1. Introduction
Constipation is a widespread health problem in modern society, which affects the quality of life, but can easily be ignored and lead to a deterioration in health. Constipation is difficult to describe as a digestive-related condition, defined as difficulty in passing stools, which is characterized by infrequent bowel movements, straining to pass stools, bloating, abdominal pain, and hard stools. There are many types of constipation, which can be divided into secondary and primary [1]. Secondary constipation is an underlying cause, such as the effects of medication or another medical condition. Primary constipation, on the other hand, is constipation that has no definite reason. The Rome IV criteria classify this condition as functional constipation, constipated irritable bowel syndrome or defecation disorder [2]. The Rome IV criteria for the diagnosis and classification of functional gastrointestinal disorders include diagnostic criteria for the symptoms of chronic constipation [3] (Table 1). For the assessment of faecal status, the Bristol scale provides a classification and description of faecal concentrations (Figure 1). The Bristol Stool Form Scale can help the Rome IV to make a more accurate assessment.
The causes of chronic constipation vary between people of different ages and genders. Medications, poor dietary patterns, low dietary fibre intake, prolonged physical inactivity, excessive anxiety, and stress can all contribute to constipation. For constipation, secondary constipation is more targeted, where the doctor only needs to address the secondary cause to get relief. However, functional constipation is more common, and doctors will make recommendations based on the specific situation. The use of laxatives is widespread in treating constipation, with osmotic laxatives such as polyethylene glycol 3350 and stimulant laxatives such as senna. However, some laxatives, such as senna, are more harmful to the body and can cause cramps. So, doctors prefer to treat constipation by increasing fibre and fluid intake and exercising correctly [1].
Dietary fibre is a nutrient obtained from plants that resist digestion by the body's digestive enzymes and thus undergoes fermentation in the large intestine [5, 6]. In the Institute of Medicine of the Institute of Medicine (IOM), dietary fibre is an endogenous food fibre, a naturally occurring edible fibre. Another type of fibre is functional fibre, which is scientifically extracted or synthesized [7]. Also, the most common classification of dietary fibre is by its solubility. It is classified as soluble or insoluble fibre. Soluble fibre comprises non-cellulosic polysaccharides (pectin, gum), while insoluble dietary fibre is mainly composed of cellulose, hemicellulose and lignin [8]. Soluble fibre absorbs water, thus creating a gel-like structure, which simultaneously slows down digestion and gives a feeling of satiety. It also reduces the absorption of fat, glucose, and fructose. Insoluble fibre, on the other hand, retains water, increases the number of faeces, increases intestinal motility, and maintains intestinal microflora. Dietary fibre can be found in whole grain diets, soybeans, and fibrous plants like broccoli. So, for constipation, more people recommend taking more insoluble fibre to speed up bowel movements. However, whether dietary fibre can affect constipation patients needs to be evaluated in experimental studies. This paper aims to investigate whether dietary fibre has a beneficial or detrimental effect on the bodies of people of different ages and genders with constipation.
Table 1. Definitions of Constipation in Rome IV [4].
Symptoms and diagnosis | Criteria fulfilled over the previous 3 months with symptom onset at least 6 months prior to diagnosis |
Straining to evacuate | >25% of defecations |
Lumpy or hard stools | >25% of defecations |
Sensation of incomplete evacuation | >25% of defecations |
Sensation of anorectal obstruction/blockage | >25% of defecations |
Manual maneuvers to facilitate defecations | >25% of defecations |
Evacuations per week | > 3 |
Number of criteria for diagnosis | ≥ 2 |
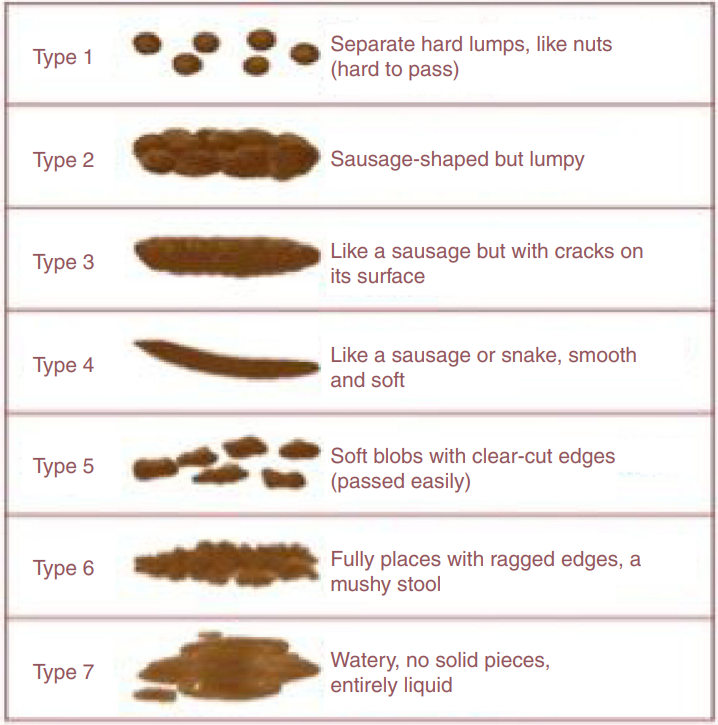
Figure 1. Bristol Stool Form Scale [4].
2. Children patients
2.1. The main cause of constipation
Constipation in children has always been a symptom of great concern to parents. In childhood, the physical function of children changes each period significantly, so the diagnosis of constipation in children is divided into infants and adolescents. Here organic and functional constipation is children's primary type of constipation, and functionality accounts for a large proportion. The cause of organic constipation is determined by organic disease, dietary fibre is not evident in it, so this article only discusses functional constipation in children. The diagnosis of constipation in recent years is based on the Rome IV. The prevalence of constipation in children ranges from 0.7% to 30%, with the highest in Oceania at 19.7% [9].
Infants and young children with functional constipation may be due to no toilet training, or parents are unaware of the average frequency of excretion in infants and young children. Infants and young children will have painful bowel movements due to excessive faeces during excretion; infants and young children will unconsciously begin to contract the sphincter because of pain and thus prohibit defecation. The longer the faeces stay in the colon, the larger the faeces volume will gradually become immense. The water will decrease and become harder [10]. In adolescence, due to the addition of school life patterns, the time of defecation is disturbed, so there is not enough time for elimination [11]. It could also be eating habits.
2.2. The dietary fibre intake in children
Experts advise that dietary fibre intake for children should not be too homogeneous and that it is best to obtain dietary fibre from a wide range of foods. There are also different dietary fibre recommendations for different ages. The recommended amount of fibre intake for children after 2-3 years of age is "age +5g-10g" [12]. For example, the recommended intake for a five-year-old is 5 years old+5g=10g. Years plus 5g is the most reasonable and minimum recommendation. At the same time, there is no detailed evidence of the adverse effects of plus 10g, but adding more than this amount is unreasonable, which will cause adverse reactions in children [12].
2.3. How does dietary fibre affect children patients with constipation
First, whether fibre has a therapeutic effect on children with constipation through experiments conducted by Weber's team in 2014 investigated whether dietary fibre would affect children with chronic constipation after stopping the stool softener. Healthcare professionals treated sixty patients aged 4-12 years with the same frequency and state of bowel movements under maintenance. Patients then discontinued the use of stool softeners. The number of participants in the experiment was divided into a group of people with edible fibre mixtures and a group of edible maltodextrin placebos with a 1:1 ratio. The doses consumed in both groups were based on the children's weight, with 18g being a watershed and children above 18g being given more. During the four weeks of the experimental study, patients were assessed by weekly questionnaire analysis. At the same time, the colonic transit time was obtained by recording the information of abdominal X-ray on the seventh day through the daily intake of radiopaque marker capsules during the last week [13].
The questionnaire evaluation was used to determine whether each patient was successfully treated, and the range of success was regular bowel movements without using stool softeners. The information in Table 2 shows that six patients did not participate in the trial for some reason. Also, there were nine failures in the fibre group and 10 in the placebo group. Regarding success, the fibre group was higher but not so different from the placebo group. This data indicates that dietary fibre is no substitute for stool softener in treating children with chronic constipation.
In addition to investigating the success of treatment, the frequency of defecation, the status of stool, and colonic transit time (CCT) were recorded by patients. These are adequate to analyze whether fibre affects the symptoms of pediatric patients. In these records, it was found from Table 3 that intake of dietary fibre mixture increases the defecation frequency of patients (0.529 ± 0.423).
According to Table 4, patients in the dietary fibre group excreted non-hardened stools more than those in the placebo group, accounting for 60 per cent. The control group had only four non-hardened seats, accounting for 16.7 per cent of the entire group. However, the right and left colon and rectosigmoid transit times did not differ significantly between the two groups. In this experiment, dietary fibre has a somewhat more significant effect on faeces while enhancing the desire to defecate in children but does not improve CTT very much.
For chronic constipation in children, dietary fibre does not cure this, but it can be used to help patients avoid recurrence and exacerbations. At the same time, in the study of Chao et al., it was found that the dietary fibre content for improving constipation should also increase with age. And the intake of dietary fibre may offset the need for short-term constipation in children to consume laxatives [14].
Table 2. The Primary outcome measures in Weber experiment [13].
Variable | Dietary fibre mixture group, n=26, n (%) | Control group, n=28, n (%) | RR (95% CI) | NNT |
Therapeutic failures | 9 (34.6) | 10 (35.7) | 0.98 (0.54-1.75) | 100 |
Therapeutic successes | 17 (65.4) | 18 (64.3) | ||
X2 test (P=0.933). CI=confidence interval; NNT=number needed to treat; RR =risk ratio | ||||
Table 3. Defecation frequency in the Weber experiment [13].
Dietary fibre mixture group, n=20 | Control group, n=24 | P | |
Defecation frequency | |||
Basal | 0.564±0.299† | 0.675±0.304‡ | 0.230* |
Final | 1.093±0.452† | 0.907±0.310‡ | 0.114* |
Δ(final - basal) | 0.529±0.423 | 0.232±0.350 | 0.014* |
SD = standard deviation *Student t test, mean ±SD. Paired t test. †P<0.001. ‡P=0.004. | |||
Table 4. Stool consistency according to the Bristol Stool Form Scale in Weber experiment [13].
Stool consistency | Dietary fiber mixture group, n=20, n (%) | Control group, n=24, n (%) | RR (95% CI) | NNT |
Hardened | 8 (40.0) | 20 (83.3) | 0.38 (0.20-0.73) | 3 |
Nonhardened | 12 (60.0) | 4 (16.7) | ||
X2 test (P=0.003). Stool consistency = predominant type of feces according to the Bristol Stool Form Scale. Hardened stools: type 1, 2, and/or 3; nonhardened stools: type 4, 5, 6, and/or 7. CI=confidence interval; NNT=number needed to treat; RR =risk ratio | ||||
3. Adult patients
3.1. The main cause of constipation
The constipation of the prevalence of adults is not low, even higher than the prevalence of statistics. Because many adults feel that constipation is not severe and it does not affect their personal lives too much at first, they do not go to the hospital. They usually go to the pharmacy to buy supplementary nutrients or laxatives for excretion. Compared with acute constipation, there are relatively many people with chronic constipation. The main reasons for being more prone to constipation are gender, lack of exercise and inadequate fluid and dietary fibre intake, as well as high levels of work or too many late nights at school leading to excessive mental tension, stress and too much exertion. Through research conducted by Moezi et al. in 2019 [9], a survey of 9,000 adults in southern Iran with chronic constipation showed that the prevalence of women was 2.6% higher than that of men, and people with insufficient weight were more likely to get it. People with less exercise were more likely to get.
At the same time, it has been found in other studies that the reason for the higher prevalence of women is because dysmenorrhea during menstruation causes women to start taking analgesic drugs, which may lead to an increase in the risk of women. Hormonal differences compared to men, as well as the effect of progesterone on the gut, all affect the rate. Pelvic floor muscle problems caused by childbirth can also play a role [15].
3.2. The dietary fibre intake in adult
For adults' dietary fibre intake, there is no need for particular calculations like children. In each country, there are dietary fibre requirements for their people. Different countries have different geographical environments and economic developments, which are the conditions that national professional institutions will consider. The detailed definition of dietary fibre in all countries is also different, so there are many differences in intake (Table 5).
Table 5. The recommendation dietary fibre of adult in different country [16].
Country | Dietary Fibre Recommendation |
United States | 28 g/2000 kcal |
Australia | 25–40 g/d |
Canada | Women: 25, Men: 38 g/d |
Mexico | 25 g/d |
United Kingdom | 18 g/d (not include resistant starches or short oligomers) | 30 g/d |
European Union | 25 g/d |
India | 40 g/2000 kcal |
Turkey | Women: 25 g/d, Men: 29 g/d |
Norway | At least 25–35 g/d, or approximately 3 g per MJ |
Republic of South Korea | Men: 20g/d, Women: 25g/d; 12g/1000 kcal |
South Africa | 18–38 g/d |
3.3. How does dietary fibre affect adult patients with constipation
Compared to children, adults have more mature organ systems and more robust immune systems than children. But constipation is still common in adults, especially women. In 2005, Arya et al. investigated the risk of chronic constipation in women with pelvic organ prolapse and the association with dietary fibre. In this study, 60 females with pelvic organ prolapse(POP) and 30 females of similar age without pelvic organ prolapse were identified for comparison. They were surveyed for dietary fibre intake and constipation symptoms. According to the questionnaire results, 42 people in the POP group were constipated, and their main symptom was difficulty in passing stools (69%). In comparison, 11 in the control group were constipated, and their main symptom was hard stools (35%) and the inability to empty them (45%). Also, for dietary fibre, the women in the POP group consumed more soluble and less insoluble fibre [17]. Controlling dietary fibre has helped some people with pelvic organ prolapse lower their risk of constipation. So, increasing the intake of insoluble fibre will reduce the risk of constipation.
Consuming more dietary fibre does not, however, necessarily make constipation better or treat it. Ho et al. conducted a study in 2012 to determine whether reducing or stopping dietary fibre would reduce the risk of constipation. The study was conducted on patients with idiopathic constipation and patients who passed standard colonoscopy. 62 patients (16 men and 47 women) were asked to abstain from dietary fibre for a fortnight while consuming protein and carbohydrates. Small amounts of fibre were slowly restored after two weeks. Finally, data on the patients' constipation symptoms and dietary fibre intake were collected at one month and six months. Because of various factors, the study participants were divided into three groups: no fibre diet, reduced fibre diet and high fibre diet [18]. Table 6 demonstrates that the frequency of bowel movements rose in individuals who did not consume any fibre and those who did but remained unchanged in those who consumed high amounts of fibre. This finding is not the same as any of the previous experiments. However, the effect of insoluble fibre is to increase the volume of faeces and soluble is to slow down digestion. It is possible that consuming more of it will burden the gut and anus. Therefore, controlling dietary fibre intake is a treatment for chronic constipation in the future.
Table 6. The bowel frequency during 6 months [18].
Numbers of people | In 1-month bowel frequency | After 6 months bowel frequency | |
0 fibre intake | 41 | 3.75d (±1.59d) | 1.0d (±0.00d) |
Reduced fibre intake | 16 | 4.19d (±2.09d) | 1.9d (±1.21d) |
High fibre intake | 6 | 6.83d (±1.03d) | 6.83d (±1.03d) |
4. Old patients
4.1. The main cause of constipation
According to study data [9, 19], the prevalence of constipation increases with age. However, intestinal physiological changes with age are not the leading cause of constipation in the elderly. Generally, intestinal function in the elderly is normal. Insufficient dietary fibre intake, physical weakness caused by mobility, and inability to exercise the muscles around the anus can easily lead to constipation in the elderly [19]. Organic constipation is more common than other types of constipation. Some medications commonly taken by the elderly, such as opioid painkillers and oral iron supplements, can have constipation as a side effect. Because older people have a lower immune system and lower body function, they are more likely to suffer from a range of diseases than adults. Older people with neurological conditions, gastrointestinal disorders and diseases related to metabolism are all constipated [20].
4.2. The dietary fibre intake in old people
With the increase of age, people reach old age, and physical functions begin to decline gradually. Dental health and bite force related to eating are relatively reduced in digestive capacity, which can significantly affect the intake of nutrients in the elderly. Because they cannot chew and swallow and digest normally, the dietary intake of the elderly will generally be much less. For people with constipation, it is recommended to consume 20-25g of dietary fibre per day. Dietary fibre, combined with adequate fluid intake and a certain amount of exercise, is helpful [19].
4.3. How does dietary fibre affect old patients with constipation
A minor symptom may evolve into a severe disease in old age. In the same way, the diet of the elderly also needs to be very strictly planned, and some nutrients exceeding the standard may have a harmful impact. Therefore, for elderly patients with constipation, dietary fibre intake depends on their physical condition. If it is mild constipation, dietary fibre can be gradually increased by 5g, and the amount of water consumed should also increase. But for some patients with severe constipation, the impact of dietary fibre is minimal. Primarily because of intestinal transit and emptying problems in elderly patients, excessive nutritional fibre intake is likely to produce more negative symptoms [21].
To maximize the function of dietary fibre to help older people with constipation, Sturtzel and Elmadfa investigated in 2008 whether dietary fibre can help older people with constipation reduce the use of laxatives. Thirty people aged 57 to 100 years who used laxatives were divided into the fibre and control groups, with 15 in each group. The fibre group were given dietary fibre oat bran mixed into their daily diet. By recording the patient's laxative use, weight, and diet, see if a treatment option that can replace laxatives can be developed [22].
The information in Figure1 and Figure2 shows that the frequency of laxative use in the fibrous group decreases in the later stages, and there is no significant change in body weight. In contrast, in the control group, the number of laxatives used increased in the third stage, and the patient's weight decreased. This shows that dietary fibre can help patients with constipation relieve symptoms, reduce the number of laxatives used, and live more comfortably. In the future, it is possible to develop in this regard, little by little, to change the dietary patterns of elderly constipation patients. Although it may not cure all the elderly with constipation, improving a little is a great success.
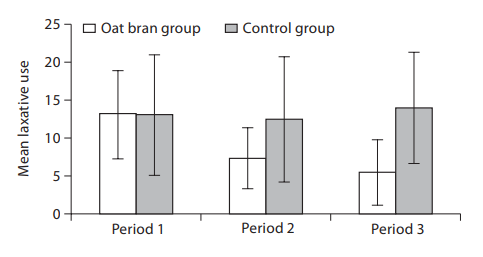
Figure 2. Mean laxative use per patient per period (= 23 days) in the oat bran and control groups [22].
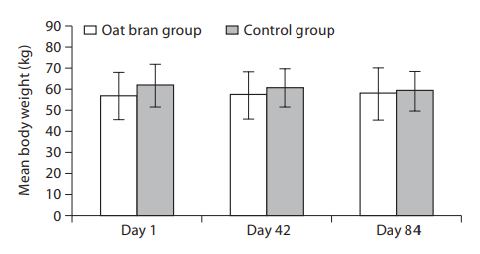
Figure 3. Mean body weights on days 1, 42 and 84 in the oat bran and control groups [22].
5. Conclusion
People of different ages need different dietary fibres every day. Dietary fibre has a positive effect on the general symptoms of constipation. It can improve and help people prevent the appearance of constipation symptoms. But for, some patients with unique constipation need to reduce their dietary fibre to a certain extent. Therefore, patients with constipation need to understand their causes and the severity of symptoms in detail to decide whether to increase or decrease dietary fibre intake. Diets are safer and less harmful to the human body than drugs. However, according to current research, dietary fibre does not have the effect of completely curing constipation. Making people safer to treat constipation is a problem that needs to be studied.
References
[1]. B. Jani,E. Marsicano, "Constipation: evaluation and management," Missouri medicine, 115(3), 236 (2018).
[2]. A. E. Bharucha,B. E. Lacy, "Mechanisms, evaluation, and management of chronic constipation," Gastroenterology, 158(5), 1232-1249. e3 (2020).
[3]. M. Russo, C. Strisciuglio, E. Scarpato, et al., "Functional chronic constipation: Rome III criteria versus Rome IV criteria," Journal of neurogastroenterology and motility, 25(1), 123 (2019).
[4]. C. W. Sobrado, I. J. F. Corrêa Neto, R. A. Pinto, et al., "Diagnosis and treatment of constipation: a clinical update based on the Rome IV criteria," Journal of Coloproctology (Rio de Janeiro), 38, 137-144 (2018).
[5]. M. Ciudad-Mulero, V. Fernández-Ruiz, M. C. Matallana-González, et al., "Dietary fiber sources and human benefits: The case study of cereal and pseudocereals," in: Advances in food and nutrition research, edited by (Elsevier, 2019), pp. 83-134.
[6]. R. Kay, "Dietary fiber," Journal of lipid research, 23(2), 221-242 (1982).
[7]. N. D. Turner,J. R. Lupton, "Dietary fiber," Advances in nutrition, 2(2), 151-152 (2011).
[8]. R. Korczak,J. L. Slavin, "Definitions, regulations, and new frontiers for dietary fiber and whole grains," Nutrition reviews, 78(Supplement_1), 6-12 (2020).
[9]. P. Moezi, A. Salehi, H. Molavi, et al., "Prevalence of chronic constipation and its associated factors in pars cohort study: A study of 9000 adults in Southern Iran," Middle East journal of digestive diseases, 10(2), 75 (2018).
[10]. S. S. Baker, G. S. Liptak, R. B. Colletti, et al., "Constipation in Infants and Children: Evaluation and Treatment," Journal of Pediatric Gastroenterology and Nutrition, 29(5), 612-626 (1999).
[11]. Y. Vandenplas,T. Devreker, "Functional constipation in children", SciELO Brasil, 2019, pp. 1-3.
[12]. J. T. Dwyer, "Dietary fiber for children: how much?," Pediatrics, 96(5), 1019-1022 (1995).
[13]. T. K. Weber, M. S. Toporovski, S. Tahan, et al., "Dietary fiber mixture in pediatric patients with controlled chronic constipation," Journal of pediatric gastroenterology and nutrition, 58(3), 297-302 (2014).
[14]. H.-C. Chao, M.-W. Lai, M.-S. Kong, et al., "Cutoff volume of dietary fiber to ameliorate constipation in children," The Journal of pediatrics, 153(1), 45-49. e1 (2008).
[15]. P. a. Chiarelli, W. Brown,P. McElduff, "Constipation in Australian women: prevalence and associated factors," International Urogynecology Journal, 11(2), 71-78 (2000).
[16]. K. B. Miller, "Review of whole grain and dietary fiber recommendations and intake levels in different countries," Nutrition Reviews, 78(Supplement_1), 29-36 (2020).
[17]. L. A. Arya, J. M. Novi, A. Shaunik, et al., "Pelvic organ prolapse, constipation, and dietary fiber intake in women: a case-control study," American journal of obstetrics and gynecology, 192(5), 1687-1691 (2005).
[18]. K.-S. Ho, C. Y. M. Tan, M. A. M. Daud, et al., "Stopping or reducing dietary fiber intake reduces constipation and its associated symptoms," World Journal of Gastroenterology: WJG, 18(33), 4593 (2012).
[19]. P. Gallagher,D. O'Mahony, "Constipation in old age," Best Practice & Research Clinical Gastroenterology, 23(6), 875-887 (2009).
[20]. D. Gandell, S. E. Straus, M. Bundookwala, et al., "Treatment of constipation in older people," Cmaj, 185(8), 663-670 (2013).
[21]. A. Mari, M. Mahamid, H. Amara, et al., "Chronic constipation in the elderly patient: updates in evaluation and management," Korean Journal of Family Medicine, 41(3), 139 (2020).
[22]. B. Sturtzel,I. Elmadfa, "Intervention with dietary fiber to treat constipation and reduce laxative use in residents of nursing homes," Annals of Nutrition and Metabolism, 52(Suppl. 1), 54-56 (2008).
Cite this article
Zhou,J. (2023). Effects of Dietary Fibre on People with Constipation. Theoretical and Natural Science,4,56-64.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 2nd International Conference on Biological Engineering and Medical Science (ICBioMed 2022), Part II
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. B. Jani,E. Marsicano, "Constipation: evaluation and management," Missouri medicine, 115(3), 236 (2018).
[2]. A. E. Bharucha,B. E. Lacy, "Mechanisms, evaluation, and management of chronic constipation," Gastroenterology, 158(5), 1232-1249. e3 (2020).
[3]. M. Russo, C. Strisciuglio, E. Scarpato, et al., "Functional chronic constipation: Rome III criteria versus Rome IV criteria," Journal of neurogastroenterology and motility, 25(1), 123 (2019).
[4]. C. W. Sobrado, I. J. F. Corrêa Neto, R. A. Pinto, et al., "Diagnosis and treatment of constipation: a clinical update based on the Rome IV criteria," Journal of Coloproctology (Rio de Janeiro), 38, 137-144 (2018).
[5]. M. Ciudad-Mulero, V. Fernández-Ruiz, M. C. Matallana-González, et al., "Dietary fiber sources and human benefits: The case study of cereal and pseudocereals," in: Advances in food and nutrition research, edited by (Elsevier, 2019), pp. 83-134.
[6]. R. Kay, "Dietary fiber," Journal of lipid research, 23(2), 221-242 (1982).
[7]. N. D. Turner,J. R. Lupton, "Dietary fiber," Advances in nutrition, 2(2), 151-152 (2011).
[8]. R. Korczak,J. L. Slavin, "Definitions, regulations, and new frontiers for dietary fiber and whole grains," Nutrition reviews, 78(Supplement_1), 6-12 (2020).
[9]. P. Moezi, A. Salehi, H. Molavi, et al., "Prevalence of chronic constipation and its associated factors in pars cohort study: A study of 9000 adults in Southern Iran," Middle East journal of digestive diseases, 10(2), 75 (2018).
[10]. S. S. Baker, G. S. Liptak, R. B. Colletti, et al., "Constipation in Infants and Children: Evaluation and Treatment," Journal of Pediatric Gastroenterology and Nutrition, 29(5), 612-626 (1999).
[11]. Y. Vandenplas,T. Devreker, "Functional constipation in children", SciELO Brasil, 2019, pp. 1-3.
[12]. J. T. Dwyer, "Dietary fiber for children: how much?," Pediatrics, 96(5), 1019-1022 (1995).
[13]. T. K. Weber, M. S. Toporovski, S. Tahan, et al., "Dietary fiber mixture in pediatric patients with controlled chronic constipation," Journal of pediatric gastroenterology and nutrition, 58(3), 297-302 (2014).
[14]. H.-C. Chao, M.-W. Lai, M.-S. Kong, et al., "Cutoff volume of dietary fiber to ameliorate constipation in children," The Journal of pediatrics, 153(1), 45-49. e1 (2008).
[15]. P. a. Chiarelli, W. Brown,P. McElduff, "Constipation in Australian women: prevalence and associated factors," International Urogynecology Journal, 11(2), 71-78 (2000).
[16]. K. B. Miller, "Review of whole grain and dietary fiber recommendations and intake levels in different countries," Nutrition Reviews, 78(Supplement_1), 29-36 (2020).
[17]. L. A. Arya, J. M. Novi, A. Shaunik, et al., "Pelvic organ prolapse, constipation, and dietary fiber intake in women: a case-control study," American journal of obstetrics and gynecology, 192(5), 1687-1691 (2005).
[18]. K.-S. Ho, C. Y. M. Tan, M. A. M. Daud, et al., "Stopping or reducing dietary fiber intake reduces constipation and its associated symptoms," World Journal of Gastroenterology: WJG, 18(33), 4593 (2012).
[19]. P. Gallagher,D. O'Mahony, "Constipation in old age," Best Practice & Research Clinical Gastroenterology, 23(6), 875-887 (2009).
[20]. D. Gandell, S. E. Straus, M. Bundookwala, et al., "Treatment of constipation in older people," Cmaj, 185(8), 663-670 (2013).
[21]. A. Mari, M. Mahamid, H. Amara, et al., "Chronic constipation in the elderly patient: updates in evaluation and management," Korean Journal of Family Medicine, 41(3), 139 (2020).
[22]. B. Sturtzel,I. Elmadfa, "Intervention with dietary fiber to treat constipation and reduce laxative use in residents of nursing homes," Annals of Nutrition and Metabolism, 52(Suppl. 1), 54-56 (2008).









