1. Introduction
People of the 21st century are in a new pandemic of mental illnesses. The latest data from the World Health Organization indicates that approximately 1 in every eight people has a mental disorder [1]. Following the unprecedented outbreak of Coronavirus across the globe, survey data suggests an over 25% increase in both Major Depressive Disorder (MDD) and anxiety disorder (AD) is evident in 2020 alone [2]. In addition to the suffering, people with mental disabilities often fall victim to social discrimination, stigma, and lack of access to adequate care.
However, recent studies point out that current treatments for mental illnesses, including psychoactive drugs and psychological therapies, fare less well in the long run. Conventional medicine, which uses prescription pills such as anti-depressant as the front line in reaction to mental health crises, is showing declining utility in many follow-up studies and systematic reviews. Mulder and Frampton found that the recovery and relapse rate for mood disorders was no better now than 50 years ago when anti-depressants were less prescribed [3]. Despite the compromised methodology of this study due to the lack of historical data, the result still tells us of the limitation of psychoactive drugs in treating mental illness. More worryingly, in a study back in 2004, Martin et al. found a 3-fold bipolar conversion rate among children aged 10-14 years when treated with anti-depressants for depression [4]. As these studies indicate, an effective long-term solution is needed to prevent and treat this worldwide mental illness crisis.
The human brain and heart, two critical and 24-hour working organs in the body, have an indicative role in survival and health. Diets have a lot to do with one's cardiovascular fitness. Scientists have confidently established that after years of research. So, it is natural for one to wonder could dietary patterns also impact our brain health.
2. The Gut-Brain axis
Science ties the knot between mental health and nutrition through one’s gut. The gut microbiome, everything living from one’s mouth to the colon, has been the new spotlight of health-related research. It could include all the bacteria, viruses, fungi, and other microscopic organisms in the digestive tract. The amount of bacterial DNA (deoxyribonucleic acid) in an average human body is ten times greater than the body’s own DNA. These ever-humbling observations and findings have changed the old notion that all bacteria are harmful. Gut microbes are a massive community in our bodies.
They not only help to resist the invasion of foreign germs but also secrete immunoglobulins to help the body improve its immunity. For example, they can regulate the body’s physiology by promoting the repair of damaged mucous membranes. In addition, it is the role of intestinal microorganisms to promote intestinal digestion and absorption. Gut-brain axis is the two-way signaling and association between the gut and the brain (Figure 1) [5].
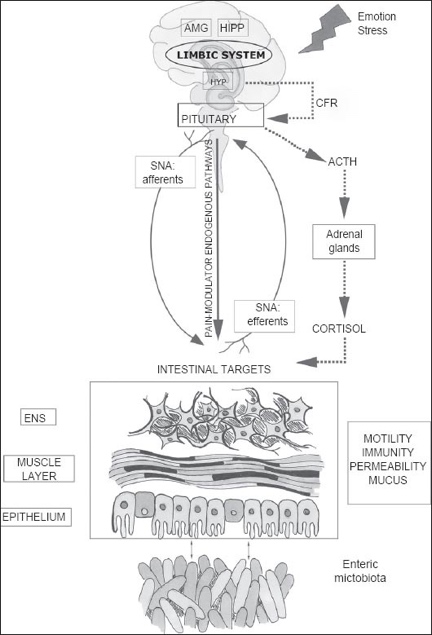
Figure 1. An illustration of the interaction between gut-brain axis and microbiota [5].
The primary role of our gastrointestinal tract is to store food, digest, and absorb nutrients. The endless microvilli constantly transport nutrients from food into the bloodstream through the cellular membrane transport system to provide energy for all our vital activities. In this process, the role of intestinal microorganisms is pivotal. Bifidobacterium, yeast, and E. coli all play their respective roles in the breakdown of surimi and partial processing. The products of these microorganisms can be better absorbed and utilized by the intestinal mucosa.
Numerous studies have confirmed that the central nervous system (CNS) and the gastrointestinal tract is bidirectional. This interaction has huge impact on one’s intestinal motility, absorption, endocrine, and immune functions. Since gut microbes play a critical role in the brain-gut axis, we can consider the CNS, the autonomic nervous system, the enteric nervous system, the GI tract, and a wide variety of gut flora, the brain-gut-bacterial axis. In this system, signal transduction regulates the body in two directions. From the bottom up, afferent fibers project to the central nervous system. From the top down, efferent fibers project to the smooth muscle cells of the intestinal wall. This bi-directional relationship constitutes the down-top and top-down systems of regulation.
In these reciprocal processes, the intestinal microorganisms become the ultimate regulator of the central system by secreting substances and directly stimulating the epithelial tissues of the GI tract, or they can undergo a series of changes in the endocrine, dynamics, and permeability of the intestinal mucosa in response to the downstream signals from the central system. In turn, this change triggers a change in the center. This is a cycle in which the intestinal microbes are an essential part.
3. Nutrients related to neurotransmitters
From a nutritional point of view, cultivating a positive gut-brain axis means eating a wide variety of foods, including leafy greens, legumes, and fresh fruit. Expose one’s gastrointestinal system to diverse food as one’s ancestors who once eat the plants in nature and animals they hunt. Amino acids are the essential elements that makeup proteins. There are two types of amino acids, essential and non-essential. Essential amino acids are those that the body cannot synthesize on its own and must be supplemented through diet and other food sources. Non-essential amino acids can be made or synthesized in the body but are usually best consumed through the diet.
Amino acids are vital substances for our bodies. Different amino acids have other functional properties. Without them, we cannot survive. The importance of having various food to develop a healthy gut cannot be stressed enough. Chemicals, such as tryptophan, tyrosine, and Indole-2-Latic Acid (ILA), enter the body through food and are vital for daily functioning.
Tryptophan, an essential precursor to the brain's serotonin and melatonin, is rich in foods like eggs and chia seeds (Figure 2). It is an essential amino acid in the central nervous system and is a precursor to the crucial neurotransmitter pentraxin (5-HT). Tryptophan is decarboxylated to tryptamine in the body, and under the action of hydroxylase, 5-hydroxytryptamine (5-HT) is produced. 5-HT has the effect of neutralizing epinephrine and norepinephrine, which can improve sleep quality, shorten sleep latency, lengthen slow-wave sleep, reduce waking time, increase total sleep, and is effective for sleep disorders such as difficulty falling asleep, early waking, and excessive dreaming; when the brain When the level of 5-hydroxytryptamine in the brain is reduced, it will show abnormal behavior, appearing restlessness, delusional hallucinations, and insomnia, etc. It has a role in promoting the differentiation of bone marrow T-lymphocyte precursors into mature T-lymphocytes. It is thought to be the only amino acid associated with itself and has been linked to the development of several autoimmune diseases (e.g., autoimmune asthma). Therefore, tryptophan deficiency leads to a decrease in humoral immune function.
Professor Wurtman of the Massachusetts Institute of Technology found that the concentration of the brain neurotransmitter 5-hydroxytryptamine depends on the amount of tryptophan consumed from the diet [6]. Wurtman further showed that the concentration of serotonin in the brain is directly proportional to the attention of tryptophan in the brain and blood. The amount of tryptophan consumed in the diet directly affects serotonin in the blood, brain, and whole body. This is the first recognized and proven direct control of brain neurotransmitters by a single amino acid. Neurotransmitters are specific chemicals that act as "messengers" in synaptic transmission, referred to as transmitters. With the development of neurobiology, many neuroactive substances have been discovered in the nervous system. The brain has four neurotransmitters: biogenic amines, amino acids, peptides, and others. The biogenic amine neurotransmitters were the first to be discovered and included 5-hydroxytryptamine (5-HT), also known as (serotonin), dopamine (DA), norepinephrine (NE), and epinephrine (E).
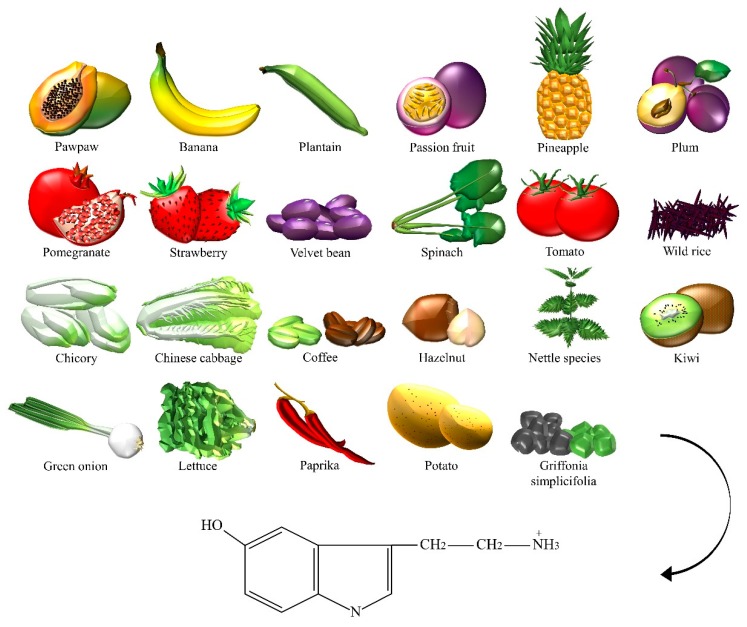
Figure 2. Food that contains serotonin [7].
Many health problems are associated with low levels of 5-hydroxytryptamine (serotonin) in the brain. There are many causes of reduced serotonin, including stress, lack of sleep, poor nutrition, and lack of exercise. When reduced below the required amount, people experience problems such as difficulty concentrating, which can indirectly affect personal planning and organizational skills. This condition is also often accompanied by stress and boredom and can cause depression if serotonin levels drop. Simply put, serotonin makes people happy, and a deficiency of serotonin causes bad moods such as depression and anxiety.
Tyrosine, also known as L-tyrosine, is a non-essential amino acid. Although tyrosine is critical, it is considered a "non-essential" amino acid because the body itself can convert phenylalanine to tyrosine [8]. In most animals, melatonin is produced by the pineal cells in the pineal gland (Figure 3). In humans, 5-hydroxytryptamine (also known as serotonin) is converted to N-acetyl-5-hydroxytryptamine by the reaction with acetyl coenzyme A catalyzed by N-acetyltransferase. Then N-acetyl-5-hydroxytryptamine is methylated to melatonin by S-adenosylmethionine catalyzed by acetyl serotonin O-methyltransferase. Melatonin is associated with the body's circadian rhythm and contributes to sleep, which partially offsets the epinephrine and norepinephrine, and can alter sleep duration. Animals with reduced serotonin and melatonin will show abnormal behaviors and symptoms in their brains.
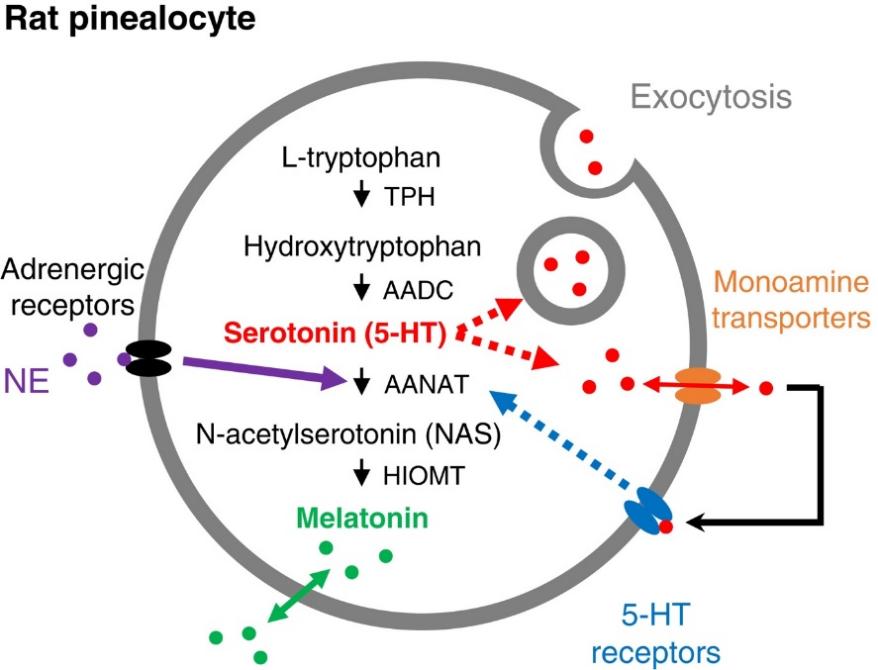
Figure 3. Illustration of melatonin synthesis in rat pinacocytes [9].
Similarly, tyrosine produces dopamine and epinephrine in almonds and lima beans. These two chemicals both play crucial roles in living an active life. It propels and initiates people to do things. Last, fermented food like pickles and kimchi is rich in ILA. Certain bacteria in the gut convert ILA to IPA (indole-3-propionic acid), one of the most potent antioxidants in the body [7]. Antioxidants break down the free radicals that damage one’s cells and DNA and keep one’s body healthy longer.
4. Using Nutrients to treat mental illness
Currently, the prevention and treatment of depression are still dominated by psychological interventions and antidepressant medications. In addition, dietary nutrition interventions in the clinical management of depression have received much attention in recent years.
The Mediterranean dietary pattern is one of the most popular nutritional patterns in modern nutrition, which emphasizes the consumption of olive oil, legumes, whole grains, fruits, vegetables, and fish, appropriate dairy products, moderate consumption of red wine, and less red meat and processed meat products [10]. This dietary pattern is rich in unsaturated fatty acids and low in saturated fat. Total fat produces about 25-35% of the total energy while saturated fat composing for only about 7-8% [11]. Compared with the Mediterranean dietary pattern, the Western one is a typical unhealthy one, a diet mainly based on animal foods, with the "three highs and one low" characteristics of high calories, high saturated fat, high protein, and low dietary fiber. Most studies have shown that having a Western diet is positively linked to the rate of depression. This difference is closely related to changes in the diversity of gut microbiota induced by food components, resulting in health changes based on the gut-brain axis.
The Japanese dietary pattern is also the world's most respected dietary pattern structure. It is marked by consuming a lot of vegetables and fruits, and meat is mainly fish and seafood, especially deep-sea fish, which is rich in protein and polyunsaturated fatty acids.
From the above dietary structure and related research results, we can find a pattern: a healthy dietary way rich in unsaturated fatty acids can lessen the probability of getting depressive disorders and alleviate the depression symptoms [12], while an unhealthy dietary pattern high in saturated fatty acids and trans fatty acids can contribute to the development of depression. This suggests that the prevention or improvement of depression should be based on an adequate intake of unsaturated fatty acids while reducing the intake of saturated and trans fatty acids [13]. Omega-3 fatty acids have the highest association with depression among unsaturated fatty acids. The mechanism is that Omega-3 deficiency can cause neurotransmission changes, increased secretion of pro-inflammatory cytokines, and apoptosis of neurons, all of which are closely related to the pathogenesis of depression. Different molecular structures of Omega-3 have different metabolic pathways in the body and enter the brain in different ways and with extra efficiency [11].
A healthy diet, such as the Japanese diet, can help people regulate emotional and physical functions. More importantly, eating healthy reduces stress-induced inflammation, a risk factor for developing psychiatric disorders. A study by Böbel et al. in 2018 showed that healthy young adults have more stress-induced inflammation in the same stressful environment compared to a rural population [14]. Although scientists have difficulty directly linking mental illness and diets, evidence of improving nutritional intake to treat or prevent psychiatric disorders is promising.
Many meta-analyses from different countries and populations looked at the relationship between nutrition and depression with various methods. They all have proved that consuming mostly healthy food is reversely associated with depression and depression risk. In 2017, a 12-week randomized controlled experiment in Australia provided the first piece of the experimental evidence on diet and depression. Using a ModiMed Diet, a refined version of the Mediterranean diet for Australians, researchers saw a significant reduction in depressive symptoms in the experiment group [15]. However, experiment on diets has shortcomings like the inability to blind participants. People know what they are eating. In Spain in 2013, one of the most extensive clinical trials done on nutrition that examines cardiovascular events and diet on nearly 8000 people across Spain was also able to link a lower adherence to a Mediterranean diet with an increased risk for depression in people with diabetes [16]. Yet, more randomized and controlled studies are needed for scientists to reach a sounder conclusion.
5. Conclusion
So far, it can be sure that diet is closely related to our body's ability to regulate itself. But how much diet works as a treatment for mental illness needs more evidence and research. This article elucidates the role of diet in one’s mental health. The prevalence of mental illness in the current population requires seeking effective long-term treatment other than psychoactive drugs. The gut-brain axis offers new insight into dietary therapy for many health problems. The intrinsic mechanisms of diet change in generating positive mental health outcomes are mapped out by understanding the mood-moderating chemicals, tryptophan, tyrosine, indole-2-lactic acid, and others. In the end, studies about using healthy diets, such as the Mediterranean diet, and the Japanese diet, as a means of treatment are cited to testify to the progress scientists have had so far. Scientists have begun to write dietary guidelines for depressed patients. It is safe to say that most people know the importance of eating healthily. Eating better should be a universal public health intervention not because it helps patients with mental illness but because eating better makes people healthier in the long run.
References
[1]. WHO, "Mental disorders", 08 June 2020, https://www.who.int/news-room/fact-sheets/detail/mental-disorders, (Accessed 1st Oct 2022).
[2]. WHO, "Mental Health and COVID-19: Early evidence of the pandemic’s impact: Scientific brief, 2 March 2022," (2022).
[3]. R. T. Mulder,C. M. Frampton, "Outcome of mood disorders before psychopharmacology: A systematic review," Australian & New Zealand Journal of Psychiatry, 48(3), 224-236 (2014).
[4]. A. Martin, C. Young, J. F. Leckman, et al., "Age effects on antidepressant-induced manic conversion," Arch Pediatr Adolesc Med, 158(8), 773-80 (2004).
[5]. M. Carabotti, A. Scirocco, M. A. Maselli, et al., "The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems," Ann Gastroenterol, 28(2), 203-209 (2015).
[6]. R. J. Wurtman, "Tryptophan," (2004).
[7]. M. Briguglio, B. Dell'Osso, G. Panzica, et al., "Dietary Neurotransmitters: A Narrative Review on Current Knowledge," Nutrients, 10(5) (2018).
[8]. O. Akimitsu, K. Wada, T. Noji, et al., "The relationship between consumption of tyrosine and phenylalanine as precursors of catecholamine at breakfast and the circadian typology and mental health in Japanese infants aged 2 to 5 years," Journal of Physiological Anthropology, 32(1), 13 (2013).
[9]. B. H. Lee, B. Hille,D.-S. Koh, "Serotonin modulates melatonin synthesis as an autocrine neurotransmitter in the pineal gland," Proceedings of the National Academy of Sciences, 118(43), e2113852118 (2021).
[10]. J. H. Medicine, "Take Your Diet to the Mediterranean," (2022).
[11]. T. Psaltopoulou, T. N. Sergentanis, D. B. Panagiotakos, et al., "Mediterranean diet, stroke, cognitive impairment, and depression: A meta-analysis," Ann Neurol, 74(4), 580-91 (2013).
[12]. Y. Li, M. R. Lv, Y. J. Wei, et al., "Dietary patterns and depression risk: A meta-analysis," Psychiatry Res, 253, 373-382 (2017).
[13]. J. S. Lai, S. Hiles, A. Bisquera, et al., "A systematic review and meta-analysis of dietary patterns and depression in community-dwelling adults," Am J Clin Nutr, 99(1), 181-97 (2014).
[14]. T. S. Böbel, S. B. Hackl, D. Langgartner, et al., "Less immune activation following social stress in rural vs. urban participants raised with regular or no animal contact, respectively," Proceedings of the National Academy of Sciences, 115(20), 5259-5264 (2018).
[15]. F. N. Jacka, A. O'Neil, R. Opie, et al., "A randomised controlled trial of dietary improvement for adults with major depression (the 'SMILES' trial)," BMC Med, 15(1), 23 (2017).
[16]. A. Sánchez-Villegas, M. A. Martínez-González, R. Estruch, et al., "Mediterranean dietary pattern and depression: the PREDIMED randomized trial," BMC Medicine, 11(1), 208 (2013).
Cite this article
Que,J. (2023). Treating Mental Illness with Dietary Improvement. Theoretical and Natural Science,4,65-71.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 2nd International Conference on Biological Engineering and Medical Science (ICBioMed 2022), Part II
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. WHO, "Mental disorders", 08 June 2020, https://www.who.int/news-room/fact-sheets/detail/mental-disorders, (Accessed 1st Oct 2022).
[2]. WHO, "Mental Health and COVID-19: Early evidence of the pandemic’s impact: Scientific brief, 2 March 2022," (2022).
[3]. R. T. Mulder,C. M. Frampton, "Outcome of mood disorders before psychopharmacology: A systematic review," Australian & New Zealand Journal of Psychiatry, 48(3), 224-236 (2014).
[4]. A. Martin, C. Young, J. F. Leckman, et al., "Age effects on antidepressant-induced manic conversion," Arch Pediatr Adolesc Med, 158(8), 773-80 (2004).
[5]. M. Carabotti, A. Scirocco, M. A. Maselli, et al., "The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems," Ann Gastroenterol, 28(2), 203-209 (2015).
[6]. R. J. Wurtman, "Tryptophan," (2004).
[7]. M. Briguglio, B. Dell'Osso, G. Panzica, et al., "Dietary Neurotransmitters: A Narrative Review on Current Knowledge," Nutrients, 10(5) (2018).
[8]. O. Akimitsu, K. Wada, T. Noji, et al., "The relationship between consumption of tyrosine and phenylalanine as precursors of catecholamine at breakfast and the circadian typology and mental health in Japanese infants aged 2 to 5 years," Journal of Physiological Anthropology, 32(1), 13 (2013).
[9]. B. H. Lee, B. Hille,D.-S. Koh, "Serotonin modulates melatonin synthesis as an autocrine neurotransmitter in the pineal gland," Proceedings of the National Academy of Sciences, 118(43), e2113852118 (2021).
[10]. J. H. Medicine, "Take Your Diet to the Mediterranean," (2022).
[11]. T. Psaltopoulou, T. N. Sergentanis, D. B. Panagiotakos, et al., "Mediterranean diet, stroke, cognitive impairment, and depression: A meta-analysis," Ann Neurol, 74(4), 580-91 (2013).
[12]. Y. Li, M. R. Lv, Y. J. Wei, et al., "Dietary patterns and depression risk: A meta-analysis," Psychiatry Res, 253, 373-382 (2017).
[13]. J. S. Lai, S. Hiles, A. Bisquera, et al., "A systematic review and meta-analysis of dietary patterns and depression in community-dwelling adults," Am J Clin Nutr, 99(1), 181-97 (2014).
[14]. T. S. Böbel, S. B. Hackl, D. Langgartner, et al., "Less immune activation following social stress in rural vs. urban participants raised with regular or no animal contact, respectively," Proceedings of the National Academy of Sciences, 115(20), 5259-5264 (2018).
[15]. F. N. Jacka, A. O'Neil, R. Opie, et al., "A randomised controlled trial of dietary improvement for adults with major depression (the 'SMILES' trial)," BMC Med, 15(1), 23 (2017).
[16]. A. Sánchez-Villegas, M. A. Martínez-González, R. Estruch, et al., "Mediterranean dietary pattern and depression: the PREDIMED randomized trial," BMC Medicine, 11(1), 208 (2013).









