1. Introduction
1.1. Background
The novel Corona Virus Disease (COVID-19) brought almost all fields to a temporary standstill since its first outbreak in Wuhan, China, in December 2019. The rapid and fierce spread of this infectious disease to all countries made it to be declared a pandemic by the World Health Organization in the first quarter of the year 2020 [1]. In China, the prevention and control of COVID-19 is the most important component of all public health policies between 2020 and 2023. According to the official information of the National Health Commission of People’s Republic of China [2], in 2020, the National Health Commission of China issued the first plan for the prevention and control of pneumonia caused by novel coronavirus infections, to 8 January 2023, when COVID-19 was formally transferred from "Category B A" to "Category B B". This period includes but is not limited to checking the health code of anyone entering the community, cancellations of public gatherings, long-term quarantine system, and all-staff nucleic acid testing [3]. All of them highlight the "reshaping" of China's infectious disease prevention and control methods and policies due to this global public health emergency.
Along with the process of this "reshaping", there is no doubt that we need to pay attention to its impact on other infectious diseases that also threaten people's lives and property. Both sexually transmitted infectious (STIs) and acquired immune deficiency syndrome (AIDS) are major public health issues worldwide and are continuously one of the largest health burdens globally [4]. Though most STIs are not life-threatning, budgets and life-long influences affect patients’ quality of life. Although most countries showed a decrease in age-standardised rates of incidence and DALYs for STIs, the absolute incident cases and DALYs increased from 1990 to 2019 [5]. Despite two decades of well-funded and comprehensive response efforts, the Chinese Government has made great achievements in the prevention and control of AIDS [6]. It has proposed to achieve the "95-95-95 target" by 2030 in terms of the detection, treatment and success of viral suppression, HIV/AIDS still remains a major problem in China [7].
1.2. Objective
Both globally and in China, STIs and HIV/AIDS are significant public health issues that require high levels of investment over a long period, and their impact in particular situations, such as global public health emergencies, and how the government adapts to such impacts are very important concerns. After the outbreak of COVID-19 in 2020, along with the government and society putting much energy into the prevention and control of COVID-19, a considerable portion of policies and resources have also been significantly shifted towards the prevention and control of COVID-19 in such an important context [8].
2. Methodology
2.1. Regional Narration
This review focuses on the South China region, which includes the Guangxi Zhuang Autonomous Region, Guangdong Province, and Hainan Province that located in the mainland side [9], and the Hong Kong and Macao Special Administrative Region where "one country, two systems" is in practice.
2.2. Search strategy and screening
In this literature review, the official website of the Bureau for Disease Control and Prevention of China National Health Commission was used to obtain the documents related to HIV/STI prevention to clarify important time points based on the information in the article by Yan et al. [10]. At the same time, in order to provide an accurate and reliable comparative description of HIV/STI epidemiological characteristics, such as the prevalence trends, distributions, and disease burdens in southern China region before or after 2020 and related prevention and control policies in this article, literature searches are conducted from the most commonly used databases in both English (Web of Science and PubMed) and Chinese (CNKI and Wanfang Data).
2.3. In/exclusive criteria
The inclusion criteria include the description of the prevalence, trend, and triple distribution of HIV/AIDS and STIs within the region of southern China region whether it covers some key areas and high risk groups, research on prevention and control measures, policies and strategies for HIV/AIDS and STIs. The exclusion criteria screen out the literature that can not be used in this review. The articles not related to HIV/AIDS and STIs, like epidemiological studies of cancer, other chronic diseases, acute infectious diseases are not included in this review. Moreover, co-morbidities of HIV/AIDS that are not STIs, like tuberculosis, discussions specific to HIV-induced immunocompromised leading to infections with a wide range of opportunistic pathogens like Pneumocystis carinii pneumonia [11], should also be excluded. Meanwhile, the articles focus on molecular epidemiology, drug resistance, laboratory markers, genetic variation, and diagnostic studies of HIV/AIDS and its subtypes, cognitive and behavioural risk factors associated with HIV/AIDS, STIs, etc and sub-county geographies were also excluded from this review [12].
3. Result
3.1. Overview
The initial search of online databases retrieved 1837 records. There were 166 duplicate records, resulting in the remainder of 1671 records for the subsequent steps. Immediately following the exclusion by title and abstract session, a total of 1,537 papers were excluded either because they did not meet the inclusive criteria or because of the exclusive criteria. Therefore, about 134 articles entered the full-text screening step. Finally, 38 eligible records were selected for information extraction and summarized as follows: 33 of them are studies closely related to the prevalence, trend analysis, and triple distribution of HIV/STIs in the provinces and special administrative regions of Southern China before or after 2020 towards the general population and 6 key groups [13-45], and the other 5 are descriptions and summaries of prevention or control strategy to HIV/STIs in Southern China region or in China as a whole. The literature screening Flow Diagram (Figure 1) illustrates the details of the selection process.
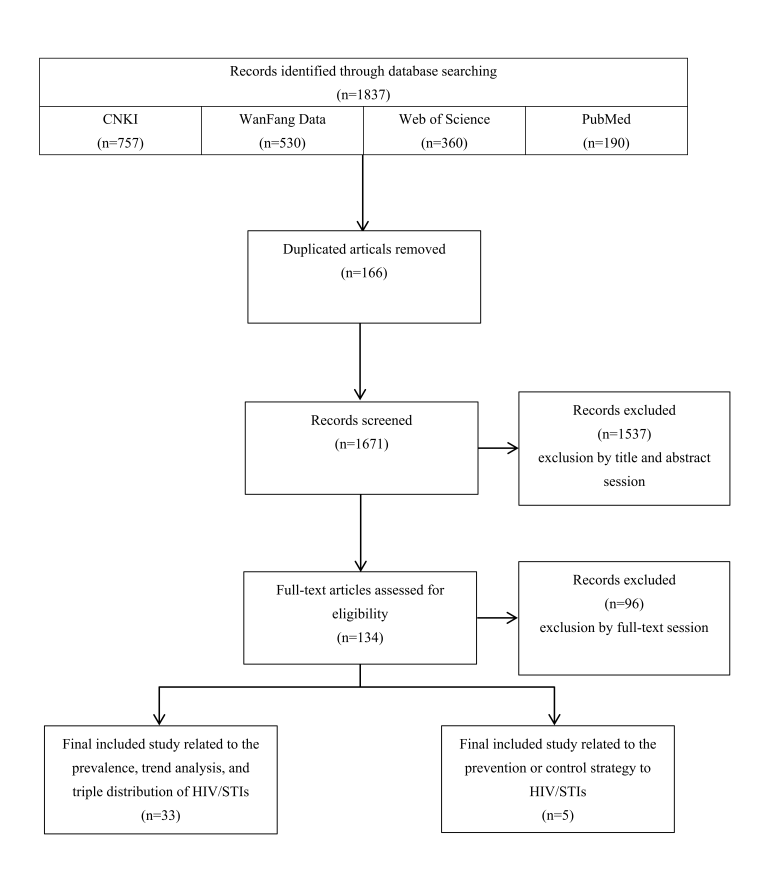
Figure 1. The flow diagram of literature screening.
3.2. General population
From a general population perspective, the epidemiological characteristics of sexually transmitted diseases and HIV/AIDS in Southern China are exhibited as follows. In Hainan Province[19], from 2009 to 2017, the annual growth rate of Chlamydia trachomatis infection in the genital tract reached 34.15%, with the incidence rate increasing from 8.04 per 100,000 in 2009 to 78.57 per 100,000 in 2017. Additionally, a study from Haikou City indicated that [16], from 2016 to 2020, the syphilis infection rate among men was 11.39%, with a significant association between HIV infection and a history of STIs (OR=6.33).
In Guangdong Province, particularly in Guangzhou City, between 2012 and 2021, there was a continuous upward trend in HIV infections in Guangzhou, reflecting a critical need for enhanced HIV control measures. An analysis of data from Panyu District in Guangzhou from 2010 to 2017 showed that the HIV infection rate had been rising annually before 2020 [18]. This trend was variably impacted during the pandemic. Particularly in the early stages of the pandemic, the reallocation of public health resources to combat COVID-19 led to restricted conventional screening and treatment services for HIV and other STIs [46].
Furthermore, the analysis from 2010 to 2017 in Panyu District revealed regional characteristics of the AIDS epidemic [18], with the incidence rate gradually increasing from a low level in 2010 to a significant peak in 2017. This rise reflects an increase in community transmission of HIV and a growing demand for screening and preventive measures. In Hong Kong, 2020, data showed that the infection rate of Chlamydia trachomatis among sexually active young women was 5.8%, 4.8% among young men, and 4.1% among sexually active women of the same age group [15]. Changes in social behaviors and adaptive prevention measures during the pandemic likely affected the reporting and management of these cases [47].
3.3. Men Who Have Sex with Men (MSM)
The first subgroup of this review target: Men who have sex with men (MSM) are a diverse group with varying sexual identities and behaviors [48, 49]. Because male-to-male intercourse is more likely to cause mucosal injury than male-to-female intercourse, and the risk factor of multipartnering is more common in the MSM community, the MSM group [50] faces unique health challenges, including higher rates of sexually transmitted infections, other mental health issues, and substance use [51]. In the United States, MSM accounts for the majority of HIV infections [52]. The criminalization of same-sex behavior and stigma against MSM compromise their human rights and contribute to the spread of HIV and other sexually transmitted infections [49]. In conclusion, the MSM population is an unavoidable target population because of its specificity and high risk worldwide. Therefore, in this review, the MSM population is the first high-risk sub-population to be focused.
Based on the analysis of the MSM population in Southern China, prior to 2020, there was a noticeable increase in the incidence of HIV and other STIs among the MSM population across different regions. In Shenzhen's Longgang district, for example, retrospective data from June 2015 to June 2018 showed HIV, TP, and herpes simplex virus type 2 (HSV-2) infection rates of 15.46%, 7.23%, and 2.12%, respectively [20].Age, marital status, education level, occupation, and income were significantly associated with these infections [20].
In Guangzhou and Haikou, the prevalence of HIV/AIDS among MSM from 2007 to 2020 integrally showed a rise. However, the growth rate of reported HIV cases among MSM showed a decline in 2019 and 2020 [21, 22], with a substantial portion of infections occurring in young adults, particularly those who are highly mobile, unmarried, and from the Han ethnicity. This trend suggested the shift and disruption in health service delivery during a pandemic and an upgrade need for targeted public health strategies.
In Guilin City, despite a high rate of HIV knowledge among MSM (90.9%), the actual practice of safe behaviors lagged, with consistent condom use not aligning with the level of awareness [23]. This disconnection highlights the impact of the pandemic on educational and intervention strategies, which could not be as effective due to social distancing and other COVID-related restrictions.
3.4. Heterosexual contact/sex workers
Before the onset of the COVID-19 pandemic, the surveillance data from 2015 to 2019 in Guangxi specifically focusing on the clientele of sex workers (patrons) indicated significant levels of HIV and STI transmissions [27], highlighting the critical role this group plays in the broader epidemiological landscape of STIs. In Guangdong, a study between 2016 and 2018 highlighted a substantial number of HIV/AIDS cases attributed to heterosexual transmission (2,935 cases) [26], with a considerable prevalence in unmarried individuals and migrants, reflecting the mobility and sexual behaviors of this group. Non-commercial, non-marital sexual transmission was predominant, accounting for 61.8% of transmissions, highlighting the importance of targeted educational and intervention measures for these populations.
The COVID-19 pandemic brought substantial disruptions that likely impacted the trends observed in the previous years. For female sex workers in Southern China, the analysis from 2019 to 2022 indicates the impact of the pandemic on the prevalence of Chlamydia and gonorrhea [25]. Particularly along the Sino-Vietnam border, female sex workers (FSWs), both local and cross-border migrants, presented a higher risk group, with variable HIV, syphilis infection rates over the years. Cross-sectional surveys from 2016 to 2021 reported a general decline in STIs among these groups [24], with notable variations between local and migrant workers, which shows a complex picture with a slight decrease in HIV prevalence among local FSWs but a fluctuating pattern for cross-border FSWs, reflecting the unique challenges faced by these groups due to their mobility and the varying degrees of access to health services.
3.5. Youth and Students with HIV
This section targets the “youth and students” age group between 15 and 24 years old. In Guangxi, Yulin, from 2011 to 2020, a total of 395 male cases aged 15-24 were reported, with significant transmission attributed to both heterosexual (53.7%) and homosexual (44.1%) contacts [31]. Moreover, Huizhou (Guangdong) 's study from 2010 to 2018 reflected similar patterns among young students, predominantly involving unmarried male university students engaging in homosexual behaviors as the primary transmission route [33]. This highlights the crucial role of sexual behavior in the spread of HIV within this demographic.
Nevertheless, studies like those from Beihai, Guangxi (2007-2018) [34] and Hainan (2011-2019) [32] indicate that the number of HIV/AIDS cases among groups of young people aged 15-24 years who report their occupation as students in the Integrated AIDS Control Information System (IACIS) was already significant, with an apparent prevalence of male homosexual transmission, underscoring the continuing trend of higher educational level among those affected. In Hainan, the proportion of young students engaging in sexual activities remains considerable, with low condom usage rates indicating persistent risky behaviors despite awareness campaigns. The data from 2011 to 2019 show that while homosexual transmission remains predominant, heterosexual transmission has seen a decrease [32].
3.6. Drug users
HIV, HCV, and syphilis infections among drug users were significant concerns. For instance, data from Nanning between 2019 and 2021 showed a male-dominated, predominantly low-educated drug-using population, with a substantial portion engaging in injection drug use, which was significantly linked to HIV transmission [28]. Similarly, in Qinzhou, a significant rate of injection drug use and needle sharing was noted, with a high prevalence of HCV and syphilis among these populations [29], highlighting ongoing risky behaviors that facilitate the spread of these infections.
Despite high levels of awareness about HIV/AIDS among drug users, actual practices such as needle sharing and unprotected sexual activities continued to pose significant risks. In Yangjiang, for instance, the HIV prevalence among drug users was noted to be 8.4% during 2017-2018, with high-risk behaviors like needle sharing increasing the risk of HIV infection substantially [30]. Amid and following the pandemic's peak, there was a notable continuation of high-risk behaviors among drug users. Studies like those in Nanning highlighted an increase in the use of traditional drugs over newer synthetic drugs among the population despite ongoing interventions [28]. The continued high rates of needle sharing and unprotected sex after drug use were particularly concerning, given their direct correlation with higher HIV transmission rates.
3.7. Older adults, pregnant women and infants
Older adults showed a notable incidence of HIV/AIDS, with a higher prevalence among men and those aged between 50 and 69 years, particularly in Yangjiang (Guangdong) [40] and Wuzhou (Guangxi) [41]. For pregnant women in Guangzhou, there was a consistently low prevalence of HIV (0.01%) from 2017 to 2021 [39]. Syphilis and hepatitis B were more prevalent, with hepatitis B showing a declining trend in positivity over the years, suggesting effective screening and vaccination programs. The low rate of HIV and syphilis transmission from mother to child indicates successful intervention strategies during prenatal care. In infants, mother-to-child transmission (MTCT) of HIV in Guangxi showed a low transmission rate (2.1%), with high ART uptake among mothers suggesting effective perinatal intervention strategies [37]. However, certain regions still exhibited slightly higher rates, indicating the need for enhanced focus on universal ART coverage and monitoring to eliminate MTCT goals [37].
3.8. Foreigners, foreign labours and the population associated with border areas
The HIV prevalence among the entry-exit population at Guangzhou port was relatively high, with a detection rate of 7.4 per 10,000 from 2010 to 2020 [45]. Among these, a significant number were Africans and Asians, with male travelers showing a higher prevalence than females. The prevalence was notably high among the 31-40 age group, emphasizing the need for focused surveillance and prevention measures. For outbound travelers at Guangzhou port from 2016 to 2019 [54], the syphilis infection rate varied, with the highest rate recorded in 2016 (4.74 per 1,000) and a decline by 2019 (2.55 per 1,000). Older age groups showed higher infection rates, highlighting the importance of targeted health education and monitoring programs to control cross-border spread. Meanwhile, among Filipino migrants in China, particularly domestic workers in Macao, barriers to HIV/syphilis testing included low perceived need and lack of time, despite the high risk negatively influencing their migration status and social conditions [43].
4. Discussion
4.1. The HIV/STIs prevention and control strategies
The COVID-19 pandemic significantly impacted the global health systems, creating unique challenges for the prevention and control of HIV/STIs. In Southern China, as reflected in various studies and guidelines [7, 53-56], strategic adaptations were necessary to mitigate these challenges, ensuring the continuity and effectiveness of HIV/STI prevention measures during and after the pandemic.
4.1.1. Impact of COVID-19 on HIV/STI Prevention and Control
The pandemic of COVID-19 had a significant impact on HIV/STI prevention and control both worldwide and in China, particularly among key populations. In India, clinic-based data showed a decrease in HIV-related service utilization among MSM and drug users[57]. In China, disruptions due to COVID-19 were estimated to increase HIV transmission and mortality among MSM [57]. The pandemic has also affected STI/HIV control programs, with altered health-seeking behavior and reduced clinic capacity [59]. The pandemic caused a shift in healthcare priorities, with significant resources diverted to combat COVID-19. This shift led to disruptions in routine HIV/STI services, including screening, diagnosis, and treatment, As the studies suggest that Guangxi Province responded by integrating HIV/STI services with COVID-19 health interventions [53].
4.1.2. Adaptation of Guidelines and Strategies
The updated Chinese guidelines for HIV/AIDS treatment in 2021 [7] emphasized the importance of maintaining ART therapy continuity and integrating telemedicine services to provide care while minimizing COVID-19 exposure risk. These guidelines also highlighted the importance of addressing social determinants of health, such as stigma and discrimination, which were exacerbated during the pandemic due to heightened vulnerabilities among marginalized groups.
4.1.3. Technological Innovations and Policy Adjustments
The research by Brohi summarized the role of technologies such as AI, big data analysis, high-performance computing, telecommunication and many other digital health technologies in fighting against COVID-19 [60] . In response to the pandemic, health services adopted these technologies to facilitate remote consultations, prescription refills, and follow-up visits [61, 62], ensuring that people living with COVID-19 and other infectious diseases could have continuation of care and increased access to their treatment without interruption [63]. For instance, Guangdong Province utilized online platforms to provide education and counseling services, which proved essential during lockdowns and travel restrictions [54].
4.1.4. Preventive Measures and Screening
By comparing the Chinese guidelines for the diagnosis and treatment of HIV/AIDS published by the Chinese Medical Association in 2018 and 2021 [7,56], respectively, it is clear that after 2020, the new version of the guidelines appears for the first time to guide postexposure prophylaxis (PEP) for the first time in the new post-2020 guidelines. PrEP and PEP both adapted during the pandemic are critical components of the HIV prevention toolkit. These measures were particularly emphasized in regions with high rates of HIV among key populations, such as MSM and sex workers [64-66]. The integration of routine syphilis screening for pregnant women and rapid syphilis and HIV testing for high-risk groups ensured early detection and treatment, thereby reducing the transmission rates, particularly mother-to-child transmission, which continued to decline [64-66].
4.2. Future prospects
During the initial outbreak of COVID-19, public health resources were predominantly redirected towards fighting against the spread of SARS-COV-2, which affected the regular screening, prevention, and treatment services for HIV and STIs [67]. For instance, restrictions and the re-allocation of healthcare resources led to reduced accessibility to routine healthcare services, including those for HIV and STIs. In the general population of Guangzhou city, this disruption contributed to a temporary decline in new diagnoses, not necessarily due to a reduction in incidence but rather a decrease in detection and reporting [54]. At the same time, HIV and syphilis rates fluctuate among heterosexuals and sex workers in the Sino-Vietnamese border region [24], and access to health services for this population has been significantly impacted by the impact on mobility in the context of border closures. Moreover, HIV transmission and mortality rates are increasing in the context of resource displacement due to decreased utilization of services related to HIV/STIs during the pandemic, particularly among MSM and drug users.
However, the pandemic also prompted public health authorities to innovate and adapt. Telehealth services saw a significant expansion, although initially a response to COVID-19, provided a benefit for managing other health conditions [68]. Services such as virtual consultations and at-home testing kits for HIV and STIs became more commonplace, helping to maintain some continuity of care even when traditional in-person services were disrupted [68]. Moreover, the emphasis on hygiene practices and public health awareness during the pandemic could have indirectly influenced the behaviors related to the transmission of sexually transmitted infections [70]. For example, in Guangdong Province [53], the use of online platforms to provide education and counselling services, especially during the lockdown and travel restrictions, the increased awareness and practices such as reduced casual sexual encounters created by the innovation of online platforms during lockdowns might have contributed to temporary reductions in STI rates.
In addition to technological innovations, HIV/STIs post-exposure prophylaxis became more widely available with the launch of the new guideline in 2021 [7], it's also important to consider the long-term implications of these changes. The integration of HIV and STI services with COVID-19 response mechanisms—like using HIV testing labs to also process COVID-19 tests—demonstrates a model of integrated disease surveillance that could strengthen overall public health responsiveness. For example, the AIDS Conquest Project in Guangxi ensured that HIV testing and treatment were not overlooked by increasing community-based interventions and integrating HIV services with COVID-19 response teams [53]. However, this integration must be managed carefully to avoid undermining the services for either group of diseases.
As public health strategies evolve in the post-pandemic period, assessing which new or adapted practices should be continued or expanded will be crucial. For example, telehealth has shown potential not only for routine care but also for reaching special populations like students, drug users, elderly and infants who may face barriers to accessing traditional health services. The lessons learned from the pandemic response could thus inform more resilient and flexible public health strategies that better integrate the management model of various infectious diseases, including COVID-19, HIV and STIs.
5. Conclusion
The COVID-19 pandemic, emerging as a global health emergency in 2020, substantially impacted the prevention and control of HIV and STIs in Southern China. This literature review summarized epidemiological characters and policy adaptations before and after the pandemic, highlighting significant disruptions and innovations. In regions of Southern China, the pandemic-induced reallocation of health resources led to reduced accessibility to routine HIV/STI services, impacting detection and treatment rates. The key populations affected by HIV/STIs during the normal time including MSM, drug users, sex workers, teenagers, Older adults, pregnant women, infants and foreigners experienced heightened vulnerabilities due to social distancing and mobility restrictions. However, the pandemic also spurred significant innovations, such as telehealth services, which provided virtual consultations and at-home testing kits, ensuring continuity of care. Additionally, public health measures like community-based interventions and the integration of HIV/STI services with COVID-19 response mechanisms demonstrated resilience and adaptability. Consider the limitation, as HIV and STIs are still a broad taboo topics in China, both in private and academic situations, under the influence of China's general environment and traditional thought [71]. Therefore, in the process of doing this literature review, even in Southern China which is a relatively economically developed region, there still exists a great imbalance in the geographical research data on HIV/STIs. There is no way to establish a more intuitive and one-to-one correlation between HIV/STIs before and after 2020, and this review can only make a rough judgement of the impact of COVID-19 on the prevention and control strategies of HIV/STIs in South China by using different diseases and different indicators, and provide further conclusions. Future strategies should consider the origin of the shortcomings this literature review, has and prepare for future similar situations by building on the innovations, ensuring robust, flexible public health systems capable of managing multiple health crises effectively.
References
[1]. Vishnu, K. N., Kumar Uppala, P., Vangoori, Y., & Rao Gudhanti, S. N. (2021). A review on Covid 19 pandemic and its global effects. Asian Journal of Pharmaceutical Research, 242–246. https://doi.org/10.52711/2231-5691.2021.00042
[2]. National Health Commission of People’s Republic of China. (2023). http://www.nhc.gov.cn/xcs/zhengcwj/202301/bdc1ff75feb94934ae1dade176d30936.shtml?R0NMKk6uozOC=1673325152096
[3]. Wu, Y., Zhang, Q., Li, L., Li, M., & Zuo, Y. (2021). Control and Prevention of the COVID-19 epidemic in China: A Qualitative community case study. Risk Management and Healthcare Policy, Volume 14, 4907–4922. https://doi.org/10.2147/rmhp.s336039
[4]. Liu, X., McGoogan, J. M., & Wu, Z. (2021). Human immunodeficiency virus/acquired immunodeficiency syndrome prevalence, incidence, and mortality in China, 1990 to 2017: a secondary analysis of the Global Burden of Disease Study 2017 data. Chinese Medical Journal/Chinese Medical Journal, 134(10), 1175–1180. https://doi.org/10.1097/cm9.0000000000001447
[5]. Zheng, Y., Yu, Q., Lin, Y., Zhou, Y., Lan, L., Yang, S., & Wu, J. (2022). Global burden and trends of sexually transmitted infections from 1990 to 2019: an observational trend study. Lancet. Infectious Diseases/the Lancet. Infectious Diseases, 22(4), 541–551. https://doi.org/10.1016/s1473-3099(21)00448-5
[6]. He, N. (2021). Research progress in the epidemiology of HIV/AIDS in China. China CDC Weekly, 3(48), 1022–1030. https://doi.org/10.46234/ccdcw2021.249
[7]. Li, T. (2022). Chinese guidelines for the diagnosis and treatment of hiv/aids (2021 edition). Infectious Diseases & Immunity.
[8]. Güner, R., Hasanoğlu, I., & Aktaş, F. (2020). COVID-19: Prevention and control measures in community. Turkish Journal of Medical Sciences, 50(SI-1), 571–577. https://doi.org/10.3906/sag-2004-146
[9]. Zhao, H. (1988). The People’s Republic of China--South. In The Geojournal library (pp.355 – 368). https://doi.org/10.1007/978-94-009-2999-9_40
[10]. Yan, J., Li, Y., & Zhou, P. (2022). Impact of covid-19 pandemic on the epidemiology of stds in China: Based on the GM (1,1) model. BMC Infectious Diseases. https://doi.org/10.21203/rs.3.rs-994599/v1
[11]. Ernst, P., Chen, M. F., Wang, N. S., & Cosio, M. (1983). Symbiosis of Pneumocystis carinii and cytomegalovirus in a case of fatal pneumonia. PubMed, 128(9), 1089–1092. https://pubmed.ncbi.nlm.nih.gov/6301670
[12]. Starace, F., Bartoli, L., Aloisi, M. S., Antinori, A., Narciso, P., Ippolito, G., Ravasio, L., Moioli, M. C., Vangi, D., Gennero, L., Coronado, O. V., Giacometti, A., Nappa, S., Perulli, M. L., Montesarchio, V., La Gala, A., Ricci, F., Cristiano, L., De Marco, M., . . . Monforte, A. D. (2002). Cognitive and affective disorders associated to HIV infection in the HAART era: findings from the NeuroICONA study. Acta Psychiatrica Scandinavica, 106(1), 20–26. https://doi.org/10.1034/j.1600-0447.2002.02289.x
[13]. Chen, H., Luo, L., Pan, S. W., Lan, G., Zhu, Q., Li, J., Zhu, J., Chen, Y., Shen, Z., Ge, X., Tang, Z., Xing, H., Shao, Y., Ruan, Y., & Yang, W. (2019). HIV Epidemiology and Prevention in Southwestern China: Trends from 1996-2017. Current HIV Research, 17(2), 85–93. https://doi.org/10.2174/1570162x17666190703163838
[14]. Lin, Q., Deng, B., Rui, J., Guo, S. B., Hu, Q. Q., Chen, Q. P., Tang, C., Zhou, L. A., Zhao, Z. Y., Lin, S. N., Zhu, Y. Z., Yang, M., Wang, Y., Xu, J. W., Liu, X. C., Yang, T. L., Li, P. H., Li, Z. Y., Luo, L., . . . Chen, T. M. (2021). Epidemiological Characteristics and Transmissibility of Human Immunodeficiency Virus in Nanning City, China, 2001-2020. Frontiers in Public Health, 9, Article 689575. https://doi.org/10.3389/fpubh.2021.689575
[15]. Wong, W. C. W., Tucker, J. D., Man, H. K., Emch, M., Yang, L. G., & Zhao, Y. (2021). Prevalence and contextual risk factors of sexually transmitted infections in Hong Kong: abridged secondary publication. Hong Kong Med J, 3, 40–43. https://europepmc.org/article/MED/34075891
[16]. Feng, Y., Xu, Y., Zhu, K., Chen, H., & Chen, S. (2023). Analysis on prevalence and influence factors of syphilis in male patients attending STD clinic in Haikou. Zhongguo Xingkexue, 32(01), 144-147. https://kns.cnki.net/kcms2/article/abstract?v=yqeyU9EK6jRIpmsnWOOwvKITVJ1d-hfS_ad_vpW3CDHlzRYl7jpyLhIt5ZgK11AmknKz6gjCi_cHHgU-DalBUbhsWktUNtduZIeeNKoz6gYHWaNKFixuPdL-ydvO6E_kzhWpvolMTPELO6i0VJ8McQ==&uniplatform=NZKPT&language=CHS
[17]. Zeng, X., Fu, P., Wang, Z., Zhang, F., Zheng, Y., & Qin, L., (2020). Analysis on the characteristics and transmission routes of AIDS epidemic in Hainan. China Tropical Medicine, 20(8), 735-738. https://doi.org/10.13604/j.cnki.46-1064/r.2020.08.09
[18]. Luo, J., Yang, Y., Liang, S., Xiong, T., Meng, W., & He, Q. (2019). Analysis on HIV/AIDS epidemic situation in Panyu district, Guangzhou, from 2010 to 2017. Journal of Tropical Medicine, 19(07), 907-909. https://kns.cnki.net/kcms2/article/abstract?v=yqeyU9EK6jQRDQ54l_G9OiTUW1Sv6723IjczZ110-MM19q0Ocs_MKzWAMKIsgrGr4evyuPzXXfWNgOcWvweqdsqGX0CDMMPxGEZsthgjfundcX91QWAGfJYWMQeLaPx7-A1_XhPmnh6nhwgdAEWN0Q==&uniplatform=NZKPT&language=CHS
[19]. Lu, J., Xu, Y., Zhu, K., & Feng, Z. (2020). Current status and countermeasures for Chlamydia trachomatis infection in the reproductive tract in Hainan Province, 2009-2017. Chinese Journal of AIDS & STD, 26(02), 209-211. https://doi.org/10.13419/j.cnki.aids.2020.02.28
[20]. Chunru, L. U. (2019). Analysis on hiv,tp and hsv-2 virus infection status and influencing factors in msm population in longgang district of shenzhen. China Medicine and Pharmacy.
[21]. Zhu, C., Yang, Y., Wu, S., Liang, S., Xiong, T., & Meng, W. (2021). AIDS epidemic characteristics in men who have sex with men at Panyu District, Guangzhou from 2007 to 2020. International Medicine and Health Guidance News, 27(13), 1899-1903. https://doi.org/10.3760/cma.j.issn.1007-1245.2021.13.001
[22]. Wang, Z., Zheng, Y., Zhao, D., Qin, L., Yan, C., & Lu, Q. (2022). Trends and Causes Analysis of HIV Infection Rate Among Cross-Sectional Surveys of Men Who Had Sex with Men in Haikou Prefecture 2008-2017. the Chinese Journal of Dermatovenereology, 36(6), 683-689. https://doi.org/10.13735/j.cjdv.1001-7089.202111042
[23]. Yang, D., Jiang, F., Liu, Y., & Fu, X. (2021). HIV infection status of men who have sex with men and its influencing factors in Guilin, 2017-2020. South China Journal of Preventive Medicine, 47(10), 1315-1318. https://doi.org/10.12183/j.scjpm.2021.1315
[24]. Liang, B., Zhang, F., Ou, Y., Zhang, P., Bao, L., Mo, S., Nong, A., Wei, D., Wu, Z., Xie, H., Yang, Y., Liu, D., Liang, H., & Ye, L. (2023). Prevalence, trends and correlates of HIV, syphilis and HCV infection among Chinese local and cross-border migrant female sex workers in the Sino-Vietnam border area of Guangxi, 2016–2021. AIDS and Behavior, 28(4), 1257–1269. https://doi.org/10.1007/s10461-023-04153-6
[25]. Wang, J., Zhao, P., Xu, W., & Wang, C. (2023). Changing trends in Chlamydia and gonorrhea infections among female sex workers in Southern China: a surveillance data analysis spanning 2019 to 2022. Journal of Public Health. https://doi.org/10.1093/pubmed/fdad222
[26]. Wei, T., Shao-Chu, L. , & Jin, Z. . (2019). Modes of hiv transmission through heterosexual contact among hiv/aids cases in shenzhen city. Practical Preventive Medicine.
[27]. Yang, D., Jiang, F., Xu, F., Fu, X., & Liu, Y. (2022). Analysis of the results of HIV STD surveillance in the client population in Guilin, 2015-2019. South China Journal of Preventive Medicine, 48(01), 74-76, 80. https://kns.cnki.net/kcms2/article/abstract?v=yqeyU9EK6jTE8RqOL4UV0EsKhHNaoyFyRPrtUkijkWmZNx-PfkGB_HGPzLfbOr8LqeaSt6j-oAnrW4KHtlYn6t5eyecwh3KbvnDY81l8HblP92ONYF_raLoYHbljxeMt6wUp_cZV80dx7h4bVR2PZw==&uniplatform=NZKPT&language=CHS
[28]. Zhan, J., Mo, J., Xu, X., Liu, J., & Qin, W. (2023). Analysis of sentinel surveillance on AIDS among drug users in Nanning from 2019 to 2021. Prasitoses and infectious Diseases, 21(4), 187-191,197. https://d.wanfangdata.com.cn/periodical/ChlQZXJpb2RpY2FsQ0hJTmV3UzIwMjMxMjI2EhFzeWpzY2J6ejIwMjMwNDAwMhoIMXg2MnU4bzQ%3D
[29]. Lin, Z., Zhi, J., Chen, H., Jiang, J., Chen, Y., & Liang, B. (2019). Analysis on infection status of sexually transmitted diseases and influencing factors of HIV infection among drug users in Qinzhou. Henan Journal of preventive Medicine, 30(06), 401-404, 417. https://doi.org/10.13515/j.cnki.hnjpm.1006-8414.2019.06.001
[30]. Mai, J., Zeng, G., & Tan, X. (2019). Study on HIV Infection Status and Risk Factors of Drug Abusing Population in Yangjiang City. Strait Journal of Preventive Medicine, 25(03), 37-39. https://kns.cnki.net/kcms2/article/abstract?v=yqeyU9EK6jTbGiuAx_1QpNJm86oufMQdGqRgPYlbM-zuSGRxEf1vOw04z7rOCL6jGQXZA37nE0ZUJADpCrJrIDaF3RRoY4wBqOsTH2gQZx9DfU3mQ6suUsu64JR79jg2JSKv3BMiNzA85egMuB1d9A==&uniplatform=NZKPT&language=CHS
[31]. Zhang, D., Qin, X., Ye, R., Qin, X., Jiang, N., & Li, J. (2021) Epidemiological characterisation of HIV/AIDS cases among adolescent males aged 15-24 years in Yulin City, 2011-2020. Applied Preventive Medicine, 27(6), 547-549. https://doi.org/10.3969/j.issn.1673-758X.2021.06.020
[32]. Zeng, X., Wang, Z., Zhang, F., Zheng, Y., & Fu, P. (2021) The epidemic characteristics and risk factors of AIDS among students in Hainan Province. Zhongguo Jiankang Jiaoyu, 37(06), 492-495. https://doi.org/10.16168/j.cnki.issn.1002-9982.2021.06.003
[33]. Li, X., & Wang, C. (2019). Epidemiological characterisation of AIDS-related characteristics among young students in Huizhou City (2010-2018). Journal of Dermatology and Venereology, 41(3), 342-343. https://doi.org/10.3969/j.issn.1002-1310.2019.03.012
[34]. Nailing, M. , Weigui, G. , Xianrui, W. , Juxian, P. , & Jiannan, L. . (2019). Hiv/aids epidemic status among students in beihai, guangxi, 2007-2018. China Tropical Medicine.
[35]. Lu, Z., Zhao, P. Z., Lu, H. J., & Xiao, M. F. (2023). Analyses of human papillomavirus, Chlamydia trachomatis, Ureaplasma urealyticum, Neisseria gonorrhoeae, and co-infections in a gynecology outpatient clinic in Haikou area, China. Bmc Womens Health, 23(1), Article 117. https://doi.org/10.1186/s12905-023-02259-6
[36]. Wang, C., Zhao, P. Z., Xiong, M. Z., Tucker, J. D., Ong, J. J., Hall, B. J., Sami, M., Zheng, H. P., & Yang, B. (2021). New Syphilis Cases in Older Adults, 2004-2019: An Analysis of Surveillance Data From South China. Frontiers in Medicine, 8, Article 781759. https://doi.org/10.3389/fmed.2021.781759
[37]. Zhao, J. Y., Chen, Q. P., Fu, C. Y., Qin, Q. H., Huang, H. F., Feng, Y. Y., Wei, Y. C., Li, Y., Huang, A. D., Xu, Q. Q., & She, S. Y. (2020). Rate of the HIV Transmission and Associated Factors Among HIV-Exposed Infants in Guangxi, China: 2014-2019. Aids Research and Human Retroviruses, 36(8), 647-655. https://doi.org/10.1089/aid.2020.0073
[38]. Zhong, S., Ou, Y., Zhang, F., Lin, Z., Huang, R., Nong, A., Wu, Z., Liang, H., Qin, C., Wei, Q., Yang, Y., Yu, D., Tang, X., Ye, L., Liu, D., Liang, H., & Liang, B. (2022). Prevalence trends and risk factors associated with HIV, syphilis, and hepatitis C virus among pregnant women in Southwest China, 2009-2018. AIDS Res Ther, 19(1), 31. https://doi.org/10.1186/s12981-022-00450-7
[39]. Yan, Y., Ai, X., Gao, H., Yang, C., & Liu, Y. (2023) Analysis on epidemiology of hepatitis B, syphilis and AIDS among pregnant women in Guangzhou from 2017 to 2021. Journal of Tropical Medicine, 23(07), 1034-1038. https://kns.cnki.net/kcms2/article/abstract?v=yqeyU9EK6jSlLguHC0n8-MKe263v613Yz073xakeaOZqOL2hZTpQoFNPROkBS-7XPdkzdIiKvs0O31P1UMxaoPDU-EzQHuruHxPRA8VZyCLSI9CRdCbq8m8PscpQ1hmbTHkIRLG-wijcgwap08UP2g==&uniplatform=NZKPT&language=CHS
[40]. Zeng, G., Ye, C., Liu, C., Liang, S., & Yang, G. (2022). Epidemiological characteristics of newly reported HIV/AIDS cases aged ≥50 years in Yangjiang City, 2017-2021. Jiangsu Journal of Preventive Medicine, 33(6), 699-701. https://doi.org/10.13668/j.issn.1006-9070.2022.06.022
[41]. Tan, L., Chen, Y., Li, J., & Huang, S. (2020). Analysis of the elderly HIV/AIDS cases in Wuzhou, Guangxi, 2014-2018. China Tropical Medicine, 20(1), 49-52. https://doi.org/10.13604/j.cnki.46-1064/r.2020.01.11
[42]. Chimungu, B., Fu, M. Q., Wu, J., Wu, J. L., Huang, L. P., Dai, Y. C., Tang, S. X., Zhang, J. M., & Wan, C. S. (2020). Prevalence of sexually transmitted infections among foreigners living in Guangzhou, China: a cross-sectional study (2010-2017). Bmc Infectious Diseases, 20(1), Article 345. https://doi.org/10.1186/s12879-020-04995-8
[43]. Hall, B. J., Yang, X. Y., Huang, L., Yi, G. C., Chan, E. W. W., Tucker, J. D., & Latkin, C. A. (2020). Barriers and Facilitators of Rapid HIV and Syphilis Testing Uptake Among Filipino Transnational Migrants in China. Aids and Behavior, 24(2), 418-427. https://doi.org/10.1007/s10461-019-02449-0
[44]. Li, Z., Sun, K., Zhu, Y., Qi, P., Ming, H., & Chen, C. (2023). Survey on syphilis among exit travelers at Guangzhou port from 2016 to 2019. Chinese Journal of Frontier Health and Quarantine, 46(06), 575-577. https://doi.org/10.16408/j.1004-9770.2023.06.017
[45]. Huang, N., Li, X., Liang, R., Chen, J., Qi, P., & Wen, Y. (2022). Analysis of HIV infection status of entry-exit population at Guangzhou port from 2010 to 2020. Chinese Journal of Frontier Health and Quarantine, 45(02), 163-166. https://doi.org/10.16408/j.1004-9770.2022.02.020
[46]. Thu, H. N., Quynh, A. N., Hai, O. K., Thanh, H. L. T., & Thanh, H. N. (2022). Impact of the COVID‐19 pandemic on provision of HIV/AIDS services for key populations. the International Journal of Health Planning and Management, 37(5), 2852–2868. https://doi.org/10.1002/hpm.3508
[47]. Liu, J., Kamarudin, K. M., Liu, Y., Zou, J., & Zhang, J. (2022). Developing a behavior change framework for pandemic prevention and control in public spaces in China. Sustainability, 14(4), 2452. https://doi.org/10.3390/su14042452
[48]. Pachauri, S., Pachauri, A., & Mittal, K. (2021). Men Who Have Sex with Men. In SpringerBriefs in public health (pp. 9–25). https://doi.org/10.1007/978-981-16-4578-5_2
[49]. Ross, M. W. (1992). Men who have sex with men. AIDS Care, 4(4), 457 – 459. https://doi.org/10.1080/09540129208253122
[50]. Koblin, B. A., Husnik, M. J., Colfax, G., Huang, Y., Madison, M., Mayer, K., Barresi, P. J., Coates, T. J., Chesney, M. A., & Buchbinder, S. (2006). Risk factors for HIV infection among men who have sex with men. AIDS, 20(5), 731–739. https://doi.org/10.1097/01.aids.0000216374.61442.55
[51]. Baber, J., & Dayan, L. (2006). Men who have sex with men--a management approach for GPS. Aust Fam Physician, 35(10), 797–800. https://www.ncbi.nlm.nih.gov/pubmed/17019455
[52]. Men Who Have Sex with Men. (2005). [Dataset]. In PsycEXTRA Dataset. https://doi.org/10.1037/e663272007-001
[53]. Ma, S., Chen, Y., Lai, X., Lan, G., Ruan, Y., Shen, Z., Zhu, Q., & Tang, S. (2022). Predicting the HIV/AIDS epidemic and measuring the effect of AIDS Conquering Project in Guangxi Zhuang Autonomous Region. PloS One, 17(7), e0270525. https://doi.org/10.1371/journal.pone.0270525
[54]. Tang, X. J., Chen, W., Tang, S. Q., Zhao, P. Z., Ling, L., & Wang, C. (2022). The evaluation of preventive and control measures on congenital syphilis in Guangdong Province, China: a time series modeling study. Infection, 50(5), 1179-1190. https://doi.org/10.1007/s15010-022-01791-1
[55]. Wu, R., Tan, T., & Gao, H. (2022). A review of HIV epidemic trend analysis and prevention strategies. Chinese Practical Journal of Rural Doctor, 29(08), 28-31. https://kns.cnki.net/kcms2/article/abstract?v=yqeyU9EK6jTIhmZaWrvpIJYYGJJsCyWSloFP2JR4tkVH6KwU1je6u9u9c2DMj5adW5ATPBTEZ28y5uYhYP-2gNTIIki9laiSZBmM81Q1uZwEot_fJrWrE5uk6XwKzX5l3feWLG29gJkq1DNM_ovvcg==&uniplatform=NZKPT&language=CHS
[56]. AIDS, Hepatitis, C, Professional, Group, & Society, et al. (2018). chinese guidelines for diagnosis and treatment of hiv/aids (2018). Zhonghua Nei Ke Za Zhi.
[57]. McFall, A. M., Menezes, N. P., Srikrishnan, A. K., Solomon, S. S., Anand, S., Baishya, J. J., Lucas, G. M., Celentano, D. D., & Mehta, S. H. (2022). Impact of the COVID‐19 pandemic on HIV prevention and care services among key populations across 15 cities in India: A longitudinal assessment of clinic‐based data. Journal of the International AIDS Society, 25(7). https://doi.org/10.1002/jia2.25960
[58]. Booton, R. D., Fu, G., MacGregor, L., Li, J., Ong, J. J., Tucker, J. D., Turner, K. M., Tang, W., Vickerman, P., & Mitchell, K. M. (2021). The impact of disruptions due to COVID‐19 on HIV transmission and control among men who have sex with men in China. Journal of the International AIDS Society, 24(4). https://doi.org/10.1002/jia2.25697
[59]. Ogunbodede, O. T., Zablotska-Manos, I., & Lewis, D. A. (2021). Potential and demonstrated impacts of the COVID-19 pandemic on sexually transmissible infections: Republication. Current Opinion in HIV and AIDS, 16(2), 115–120. https://doi.org/10.1097/coh.0000000000000672
[60]. Brohi, S. N., Jhanjhi, N., Brohi, N. N., & Brohi, M. N. (2020). Key Applications of State-of-the-Art Technologies to Mitigate and Eliminate COVID-19. https://doi.org/10.36227/techrxiv.12115596
[61]. Jnr, N. B. A. (2020). Use of telemedicine and virtual care for remote treatment in response to COVID-19 pandemic. Journal of Medical Systems, 44(7). https://doi.org/10.1007/s10916-020-01596-5
[62]. Mehraeen, E., Mehrtak, M., SeyedAlinaghi, S., Nazeri, Z., Afsahi, A. M., Behnezhad, F., Vahedi, F., Barzegary, A., Karimi, A., Mehrabi, N., Dadras, O., & Jahanfar, S. (2022). Technology in the Era of COVID-19: A Systematic Review of Current evidence. Infectious Disorders. Drug Targets, 22(4). https://doi.org/10.2174/1871526522666220324090245
[63]. Appleton, R., Williams, J., Juan, N. V. S., Needle, J. J., Schlief, M., Jordan, H., Rains, L. S., Goulding, L., Badhan, M., Roxburgh, E., Barnett, P., Spyridonidis, S., Tomaskova, M., Mo, J., Harju-Seppänen, J., Haime, Z., Casetta, C., Papamichail, A., Lloyd-Evans, B., . . . Johnson, S. (2021). Implementation, adoption, and Perceptions of Telemental Health during the COVID-19 Pandemic: Systematic review. JMIR. Journal of Medical Internet Research/Journal of Medical Internet Research, 23(12), e31746. https://doi.org/10.2196/31746
[64]. Portman, M. (2018). HIV prevention strategies. Medicine, 46(5), 293– 299. https://doi.org/10.1016/j.mpmed.2018.02.009
[65]. Jones, A., Cremin, I., Abdullah, F., Idoko, J., Cherutich, P., Kilonzo, N., Rees, H., Hallett, T., O’Reilly, K., Koechlin, F., Schwartlander, B., De Zalduondo, B., Kim, S., Jay, J., Huh, J., Piot, P., & Dybul, M. (2014). Transformation of HIV from pandemic to low-endemic levels: a public health approach to combination prevention. Lancet, 384(9939), 272–279. https://doi.org/10.1016/s0140-6736(13)62230-8
[66]. Vermund, S. H. (2014). Global HIV Epidemiology: A guide for strategies in prevention and care. Current HIV/AIDS Reports, 11(2), 93–98. https://doi.org/10.1007/s11904-014-0208-x
[67]. Thu, H. N., Quynh, A. N., Hai, O. K., Thanh, H. L. T., & Thanh, H. N. (2022). Impact of the COVID‐19 pandemic on provision of HIV/AIDS services for key populations. the International Journal of Health Planning and Management, 37(5), 2852–2868. https://doi.org/10.1002/hpm.3508
[68]. Griggs, G. K. (2021). Innovations in Virtual Care During the Pandemic: Implications for the future. North Carolina Medical Journal, 82(4), 252–254. https://doi.org/10.18043/ncm.82.4.252
[69]. Seiler, N., Chaudhry, H. J., Lovitch, K., Heyison, C., Karacuschansky, A., Organick-Lee, P., Osei, A., Stoll, H., Dwyer, G., & Horton, K. (2022). Telehealth services and the law: the rapidly evolving regulatory landscape and considerations for sexually transmitted infection and HIV services. Sexually Transmitted Diseases, 49(11S), S18–S21. https://doi.org/10.1097/olq.0000000000001629
[70]. Conrad, R., Rayala, H., Diamond, R., Jd, Busch, B., Kramer, N., & Ma. (2020). Expanding Telemental Health in Response to the COVID-19 Pandemic. Telemed J E Health. https://www.psychiatrictimes.com/coronavirus/expanding-telemental-health-response-covid-19-pandemic
[71]. Lieber, E., Chin, D., Li, L., Rotheram-Borus, M. J., Detels, R., Wu, Z., & Guan, J. (2009). Sociocultural Contexts and Communication about Sex in China: Informing HIV/STD Prevention Programs. AIDS Education and Prevention, 21(5), 415–429. https://doi.org/10.1521/aeap.2009.21.5.415
Cite this article
Liao,W. (2024). The impact on prevention and control strategies for HIV/STIs from COVID-19 pandemic to post-pandemic period in Southern China(2020-2023): A literature review. Theoretical and Natural Science,59,246-258.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 4th International Conference on Biological Engineering and Medical Science
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Vishnu, K. N., Kumar Uppala, P., Vangoori, Y., & Rao Gudhanti, S. N. (2021). A review on Covid 19 pandemic and its global effects. Asian Journal of Pharmaceutical Research, 242–246. https://doi.org/10.52711/2231-5691.2021.00042
[2]. National Health Commission of People’s Republic of China. (2023). http://www.nhc.gov.cn/xcs/zhengcwj/202301/bdc1ff75feb94934ae1dade176d30936.shtml?R0NMKk6uozOC=1673325152096
[3]. Wu, Y., Zhang, Q., Li, L., Li, M., & Zuo, Y. (2021). Control and Prevention of the COVID-19 epidemic in China: A Qualitative community case study. Risk Management and Healthcare Policy, Volume 14, 4907–4922. https://doi.org/10.2147/rmhp.s336039
[4]. Liu, X., McGoogan, J. M., & Wu, Z. (2021). Human immunodeficiency virus/acquired immunodeficiency syndrome prevalence, incidence, and mortality in China, 1990 to 2017: a secondary analysis of the Global Burden of Disease Study 2017 data. Chinese Medical Journal/Chinese Medical Journal, 134(10), 1175–1180. https://doi.org/10.1097/cm9.0000000000001447
[5]. Zheng, Y., Yu, Q., Lin, Y., Zhou, Y., Lan, L., Yang, S., & Wu, J. (2022). Global burden and trends of sexually transmitted infections from 1990 to 2019: an observational trend study. Lancet. Infectious Diseases/the Lancet. Infectious Diseases, 22(4), 541–551. https://doi.org/10.1016/s1473-3099(21)00448-5
[6]. He, N. (2021). Research progress in the epidemiology of HIV/AIDS in China. China CDC Weekly, 3(48), 1022–1030. https://doi.org/10.46234/ccdcw2021.249
[7]. Li, T. (2022). Chinese guidelines for the diagnosis and treatment of hiv/aids (2021 edition). Infectious Diseases & Immunity.
[8]. Güner, R., Hasanoğlu, I., & Aktaş, F. (2020). COVID-19: Prevention and control measures in community. Turkish Journal of Medical Sciences, 50(SI-1), 571–577. https://doi.org/10.3906/sag-2004-146
[9]. Zhao, H. (1988). The People’s Republic of China--South. In The Geojournal library (pp.355 – 368). https://doi.org/10.1007/978-94-009-2999-9_40
[10]. Yan, J., Li, Y., & Zhou, P. (2022). Impact of covid-19 pandemic on the epidemiology of stds in China: Based on the GM (1,1) model. BMC Infectious Diseases. https://doi.org/10.21203/rs.3.rs-994599/v1
[11]. Ernst, P., Chen, M. F., Wang, N. S., & Cosio, M. (1983). Symbiosis of Pneumocystis carinii and cytomegalovirus in a case of fatal pneumonia. PubMed, 128(9), 1089–1092. https://pubmed.ncbi.nlm.nih.gov/6301670
[12]. Starace, F., Bartoli, L., Aloisi, M. S., Antinori, A., Narciso, P., Ippolito, G., Ravasio, L., Moioli, M. C., Vangi, D., Gennero, L., Coronado, O. V., Giacometti, A., Nappa, S., Perulli, M. L., Montesarchio, V., La Gala, A., Ricci, F., Cristiano, L., De Marco, M., . . . Monforte, A. D. (2002). Cognitive and affective disorders associated to HIV infection in the HAART era: findings from the NeuroICONA study. Acta Psychiatrica Scandinavica, 106(1), 20–26. https://doi.org/10.1034/j.1600-0447.2002.02289.x
[13]. Chen, H., Luo, L., Pan, S. W., Lan, G., Zhu, Q., Li, J., Zhu, J., Chen, Y., Shen, Z., Ge, X., Tang, Z., Xing, H., Shao, Y., Ruan, Y., & Yang, W. (2019). HIV Epidemiology and Prevention in Southwestern China: Trends from 1996-2017. Current HIV Research, 17(2), 85–93. https://doi.org/10.2174/1570162x17666190703163838
[14]. Lin, Q., Deng, B., Rui, J., Guo, S. B., Hu, Q. Q., Chen, Q. P., Tang, C., Zhou, L. A., Zhao, Z. Y., Lin, S. N., Zhu, Y. Z., Yang, M., Wang, Y., Xu, J. W., Liu, X. C., Yang, T. L., Li, P. H., Li, Z. Y., Luo, L., . . . Chen, T. M. (2021). Epidemiological Characteristics and Transmissibility of Human Immunodeficiency Virus in Nanning City, China, 2001-2020. Frontiers in Public Health, 9, Article 689575. https://doi.org/10.3389/fpubh.2021.689575
[15]. Wong, W. C. W., Tucker, J. D., Man, H. K., Emch, M., Yang, L. G., & Zhao, Y. (2021). Prevalence and contextual risk factors of sexually transmitted infections in Hong Kong: abridged secondary publication. Hong Kong Med J, 3, 40–43. https://europepmc.org/article/MED/34075891
[16]. Feng, Y., Xu, Y., Zhu, K., Chen, H., & Chen, S. (2023). Analysis on prevalence and influence factors of syphilis in male patients attending STD clinic in Haikou. Zhongguo Xingkexue, 32(01), 144-147. https://kns.cnki.net/kcms2/article/abstract?v=yqeyU9EK6jRIpmsnWOOwvKITVJ1d-hfS_ad_vpW3CDHlzRYl7jpyLhIt5ZgK11AmknKz6gjCi_cHHgU-DalBUbhsWktUNtduZIeeNKoz6gYHWaNKFixuPdL-ydvO6E_kzhWpvolMTPELO6i0VJ8McQ==&uniplatform=NZKPT&language=CHS
[17]. Zeng, X., Fu, P., Wang, Z., Zhang, F., Zheng, Y., & Qin, L., (2020). Analysis on the characteristics and transmission routes of AIDS epidemic in Hainan. China Tropical Medicine, 20(8), 735-738. https://doi.org/10.13604/j.cnki.46-1064/r.2020.08.09
[18]. Luo, J., Yang, Y., Liang, S., Xiong, T., Meng, W., & He, Q. (2019). Analysis on HIV/AIDS epidemic situation in Panyu district, Guangzhou, from 2010 to 2017. Journal of Tropical Medicine, 19(07), 907-909. https://kns.cnki.net/kcms2/article/abstract?v=yqeyU9EK6jQRDQ54l_G9OiTUW1Sv6723IjczZ110-MM19q0Ocs_MKzWAMKIsgrGr4evyuPzXXfWNgOcWvweqdsqGX0CDMMPxGEZsthgjfundcX91QWAGfJYWMQeLaPx7-A1_XhPmnh6nhwgdAEWN0Q==&uniplatform=NZKPT&language=CHS
[19]. Lu, J., Xu, Y., Zhu, K., & Feng, Z. (2020). Current status and countermeasures for Chlamydia trachomatis infection in the reproductive tract in Hainan Province, 2009-2017. Chinese Journal of AIDS & STD, 26(02), 209-211. https://doi.org/10.13419/j.cnki.aids.2020.02.28
[20]. Chunru, L. U. (2019). Analysis on hiv,tp and hsv-2 virus infection status and influencing factors in msm population in longgang district of shenzhen. China Medicine and Pharmacy.
[21]. Zhu, C., Yang, Y., Wu, S., Liang, S., Xiong, T., & Meng, W. (2021). AIDS epidemic characteristics in men who have sex with men at Panyu District, Guangzhou from 2007 to 2020. International Medicine and Health Guidance News, 27(13), 1899-1903. https://doi.org/10.3760/cma.j.issn.1007-1245.2021.13.001
[22]. Wang, Z., Zheng, Y., Zhao, D., Qin, L., Yan, C., & Lu, Q. (2022). Trends and Causes Analysis of HIV Infection Rate Among Cross-Sectional Surveys of Men Who Had Sex with Men in Haikou Prefecture 2008-2017. the Chinese Journal of Dermatovenereology, 36(6), 683-689. https://doi.org/10.13735/j.cjdv.1001-7089.202111042
[23]. Yang, D., Jiang, F., Liu, Y., & Fu, X. (2021). HIV infection status of men who have sex with men and its influencing factors in Guilin, 2017-2020. South China Journal of Preventive Medicine, 47(10), 1315-1318. https://doi.org/10.12183/j.scjpm.2021.1315
[24]. Liang, B., Zhang, F., Ou, Y., Zhang, P., Bao, L., Mo, S., Nong, A., Wei, D., Wu, Z., Xie, H., Yang, Y., Liu, D., Liang, H., & Ye, L. (2023). Prevalence, trends and correlates of HIV, syphilis and HCV infection among Chinese local and cross-border migrant female sex workers in the Sino-Vietnam border area of Guangxi, 2016–2021. AIDS and Behavior, 28(4), 1257–1269. https://doi.org/10.1007/s10461-023-04153-6
[25]. Wang, J., Zhao, P., Xu, W., & Wang, C. (2023). Changing trends in Chlamydia and gonorrhea infections among female sex workers in Southern China: a surveillance data analysis spanning 2019 to 2022. Journal of Public Health. https://doi.org/10.1093/pubmed/fdad222
[26]. Wei, T., Shao-Chu, L. , & Jin, Z. . (2019). Modes of hiv transmission through heterosexual contact among hiv/aids cases in shenzhen city. Practical Preventive Medicine.
[27]. Yang, D., Jiang, F., Xu, F., Fu, X., & Liu, Y. (2022). Analysis of the results of HIV STD surveillance in the client population in Guilin, 2015-2019. South China Journal of Preventive Medicine, 48(01), 74-76, 80. https://kns.cnki.net/kcms2/article/abstract?v=yqeyU9EK6jTE8RqOL4UV0EsKhHNaoyFyRPrtUkijkWmZNx-PfkGB_HGPzLfbOr8LqeaSt6j-oAnrW4KHtlYn6t5eyecwh3KbvnDY81l8HblP92ONYF_raLoYHbljxeMt6wUp_cZV80dx7h4bVR2PZw==&uniplatform=NZKPT&language=CHS
[28]. Zhan, J., Mo, J., Xu, X., Liu, J., & Qin, W. (2023). Analysis of sentinel surveillance on AIDS among drug users in Nanning from 2019 to 2021. Prasitoses and infectious Diseases, 21(4), 187-191,197. https://d.wanfangdata.com.cn/periodical/ChlQZXJpb2RpY2FsQ0hJTmV3UzIwMjMxMjI2EhFzeWpzY2J6ejIwMjMwNDAwMhoIMXg2MnU4bzQ%3D
[29]. Lin, Z., Zhi, J., Chen, H., Jiang, J., Chen, Y., & Liang, B. (2019). Analysis on infection status of sexually transmitted diseases and influencing factors of HIV infection among drug users in Qinzhou. Henan Journal of preventive Medicine, 30(06), 401-404, 417. https://doi.org/10.13515/j.cnki.hnjpm.1006-8414.2019.06.001
[30]. Mai, J., Zeng, G., & Tan, X. (2019). Study on HIV Infection Status and Risk Factors of Drug Abusing Population in Yangjiang City. Strait Journal of Preventive Medicine, 25(03), 37-39. https://kns.cnki.net/kcms2/article/abstract?v=yqeyU9EK6jTbGiuAx_1QpNJm86oufMQdGqRgPYlbM-zuSGRxEf1vOw04z7rOCL6jGQXZA37nE0ZUJADpCrJrIDaF3RRoY4wBqOsTH2gQZx9DfU3mQ6suUsu64JR79jg2JSKv3BMiNzA85egMuB1d9A==&uniplatform=NZKPT&language=CHS
[31]. Zhang, D., Qin, X., Ye, R., Qin, X., Jiang, N., & Li, J. (2021) Epidemiological characterisation of HIV/AIDS cases among adolescent males aged 15-24 years in Yulin City, 2011-2020. Applied Preventive Medicine, 27(6), 547-549. https://doi.org/10.3969/j.issn.1673-758X.2021.06.020
[32]. Zeng, X., Wang, Z., Zhang, F., Zheng, Y., & Fu, P. (2021) The epidemic characteristics and risk factors of AIDS among students in Hainan Province. Zhongguo Jiankang Jiaoyu, 37(06), 492-495. https://doi.org/10.16168/j.cnki.issn.1002-9982.2021.06.003
[33]. Li, X., & Wang, C. (2019). Epidemiological characterisation of AIDS-related characteristics among young students in Huizhou City (2010-2018). Journal of Dermatology and Venereology, 41(3), 342-343. https://doi.org/10.3969/j.issn.1002-1310.2019.03.012
[34]. Nailing, M. , Weigui, G. , Xianrui, W. , Juxian, P. , & Jiannan, L. . (2019). Hiv/aids epidemic status among students in beihai, guangxi, 2007-2018. China Tropical Medicine.
[35]. Lu, Z., Zhao, P. Z., Lu, H. J., & Xiao, M. F. (2023). Analyses of human papillomavirus, Chlamydia trachomatis, Ureaplasma urealyticum, Neisseria gonorrhoeae, and co-infections in a gynecology outpatient clinic in Haikou area, China. Bmc Womens Health, 23(1), Article 117. https://doi.org/10.1186/s12905-023-02259-6
[36]. Wang, C., Zhao, P. Z., Xiong, M. Z., Tucker, J. D., Ong, J. J., Hall, B. J., Sami, M., Zheng, H. P., & Yang, B. (2021). New Syphilis Cases in Older Adults, 2004-2019: An Analysis of Surveillance Data From South China. Frontiers in Medicine, 8, Article 781759. https://doi.org/10.3389/fmed.2021.781759
[37]. Zhao, J. Y., Chen, Q. P., Fu, C. Y., Qin, Q. H., Huang, H. F., Feng, Y. Y., Wei, Y. C., Li, Y., Huang, A. D., Xu, Q. Q., & She, S. Y. (2020). Rate of the HIV Transmission and Associated Factors Among HIV-Exposed Infants in Guangxi, China: 2014-2019. Aids Research and Human Retroviruses, 36(8), 647-655. https://doi.org/10.1089/aid.2020.0073
[38]. Zhong, S., Ou, Y., Zhang, F., Lin, Z., Huang, R., Nong, A., Wu, Z., Liang, H., Qin, C., Wei, Q., Yang, Y., Yu, D., Tang, X., Ye, L., Liu, D., Liang, H., & Liang, B. (2022). Prevalence trends and risk factors associated with HIV, syphilis, and hepatitis C virus among pregnant women in Southwest China, 2009-2018. AIDS Res Ther, 19(1), 31. https://doi.org/10.1186/s12981-022-00450-7
[39]. Yan, Y., Ai, X., Gao, H., Yang, C., & Liu, Y. (2023) Analysis on epidemiology of hepatitis B, syphilis and AIDS among pregnant women in Guangzhou from 2017 to 2021. Journal of Tropical Medicine, 23(07), 1034-1038. https://kns.cnki.net/kcms2/article/abstract?v=yqeyU9EK6jSlLguHC0n8-MKe263v613Yz073xakeaOZqOL2hZTpQoFNPROkBS-7XPdkzdIiKvs0O31P1UMxaoPDU-EzQHuruHxPRA8VZyCLSI9CRdCbq8m8PscpQ1hmbTHkIRLG-wijcgwap08UP2g==&uniplatform=NZKPT&language=CHS
[40]. Zeng, G., Ye, C., Liu, C., Liang, S., & Yang, G. (2022). Epidemiological characteristics of newly reported HIV/AIDS cases aged ≥50 years in Yangjiang City, 2017-2021. Jiangsu Journal of Preventive Medicine, 33(6), 699-701. https://doi.org/10.13668/j.issn.1006-9070.2022.06.022
[41]. Tan, L., Chen, Y., Li, J., & Huang, S. (2020). Analysis of the elderly HIV/AIDS cases in Wuzhou, Guangxi, 2014-2018. China Tropical Medicine, 20(1), 49-52. https://doi.org/10.13604/j.cnki.46-1064/r.2020.01.11
[42]. Chimungu, B., Fu, M. Q., Wu, J., Wu, J. L., Huang, L. P., Dai, Y. C., Tang, S. X., Zhang, J. M., & Wan, C. S. (2020). Prevalence of sexually transmitted infections among foreigners living in Guangzhou, China: a cross-sectional study (2010-2017). Bmc Infectious Diseases, 20(1), Article 345. https://doi.org/10.1186/s12879-020-04995-8
[43]. Hall, B. J., Yang, X. Y., Huang, L., Yi, G. C., Chan, E. W. W., Tucker, J. D., & Latkin, C. A. (2020). Barriers and Facilitators of Rapid HIV and Syphilis Testing Uptake Among Filipino Transnational Migrants in China. Aids and Behavior, 24(2), 418-427. https://doi.org/10.1007/s10461-019-02449-0
[44]. Li, Z., Sun, K., Zhu, Y., Qi, P., Ming, H., & Chen, C. (2023). Survey on syphilis among exit travelers at Guangzhou port from 2016 to 2019. Chinese Journal of Frontier Health and Quarantine, 46(06), 575-577. https://doi.org/10.16408/j.1004-9770.2023.06.017
[45]. Huang, N., Li, X., Liang, R., Chen, J., Qi, P., & Wen, Y. (2022). Analysis of HIV infection status of entry-exit population at Guangzhou port from 2010 to 2020. Chinese Journal of Frontier Health and Quarantine, 45(02), 163-166. https://doi.org/10.16408/j.1004-9770.2022.02.020
[46]. Thu, H. N., Quynh, A. N., Hai, O. K., Thanh, H. L. T., & Thanh, H. N. (2022). Impact of the COVID‐19 pandemic on provision of HIV/AIDS services for key populations. the International Journal of Health Planning and Management, 37(5), 2852–2868. https://doi.org/10.1002/hpm.3508
[47]. Liu, J., Kamarudin, K. M., Liu, Y., Zou, J., & Zhang, J. (2022). Developing a behavior change framework for pandemic prevention and control in public spaces in China. Sustainability, 14(4), 2452. https://doi.org/10.3390/su14042452
[48]. Pachauri, S., Pachauri, A., & Mittal, K. (2021). Men Who Have Sex with Men. In SpringerBriefs in public health (pp. 9–25). https://doi.org/10.1007/978-981-16-4578-5_2
[49]. Ross, M. W. (1992). Men who have sex with men. AIDS Care, 4(4), 457 – 459. https://doi.org/10.1080/09540129208253122
[50]. Koblin, B. A., Husnik, M. J., Colfax, G., Huang, Y., Madison, M., Mayer, K., Barresi, P. J., Coates, T. J., Chesney, M. A., & Buchbinder, S. (2006). Risk factors for HIV infection among men who have sex with men. AIDS, 20(5), 731–739. https://doi.org/10.1097/01.aids.0000216374.61442.55
[51]. Baber, J., & Dayan, L. (2006). Men who have sex with men--a management approach for GPS. Aust Fam Physician, 35(10), 797–800. https://www.ncbi.nlm.nih.gov/pubmed/17019455
[52]. Men Who Have Sex with Men. (2005). [Dataset]. In PsycEXTRA Dataset. https://doi.org/10.1037/e663272007-001
[53]. Ma, S., Chen, Y., Lai, X., Lan, G., Ruan, Y., Shen, Z., Zhu, Q., & Tang, S. (2022). Predicting the HIV/AIDS epidemic and measuring the effect of AIDS Conquering Project in Guangxi Zhuang Autonomous Region. PloS One, 17(7), e0270525. https://doi.org/10.1371/journal.pone.0270525
[54]. Tang, X. J., Chen, W., Tang, S. Q., Zhao, P. Z., Ling, L., & Wang, C. (2022). The evaluation of preventive and control measures on congenital syphilis in Guangdong Province, China: a time series modeling study. Infection, 50(5), 1179-1190. https://doi.org/10.1007/s15010-022-01791-1
[55]. Wu, R., Tan, T., & Gao, H. (2022). A review of HIV epidemic trend analysis and prevention strategies. Chinese Practical Journal of Rural Doctor, 29(08), 28-31. https://kns.cnki.net/kcms2/article/abstract?v=yqeyU9EK6jTIhmZaWrvpIJYYGJJsCyWSloFP2JR4tkVH6KwU1je6u9u9c2DMj5adW5ATPBTEZ28y5uYhYP-2gNTIIki9laiSZBmM81Q1uZwEot_fJrWrE5uk6XwKzX5l3feWLG29gJkq1DNM_ovvcg==&uniplatform=NZKPT&language=CHS
[56]. AIDS, Hepatitis, C, Professional, Group, & Society, et al. (2018). chinese guidelines for diagnosis and treatment of hiv/aids (2018). Zhonghua Nei Ke Za Zhi.
[57]. McFall, A. M., Menezes, N. P., Srikrishnan, A. K., Solomon, S. S., Anand, S., Baishya, J. J., Lucas, G. M., Celentano, D. D., & Mehta, S. H. (2022). Impact of the COVID‐19 pandemic on HIV prevention and care services among key populations across 15 cities in India: A longitudinal assessment of clinic‐based data. Journal of the International AIDS Society, 25(7). https://doi.org/10.1002/jia2.25960
[58]. Booton, R. D., Fu, G., MacGregor, L., Li, J., Ong, J. J., Tucker, J. D., Turner, K. M., Tang, W., Vickerman, P., & Mitchell, K. M. (2021). The impact of disruptions due to COVID‐19 on HIV transmission and control among men who have sex with men in China. Journal of the International AIDS Society, 24(4). https://doi.org/10.1002/jia2.25697
[59]. Ogunbodede, O. T., Zablotska-Manos, I., & Lewis, D. A. (2021). Potential and demonstrated impacts of the COVID-19 pandemic on sexually transmissible infections: Republication. Current Opinion in HIV and AIDS, 16(2), 115–120. https://doi.org/10.1097/coh.0000000000000672
[60]. Brohi, S. N., Jhanjhi, N., Brohi, N. N., & Brohi, M. N. (2020). Key Applications of State-of-the-Art Technologies to Mitigate and Eliminate COVID-19. https://doi.org/10.36227/techrxiv.12115596
[61]. Jnr, N. B. A. (2020). Use of telemedicine and virtual care for remote treatment in response to COVID-19 pandemic. Journal of Medical Systems, 44(7). https://doi.org/10.1007/s10916-020-01596-5
[62]. Mehraeen, E., Mehrtak, M., SeyedAlinaghi, S., Nazeri, Z., Afsahi, A. M., Behnezhad, F., Vahedi, F., Barzegary, A., Karimi, A., Mehrabi, N., Dadras, O., & Jahanfar, S. (2022). Technology in the Era of COVID-19: A Systematic Review of Current evidence. Infectious Disorders. Drug Targets, 22(4). https://doi.org/10.2174/1871526522666220324090245
[63]. Appleton, R., Williams, J., Juan, N. V. S., Needle, J. J., Schlief, M., Jordan, H., Rains, L. S., Goulding, L., Badhan, M., Roxburgh, E., Barnett, P., Spyridonidis, S., Tomaskova, M., Mo, J., Harju-Seppänen, J., Haime, Z., Casetta, C., Papamichail, A., Lloyd-Evans, B., . . . Johnson, S. (2021). Implementation, adoption, and Perceptions of Telemental Health during the COVID-19 Pandemic: Systematic review. JMIR. Journal of Medical Internet Research/Journal of Medical Internet Research, 23(12), e31746. https://doi.org/10.2196/31746
[64]. Portman, M. (2018). HIV prevention strategies. Medicine, 46(5), 293– 299. https://doi.org/10.1016/j.mpmed.2018.02.009
[65]. Jones, A., Cremin, I., Abdullah, F., Idoko, J., Cherutich, P., Kilonzo, N., Rees, H., Hallett, T., O’Reilly, K., Koechlin, F., Schwartlander, B., De Zalduondo, B., Kim, S., Jay, J., Huh, J., Piot, P., & Dybul, M. (2014). Transformation of HIV from pandemic to low-endemic levels: a public health approach to combination prevention. Lancet, 384(9939), 272–279. https://doi.org/10.1016/s0140-6736(13)62230-8
[66]. Vermund, S. H. (2014). Global HIV Epidemiology: A guide for strategies in prevention and care. Current HIV/AIDS Reports, 11(2), 93–98. https://doi.org/10.1007/s11904-014-0208-x
[67]. Thu, H. N., Quynh, A. N., Hai, O. K., Thanh, H. L. T., & Thanh, H. N. (2022). Impact of the COVID‐19 pandemic on provision of HIV/AIDS services for key populations. the International Journal of Health Planning and Management, 37(5), 2852–2868. https://doi.org/10.1002/hpm.3508
[68]. Griggs, G. K. (2021). Innovations in Virtual Care During the Pandemic: Implications for the future. North Carolina Medical Journal, 82(4), 252–254. https://doi.org/10.18043/ncm.82.4.252
[69]. Seiler, N., Chaudhry, H. J., Lovitch, K., Heyison, C., Karacuschansky, A., Organick-Lee, P., Osei, A., Stoll, H., Dwyer, G., & Horton, K. (2022). Telehealth services and the law: the rapidly evolving regulatory landscape and considerations for sexually transmitted infection and HIV services. Sexually Transmitted Diseases, 49(11S), S18–S21. https://doi.org/10.1097/olq.0000000000001629
[70]. Conrad, R., Rayala, H., Diamond, R., Jd, Busch, B., Kramer, N., & Ma. (2020). Expanding Telemental Health in Response to the COVID-19 Pandemic. Telemed J E Health. https://www.psychiatrictimes.com/coronavirus/expanding-telemental-health-response-covid-19-pandemic
[71]. Lieber, E., Chin, D., Li, L., Rotheram-Borus, M. J., Detels, R., Wu, Z., & Guan, J. (2009). Sociocultural Contexts and Communication about Sex in China: Informing HIV/STD Prevention Programs. AIDS Education and Prevention, 21(5), 415–429. https://doi.org/10.1521/aeap.2009.21.5.415