1. Introduction
Coronary atherosclerotic heart disease (CAD) is the most common cardiovascular disease globally and is the primary cause of mortality. The disease significantly risks individuals’ health and overall quality of life. Among these conditions, myocardial infarction is the most severe manifestation of this particular illness. Coronary angiography is widely accepted as the preferred approach for evaluating coronary artery disease. The available data about patients with a diagnosis of myocardial infarction who have had coronary angiography reveals that most of these patients show obstructive myocardial infarction. However, it is noteworthy that a small percentage of these patients, ranging from around 5% to 10%, do not show any coronary obstruction, which means coronary arteries show either normal or less than 50% stenosis in angiography, hence defining it as myocardial infarction with non-obstructive coronary arteries (MINOCA). MINOCA signifies the presence of inadequate coronary artery blood supply or direct myocardial dysfunction at the pathological level based on a common finding on coronary angiography: the absence of 50% coronary artery stenosis and no evidence of atherosclerotic plaque rupture. Developing a more precise understanding of the disease is crucial to get more accurate and comprehensive assessment and prediction of the diagnosis and prognosis of patients with MINOCA.
To enhance the precision of clinical outcomes for patients with MINOCA, multiple methods are produced to broaden their applicability to MINOCA. Within these approaches, cardiovascular magnetic resonance, specifically a form of magnetic resonance imaging, emerges as one of the more efficacious techniques for diagnosing and prognosis MINOCA. This technique enables a detailed examination of the heart’s morphology, structure and function through multiple sequences and parameters. The T1-weighted image provides valuable insights into the anatomical structure of the heart, while the T2-weighted image shows a remarkable sensitivity toward detecting myocardial oedema. Besides, kinetic sequences offer a comprehensive depiction of dynamic behaviors of the heart. Lastly, late gadolinium enhancement technology serves as a way to effectively highlight fibrous or necrotic myocardium in patients. The development of CMR and the expansion of its therapeutic applications position itself as a pivotal tool in identifying and managing diverse cardiovascular conditions. The following contents centers on the role of CMR in the assessment and prediction of MINOCA.
2. Pathological manifestations of MINOCA and imaging features of cardiovascular magnetic resonance
On coronary angiography, individuals who have experienced myocardial infarction (MI) generally have notable narrowing of the epicardial coronary arteries, either with or without observable indications of impaired blood flow in the distal coronary regions. The predominant mechanism observed is intracoronary thrombosis after the rupture of an atherosclerotic plaque. Nevertheless, some people do not have the clinical manifestations of coronary artery disease (CAD) despite presenting histological evidence of the condition, which is called MINOCA. Patients presenting with MINOCA have a prevalence of less than 10% among cases of myocardial infarction. Moreover, patients with MINOCA tend to be younger than those with atherosclerotic acute coronary syndrome (ACS), with a higher proportion of female patients than males [1].
The initial symptoms of patients with MINOCA are similar to those of ACS patients, including chest discomfort, shortness of breath, arrhythmias and cardiac arrest. What’ s more, non-ST-segment elevation is its typical feature on the electrocardiography (ECG). When patients develop MINOCA in combination with coronary insufficiency, the main causes are classified into four major categories: epicardial coronary vasospasm, microvascular coronary artery dysfunction, spontaneous coronary artery dissection and coronary artery thrombosis, while non-coronary causes should take into account for various myocardial infections such as takotsubo syndrome (TTS) or stress cardiomyopathy (TCM) [1].
Coronary angiography, which is frequently used clinically to detect myocardial infarction, does not have the characteristic features that can predict MINOCA specifically, so an increasing number of additional tests are being used to explore their roles in the diagnosis and prognosis of MINOCA. For example, intravascular ultrasound and optical coherence tomography are used to determine the coronary aetiology of MINOCA, and some imaging techniques such as CMR and echocardiography show high quality in detecting heart integrity and function, which are essential for diagnosing MINOCA and directing its prognosis.
CMR, an MRI method of the heart, has the characteristics of multi-parametric, multi-planar, and multi-sequence imaging. Its high repeatability and excellent soft tissue resolution among other features provide wide range of utility in clinical medicine. Thus, it is currently the “gold standard” for noninvasive cardiac anatomy and function assessment. Several major methods are designed to accomplish CMR examination, including cardiac DTI, cine CMR imaging and quantitative parametric imaging, which contains T1, T2 mapping and extracellular volume fraction (ECV). The following steps demonstrate the general standard process for a CMR examination on clinic patients: positioning the patient’s heart is the first step during the whole examination, before a cardiac and cine scans are carried out in sequence. Later, the patient is given a contrast agent and a myocardial perfusion scan. After this scan, the contrast agent is injected into patients again and finally a delayed enhancement MR scan is carried out. Cardiac T1, T2 mapping and DTI techniques enable assessment of water molecule diffusion motion and cardiac tissue T1 and T2 levels, which exactly respond to cellular and molecular myocardial microstructural changes [2]. To detect lesions in the periphery of nonischemic cardiomyopathy and focal myocardial fibrosis, T1 mapping can identify varying degrees of interstitial fibrotic changes. T2 mapping is primarily utilized to evaluate myocardial fibrosis and also able to mainly assess myocardial edema and detect diseases like acute myocardial infarction or myocarditis in the early time. What’ s more, it is a good way to clarify the extent and magnitude of edema for early diagnosis with T2 [2]. Contrarily, cine-CMR imaging concentrates on gathering data regarding cardiac structure, valve and ventricular wall motion, particularly left ventricular functional parameters, and it usually offers proof of changes in myocardial micro-structure in heart illness.
Delineation of left ventricular segmentation and corresponding blood supply in CMR imaging results in patients with MINOCA is based on the American Heart Association 17-segment model, and the area of myocardial infarction is graded as follows: Grade 0: normal, 0 point; Grade I: ≤25%, 1 point; Grade II: 26% to 50%, 2 points; Grade III: 51% to 75%, 3 points; Grade IV ≥75%, 4 points [3]. CMR imaging characteristics of patients with MINOCA are shown to have the following four common features: (1) patients with MINOCA are younger, and the electrocardiogram is characterized by non-ST-segment elevation; (2) patients with MINOCA have smaller grades of myocardial infarct area, degrees of transmural penetration, less number of affected segments and better cardiac function; (3) myocardial infarction segments are mainly located in the anterior wall, anterior septal wall and inferior interseptal wall, which are all dominated by the left anterior descending coronary artery, this indicates that there is a higher likelihood of myocardial infarction controlled by the left anterior ascending coronary artery; (4) the degree of transmurality of myocardial infarction in patients with MINOCA is mainly Grade I, most of which are subendocardial myocardial infarctions [3].
3. Role of cardiovascular magnetic resonance in MINOCA diagnosis
Since the etiology of patients with MINOCA is varied and can be linked to several pathological disorders, therapy strategies for MINOCA increasingly emphasise the significance of the early clinical detection of MINOCA. In some meta analysis, it has been proven that CMR can differentiate normal myocardium from myocardial lesions such as myocardial infarction, myocarditis, Takotsubo syndrome and cardiomyopathies [4]. According to the study, approximately one-third of patients with MINOCA suffer from cardiomyopathies, and MINOCA patients with MI or TTS take up 20% of each. The remaining one-quarter patients have normal myocardium. Therefore, the diagnostic capability of CMR and clinical procedure selection to CMR are gradually becoming under closer scrutiny. The chosen timing of CMR exams on patients leads to perform various outcomes in a retrospective research, and it is statistically showed that patients given CMR within two weeks of hospitalization have a more accurate diagnosis rate than those who take CMR sooner or later.
There is a prospective study, called SMINC-2, studying the efficiency of CMR in diagnosing MINOCA [4]. In this study, T1 mapping and ECV are used to characterize features of MINOCA and contrast with SMINC-1, a former prospective study. The study eliminates individuals who would interfere with CMR imaging testing or the results of diagnostic imaging and employs 112 patients who meet the standard of current diagnostic criteria for MI and has a confirmed diagnosis of MINOCA by invasive coronary angiography as participants. During the experiment, research participants require CMR imaging 2-4 days following admission in hospital. Main finding of the study, which highlights the value of CMR as a diagnostic tool for MINOCA, is that the diagnosis results of MINOCA in 77% of patients with early CMR imaging are consistent with previous diagnosis and obtain higher identification of patient etiologies like myocarditis and TTS.
In patients with suspected non-ST-segment elevation myocardial infarction, CMR can accurately distinguish obstructive CAD and MINOCA, and then be used to confirm the early diagnosis of MINOCA for patient. T2 mapping, cine CMR and late gadolinium enhancement (LGE) imaging are all combined in a study of NSTEMI to diagnose potential obstructive CAD and ACS, and to propose their coronary etiology simultaneously [5]. The findings in this study demonstrate that CMR has 70% higher sensitivity, specificity and overall accuracy for detecting obstructive CAD than others. This study demonstrates that the utilization of a comprehensive multicomponent CMR analysis, which includes cine CMR, T2 mapping and LGE imaging along with adenosine vasodilator stress perfusion imaging, exhibits favorable sensitivity, reasonable specificity and high accuracy in identifying obstructive CAD in patients with non-ST-segment elevation myocardial infarction (NSTEMI). Consequently, this approach serves as a crucial diagnostic approach for the detection of MINOCA.
In addition, the utilization of CMR can be integrated with methodologies such as endomyocardial biopsy to facilitate the prompt identification of individuals presenting with unexplained MINOCA. For instance, eosinophilic myocarditis, an infrequent etiology of MINOCA, has limited diagnostic sensitivity owing to sporadic absence of peripheral eosinophilia. Furthermore, it frequently presents perplexing features such as nearly normal coronary angiograms and unchanged electrocardiograms, which are not conducive to clinical evaluation. A single case study demonstrates that employing natural T1 and T2 calibrations, combined with LGE, unveiled pronounced myocardial injury and edema, starkly contrasting with the patient’s mild symptoms [6]. At this time, an intramyocardial biopsy of the patient reveals a substantial infiltration of eosinophils within the myocardium. Symptomatic therapy is provided, and subsequently, a follow-up CMR is conducted. The follow-up CMR shows a noteworthy amelioration in myocardial edema and cardiac function. The results of CMR in this case is shown in Figure 1.
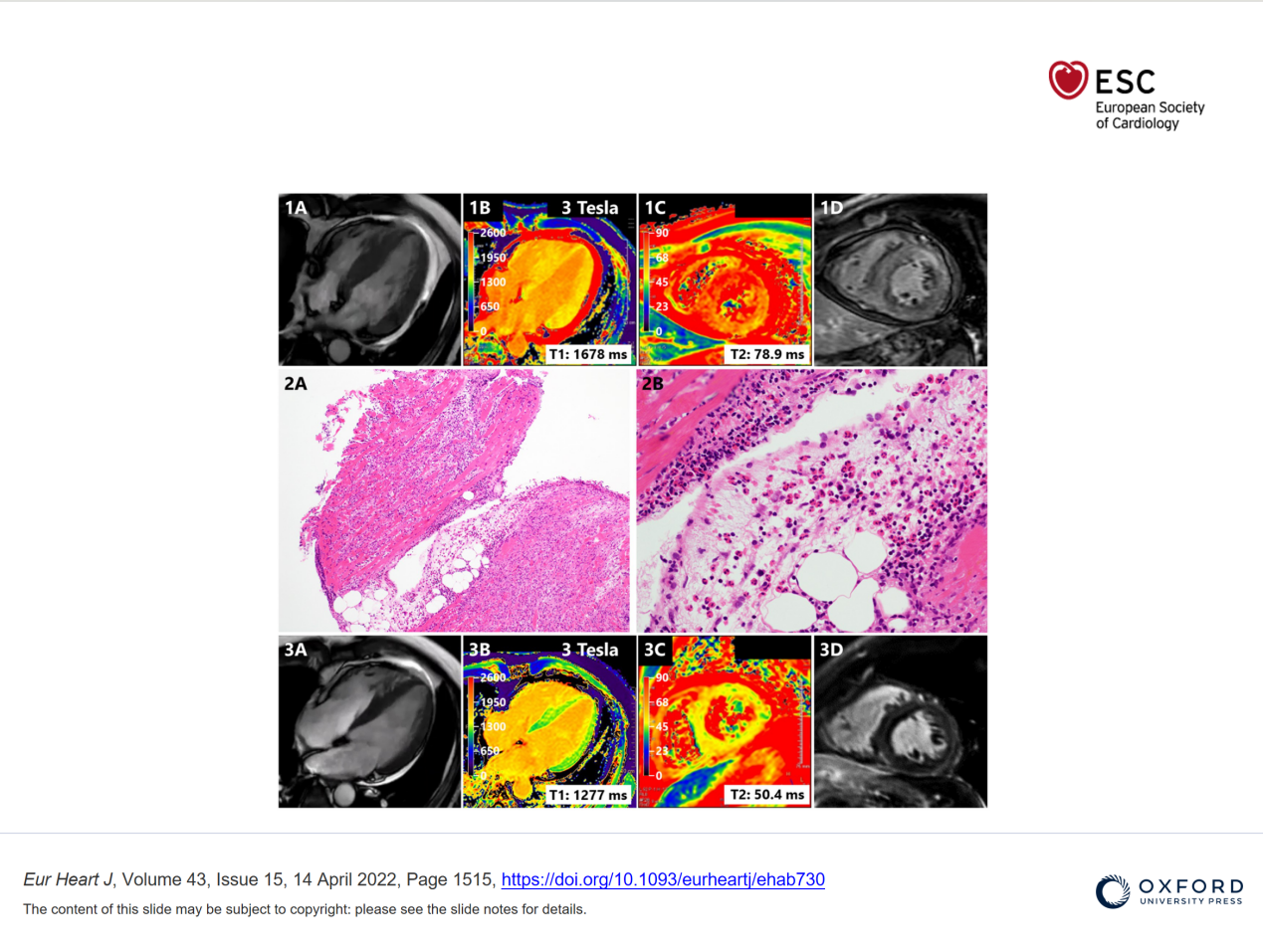
Figure 1. CMR imaging of the patient in acute phase [6].
The etiology of MINOCA presents variability. And its clinical manifestations, epidemiological characteristics, diagnostic approaches, therapeutic interventions, and prognostic outcomes differ to some extent from those observed in coronary artery obstructive myocardial infarction. Hence, the significance of early and differential diagnoses in clinical practice cannot be overstated. By elucidating the underlying causes of a given pathology, healthcare professionals can develop a rational and personalized treatment regimen and conduct thorough long-term monitoring to enhance recovery rates and prognosis outcomes.
4. Role of cardiovascular magnetic resonance in MONICA prognosis
The diagnosis of MINOCA often requires the fulfillment of three specific requirements during coronary angiography: (a) The observed case satisfies the universally accepted criteria for myocardial infarction. (b) The results of coronary angiography indicate the absence of any significant obstruction in the coronary arteries, as defined by no any narrowing of more than 50% in diameter in an artery that could potentially cause myocardial infarction. (c) No noticeable clinical cause can be readily determined for the acute presentation. Moreover, many clinical conditions unrelated to ischemia or thrombosis can display clinical characteristics that resemble those of myocardial infarction. Examples of such conditions are myocarditis and Takotsubo syndrome [7]. Using late gadolinium enhancement technology, CMR presents a notable degree of sensitivity in detecting myocardial changes and can ascertain the underlying etiology of myocardial infarction with MINOCA in a range of 65% to 90% of cases. Gadolinium, a compound with low molecular weight, can readily permeate capillaries and spread into extracellular fluids. In normal myocardium, it is efficiently eliminated from the body within a short period, while in the situation of myocardial necrosis, gadolinium tends to gather, thereby rendering it highly responsive in the detection of myocardial necrosis. However, the prognosis of patients diagnosed with MINOCA in prior studies remains uncertain, so does the potential of CMR as a predictive assessment tool for these patients. Consequently, several ongoing studies are dedicated to exploring the role of CMR in determining the prognosis of MINOCA.
In a prospective study, individuals initially diagnosed with acute coronary syndrome (ACS), heart failure or other medical conditions are enrolled in a follow-up investigation that applied integrated CMR imaging. The primary imaging method utilized in this investigation involves Cine CMR, T2-STIR CMR, and LGE imaging. The study examines the associations between cardiovascular risk factors, comorbidities, treatment received after discharge, and major adverse cardiovascular events (MACE) during the follow-up period. The conclusive study demonstrates that, despite a rising incidence of risk factors and modifications in individual behavior throughout follow-up, thereby introducing additional influencing factors, it can be inferred that CMR can ascertain the prognosis of patients with various forms of myocardial infarction. This is due to its ability to provide information regarding the extent and site of the infarction, along with other parameters that show a strong correlation with the exact prognosis of patients [8].
In addition, early CMR not only aids in the diagnostic process, but also facilitates risk stratification by utilizing the established diagnosis and enhances the ability to predict adverse outcomes through the analysis of related data [9]. Based on imaging findings, CMR supports the appropriate modification of secondary prevention drugs for patients diagnosed with MINOCA . This approach optimizes identifying unneeded treatments, hence expediting the alleviation of patients’ symptoms. By categorizing individuals diagnosed with MINOCA and ensuring appropriate follow-up, a research team discovers that the prognostic outcomes of groups categorized based on CMR findings are superior to those of groups lacking a CMR diagnosis. Furthermore, the team observes a significant correlation between CMR parameters and prognostic outcomes, underscoring the potential of CMR to enhance risk prediction in MINOCA.
The present studies provide evidence that CMR demonstrates a greater prognostic significance compared to conventional clinical factors, including age, sex, coronary heart disease (CHD) risk factors, ST-segment elevation, and peak troponin levels [10]. Moreover, the study shows that an unfavourable outcome is independently associated with a specific CMR diagnosis of acute myocardial infarction (AMI), myocarditis, and non-ischemic cardiomyopathy (NICM), and the flowchart of this study is below in Figure 2. Conversely, a normal CMR examination indicates a favorable prognosis, among other findings.
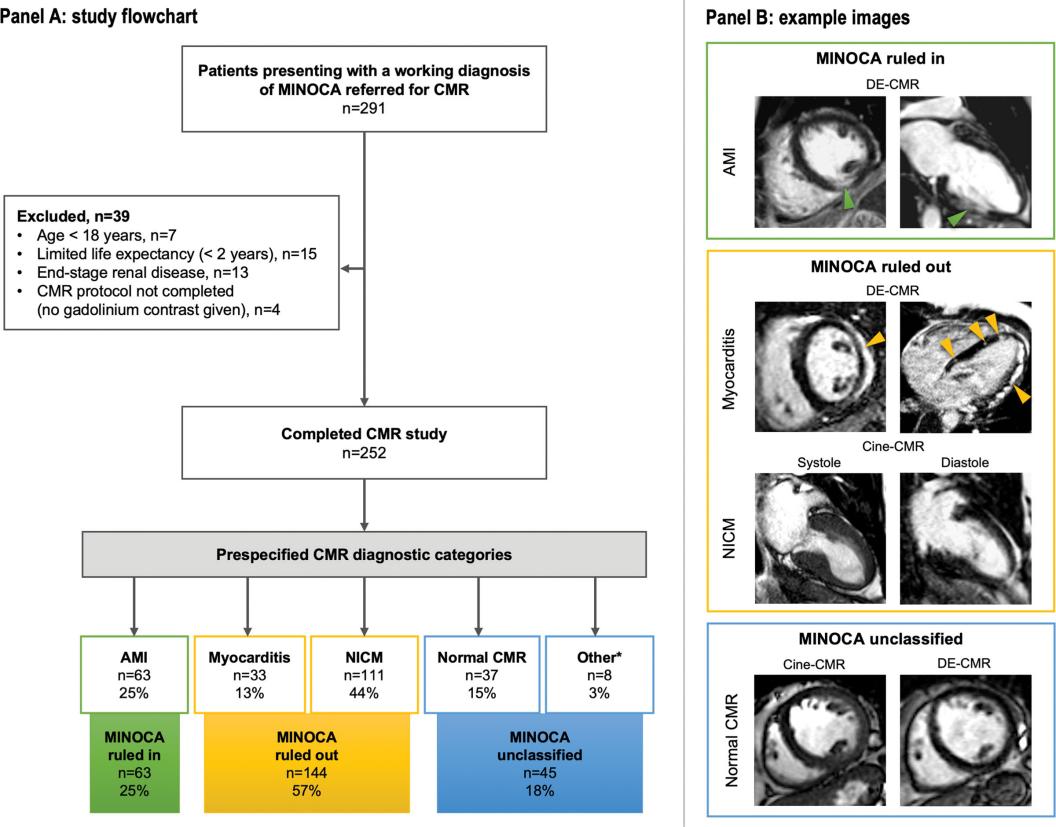
Figure 2. Study Flowchart [10].
Although the limitations pose by factors such as sample size, referral bias, and the absence of modern technology for characterizing coronary plaque in prior studies, these results underscore the significance of CMR imaging in the diagnostic and prognostic evaluation of MINOCA. Accurate phenotypic diagnosis of MINOCA is of paramount importance as it offers essential insights into the underlying etiology, so that facilitating the optimization of therapeutic decision-making and enhancing prognostic outcomes within the clinical setting.
5. Conclusions
According to different researches, CMR impels clinical practice to earlier detection, improved risk stratification and advanced assessment of the prognosis of patients with MINOCA due to its advantages such as non-invasive nature, high-resolution capabilities and ability to provide correct diagnoses. CMR offers extensive insight into the diagnosis and prognosis of this condition, with information on the overall cardiac function and myocardial perfusion status, and enables the assessment of myocardial function at the molecular level and identification of myocardial segments with microcirculation abnormalities. Thus, no matter the level of troponin peak or the results of coronary angiography, clinicians should strongly provide CMR for all patients with MINOCA within 14 days.
However, it is important to acknowledge and prioritize some concerns that require immediate attention in the forthcoming period. For instance, one potential concern regarding gadolinium contrast agents is their capacity to traverse the blood-brain barrier and accumulate within the brain, posing potential risks to human brain issue. What’ s more, the absence of standard in quantitative imaging maps might result in fluctuations in image quality and lead to challenges for different hospitals in committing them. Additionally, the long duration of CMR gives heavier physical burden to individuals experiencing a sudden attack of MINOCA. Thus, several novel technologies, like fingerprinting and quick scanning sequences, are being devised, with more necessary clinical validation to be done to ascertain their efficacy and reliability.
In general, there are some significant steps, including enhancing the scale of clinical experiments, implementing more stringent access criteria, adopting more comprehensive scanning protocols, and employing more objective image analysis methods, to perform the potential to improve traditional models that incorporate new parameters. These improvements show advantages to the integration of available information, enabling a better grasp of the pathological mechanism and diagnostic process of MINOCA. More importantly, advancements can aid in risk stratification, prognosis assessment and developing precision medicine for MINOCA using CMR.
References
[1]. Vidal-Perez R, Casas CAJ, Agra-Bermejo RM, Alvarez-Alvarez B, Grapsa J, Fontes-Carvalho R, et al 2019 World J Cardiol 11(12) 305
[2]. Hausvater A, Pasupathy S, Tornvall P, Gandhi H, Tavella R, Beltrame J, et al 2019 Int J Cardiol Heart Vasc 287 128
[3]. Zhao X, Zeng D, He L and Sun W 2022 J Cardiothorac Surg 17(1) 332
[4]. Sörensson P, Ekenbäck C, Lundin M, Agewall S, Bacsovics Brolin E, Caidahl K, et al 2021 JACC: Cardiovascular Imaging 14(9) 1774
[5]. van Cauteren YJM, Smulders MW, Theunissen RALJ, Gerretsen SC, Adriaans BP, Bijvoet GP, et al 2021 J Cardiovasc Magn Reson 23(1) 40
[6]. Tsuda K, Kanzaki Y and Hoshiga M 2021 Eur Heart J 43(15) 1515
[7]. Vicente-Ibarra N, Feliu E, Bertomeu-Martínez V, Cano-Vivar P, Carrillo-Sáez P, Morillas P, et al 2021 J Cardiovasc Magn Reson 23(1) 83
[8]. Emrich T, Kros M, Schoepf UJ, Geyer M, Mildenberger P, Kloeckner R, et al 2021 Int J Cardiol Heart Vasc 327 223
[9]. Schelbert EB and Fridman Y 2023 Circ Cardiovasc Imaging 16(8) e015833
[10]. Konst RE, Parker M, Bhatti L, Kaolawanich Y, Alenezi F, Elias-Smale SE, et al 2023 Circ Cardiovasc Imaging 16(8) e014454
Cite this article
Zhang,S. (2023). Early diagnosis and prognosis of MINOCA by CMR. Theoretical and Natural Science,17,97-103.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 2nd International Conference on Modern Medicine and Global Health
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Vidal-Perez R, Casas CAJ, Agra-Bermejo RM, Alvarez-Alvarez B, Grapsa J, Fontes-Carvalho R, et al 2019 World J Cardiol 11(12) 305
[2]. Hausvater A, Pasupathy S, Tornvall P, Gandhi H, Tavella R, Beltrame J, et al 2019 Int J Cardiol Heart Vasc 287 128
[3]. Zhao X, Zeng D, He L and Sun W 2022 J Cardiothorac Surg 17(1) 332
[4]. Sörensson P, Ekenbäck C, Lundin M, Agewall S, Bacsovics Brolin E, Caidahl K, et al 2021 JACC: Cardiovascular Imaging 14(9) 1774
[5]. van Cauteren YJM, Smulders MW, Theunissen RALJ, Gerretsen SC, Adriaans BP, Bijvoet GP, et al 2021 J Cardiovasc Magn Reson 23(1) 40
[6]. Tsuda K, Kanzaki Y and Hoshiga M 2021 Eur Heart J 43(15) 1515
[7]. Vicente-Ibarra N, Feliu E, Bertomeu-Martínez V, Cano-Vivar P, Carrillo-Sáez P, Morillas P, et al 2021 J Cardiovasc Magn Reson 23(1) 83
[8]. Emrich T, Kros M, Schoepf UJ, Geyer M, Mildenberger P, Kloeckner R, et al 2021 Int J Cardiol Heart Vasc 327 223
[9]. Schelbert EB and Fridman Y 2023 Circ Cardiovasc Imaging 16(8) e015833
[10]. Konst RE, Parker M, Bhatti L, Kaolawanich Y, Alenezi F, Elias-Smale SE, et al 2023 Circ Cardiovasc Imaging 16(8) e014454