according to metabolic phenotypes into four phenotypes: Metabolically unhealthy non-obese (MUNO), Metabolically unhealthy obese (MUO), Metabolically healthy non-obese (MHNO), and Metabolically healthy obese (MHO) [14]. (Figure 2) Compared with individuals with MUO, patients with MHO are characterized by lower liver and visceral fat, but higher subcutaneous leg fat content, greater cardiorespiratory fitness and physical activity, insulin sensitivity, lower levels of inflammatory markers, and normal adipose tissue function [15].
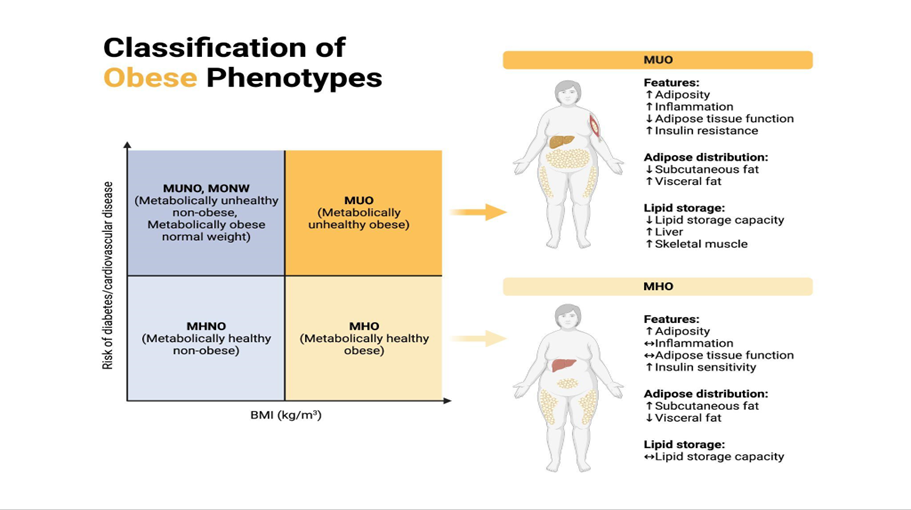
Figure 2. Classification of obese phenotypes with demonstrations of metabolically healthy and unhealthy obese.
Moreover, obesity can lead to difficulties in the treatment of cancer. For instance, obesity may hamper the treatment of endometrioid endometrial cancer (EEC) patients by external beam radiation therapy (EBRT) due to the difficulty in locating the tumors potentially causing the danger of under-dose to targets or over-dose to organs [16].
In obesity, the levels of various tumor suppressor proteins are decreased. TP53, a tumor suppressor protein, is inherently unstable within cells; however, its stability can be enhanced through phosphorylation by AMP-activated protein kinase (AMPK), an enzyme activated by adiponectin [17]. Consequently, a decline in adiponectin levels in obesity may lead to a reduction in TP53 concentration [17]. Contrary to previous findings that obesity could cause a decrease in TP53, there are also claims that in obesity, TP53 levels may increase, which can potentially worsen the release of inflammatory cytokines [17]. Nevertheless, the change of TP53 caused by obesity certainly relates to the formation of tumors.
3.1. Colorectal Cancer and Obesity
Colorectal cancer (CRC) is the third most common cancer in the US with an annual increase of 1% to 2% starting from the mid-1990s among individuals under the age of 50 [18]. There is a strong connection between obesity and CRC as excess body fat can increase the chance of an individual having cancer of the colon and rectum [19]. According to the American Cancer Society (ACS), the risk factors of colorectal cancer include being overweight or obese, having a bad diet, and lack of exercise [20]. Sex-specific MR analysis conducted by Bull, et al. [21] demonstrated that higher BMI (per 4.2 kg/m2) in men was associated with 1.23 times higher CRC odds; and among women, higher BMI (per 5.2 kg/m2) was associated with 1.09 times higher CRC odds.
Obesity can potentially increase the chance of the occurrence of second cancer for cancer survivors. According to research conducted by Gibson et al. [22], which used Cox proportional hazards regression models to examine associations between baseline (prediagnostic) BMI and risk of second obesity-associated cancers (postmenopausal breast, kidney, pancreas, esophageal adenocarcinoma, endometrium) in CRC survivors, and compared the associations to those for first obesity-associated cancers in the full cohort, CRC survivors who were overweight or obese before their diagnosis faced a higher risk of developing second obesity-associated cancers compared to survivors with a normal weight, indicating that the elevated risk of second cancers in colorectal cancer survivors might be attributed to a higher prevalence of overweight or obesity rather than an increased vulnerability in this population when compared to the general public [22].
3.2. Breast cancer and obesity
Breast cancer affects over 250,000 women in the US each year [23]. The two most common kinds of breast cancer are invasive ductal carcinoma and invasive lobular carcinoma [24]. Breast cancer is common among women who are overweight or obese by having higher levels of insulin, which triggers rapid cell division and can cause cells to lose control of their DNA regulator genes [25]. Consequently, obese women face an elevated risk of developing breast cancer which can be influenced by having a greater amount of adipose tissue and attributed to higher estrogen levels [26] produced by the adipose tissue [27]. Estrogen can serve as a catalyst for the growth of cancer cells. Estrogen stimulates the division and proliferation of breast tissue, increasing the likelihood of mutations that can lead to the development of cancer [28]. However recent studies done by the Harvard University suggested that estrogen is a more central character in cancer genesis because it directly alters how cells repair their DNA [28].
3.3. Liver cancer and obesity
The liver is one of the most common sites for cancer metastasis which is responsible for almost 25% of all cases [29]. According to a study done by Larsson, et al., people who are overweight and obese have a nearly 2-fold increased risk of liver cancer compared with people of normal weight [30]. In fact, by 2035, it is estimated that 20% of liver cancer cases globally will be attributable to having a high body mass index [31]. Obesity is linked to a higher risk of nonalcoholic fatty liver disease (NAFLD) [32] which is characterized by steatosis when the liver's uptake and synthesis of fatty acids exceed their oxidation and export as triglycerides within VLDL [32]. Obesity-related NAFLD links to liver inflammation, leading to an increase in the production of different cytokines and adipokines, which have been implicated in hepatocarcinogenesis [33]. According to a mice study, extracellular vesicles (EVs), encouraged colorectal cancer to grow in the liver and prevented immune cells from attacking metastatic tumors in the liver by launching a cascade of actions through three microRNAs that helped the cells form and develop into tumors [34]. Compared to mice with livers that could make EVs, mice that are genetically engineered to lack the ability to make EVs in their livers have colorectal cancer cells forming far fewer metastatic liver tumors [34].
3.4. Diabetes and obesity
Obesity is often accompanied by hyperglycemia [35]. Inflammations occur during obesity by pro-inflammatory molecules such as TNF-α released by white adipose tissue (WAT) macrophages that directly disrupt insulin signaling and can also lead to the development of insulin resistance (IR) and ultimately type 2 diabetes (T2D) [36]. Hyperglycemia can provide cells with more energy for dividing and affects growth factor secretion [31]. T2D has been linked to an increase in cases of obesity-related cancers including colorectal, hepatic, pancreatic, breast, and endometrial [31]. People with diabetes have a greater risk of developing certain cancers, diabetic women have a 27% greater chance of developing cancer than healthy women, and diabetic men are 19% more likely to develop cancer than healthy men [37]. Insulin sensitivity, influenced by body fat distribution, is associated with BMI regardless of weight gain, while lean individuals exhibit varying insulin sensitivity due to differences in fat distribution, with greater peripheral fat distribution associated with higher insulin sensitivity compared to central fat distribution in the abdomen and chest [38]. Obese individuals have elevated levels of several substances, such as non-esterified fatty acids, glycerol, hormones, cytokines, pro-inflammatory markers, and other factors that contribute to insulin resistance [38]. Insulin and C-peptide, which are crucial growth factors for colonic epithelial cells, are recognized as mitogens of tumor cells [39]. Hyperinsulinemia, a characteristic of metabolic diseases like type 2 diabetes, facilitates epithelial tumorigenesis by disrupting cell competition [40]. Through Drosophila genetic experiments conducted by Sabaki, et al., heterozygosity for the insulin receptor substrate chico enables oncogenic scribble (SCRIB – Scribble Planar Cell Polarity Protein) mutant cells to evade cell competition and progress into tumors [40]. Although the direct mechanism between insulin resistance and inflammation in the body remains unknown, in individuals with diabetes and insulin resistance, inflammation markers, such as tumor necrosis factor-α (TNF), interleukin-6 (IL-6), IL-8, and C-reactive protein (CRP) have been observed to be elevated, indicating the presence of inflammation [41] which can potentially cause cancer.
3.5. Obesity and inflammation
Inflammation is a complex defense mechanism employed by an organism to shield itself from harmful stimuli and initiate the recovery process. Normally, inflammation subsides promptly, but it can become chronic when the initial cause persists or remains unresolved. Individuals who are obese often experience a notable rise about two to three times in the levels of immune factors in their blood plasma, including TNF-α, Interleukin (IL)-6, monocyte chemoattractant protein (MCP)-1, CRP, and various others than those found in non-obese individuals [35].
The adipose tissue can be divided into two major types: brown adipose tissue and WAT (white adipose tissue) with different distributions (Figure 3) [42]. The development of obesity depends not only on calorie intake but on the balance between adipose tissue distribution [43]. Brown adipose tissues help regulate the body temperature in colder conditions and help store energy and calories [44], and WAT is specialized for energy storage [43].
Figure 3. Distribution of white and brown adipose tissues in the human body.
The tumor microenvironment is adapted primarily by inflammatory cells, and this environment plays a crucial role in promoting the growth, survival, and motility of cancer cells. The primary source of obesity-related inflammation is WAT, which acts as an active endocrine organ by producing and releasing a variety of cytokines, hormones, and other substances called “adipokines” [36]. In the presence of metabolic stress, adipocytes produce inflammatory mediators and chemotactic molecules such as monocyte chemoattractant protein (MCP)-1, which play a role in the recruitment and activation of immune cells particularly macrophages (Mφ) and T lymphocytes that contribute to the persistence of inflammation within WAT [35]. Inflammation has been shown to promote mutagenesis, tissue damage, and ultimately carcinogenesis [45]. In addition, cancer cells exploit certain signaling molecules in the innate immune system, such as selectins, chemokines, and their receptors, to promote cancer invasion, migration, and spread to other parts of the body [46]. When inflammation occurs in the body, reactive oxygen and nitrogen species (RONS) are produced to battle pathogens and to vitalize tissue repair and regeneration; however, these chemicals can also damage DNA, which in turn can promote cancer through the mutations in the DNA sequences [45]. Additionally, RONS can interfere with the DNA repair mechanisms by reducing their efficacy [45]. Furthermore, damage signaling and cytotoxicity can promote inflammation, creating a loop of inflammation and cellular response to DNA damage to cause inflammation [47].
3.6. Obesity and Cancer Metastasis
Obesity can influence cancer metastasis. Metastasis attributes to over 90% of cancer mortality [48]. The process of cancer metastasis begins with the development of a tumor, which then progresses through stages of localized invasion, intravasation, and extravasation. Eventually, this culminates in the formation of micrometastasis and the subsequent development of macrometastasis. Cases of prostate, pancreatic, breast cancer, and esophageal adenocarcinoma, are similar, as these cancers are situated close to adipose tissue depots [49]. The adjacent adipose tissue creates an optimal microenvironment that fosters tumor growth, progression, and metastasis where adipocytes secrete adipokines, fatty acids, and other soluble factors that support tumor cells, while immune cells infiltrate the tumor region [49]. Obese adipose tissue exhibits numerous characteristics that closely resemble the tumor microenvironment that supports cancer metastasis [49] (Figure 4).
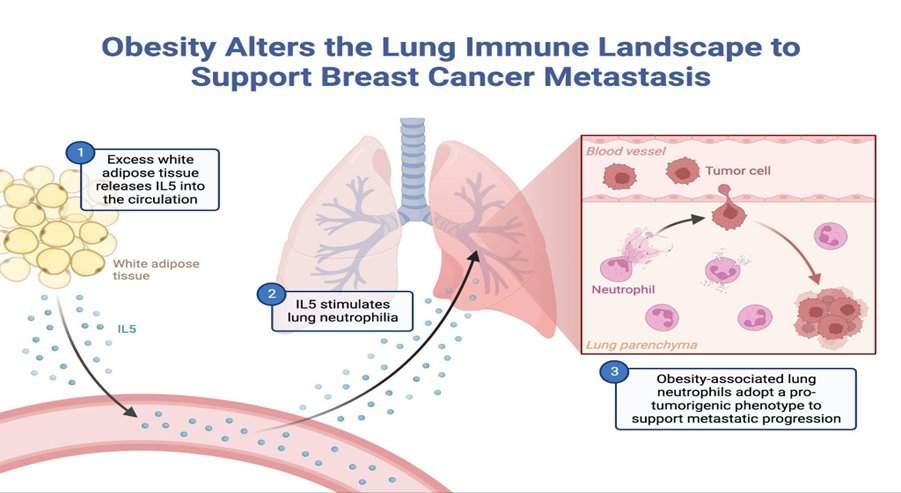
Figure 4. Schematic representation of the proposed mechanism associated with obesity-associated lung neutrophilia. IL5 derived from adipose tissue signals to IL5rα cells, causing their expansion and upregulation of Csf2. This creates an environment supporting neutrophilia in the circulation and the lungs. Lung neutrophils then adopt pro-tumorigenic transcriptional signatures and ultimately facilitate metastatic progression.
3.7. Resolutions for Obesity
There are possible solutions to resolve the obesity crisis. WHO recommends nations collaborate to establish an improved food environment that ensures universal access to and affordability of nutritious meals by regulating the promotion of high-fat, high-sugar, and high-salt food and beverages to children, implementing taxes on sugary drinks, enhancing the availability of affordable and healthy food options, and allocating areas for secure walking, cycling, and recreational activities. At the same time, schools should assist families in teaching children healthy behaviors right from the start [50]. Epidemiological studies have shown that the quantity and quality of food pregnant females consume during pregnancy affects birthweight and, in turn, the likelihood of individuals born for small or large gestational ages being obese as adults [51]. Therefore, providing nutritious food to pregnant women can help to reduce obesity. The proper method of decreasing the obesity issue is understanding the potential consequences of an unhealthy diet and knowledge about how to live a healthier one.
4. Conclusion
Obesity has become one of the major epidemics worldwide in the past few decades, leading to diseases and costing a considerable burden on the global medical system while being entirely preventable. There are strong correlations between obesity and various types of cancers or carcinogenic conditions such as inflammation, type II diabetes, or NAFLD. Obesity has become an issue only in recent years; therefore, the current healthcare system still needs further data to adjust to obese individuals in cancer treatment and detection.
References
[1]. CDC. Adult Obesity Facts | Overweight and Obesity. Retrieved Aug 18. 2023 from https://www.cdc.gov/obesity/data/adult.html.
[2]. World Health Organization (WHO). Obesity. Retrieved Aug 18. 2023 from https://www.who.int/health-topics/obesity#tab=tab_1.
[3]. CDC. Why It Matters | Overweight & Obesity. Retrieved Aug 18. 2023 from https://www.cdc.gov/obesity/about-obesity/why-it-matters.html.
[4]. World Obesity. Prevalence of Obesity. Retrieved Aug 18. 2023 from https://www.worldobesity.org/about/about-obesity/prevalence-of-obesity#:~:text=The%20World%20Obesity%20Federation%20estimates,2030%20unless%20we%20act%20soon.
[5]. CDC. Health Effects of Overweight and Obesity. Retrieved Aug 18. 2023 from https://www.cdc.gov/healthyweight/effects/index.html.
[6]. Harvard T.H. Chan School of Public Health. Obesity Preventable Sources. Retrieved Aug 18. 2023 from https://www.hsph.harvard.edu/obesity-prevention-source/obesity-causes/#:~:text= Many%20factors%20influence%20body%20weight,food%20and%20physical%20activit y%20environment.
[7]. World Cancer Day. What is Cancer? Retrieved Aug 18. 2023 from https://www.worldcancerday.org/what-cancer.
[8]. Pati S, Irfan W, Jameel A, Ahmed S, Shahid RK. 2023. Obesity and Cancer: A Current Overview of Epidemiology, Pathogenesis, Outcomes, and Management. Cancers (Basel). 15, 2(January 2023), 485. https://doi.org/10.3390/cancers15020485.
[9]. Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. 2003. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 348, 17, 1625-1638. https://doi.org/10.1056/NEJMoa021423.
[10]. Hanahan Douglas and Weinberg AR. 2011. Hallmarks of Cancer: The Next Generation. Cell. 144, 5(March 2011), 646-674. https://doi.org/10.1016/j.cell.2011.02.013.
[11]. Crudele L, Piccinin E, Moschetta A. 2021. Visceral Adiposity and Cancer: Role in Pathogenesis and Prognosis. Nutrients. 13, 6, 2101. https://doi.org/10.3390/nu13062101.
[12]. Cleveland Clinic. Visceral Fat. Retrieved Aug 18. 2023 from https://my.clevelandclinic.org/health/diseases/24147-visceral-fat.
[13]. CDC. Obesity and Cancer. Retrieved Aug 18. 2023 from https://www.cdc.gov/ cancer/obesity/index.htm.
[14]. Heshmat R, Hemati Z, Payab M, Hamzeh SS, Motlagh ME, Shafiee G, Taheri M, Ziaodini H, Qorbani M, Kelishadi R. 2018. Prevalence of different metabolic phenotypes of obesity in Iranian children and adolescents: the CASPIAN V study. J Diabetes Metab Disord. 17, 211-221. https://doi.org/10.1007/s40200-018-0363-5.
[15]. Matthias Blüher. 2020. Metabolically Healthy Obesity. Endocrine Reviews. 41, 3(June 2020). https://doi.org/10.1210/endrev/bnaa004.
[16]. Moszyńska-Zielińska, M., Chałubińska-Fendler, J., Gottwald, L., Żytko, L., Bigos, E., & Fijuth, J. 2014. Does obesity hinder radiotherapy in endometrial cancer patients? The implementation of new techniques in adjuvant radiotherapy – focus on obese patients. Menopause Review/Przegląd Menopauzalny. 13, 96-100. https://doi.org/10.5114/pm.2014.42710.
[17]. Shanmugalingam T, Bosco C, Ridley AJ, Van Hemelrijck M. 2016. Is there a role for IGF-1 in the development of second primary cancers? Cancer Med. 5, 11(November 2016), 3353-3367. https://doi.org/10.1002/cam4.871.
[18]. American Cancer Society. Key Statistics for Colorectal Cancer. Retrieved Aug 18. 2023 from https://www.cancer.org/cancer/types/colon-rectal-cancer/about/key-statistics.html#:~:text=Excluding%20skin%20cancers%2C%20colorectal%20cancer,new%20cases%20of%20colon%20cancer
[19]. World Cancer Research Fund International. Are metabolites associated with obesity causing colorectal cancer? Retrieved Aug 18. 2023 from https://www.wcrf.org/researchwefund/are-metabolites-associated-with-obesity-causing-colorectal-cancer/#:~:text=Obesity%20is%20characterised%20by%20higher,collectively%20known%20as%20colorectal%20cancer).
[20]. American Cancer Society. Colorectal Cancer Risk Factors. Retrieved Aug 18. 2023 from https://www.cancer.org/cancer/types/colon-rectal-cancer/causes-risks-prevention/risk-factors.html.
[21]. Bull, C.J., Bell, J.A., Murphy, N. et al. 2020. Adiposity, metabolites, and colorectal cancer risk: Mendelian randomization study. BMC Med. https://doi.org/10.1186/s12916-020-01855-9.
[22]. Gibson TM, Park Y, Robien K, Shiels MS, Black A, Sampson JN, Purdue MP, Freeman LE, Andreotti G, Weinstein SJ, Albanes D, Fraumeni JF Jr, Curtis RE, Berrington de Gonzalez A, Morton LM. 2014. Body mass index and risk of second obesity-associated cancers after colorectal cancer: a pooled analysis of prospective cohort studies. J Clin Oncol. https://doi.org/10.1200/JCO.2014.56.8444.
[23]. Tufail M, Cui J, Wu C. 2022. Breast cancer: molecular mechanisms of underlying resistance and therapeutic approaches. Am J Cancer Res. Retrieved Aug 18. 2023 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9360230/.
[24]. CDC. What is Breast Cancer? Retrieved Aug 18. 2023 from https://www.cdc.gov/ cancer/breast/basic_info/what-is-breast-cancer.htm.
[25]. Mueller Miles. 2022.The Insulin/Cancer Connection. Retrieved Aug 18. 2023 from https://www.lifeextension.com/magazine/2016/6/the-insulin-cancer-connection#:~:text=Research%20has%20shown%20that%20higher,of%20their%20DNA%20regulator%20genes.
[26]. Simon Stacy. 2018. How Your Weight May Affect Your Risk of Breast Cancer. Retrieved Aug 18. 2023 from https://www.cancer.org/cancer/latest-news/how-your-weight-affects-your-risk-of-breast-cancer.html#:~:text=For%20women%2C%20being%20overweight%20or, cancer%20by%20raising%20estrogen%20levels.
[27]. Uhomoibhi TO, Okobi TJ, Okobi OE, Koko JO, Uhomoibhi O, Igbinosun OE, Ehibor UD, Boms MG, Abdulgaffar RA, Hammed BL, Ibeanu C, Segun EO, Adeosun AA, Evbayekha EO, Alex KB. 2022. High-Fat Diet as a Risk Factor for Breast Cancer: A Meta-Analysis. Cureus. 14, 12. https://doi.org/10.7759/cureus.32309.
[28]. Ekaterina Pesheva. 2023. Potential path to better testing in findings that identify hormone as ‘a catalyst and a cause’ in disease. Retrieved Aug 18. 2023 from https://news. harvard.edu/gazette/story/2023/05/estrogen-a-more-powerful-breast-cancer-culprit-than-we-realized/.
[29]. Griscom JT, Wolf PS. 2023. Liver Metastasis. Treasure Island (FL): StatPearls Publishing. Retrieved Aug 18.2023 from https://www.ncbi.nlm.nih.gov/books/NBK553118/.
[30]. Larsson, S., Wolk, A. 2007. Overweight, obesity and risk of liver cancer: a meta-analysis of cohort studies. Br J Cancer. 97, 1005–1008. https://doi.org/10.1038/sj.bjc.6603932.
[31]. Harris, B.H.L., Macaulay, V.M., Harris, D.A. et al. 2022.Obesity: a perfect storm for carcinogenesis. Cancer Metastasis Rev. 41, 491–515. https://doi.org/10.1007/s10555-022-10046-2.
[32]. Elisa Fabbrini, Shelby Sullivan, and Samuel Klein. 2010. Obesity and Nonalcoholic Fatty Liver Disease: Biochemical, Metabolic and Clinical Implications. Hepatology. 51, 2(Febuary 2021), 679-689. https://doi.org/10.1002/hep.23280.
[33]. Sun B, Karin M. 2012. Obesity, inflammation, and liver cancer. J Hepatol. 56, 3(March 2012), 704-713. https://doi.org/10.1016/j.jhep.2011.09.020.
[34]. Nadia Jaber. 2023. How Fatty Liver Disease Helps Cancer Thrive in the Liver. Retrieved Aug 18. 2023 from https://www.cancer.gov/news-events/cancer-currents-blog/2023/fatty-liver-disease-cancer-metastasis.
[35]. Martyn JA, Kaneki M, Yasuhara S. 2008. Obesity-induced insulin resistance and hyperglycemia: etiologic factors and molecular mechanisms. Anesthesiology. 109, 1(July 2008), 137-148. https://doi.org/10.1097/ALN.0b013e3181799d45.
[36]. Park YM, Myers M, Vieira-Potter VJ. 2014. Adipose tissue inflammation and metabolic dysfunction: role of exercise. Mo Med. 111, 1(Jan-Feb 2014), 65-72. Retrieved Aug 18. 2023 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6179510/.
[37]. City of Hope. 2021. Cancer and diabetes: The connection is in your DNA Retrieved Aug 18. 2023 from https://www.cancercenter.com/community/blog/2021/05/diabetes-cancer#:~:text=The% 20hormone%20insulin%20used%20to,another%20risk%20factor%20for% 20cancer.
[38]. Al-Goblan AS, Al-Alfi MA, Khan MZ. 2014. Mechanism linking diabetes mellitus and obesity. Diabetes Metab Syndr Obes. 7, 587-591. https://doi.org/10.2147/DMSO.S67400.
[39]. Jung Won Park, Soo Yeon Chang, Joon Seok Lim, Soo Jung Park, Jae Jun Park, Jae Hee Cheon, Won Ho Kim, and Tae Il Kim. 2021. Impact of Visceral Fat on Survival and Metastasis of Stage III Colorectal Cancer. Gut Liver. 17, 4(January 2022). https://doi.org/10.5009/gnl20266.
[40]. Sanaki Y, Nagata R, Kizawa D, Léopold P, Igaki T. Hyperinsulinemia Drives Epithelial Tumorigenesis by Abrogating Cell Competition. Dev Cell. 53, 4(May 2020), 379-389. https://doi.org/10.1016/j.devcel.2020.04.008
[41]. Carl de Luca and Jerrold M. Olefsky. 2007. Inflammation and Insulin Resistance. FEBS Letters. 582, 1(November 2007), 97-105. https://doi.org/10.1016/j.febslet.2007.11.057.
[42]. Mohammed S. Ellulu, Ismail Patimah, Huzwah Khaza’ai, Asmah Rahmat, and Yehia Abed. 2017. Obesity and inflammation: the linking mechanism and the complications. J. Arch Med Sci 13, 4 (April 2017), 851-863. https://doi.org/10.5114/aoms.2016.58928.
[43]. Stephane Gesta, Yu-hua Tseng, C. Ronald Kahn. 2007. Developmental Origin of Fat: Tracking Obesity to Its Source. J. Cells 131, 2 (October 2007), 242-256. https://doi.org/10.1016/j.cell.2007.10.004.
[44]. Cleveland Clinics. Brown Fat. Retrieved Aug 16. 2023 from https://my. clevelandclinic.org/health/body/24015-brown-fat#:~:text=Brown%20fat% 20(brown%20adipose%20tissue,body%20compared%20to%20white%20fat.
[45]. Jennifer Kay, Elina Thadhani, Leona Samson, Bevin Engelward. 2019. Inflammation-induced DNA damage, mutations and cancer. J. dnarep. 83, 102673(October 2019). https://doi.org/10.1016/j.dnarep.2019.102673.
[46]. Lisa M. Coussensand Zena Werb. 2002. Inflammation and Cancer. Nature. 420, 860-857. https://doi.org/10.1038/nature01322.
[47]. Daniela F. Quail, Oakley C. Olson, Priya Bhardwaj, Logan A. Walsh, Leila Akkari, Marsha L. Quick, I-Chun Chen, Nils Wendel, Nir Ben-Chetrit, Jeanne Walker, Peter R. Holt, Andrew J. Dannenberg & Johanna A. Joyce. 2017. Obesity alters the lung myeloid cell landscape to enhance breast cancer metastasis through IL5 and GM-CSF. Nat Cell Bio. 19(2007), 974-987. https://doi.org/10.1038/ncb3578.
[48]. Thomas N. Seyfried and Leanne C. Huysentruyt. 2013. On the Origin of Cancer Metastasis. Begell. 18, 1-2(2013), 43-73. https://doi.org/10.1615/CritRevOncog.v18.i1-2.40.
[49]. Stephanie Annett, Gillian Moore, and Tracy Robson. 2020. Obesity and Cancer Metastasis: Molecular and Translational Perspectives. Cancers 2020. 12, 3798. https://doi. org/10.3390/cancers12123798.
[50]. World Health Organization. 2020. World Obesity Day 2022 – Accelerating action to stop obesity. Retrieved Aug 16. 2023 from https://www.who.int/news/item/04-03-2022-world-obesity-day-2022-accelerating-action-to-stop-obesity.
[51]. Sebastian D. Parlee and Ormond A. MacDougald. 2013. Maternal Nutrition and Risk of Obesity in Offspring: The Trojan Horse of Developmental Plasticity. Elsevier Sci. 1842, 3(July 2013), 495-506. https://doi.org/10.1016/j.bbadis.2013.07.007.
Cite this article
You,X. (2023). Investigating the relationship between obesity and cancer. Theoretical and Natural Science,8,230-239.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 2nd International Conference on Modern Medicine and Global Health
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. CDC. Adult Obesity Facts | Overweight and Obesity. Retrieved Aug 18. 2023 from https://www.cdc.gov/obesity/data/adult.html.
[2]. World Health Organization (WHO). Obesity. Retrieved Aug 18. 2023 from https://www.who.int/health-topics/obesity#tab=tab_1.
[3]. CDC. Why It Matters | Overweight & Obesity. Retrieved Aug 18. 2023 from https://www.cdc.gov/obesity/about-obesity/why-it-matters.html.
[4]. World Obesity. Prevalence of Obesity. Retrieved Aug 18. 2023 from https://www.worldobesity.org/about/about-obesity/prevalence-of-obesity#:~:text=The%20World%20Obesity%20Federation%20estimates,2030%20unless%20we%20act%20soon.
[5]. CDC. Health Effects of Overweight and Obesity. Retrieved Aug 18. 2023 from https://www.cdc.gov/healthyweight/effects/index.html.
[6]. Harvard T.H. Chan School of Public Health. Obesity Preventable Sources. Retrieved Aug 18. 2023 from https://www.hsph.harvard.edu/obesity-prevention-source/obesity-causes/#:~:text= Many%20factors%20influence%20body%20weight,food%20and%20physical%20activit y%20environment.
[7]. World Cancer Day. What is Cancer? Retrieved Aug 18. 2023 from https://www.worldcancerday.org/what-cancer.
[8]. Pati S, Irfan W, Jameel A, Ahmed S, Shahid RK. 2023. Obesity and Cancer: A Current Overview of Epidemiology, Pathogenesis, Outcomes, and Management. Cancers (Basel). 15, 2(January 2023), 485. https://doi.org/10.3390/cancers15020485.
[9]. Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. 2003. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 348, 17, 1625-1638. https://doi.org/10.1056/NEJMoa021423.
[10]. Hanahan Douglas and Weinberg AR. 2011. Hallmarks of Cancer: The Next Generation. Cell. 144, 5(March 2011), 646-674. https://doi.org/10.1016/j.cell.2011.02.013.
[11]. Crudele L, Piccinin E, Moschetta A. 2021. Visceral Adiposity and Cancer: Role in Pathogenesis and Prognosis. Nutrients. 13, 6, 2101. https://doi.org/10.3390/nu13062101.
[12]. Cleveland Clinic. Visceral Fat. Retrieved Aug 18. 2023 from https://my.clevelandclinic.org/health/diseases/24147-visceral-fat.
[13]. CDC. Obesity and Cancer. Retrieved Aug 18. 2023 from https://www.cdc.gov/ cancer/obesity/index.htm.
[14]. Heshmat R, Hemati Z, Payab M, Hamzeh SS, Motlagh ME, Shafiee G, Taheri M, Ziaodini H, Qorbani M, Kelishadi R. 2018. Prevalence of different metabolic phenotypes of obesity in Iranian children and adolescents: the CASPIAN V study. J Diabetes Metab Disord. 17, 211-221. https://doi.org/10.1007/s40200-018-0363-5.
[15]. Matthias Blüher. 2020. Metabolically Healthy Obesity. Endocrine Reviews. 41, 3(June 2020). https://doi.org/10.1210/endrev/bnaa004.
[16]. Moszyńska-Zielińska, M., Chałubińska-Fendler, J., Gottwald, L., Żytko, L., Bigos, E., & Fijuth, J. 2014. Does obesity hinder radiotherapy in endometrial cancer patients? The implementation of new techniques in adjuvant radiotherapy – focus on obese patients. Menopause Review/Przegląd Menopauzalny. 13, 96-100. https://doi.org/10.5114/pm.2014.42710.
[17]. Shanmugalingam T, Bosco C, Ridley AJ, Van Hemelrijck M. 2016. Is there a role for IGF-1 in the development of second primary cancers? Cancer Med. 5, 11(November 2016), 3353-3367. https://doi.org/10.1002/cam4.871.
[18]. American Cancer Society. Key Statistics for Colorectal Cancer. Retrieved Aug 18. 2023 from https://www.cancer.org/cancer/types/colon-rectal-cancer/about/key-statistics.html#:~:text=Excluding%20skin%20cancers%2C%20colorectal%20cancer,new%20cases%20of%20colon%20cancer
[19]. World Cancer Research Fund International. Are metabolites associated with obesity causing colorectal cancer? Retrieved Aug 18. 2023 from https://www.wcrf.org/researchwefund/are-metabolites-associated-with-obesity-causing-colorectal-cancer/#:~:text=Obesity%20is%20characterised%20by%20higher,collectively%20known%20as%20colorectal%20cancer).
[20]. American Cancer Society. Colorectal Cancer Risk Factors. Retrieved Aug 18. 2023 from https://www.cancer.org/cancer/types/colon-rectal-cancer/causes-risks-prevention/risk-factors.html.
[21]. Bull, C.J., Bell, J.A., Murphy, N. et al. 2020. Adiposity, metabolites, and colorectal cancer risk: Mendelian randomization study. BMC Med. https://doi.org/10.1186/s12916-020-01855-9.
[22]. Gibson TM, Park Y, Robien K, Shiels MS, Black A, Sampson JN, Purdue MP, Freeman LE, Andreotti G, Weinstein SJ, Albanes D, Fraumeni JF Jr, Curtis RE, Berrington de Gonzalez A, Morton LM. 2014. Body mass index and risk of second obesity-associated cancers after colorectal cancer: a pooled analysis of prospective cohort studies. J Clin Oncol. https://doi.org/10.1200/JCO.2014.56.8444.
[23]. Tufail M, Cui J, Wu C. 2022. Breast cancer: molecular mechanisms of underlying resistance and therapeutic approaches. Am J Cancer Res. Retrieved Aug 18. 2023 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9360230/.
[24]. CDC. What is Breast Cancer? Retrieved Aug 18. 2023 from https://www.cdc.gov/ cancer/breast/basic_info/what-is-breast-cancer.htm.
[25]. Mueller Miles. 2022.The Insulin/Cancer Connection. Retrieved Aug 18. 2023 from https://www.lifeextension.com/magazine/2016/6/the-insulin-cancer-connection#:~:text=Research%20has%20shown%20that%20higher,of%20their%20DNA%20regulator%20genes.
[26]. Simon Stacy. 2018. How Your Weight May Affect Your Risk of Breast Cancer. Retrieved Aug 18. 2023 from https://www.cancer.org/cancer/latest-news/how-your-weight-affects-your-risk-of-breast-cancer.html#:~:text=For%20women%2C%20being%20overweight%20or, cancer%20by%20raising%20estrogen%20levels.
[27]. Uhomoibhi TO, Okobi TJ, Okobi OE, Koko JO, Uhomoibhi O, Igbinosun OE, Ehibor UD, Boms MG, Abdulgaffar RA, Hammed BL, Ibeanu C, Segun EO, Adeosun AA, Evbayekha EO, Alex KB. 2022. High-Fat Diet as a Risk Factor for Breast Cancer: A Meta-Analysis. Cureus. 14, 12. https://doi.org/10.7759/cureus.32309.
[28]. Ekaterina Pesheva. 2023. Potential path to better testing in findings that identify hormone as ‘a catalyst and a cause’ in disease. Retrieved Aug 18. 2023 from https://news. harvard.edu/gazette/story/2023/05/estrogen-a-more-powerful-breast-cancer-culprit-than-we-realized/.
[29]. Griscom JT, Wolf PS. 2023. Liver Metastasis. Treasure Island (FL): StatPearls Publishing. Retrieved Aug 18.2023 from https://www.ncbi.nlm.nih.gov/books/NBK553118/.
[30]. Larsson, S., Wolk, A. 2007. Overweight, obesity and risk of liver cancer: a meta-analysis of cohort studies. Br J Cancer. 97, 1005–1008. https://doi.org/10.1038/sj.bjc.6603932.
[31]. Harris, B.H.L., Macaulay, V.M., Harris, D.A. et al. 2022.Obesity: a perfect storm for carcinogenesis. Cancer Metastasis Rev. 41, 491–515. https://doi.org/10.1007/s10555-022-10046-2.
[32]. Elisa Fabbrini, Shelby Sullivan, and Samuel Klein. 2010. Obesity and Nonalcoholic Fatty Liver Disease: Biochemical, Metabolic and Clinical Implications. Hepatology. 51, 2(Febuary 2021), 679-689. https://doi.org/10.1002/hep.23280.
[33]. Sun B, Karin M. 2012. Obesity, inflammation, and liver cancer. J Hepatol. 56, 3(March 2012), 704-713. https://doi.org/10.1016/j.jhep.2011.09.020.
[34]. Nadia Jaber. 2023. How Fatty Liver Disease Helps Cancer Thrive in the Liver. Retrieved Aug 18. 2023 from https://www.cancer.gov/news-events/cancer-currents-blog/2023/fatty-liver-disease-cancer-metastasis.
[35]. Martyn JA, Kaneki M, Yasuhara S. 2008. Obesity-induced insulin resistance and hyperglycemia: etiologic factors and molecular mechanisms. Anesthesiology. 109, 1(July 2008), 137-148. https://doi.org/10.1097/ALN.0b013e3181799d45.
[36]. Park YM, Myers M, Vieira-Potter VJ. 2014. Adipose tissue inflammation and metabolic dysfunction: role of exercise. Mo Med. 111, 1(Jan-Feb 2014), 65-72. Retrieved Aug 18. 2023 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6179510/.
[37]. City of Hope. 2021. Cancer and diabetes: The connection is in your DNA Retrieved Aug 18. 2023 from https://www.cancercenter.com/community/blog/2021/05/diabetes-cancer#:~:text=The% 20hormone%20insulin%20used%20to,another%20risk%20factor%20for% 20cancer.
[38]. Al-Goblan AS, Al-Alfi MA, Khan MZ. 2014. Mechanism linking diabetes mellitus and obesity. Diabetes Metab Syndr Obes. 7, 587-591. https://doi.org/10.2147/DMSO.S67400.
[39]. Jung Won Park, Soo Yeon Chang, Joon Seok Lim, Soo Jung Park, Jae Jun Park, Jae Hee Cheon, Won Ho Kim, and Tae Il Kim. 2021. Impact of Visceral Fat on Survival and Metastasis of Stage III Colorectal Cancer. Gut Liver. 17, 4(January 2022). https://doi.org/10.5009/gnl20266.
[40]. Sanaki Y, Nagata R, Kizawa D, Léopold P, Igaki T. Hyperinsulinemia Drives Epithelial Tumorigenesis by Abrogating Cell Competition. Dev Cell. 53, 4(May 2020), 379-389. https://doi.org/10.1016/j.devcel.2020.04.008
[41]. Carl de Luca and Jerrold M. Olefsky. 2007. Inflammation and Insulin Resistance. FEBS Letters. 582, 1(November 2007), 97-105. https://doi.org/10.1016/j.febslet.2007.11.057.
[42]. Mohammed S. Ellulu, Ismail Patimah, Huzwah Khaza’ai, Asmah Rahmat, and Yehia Abed. 2017. Obesity and inflammation: the linking mechanism and the complications. J. Arch Med Sci 13, 4 (April 2017), 851-863. https://doi.org/10.5114/aoms.2016.58928.
[43]. Stephane Gesta, Yu-hua Tseng, C. Ronald Kahn. 2007. Developmental Origin of Fat: Tracking Obesity to Its Source. J. Cells 131, 2 (October 2007), 242-256. https://doi.org/10.1016/j.cell.2007.10.004.
[44]. Cleveland Clinics. Brown Fat. Retrieved Aug 16. 2023 from https://my. clevelandclinic.org/health/body/24015-brown-fat#:~:text=Brown%20fat% 20(brown%20adipose%20tissue,body%20compared%20to%20white%20fat.
[45]. Jennifer Kay, Elina Thadhani, Leona Samson, Bevin Engelward. 2019. Inflammation-induced DNA damage, mutations and cancer. J. dnarep. 83, 102673(October 2019). https://doi.org/10.1016/j.dnarep.2019.102673.
[46]. Lisa M. Coussensand Zena Werb. 2002. Inflammation and Cancer. Nature. 420, 860-857. https://doi.org/10.1038/nature01322.
[47]. Daniela F. Quail, Oakley C. Olson, Priya Bhardwaj, Logan A. Walsh, Leila Akkari, Marsha L. Quick, I-Chun Chen, Nils Wendel, Nir Ben-Chetrit, Jeanne Walker, Peter R. Holt, Andrew J. Dannenberg & Johanna A. Joyce. 2017. Obesity alters the lung myeloid cell landscape to enhance breast cancer metastasis through IL5 and GM-CSF. Nat Cell Bio. 19(2007), 974-987. https://doi.org/10.1038/ncb3578.
[48]. Thomas N. Seyfried and Leanne C. Huysentruyt. 2013. On the Origin of Cancer Metastasis. Begell. 18, 1-2(2013), 43-73. https://doi.org/10.1615/CritRevOncog.v18.i1-2.40.
[49]. Stephanie Annett, Gillian Moore, and Tracy Robson. 2020. Obesity and Cancer Metastasis: Molecular and Translational Perspectives. Cancers 2020. 12, 3798. https://doi. org/10.3390/cancers12123798.
[50]. World Health Organization. 2020. World Obesity Day 2022 – Accelerating action to stop obesity. Retrieved Aug 16. 2023 from https://www.who.int/news/item/04-03-2022-world-obesity-day-2022-accelerating-action-to-stop-obesity.
[51]. Sebastian D. Parlee and Ormond A. MacDougald. 2013. Maternal Nutrition and Risk of Obesity in Offspring: The Trojan Horse of Developmental Plasticity. Elsevier Sci. 1842, 3(July 2013), 495-506. https://doi.org/10.1016/j.bbadis.2013.07.007.