1. Introduction
Based on the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV), Attention-Deficit/Hyperactivity Disorder (ADHD) is a prevalent mental condition arisen from childhood, affecting 3-7% of children of school age [1]. in 2007. According to the American Psychiatric Association [2], ADHD is characterised by a continuous inattention and hyperactivity, associated with many cognitive-behavioral problems, including poor academic achievement, conduct difficulties and aggressive behaviours etc. Longitudinal study conducted on children diagnosed with ADHD has shown that the early development and persisting behaviour of long-term physical aggression represent the most significant prognostic indicator for children to develop disruptive behaviour problems, characterological disturbances such as borderline personality disorder or antisocial personality disorder [3].
In the last ten years, MRI has been used to compare the anatomical differences between ADHD and observe children in different brain areas. Much focus has been paid to the investigation of neuronal circuits that establish connections between the prefrontal cortex and the basal ganglia, which are believed are important in the control of response inhibition. In particular, frontostriatal(striatum) abnormalities as well as dysfunction of dorsoanterior cingulate cortex (CCdA) were examined [4]. Similarly, a difference between prefrontal control and hyper-responsivity of the amygdala systems was found in aggressive individuals. Additionally, variation in the volume of white matter [5], the cerebellum [6], as well as the corpus callosum [7], has also been shown to be closely linked to abnormal executing functions. According to McKAY and Halperin[8], there underlies a hypothesis suggesting that the existence of an underlying impulsive personality, along with cognitive deficiencies in ADHD children, has a substantial role in predicting a dismal prognosis and increasing the probability of engaging in serious aggressive adult behaviour. This set of behaviours seems to be influenced, to some extent, with regards to the serotonergic system, and children with aggressive ADHD who exhibit signs of reduced serotonergic function tend to be more susceptible to the negative impacts of stresses.
Many researches has reported hypoactivation of the striatum in ADHD children, which was believed to exhibit numerous neuronal connections with many prefrontal regions and particularly front striatal loops [9]. Another research supporting the relation between frontal and striatal variations with ADHD was the hyperactivation of the frontal cortex along with hypoactivation of the striatum during go/no-go task [10]. Similarly, the study by Bush et al. [11], revealed the presence of bilateral activation in the ventrolateral prefrontal cortex among children diagnosed with ADHD when doing Counting Stroop tasks. This finding stands in contrast to the absence of such activation seen in the control group.
Although the interpretation of prefrontal abnormalities, characterized by either hyper/hypoactivation, vary across various studies attributed to the use of distinct experimental paradigms or the diversity of prefrontal areas under investigation, such as the dorsolateral and ventro-orbital regions. Nevertheless, the malfunction of the dorsoanterior cingulate cortex (CCdA) is frequently reported as one of the most prevalent fMRI results, due to its close association with attention, target recognition, response selection, and inhibition, as highlighted by Emond et al. [12]. The Counting Stroop task, as conducted by Zang et al. [13], suggested the hypoactivation of CCdA in individuals diagnosed with ADHD. On the contrary, Schulz et al. [14] performed a research which yielded results indicating that the activation of these areas actually increased during inhibition in teenagers who had been diagnosed with ADHD for the go/no-go test. This persumably indicates a correlation between the typical decline in behavioural symptoms of ADHD throughout adolescence and a positive regression of frontal hypoactivations.
Additionally, multiple studies have consistently shown a decrease in the volume of the corpus callosum in patients diagnosed with ADHD. Nevertheless, there is variation in the specific regions of the corpus callosum impacted, as shown across different studies. An anterior reduction was reported by Baumgardner et al. [15], whereas Semrud-Clikeman et al. [16] found the reverse. This is suggested that individuals with ADHD may have a greater impact on the anterior region of the corpus callosum, derived from the understanding that the anterior portion mostly consists of axons [17]. Several MRI studies also showed a decrease in the cerebellum or overall cerebellar volume [18] and white matter (WM) abnormalities [19].
2. Link between Aggression and ADHD
There are several studies which establish the connection between Aggression and attention deficit/hyperactivity disorder (ADHD). A study on whether comorbidity is important by Gonzalez et al., states that the disorder is related with violent behaviors including aggression [20]. One possible correlation between the two comorbidity is the problems in neurodevelopmental. ADHD symptoms are observed through their parallel progression when compared to the development in the control processes which is mediated by the prefrontal cortex [21]. Similarly, behavioral inhibitions like controlling impulsive outbursts is as a result of abnormalities in the orbitofrontal cortex [22]. The neurodevelopmental link is attributed to the alterations in the structural or functional maturation of the brain areas. Imaging results indicate that children with ADHD have a decrease in thickness of the temporal pole cortical [23]. This underdevelopment in the cortex region is also cited to be responsible for emotion regulations which can result in impulsivity like aggression behavior [24].
A study on impulsive aggression and ADHD also indicated that dysfunctional response inhibition was present in both comorbidities. Issues and deficits in the pre-frontal development were observed in both ADHD and impulsive aggression [25]. A multivariate analysis on aggression in child-patients with ADHD indicated that a reduced cortical thickness and the reduced volume of frontal-accumbal in children with ADHD correlated with the presence of aggression disorder [26]. A deficient in the inhibitory control mechanisms as a result of differential activation in insula and middle temporal sulcus was also observed in children with both ADHD and disruptive behaviours like aggression [27].
Differential developments in central serotonergic (5-HT) in children and adolescent as a link between ADHD and aggression [28]. The serotonin acts as a regulator for the pre-frontal cortex which then controls the individual’s response to external stimuli. Low 5-HT is associated with impulsive aggression while high 5-HT linked with cognitive impulsiveness in children with ADHD [29]. The symptoms presented for both disorders also indicate the correlation between the two. For instance, behavioral problems like hot/short temper as a feature of impulsive aggression observed in ADHD [30]. There are also disruptive behavioral problems observed in ADHD as it is in aggression [31]. According to Puiu et al., the intersecting symptoms and features of both disorders is because of the neurobiological framework in both ADHD and aggression as indicated in the figure below [25].
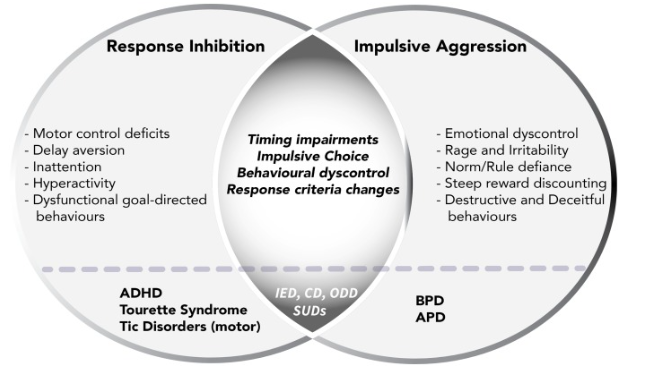
Figure 1. Neurobiological framework in ADHD and Aggression [25].
Links between ADHD and aggression have also been linked to COMT genotype. The genotype is responsible for emotional processing. According to a study by Villemonteix et al., the COMT genotype results in impairments in empathy for fear and response inhibition which then means that the genotype acts as a mediating factor in the correlation between aggression and ADHD [32]. COMT Val alleles make an individual to stop responding to positive stimuli in the environment. Aggression is thus considered as an additional symptom to children who already have the alleles that contributes to phenotypic variations leading to ADHD [33].
3. Medication to Disrupt the Correlation between ADHD and Aggression
There are less studies and evidence to indicate that medication can cure both ADHD and aggression. Studies however do indicate that medication can be used to cure aggression in children with ADHD hence aiding in disrupting the link between the two. According to Rucklidge (2018), the use of micronutrients could be used for emotional regulation and reduce aggression in children with ADHD. Such treatment options are based on targeting the hyperactivity/impulsivity levels in ADHD children and aggression due to benefits of the micronutrients have on psychological functioning [34]. Based on improving psychological functioning, medication can also target to disrupt the genetic risks in aggression outcomes in children with ADHD. This is conluded on COMT genotype and its associated link in mediating the emotional functions of children with aggression and ADHD. Thus, the treatment and medication targets COMT Val158Met which then regulates the psychological response and link between aggression outcomes in children with ADHD [35].
Other stimulants like amphetamine and pemoline are capable of treating ADHD [36,37], but reliable evidence of which have an impact on ADHD patients with aggressive behaviors can hardly be found. However, since aggression in children with ADHD is considered a comorbid disorder, stimulants treatment is considered only after behavioral treatment is proved to be ineffective. Thus, treating behaviour can be used in disrupting the correlation between aggression and ADHD [38], treating aggressive behaviors first before ADHD is treated. The figure below indicates an example of psychopharmalogical treatment of ADHD with aggression where stimulants treatment is only considered after the first stage of behavioral treatment [39].
Study on Divalproex treatment in children with ADHD and aggression indicates that aggression remits after 8 weeks for cases of chronic aggression [40]. Divalproex is used as an additional medication in instances where the stimulant medication does not effectively disrupt the correlation between ADHD and aggression. The use of stimulants medication does not lead to reduced aggression to satisfactory levels [41]. Divalproex is an antipsychotic medication that is regarded as an additional level to disrupt the ADHD and aggression correlation by acting as a mood stabilizer for enhancing behavioral stability. Divalproex sodium is very useful as a psychopharmacologic treatment of conduct disorder [42], hence why its application in aggression is regarded as an additional level to disrupting the correlation of aggression in ADHD where stimulants prove ineffective. The use of Divalproex lead to positive response from 12 out of the 15 subjects treated which provides evidence that it can be used as an effective treatment for aggressive behaviors in patients with ADHD [43].
In disrupting the correlation, the medication is administered to target aggression specifically before ADHD is treated [44]. This is especially when the ADHD is associated with maladaptive aggression which does not respond to either stimulants or behavioral treatment. Treating each disorder separately is aimed at ensuring that successful treatment of one disorder will have a positive impact on the associated disorders. For instance, medication for successfully treating ADHD assumed to have a positive impact on impulsive aggression hence treating both [45].
4. Conclusion
The correlation between ADHD and aggression is established through neurodevelopmental deficits, neurobiological features, genotype, and differentials in serotonergic. Based on the neurobiological framework, the link between ADHD and aggression is based on the intersecting features of response inhibitors and ADHD. This therefore suggests that aggression in individuals with ADHD occurs as external symptom. Based on neurodevelopmental issues, the link between aggression and ADHD is based on the underdevelopment in the brain regions which controls both disorders. The cortical thickness as well as the levels of serotonin in the brain is also attributed as a contributing factor establishing the correlation between the two disorders.
There are some clinical trials that indicate a medication that can treat both ADHD and aggression. The most common medication for disrupting the link is the use of stimulants and non-stimulants which are used in treating ADHD, the reduced aggression levels are attributed to effective treatment results in ADHD. Antipsychotic medications are used in treating aggression in cases of maladaptive aggression which does not respond to stimulants. Hence, the goal is to treat one disorder (ADHD) and use other combinations like behavioral treatment to reduce the levels of aggression.
References
[1]. American Psychiatric Association, 2000. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR), 4th ed. American Psychiatric Association, Arlington, VA.
[2]. Anderson, S.W., Barrash, J., Bechara, A., Tranel, D., 2006. Impairments of emotion and real-world complex behavior following childhood- or adult-onset damage to ventromedial prefrontal cortex. J. Int. Neuropsychol. Soc. JINS 12, 224–235.
[3]. Baumgardner, T.L., Singer, H.S., Denckla, M.B., Rubin, M.A., Abrams, M.T., Colli, M.J., Reiss, A.L., 1996. Corpus callosum morphology in children with Tourette syndrome and attention deficit hyperactivity disorder. Neurology 47, 477–482.
[4]. Bush, G., Frazier, J.A., Rauch, S.L., Seidman, L.J., Whalen, P.J., Jenike, M.A., Rosen, B.R., Biederman, J., 1999. Anterior cingulate cortex dysfunction in attention-deficit/hyperactivity disorder revealed by fMRI and the counting stroop. Biol. Psychiatry 45, 1542–1552.
[5]. Castellanos, F.X., 2002. Developmental Trajectories of Brain Volume Abnormalities in Children and Adolescents With Attention-Deficit/Hyperactivity Disorder. JAMA 288, 1740.
[6]. Castellanos, F.X., 1996. Quantitative Brain Magnetic Resonance Imaging in Attention-Deficit Hyperactivity Disorder. Arch. Gen. Psychiatry 53, 607.
[7]. Durston, S., Tottenham, N.T., Thomas, K.M., Davidson, M.C., Eigsti, I.-M., Yang, Y., Ulug, A.M., Casey, B.J., 2003. Differential patterns of striatal activation in young children with and without ADHD. Biol. Psychiatry 53, 871–878.
[8]. Emond, V., Joyal, C., Poissant, H., 2009. Neuroanatomie structurelle et fonctionnelle du trouble déficitaire d’attention avec ou sans hyperactivité (TDAH). L’Encéphale 35, 107–114.
[9]. Hazlett, E.A., New, A.S., Newmark, R., Haznedar, M.M., Lo, J.N., Speiser, L.J., Chen, A.D., Mitropoulou, V., Minzenberg, M., Siever, L.J., Buchsbaum, M.S., 2005. Reduced anterior and posterior cingulate gray matter in borderline personality disorder. Biol. Psychiatry 58, 614–623.
[10]. Konrad, K., Neufang, S., Hanisch, C., Fink, G.R., Herpertz-Dahlmann, B., 2006. Dysfunctional Attentional Networks in Children with Attention Deficit/Hyperactivity Disorder: Evidence from an Event-Related Functional Magnetic Resonance Imaging Study. Biol. Psychiatry 59, 643–651.
[11]. Krain, A.L., Castellanos, F.X., 2006. Brain development and ADHD. Clin. Psychol. Rev. 26, 433–444.
[12]. Bush, G., Frazier, J.A., Rauch, S.L., Seidman, L.J., Whalen, P.J., Jenike, M.A., Rosen, B.R., Biederman, J., 1999. Anterior cingulate cortex dysfunction in attention-deficit/hyperactivity disorder revealed by fMRI and the counting stroop. Biol. Psychiatry 45, 1542–1552.
[13]. Loeber, R., Wung, P., Keenan, K., Giroux, B., Stouthamer-Loeber, M., Van Kammen, W.B., Maugham, B., 1993. Developmental pathways in disruptive child behavior. Dev. Psychopathol. 5, 103–133.
[14]. Raine, A., Ishikawa, S.S., Arce, E., Lencz, T., Knuth, K.H., Bihrle, S., LaCasse, L., Colletti, P., 2004. Hippocampal structural asymmetry in unsuccessful psychopaths. Biol. Psychiatry 55, 185–191.
[15]. Raine, A., Lencz, T., Bihrle, S., LaCasse, L., Colletti, P., 2000. Reduced prefrontal gray matter volume and reduced autonomic activity in antisocial personality disorder. Arch. Gen. Psychiatry 57, 119–127; discussion 128-129.
[16]. Raine, A., Lencz, T., Bihrle, S., LaCasse, L., Colletti, P., 2000. Reduced prefrontal gray matter volume and reduced autonomic activity in antisocial personality disorder. Arch. Gen. Psychiatry 57, 119–127; discussion 128-129.
[17]. Hazlett, E.A., New, A.S., Newmark, R., Haznedar, M.M., Lo, J.N., Speiser, L.J., Chen, A.D., Mitropoulou, V., Minzenberg, M., Siever, L.J., Buchsbaum, M.S., 2005. Reduced anterior and posterior cingulate gray matter in borderline personality disorder. Biol. Psychiatry 58, 614–623.
[18]. Semrud-Clikeman, M., Steingard, R.J., Filipek, P., Biederman, J., Bekken, K., Renshaw, P.F., 2000. Using MRI to Examine Brain-Behavior Relationships in Males With Attention Deficit Disorder With Hyperactivity. J. Am. Acad. Child Adolesc. Psychiatry 39, 477–484.
[19]. Castellanos, F.X., 2002. Developmental Trajectories of Brain Volume Abnormalities in Children and Adolescents With Attention-Deficit/Hyperactivity Disorder. JAMA 288, 1740.
[20]. González, R. A., Kallis, C., & Coid, J. W. (2013). Adult attention deficit hyperactivity disorder and violence in the population of England: does comorbidity matter?. PLoS one, 8(9), e75575.
[21]. Vaidya, C. J. (2012). Neurodevelopmental abnormalities in ADHD. Behavioral neuroscience of attention deficit hyperactivity disorder and its treatment, 49-66.
[22]. Sugden, S. G., Kile, S. J., & Hendren, R. L. (2006). Neurodevelopmental pathways to aggression: a model to understand and target treatment in youth. The Journal of neuropsychiatry and clinical neurosciences, 18(3), 302-317.
[23]. Hoogman, M., Muetzel, R., Guimaraes, J. P., Shumskaya, E., Mennes, M., Zwiers, M. P., ... & Franke, B. (2019). Brain imaging of the cortex in ADHD: a coordinated analysis of large-scale clinical and population-based samples. American Journal of Psychiatry, 176(7), 531-542.
[24]. Sarkheil, P., Klasen, M., Schneider, F., Goebel, R., & Mathiak, K. (2019). Amygdala response and functional connectivity during cognitive emotion regulation of aversive image sequences. European archives of psychiatry and clinical neuroscience, 269, 803-811.
[25]. Puiu, A. A., Wudarczyk, O., Goerlich, K. S., Votinov, M., Herpertz-Dahlmann, B., Turetsky, B., & Konrad, K. (2018). Impulsive aggression and response inhibition in attention-deficit/hyperactivity disorder and disruptive behavioral disorders: Findings from a systematic review. Neuroscience & biobehavioral reviews, 90, 231-246.
[26]. Cha, J., Fekete, T., Siciliano, F., Biezonski, D., Greenhill, L., Pliszka, S. R., ... & Posner, J. (2015). Neural correlates of aggression in medication-naive children with ADHD: multivariate analysis of morphometry and tractography. Neuropsychopharmacology, 40(7), 1717-1725.
[27]. Bubenzer‐Busch, S., Herpertz‐Dahlmann, B., Kuzmanovic, B., Gaber, T. J., Helmbold, K., Ullisch, M. G., ... & Zepf, F. D. (2016). Neural correlates of reactive aggression in children with attention‐deficit/hyperactivity disorder and comorbid disruptive behaviour disorders. Acta Psychiatrica Scandinavica, 133(4), 310-323.
[28]. Halperin, J. M., Newcorn, J. H., Schwartz, S. T., Sharma, V., Siever, L. J., Koda, V. H., & Gabriel, S. (1997). Age-related changes in the association between serotonergic function and aggression in boys with ADHD. Biological psychiatry, 41(6), 682-689.
[29]. Oades, R. D., Lasky-Su, J., Christiansen, H., Faraone, S. V., Sonuga-Barke, E. J., Banaschewski, T., ... & Asherson, P. (2008). The influence of serotonin-and other genes on impulsive behavioral aggression and cognitive impulsivity in children with attention-deficit/hyperactivity disorder (ADHD): Findings from a family-based association test (FBAT) analysis. Behavioral and Brain Functions, 4, 1-14.
[30]. Dowson, J. H., & Blackwell, A. D. (2010). Impulsive aggression in adults with attention‐deficit/hyperactivity disorder. Acta Psychiatrica Scandinavica, 121(2), 103-110.
[31]. Young, S., Gudjonsson, G., Ball, S., & Lam, J. (2003). Attention Deficit Hyperactivity Disorder (ADHD) in personality disordered offenders and the association with disruptive behavioural problems. The Journal of Forensic Psychiatry, 14(3), 491-505.
[32]. Villemonteix, T., De Brito, S. A., Slama, H., Kavec, M., Balériaux, D., Metens, T., ... & Massat, I. (2015). Structural correlates of COMT Val158Met polymorphism in childhood ADHD: a voxel-based morphometry study. The World Journal of Biological Psychiatry, 16(3), 190-199.
[33]. Caspi, A., Langley, K., Milne, B., Moffitt, T. E., O’Donovan, M., Owen, M. J., ... & Thapar, A. (2008). A replicated molecular genetic basis for subtyping antisocial behavior in children with attention-deficit/hyperactivity disorder. Archives of general psychiatry, 65(2), 203-210.
[34]. Rucklidge, J. J., Eggleston, M. J., Johnstone, J. M., Darling, K., & Frampton, C. M. (2018). Vitamin‐mineral treatment improves aggression and emotional regulation in children with ADHD: a fully blinded, randomized, placebo‐controlled trial. Journal of Child Psychology and Psychiatry, 59(3), 232-246.
[35]. Van Goozen, S. H., Langley, K., Northover, C., Hubble, K., Rubia, K., Schepman, K., ... & Thapar, A. (2016). Identifying mechanisms that underlie links between COMT genotype and aggression in male adolescents with ADHD. Journal of child psychology and psychiatry, 57(4), 472-480.
[36]. Castells X, Blanco-Silvente L, Cunill R. Amphetamines for attention deficit hyperactivity disorder (ADHD) in adults. Cochrane Database Syst Rev. 2018 Aug 9;8(8):CD007813.
[37]. Bostic JQ, Biederman J, Spencer TJ, Wilens TE, Prince JB, Monuteaux MC, Sienna M, Polisner DA, Hatch M. Pemoline treatment of adolescents with attention deficit hyperactivity disorder: a short-term controlled trial. J Child Adolesc Psychopharmacol. 2000 Fall;10(3):205-16
[38]. Harty, S. C., Miller, C. J., Newcorn, J. H., & Halperin, J. M. (2009). Adolescents with childhood ADHD and comorbid disruptive behavior disorders: aggression, anger, and hostility. Child psychiatry and human development, 40, 85-97.
[39]. Pliszka, S. R., Crismon, M. L., Hughes, C. W., Corners, C. K., Emslie, G. J., Jensen, P. S., ... & HYPERACTIVITY, P. O. C. A. D. (2006). The Texas Children’s Medication Algorithm Project: revision of the algorithm for pharmacotherapy of attention-deficit/hyperactivity disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 45(6), 642-657.
[40]. Blader, J. C., Schooler, N. R., Jensen, P. S., Pliszka, S. R., & Kafantaris, V. (2009). Adjunctive divalproex versus placebo for children with ADHD and aggression refractory to stimulant monotherapy. American Journal of Psychiatry, 166(12), 1392-1401.
[41]. Jensen, P. S., Hinshaw, S. P., Kraemer, H. C., Lenora, N., Newcorn, J. H., Abikoff, H. B., ... & Vitiello, B. (2001). ADHD comorbidity findings from the MTA study: comparing comorbid subgroups. Journal of the American Academy of Child & Adolescent Psychiatry, 40(2), 147-158.
[42]. Jensen, P. S., Hinshaw, S. P., Kraemer, H. C., Lenora, N., Newcorn, J. H., Abikoff, H. B., ... & Vitiello, B. (2001). ADHD comorbidity findings from the MTA study: comparing comorbid subgroups. Journal of the American Academy of Child & Adolescent Psychiatry, 40(2), 147-158.
[43]. Donovan, S. J., Stewart, J. W., Nunes, E. V., Quitkin, F. M., Parides, M., Daniel, W., ... & Klein, D. F. (2000). Divalproex treatment for youth with explosive temper and mood lability: a double-blind, placebo-controlled crossover design. American Journal of Psychiatry, 157(5), 818-820.
[44]. Saylor, K. E., & Amann, B. H. (2016). Impulsive aggression as a comorbidity of attention-deficit/hyperactivity disorder in children and adolescents. Journal of child and adolescent psychopharmacology, 26(1), 19-25.
[45]. Pappadopulos, E., Macintyre Ii, J. C., Crismon, M. L., Findling, R. L., Malone, R. P., Derivan, A., ... & Jensen, P. S. (2003). Treatment recommendations for the use of antipsychotics for aggressive youth (TRAAY). Part II. Journal of the American Academy of Child & Adolescent Psychiatry, 42(2), 145-161.
Cite this article
Wang,T. (2024). Medication affecting the correlation of aggression development and Attention-Deficit/Hyperactivity Disorder (ADHD). Theoretical and Natural Science,44,254-260.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 2nd International Conference on Modern Medicine and Global Health
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. American Psychiatric Association, 2000. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR), 4th ed. American Psychiatric Association, Arlington, VA.
[2]. Anderson, S.W., Barrash, J., Bechara, A., Tranel, D., 2006. Impairments of emotion and real-world complex behavior following childhood- or adult-onset damage to ventromedial prefrontal cortex. J. Int. Neuropsychol. Soc. JINS 12, 224–235.
[3]. Baumgardner, T.L., Singer, H.S., Denckla, M.B., Rubin, M.A., Abrams, M.T., Colli, M.J., Reiss, A.L., 1996. Corpus callosum morphology in children with Tourette syndrome and attention deficit hyperactivity disorder. Neurology 47, 477–482.
[4]. Bush, G., Frazier, J.A., Rauch, S.L., Seidman, L.J., Whalen, P.J., Jenike, M.A., Rosen, B.R., Biederman, J., 1999. Anterior cingulate cortex dysfunction in attention-deficit/hyperactivity disorder revealed by fMRI and the counting stroop. Biol. Psychiatry 45, 1542–1552.
[5]. Castellanos, F.X., 2002. Developmental Trajectories of Brain Volume Abnormalities in Children and Adolescents With Attention-Deficit/Hyperactivity Disorder. JAMA 288, 1740.
[6]. Castellanos, F.X., 1996. Quantitative Brain Magnetic Resonance Imaging in Attention-Deficit Hyperactivity Disorder. Arch. Gen. Psychiatry 53, 607.
[7]. Durston, S., Tottenham, N.T., Thomas, K.M., Davidson, M.C., Eigsti, I.-M., Yang, Y., Ulug, A.M., Casey, B.J., 2003. Differential patterns of striatal activation in young children with and without ADHD. Biol. Psychiatry 53, 871–878.
[8]. Emond, V., Joyal, C., Poissant, H., 2009. Neuroanatomie structurelle et fonctionnelle du trouble déficitaire d’attention avec ou sans hyperactivité (TDAH). L’Encéphale 35, 107–114.
[9]. Hazlett, E.A., New, A.S., Newmark, R., Haznedar, M.M., Lo, J.N., Speiser, L.J., Chen, A.D., Mitropoulou, V., Minzenberg, M., Siever, L.J., Buchsbaum, M.S., 2005. Reduced anterior and posterior cingulate gray matter in borderline personality disorder. Biol. Psychiatry 58, 614–623.
[10]. Konrad, K., Neufang, S., Hanisch, C., Fink, G.R., Herpertz-Dahlmann, B., 2006. Dysfunctional Attentional Networks in Children with Attention Deficit/Hyperactivity Disorder: Evidence from an Event-Related Functional Magnetic Resonance Imaging Study. Biol. Psychiatry 59, 643–651.
[11]. Krain, A.L., Castellanos, F.X., 2006. Brain development and ADHD. Clin. Psychol. Rev. 26, 433–444.
[12]. Bush, G., Frazier, J.A., Rauch, S.L., Seidman, L.J., Whalen, P.J., Jenike, M.A., Rosen, B.R., Biederman, J., 1999. Anterior cingulate cortex dysfunction in attention-deficit/hyperactivity disorder revealed by fMRI and the counting stroop. Biol. Psychiatry 45, 1542–1552.
[13]. Loeber, R., Wung, P., Keenan, K., Giroux, B., Stouthamer-Loeber, M., Van Kammen, W.B., Maugham, B., 1993. Developmental pathways in disruptive child behavior. Dev. Psychopathol. 5, 103–133.
[14]. Raine, A., Ishikawa, S.S., Arce, E., Lencz, T., Knuth, K.H., Bihrle, S., LaCasse, L., Colletti, P., 2004. Hippocampal structural asymmetry in unsuccessful psychopaths. Biol. Psychiatry 55, 185–191.
[15]. Raine, A., Lencz, T., Bihrle, S., LaCasse, L., Colletti, P., 2000. Reduced prefrontal gray matter volume and reduced autonomic activity in antisocial personality disorder. Arch. Gen. Psychiatry 57, 119–127; discussion 128-129.
[16]. Raine, A., Lencz, T., Bihrle, S., LaCasse, L., Colletti, P., 2000. Reduced prefrontal gray matter volume and reduced autonomic activity in antisocial personality disorder. Arch. Gen. Psychiatry 57, 119–127; discussion 128-129.
[17]. Hazlett, E.A., New, A.S., Newmark, R., Haznedar, M.M., Lo, J.N., Speiser, L.J., Chen, A.D., Mitropoulou, V., Minzenberg, M., Siever, L.J., Buchsbaum, M.S., 2005. Reduced anterior and posterior cingulate gray matter in borderline personality disorder. Biol. Psychiatry 58, 614–623.
[18]. Semrud-Clikeman, M., Steingard, R.J., Filipek, P., Biederman, J., Bekken, K., Renshaw, P.F., 2000. Using MRI to Examine Brain-Behavior Relationships in Males With Attention Deficit Disorder With Hyperactivity. J. Am. Acad. Child Adolesc. Psychiatry 39, 477–484.
[19]. Castellanos, F.X., 2002. Developmental Trajectories of Brain Volume Abnormalities in Children and Adolescents With Attention-Deficit/Hyperactivity Disorder. JAMA 288, 1740.
[20]. González, R. A., Kallis, C., & Coid, J. W. (2013). Adult attention deficit hyperactivity disorder and violence in the population of England: does comorbidity matter?. PLoS one, 8(9), e75575.
[21]. Vaidya, C. J. (2012). Neurodevelopmental abnormalities in ADHD. Behavioral neuroscience of attention deficit hyperactivity disorder and its treatment, 49-66.
[22]. Sugden, S. G., Kile, S. J., & Hendren, R. L. (2006). Neurodevelopmental pathways to aggression: a model to understand and target treatment in youth. The Journal of neuropsychiatry and clinical neurosciences, 18(3), 302-317.
[23]. Hoogman, M., Muetzel, R., Guimaraes, J. P., Shumskaya, E., Mennes, M., Zwiers, M. P., ... & Franke, B. (2019). Brain imaging of the cortex in ADHD: a coordinated analysis of large-scale clinical and population-based samples. American Journal of Psychiatry, 176(7), 531-542.
[24]. Sarkheil, P., Klasen, M., Schneider, F., Goebel, R., & Mathiak, K. (2019). Amygdala response and functional connectivity during cognitive emotion regulation of aversive image sequences. European archives of psychiatry and clinical neuroscience, 269, 803-811.
[25]. Puiu, A. A., Wudarczyk, O., Goerlich, K. S., Votinov, M., Herpertz-Dahlmann, B., Turetsky, B., & Konrad, K. (2018). Impulsive aggression and response inhibition in attention-deficit/hyperactivity disorder and disruptive behavioral disorders: Findings from a systematic review. Neuroscience & biobehavioral reviews, 90, 231-246.
[26]. Cha, J., Fekete, T., Siciliano, F., Biezonski, D., Greenhill, L., Pliszka, S. R., ... & Posner, J. (2015). Neural correlates of aggression in medication-naive children with ADHD: multivariate analysis of morphometry and tractography. Neuropsychopharmacology, 40(7), 1717-1725.
[27]. Bubenzer‐Busch, S., Herpertz‐Dahlmann, B., Kuzmanovic, B., Gaber, T. J., Helmbold, K., Ullisch, M. G., ... & Zepf, F. D. (2016). Neural correlates of reactive aggression in children with attention‐deficit/hyperactivity disorder and comorbid disruptive behaviour disorders. Acta Psychiatrica Scandinavica, 133(4), 310-323.
[28]. Halperin, J. M., Newcorn, J. H., Schwartz, S. T., Sharma, V., Siever, L. J., Koda, V. H., & Gabriel, S. (1997). Age-related changes in the association between serotonergic function and aggression in boys with ADHD. Biological psychiatry, 41(6), 682-689.
[29]. Oades, R. D., Lasky-Su, J., Christiansen, H., Faraone, S. V., Sonuga-Barke, E. J., Banaschewski, T., ... & Asherson, P. (2008). The influence of serotonin-and other genes on impulsive behavioral aggression and cognitive impulsivity in children with attention-deficit/hyperactivity disorder (ADHD): Findings from a family-based association test (FBAT) analysis. Behavioral and Brain Functions, 4, 1-14.
[30]. Dowson, J. H., & Blackwell, A. D. (2010). Impulsive aggression in adults with attention‐deficit/hyperactivity disorder. Acta Psychiatrica Scandinavica, 121(2), 103-110.
[31]. Young, S., Gudjonsson, G., Ball, S., & Lam, J. (2003). Attention Deficit Hyperactivity Disorder (ADHD) in personality disordered offenders and the association with disruptive behavioural problems. The Journal of Forensic Psychiatry, 14(3), 491-505.
[32]. Villemonteix, T., De Brito, S. A., Slama, H., Kavec, M., Balériaux, D., Metens, T., ... & Massat, I. (2015). Structural correlates of COMT Val158Met polymorphism in childhood ADHD: a voxel-based morphometry study. The World Journal of Biological Psychiatry, 16(3), 190-199.
[33]. Caspi, A., Langley, K., Milne, B., Moffitt, T. E., O’Donovan, M., Owen, M. J., ... & Thapar, A. (2008). A replicated molecular genetic basis for subtyping antisocial behavior in children with attention-deficit/hyperactivity disorder. Archives of general psychiatry, 65(2), 203-210.
[34]. Rucklidge, J. J., Eggleston, M. J., Johnstone, J. M., Darling, K., & Frampton, C. M. (2018). Vitamin‐mineral treatment improves aggression and emotional regulation in children with ADHD: a fully blinded, randomized, placebo‐controlled trial. Journal of Child Psychology and Psychiatry, 59(3), 232-246.
[35]. Van Goozen, S. H., Langley, K., Northover, C., Hubble, K., Rubia, K., Schepman, K., ... & Thapar, A. (2016). Identifying mechanisms that underlie links between COMT genotype and aggression in male adolescents with ADHD. Journal of child psychology and psychiatry, 57(4), 472-480.
[36]. Castells X, Blanco-Silvente L, Cunill R. Amphetamines for attention deficit hyperactivity disorder (ADHD) in adults. Cochrane Database Syst Rev. 2018 Aug 9;8(8):CD007813.
[37]. Bostic JQ, Biederman J, Spencer TJ, Wilens TE, Prince JB, Monuteaux MC, Sienna M, Polisner DA, Hatch M. Pemoline treatment of adolescents with attention deficit hyperactivity disorder: a short-term controlled trial. J Child Adolesc Psychopharmacol. 2000 Fall;10(3):205-16
[38]. Harty, S. C., Miller, C. J., Newcorn, J. H., & Halperin, J. M. (2009). Adolescents with childhood ADHD and comorbid disruptive behavior disorders: aggression, anger, and hostility. Child psychiatry and human development, 40, 85-97.
[39]. Pliszka, S. R., Crismon, M. L., Hughes, C. W., Corners, C. K., Emslie, G. J., Jensen, P. S., ... & HYPERACTIVITY, P. O. C. A. D. (2006). The Texas Children’s Medication Algorithm Project: revision of the algorithm for pharmacotherapy of attention-deficit/hyperactivity disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 45(6), 642-657.
[40]. Blader, J. C., Schooler, N. R., Jensen, P. S., Pliszka, S. R., & Kafantaris, V. (2009). Adjunctive divalproex versus placebo for children with ADHD and aggression refractory to stimulant monotherapy. American Journal of Psychiatry, 166(12), 1392-1401.
[41]. Jensen, P. S., Hinshaw, S. P., Kraemer, H. C., Lenora, N., Newcorn, J. H., Abikoff, H. B., ... & Vitiello, B. (2001). ADHD comorbidity findings from the MTA study: comparing comorbid subgroups. Journal of the American Academy of Child & Adolescent Psychiatry, 40(2), 147-158.
[42]. Jensen, P. S., Hinshaw, S. P., Kraemer, H. C., Lenora, N., Newcorn, J. H., Abikoff, H. B., ... & Vitiello, B. (2001). ADHD comorbidity findings from the MTA study: comparing comorbid subgroups. Journal of the American Academy of Child & Adolescent Psychiatry, 40(2), 147-158.
[43]. Donovan, S. J., Stewart, J. W., Nunes, E. V., Quitkin, F. M., Parides, M., Daniel, W., ... & Klein, D. F. (2000). Divalproex treatment for youth with explosive temper and mood lability: a double-blind, placebo-controlled crossover design. American Journal of Psychiatry, 157(5), 818-820.
[44]. Saylor, K. E., & Amann, B. H. (2016). Impulsive aggression as a comorbidity of attention-deficit/hyperactivity disorder in children and adolescents. Journal of child and adolescent psychopharmacology, 26(1), 19-25.
[45]. Pappadopulos, E., Macintyre Ii, J. C., Crismon, M. L., Findling, R. L., Malone, R. P., Derivan, A., ... & Jensen, P. S. (2003). Treatment recommendations for the use of antipsychotics for aggressive youth (TRAAY). Part II. Journal of the American Academy of Child & Adolescent Psychiatry, 42(2), 145-161.