1. Introduction
Gestational diabetes mellitus (GDM) is a common pregnancy complication, which refers to abnormal glucose and carbohydrate metabolism that is first diagnosed during pregnancy. Although diabetes is not clearly diagnosed before to pregnancy, it typically shows up in pregnant women as excessively high blood sugar levels [1]. The occurrence of GDM is closely related to increased placental hormone secretion and decreased maternal insulin sensitivity during pregnancy, which can have short-term and long-term effects on the health of pregnant women and fetuses, including the risk of gestational hypertension, macrosomia, and premature birth.
GDM has become a significant public health concern impacting the health of both mothers and their unborn children due to its rising prevalence in pregnant women. In addition to raising the risk of pregnancy problems, GDM is strongly linked to postpartum diabetes, which has a significant effect on both mothers' and babies' long-term health. There is still much to learn about the precise pathophysiology of GDM, particularly in relation to hormones, insulin resistance, and hereditary factors. The majority of current research focuses on analysing individual components, and there is currently a dearth of thorough mechanism study on GDM. Therefore, identifying the pathophysiology of GDM and developing individualised management methods require a thorough investigation of the creation mechanism and various determinants of insulin resistance during pregnancy. The genesis and causes of GDM will be extensively analysed and discussed in this article using a literature review technique. Reviewing the present status of GDM research is the goal, with an emphasis on the disease's pathophysiology, risk factors, and effects on the health of mothers and infants. The essay will also provide an overview of current diagnostic techniques, intervention plans, and pertinent regulations.
2. Factors Contributing to GDM
GDM is influenced by a range of factors that include hormonal changes, underlying medical conditions, and lifestyle factors. These factors can interact in complex ways, contributing to the development of GDM during pregnancy [1].
Firstly, The placenta is responsible for providing essential nutrients and water to the fetus and secreting various hormones that are critical for maintaining pregnancy. Among these hormones, estrogen, cortisol, and human placental prolactin can interfere with insulin function, leading to what is known as the anti-insulin effect. This effect usually appears after 20 to 24 weeks of gestation, as the growing placenta increases the secretion of these hormones. As a result, the body becomes more insulin-resistant, raising the risk of developing GDM. While the pancreas usually compensates for this resistance by producing more insulin, if the pancreas fails to respond adequately, GDM can develop.
A higher risk of GDM is directly linked to pre-existing diseases such polycystic ovarian syndrome (PCOS) in addition to hormonal alterations [2]. High levels of androgens, insulin resistance, and chronic anovulation are the hallmarks of PCOS, a reproductive condition. According to a Northern California study, women with PCOS were 2.4 times more likely to develop GDM, underscoring the need of controlling the condition both before and during pregnancy. Another key factor in GDM development is the relative insufficiency of insulin secretion., which is the failure of maternal β cell mass expansion or the insufficiency of β cell insulin secretion in response to the gradual increase in insulin resistance during pregnancy [3]. Hyperlipidemia, significantly elevated serum triglycerides, may lead to lipotoxic beta cell damage, further impairing insulin secretion capacity. In addition, triglyceride-rich residual cholesterol (RC) is associated with GDM [4]. Research has shown that women with GDM have higher triglyceride levels, about 20% greater than those without GDM, and elevated triglyceride-rich residual cholesterol (RC) early in pregnancy has been positively linked with GDM risk [5].
Maternal physical conditions, particularly pre-pregnancy weight and obesity, play a crucial role in the risk of developing GDM [6]. Women who are overweight (BMI 25-29.99 kg/m²) or obese (BMI ≥ 30 kg/m²) before pregnancy are at high risk for GDM. Compared with women with BMI < 30 kg/m², women with class I obesity (BMI 30 to 34.99 kg/m²) had a nearly three-fold increased risk of GDM, and women with class II obesity (BMI 35 to 39.99 kg/m²) had a nearly four-fold increased risk of GDM(See Figure 1). Rapid weight gain during pregnancy, especially during the first trimester, is also linked to an increased risk of GDM. Finally, advanced age is another important risk factor for gestational diabetes. Advanced maternal age is positively associated with an increased risk of adverse pregnancy outcomes, including gestational diabetes [7]. In other words, as women age, they are more likely to develop insulin resistance and other metabolic changes, which increase the likelihood of developing gestational diabetes.
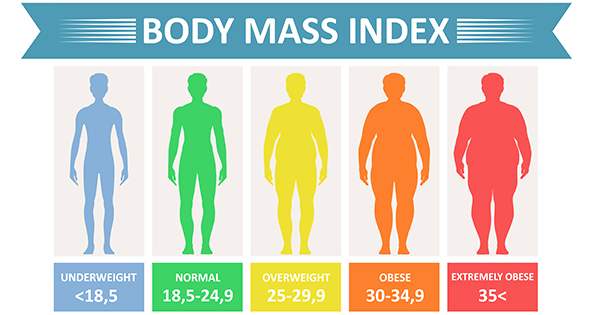
Figure 1: Body Mass Index
3. The effects and diagnosis of GDM
GDM can result in both short and long-term health consequences for the mother and their offspring. GDM increases the likelihood of pregnancy complications such as pre-eclampsia, high blood pressure, cesarean section, and macrosomia. Pre-eclampsia, a severe condition that may occur during or after pregnancy, is characterized by elevated blood pressure and the presence of protein in the urine. It increases the risk of high blood pressure, diabetes, premature birth, and miscarriage. Research has shown that women with gestational diabetes have a significantly increased risk of developing type 2 diabetes in the years after giving birth.
GDM also leads to a higher incidence of neonatal complications, such as respiratory distress syndrome, neonatal jaundice, and low Apgar score. Babies born before 37 weeks of pregnancy are more likely to have difficulty breathing, low blood sugar, and jaundice—obesity and type 2 diabetes [8]. Moreover, children born to mothers with gestational diabetes are more likely to develop obesity and type 2 diabetes later in life. Respiratory distress syndrome (RDS) primarily affecting premature infants born before 28 weeks of gestation, is caused by a deficiency of surfactants, which are essential for maintaining proper lung expansion and breathing [8].
4. GDM detection and treatment criteria
4.1. Management and Treatment of Gestational Diabetes
Gestational diabetes is usually treated through a particular diet plan and regular physical exercise and may also include daily blood sugar testing and insulin injections [9]. Vitamin D deficiency is common among pregnant women. It is associated with pregnancy complications such as gestational diabetes, hypertension, preterm birth, and early gestational age [10]. In women with gestational diabetes, vitamin D supplementation (1000-4762 IU/ day) reduces FBG, HbA1c, and serum insulin concentrations, enhancing glucose metabolism. Additionally, taking 1000 IU of vitamin D3 daily significantly lowers serum triglyceride, VLDL, total cholesterol, and LDL concentrations while reducing birth weight and the incidence of macrosomia (3.3% vs. 16.7%, p = 0.08). The primary goal is to achieve blood sugar levels comparable to those of pregnant women without gestational diabetes [10].. Inositol is a naturally occurring polyol sugar found in grains, legumes, nuts, meats, legumes, and fresh citrus fruits, acts as an insulin-sensitizing agent, improving insulin sensitivity and ovulation function, particularly in women with PCOS [2].. According to Diabetes UK, pregnant women with gestational diabetes should focus on starchy, low glycemic index (GI) foods such as whole wheat pasta, brown rice, whole-grain bread, cereals, beans, lentils, and porridge. A diet rich in fruits, vegetables, and lean proteins like fish is recommended, while sugary foods and drinks should be replaced with healthier alternatives like nuts, seeds, and low-sugar beverages.
4.2. Long-Term Dietary Focus
Follow a healthy diet and exercise regularly as recommended by the American Diabetes Association for managing gestational diabetes. The guidelines suggest combining aerobic exercises (like walking) and strength exercises (such as weight lifting) for at least 20 minutes each day. Pregnant women who engage in physical activity can achieve their desired blood sugar levels. Engaging in physical activity can assist a pregnant lady in bringing her blood pressure or cholesterol levels down to a healthy level. Additionally, exercise during pregnancy can lower stress, maintain joint flexibility, strengthen the heart and bones, and increase muscular strength. Additionally, it can lower the risk of type 2 diabetes. Women with GDM should also keep a daily check on their blood sugar levels. Typically, blood glucose (blood sugar) is tested. Before breakfast, one or two hours after waking up, and one or two hours after meals start [10]. Along with pregnan women eating plans and staying active, insulin is usually used, when necessary, to manage blood glucose. The target blood glucose range is as follows: fasting levels should be under 95 mg/dL, one hour after a meal should be below 140 mg/dL, and two hours after a meal should be under 120 mg/dL. If a woman's blood sugar is still unstable after 1 to 2 weeks of diet and exercise, she may need medication. This is especially true if her blood sugar was very high at diagnosis or if she has been diagnosed with gestational diabetes (GDM). The doctor may recommend metformin (a pill) or insulin injections. Metformin is usually taken up to 3 times a day with or after meals.
Besides, dietary advice and interventions are essential for preventing gestational diabetes. Experts recommend consuming more foods with a low dietary GI. GI refers to the ability of carbohydrate foods to induce postprandial blood glucose. Compared with the rapid increase in postprandial blood glucose caused by high-GI foods, low-GI foods (such as whole grains and various fruits and vegetables) can cause a low increase in postprandial blood glucose concentration. Dietary fiber may affect blood glucose stability through several mechanisms. For example, Dietary fibre may influence blood glucose stability through a variety of methods. A high-fiber diet reduces hunger and overall energy intake, resulting in weight loss and improved insulin sensitivity. In addition, higher fibre intake may lower glucose absorption and insulin secretion by delaying stomach emptying and decreasing digestion. On the other hand, the intake of red meat and processed meat may affect blood glucose control through multiple mechanisms. These mechanisms include the negative effects of components such as saturated fat and cholesterol, the effects of nitrites used as preservatives on insulin sensitivity and pancreatic beta cell function, and the toxic effects of advanced glycation end products (AGE) generated during heating and processing of meat. Restricting caloric intake may further improve blood glucose control and insulin sensitivity by promoting weight loss and reducing fat mass.
4.3. Global Sustainable Solutions
The World Health Organization (WHO) launched the Global Diabetes Compact in 2021, a comprehensive framework that provides countries with a thorough plan to improve diabetes care as part of a broader NCD strategy. The Compact's aim is to strengthen healthcare systems to ensure that all people, including pregnant women at risk of gestational diabetes, receive appropriate screening and care. It emphasizes equitable access to diagnosis, treatment, and essential services, intending to leave no patient behind due to resource constraints [11].
In 2022, the 75th World Health Assembly adopted ambitious global targets for diabetes management to be achieved by 2030, such as diagnosing 80% of people with diabetes, achieving glycemic control in 80% of those diagnosed, and ensuring that 100% of people with type 1 diabetes have access to affordable insulin and monitoring tools. Although GDM is not explicitly included in these targets, WHO emphasizes that effective GDM screening and treatment are critical to preventing long-term risks such as type 2 diabetes and cardiovascular disease in mothers and offspring. WHO recommends that GDM screening with a 75-g oral glucose tolerance test (OGTT) be included in maternal care plans and emphasizes the importance of early diagnosis during pregnancy and regular postpartum follow-up to mitigate future health risks. These efforts reflect a global commitment to making diabetes a public health priority, aimed at reducing intergenerational disparities and improving outcomes for people with GDM. In the United States, a multifaceted approach has been adopted, including universal GDM screening starting at 24 weeks of pregnancy, cost-reduction initiatives, and education programs. Policies such as the Affordable Care Act (ACA) require GDM screening as a preventive service, while some states have expanded Medicaid coverage to improve accessibility for low-income populations. The American Diabetes Association (ADA) further advocates for insurance reform and cost caps for basic diabetes management products (such as insulin), while emphasizing that lifestyle interventions, including personalized nutrition and physical activity, are effective strategies for managing GDM.
The world should continue to promote equity and accessibility in diabetes care, strengthen policy coordination and resource allocation. The focus will be on promoting GDM screening and postpartum follow-up, and increasing service coverage for low-income and vulnerable groups. At the same time, more personalized nutrition guidance, healthy lifestyle interventions and innovative technology applications will be incorporated to comprehensively reduce intergenerational health disparities and achieve the sustainable development goals of diabetes management.
5. Conclusion
In conclusion, GDM poses a significant public health challenge due to its rising prevalence and its effects on maternal and infant health. This article highlights that GDM is influenced by hormonal fluctuations, genetic predisposition, insulin resistance, and lifestyle factors. It is associated with both immediate risks, such as pregnancy complications, and long-term consequences, including an elevated risk of type 2 diabetes for both mothers and their children. Effective management of GDM necessitates a comprehensive approach, incorporating dietary adjustments, regular physical activity, consistent blood glucose monitoring, and, when required, medication or insulin therapy.
In addition, public health strategies that emphasize dietary recommendations, such as the adoption of low-glycemic index foods and high-fiber diets, and global interventions targeting obesity and physical inactivity are essential to reduce the incidence of GDM. Continued research on the underlying mechanisms of GDM and the development of personalized intervention strategies are essential to advance care and mitigate its health impact. However, this study did not explore in depth how ethnic, cultural, and socioeconomic factors affect the incidence and management of GDM, which may have significant effects in different populations. Future research should focus on the impact of different social, cultural, and economic backgrounds on the incidence and management of GDM to provide a basis for the development of more inclusive public health policies.
References
[1]. Sweeting, A., Wong, J., Murphy, H. R., & Ross, G. P. (2022). A clinical update on gestational diabetes mellitus. Endocrine Reviews, 43(5), 763–793. https://doi.org/10.1210/endrev/bnac003
[2]. Lo, J. C., Feigenbaum, S. L., Escobar, G. J., Yang, J., Crites, Y. M., & Ferrara, A. (2006). Increased prevalence of gestational diabetes mellitus among women with diagnosed polycystic ovary syndrome: A population-based study. Diabetes Care, 29(8), 1915–1917. https://doi.org/10.2337/dc06-0877
[3]. Hu, J., et al. (2021). Association of maternal lipid profile and gestational diabetes mellitus: A systematic review and meta-analysis of 292 studies and 97,880 women. eClinicalMedicine, 34, 100830.
[4]. Contreras-Duarte, S., Carvajal, L., Fuenzalida, B., Cantin, C., Sobrevia, L., & Leiva, A. (2019). Maternal dyslipidaemia in pregnancy with gestational diabetes mellitus: Possible impact on foetoplacental vascular function and lipoproteins in the neonatal circulation. Current Vascular Pharmacology, 17(1), 52–71. https://doi.org/10.2174/1570161115666171116154247
[5]. Su, S., Zhang, E., Gao, S., et al. (2024). Associations of remnant cholesterol in early pregnancy with gestational diabetes mellitus risk: A prospective birth cohort study. Lipids in Health and Disease, 23, 243. https://doi.org/10.1186/s12944-024-02230-w
[6]. Zhu, Z., Wang, K., Hao, X., Chen, L., Liu, Z., & Wang, C. (2022). Causal graph among serum lipids and glycemic traits: A Mendelian randomization study. Diabetes, 71(8), 1818–1826. https://doi.org/10.2337/db21-0734
[7]. Cleary-Goldman, J., Malone, F. D., Vidaver, J., Ball, R. H., Nyberg, D. A., Comstock, C. H., Saade, G. R., Eddleman, K. A., Klugman, S., Dugoff, L., Timor-Tritsch, I. E., Craigo, S. D., Carr, S. R., Wolfe, H. M., Bianchi, D. W., & D'Alton, M. (2005). Impact of maternal age on obstetric outcome. Obstetrics & Gynecology, 105(5 Part 1), 983–990. https://doi.org/10.1097/01.AOG.0000158118.75532.51
[8]. Yamamoto, J. M., Kellett, J. E., Balsells, M., Garcia-Patterson, A., Hadar, E., Sola, I., & Corcoy, R. (2018). Gestational diabetes mellitus and diet: A systematic review and meta-analysis of randomized controlled trials examining the impact of modified dietary interventions on maternal glucose control and neonatal birth weight. Diabetes Care, 41(7), 1346–1361. https://doi.org/10.2337/dc18-0191
[9]. Persson, M., Norman, M., & Hanson, U. (2009). Obstetric and perinatal outcomes in Type 1 diabetic pregnancies: A large, population-based study. Diabetes Care, 32(11), 2005–2009. https://doi.org/10.2337/dc09-0656
[10]. Zakaria, H. The Role of Lifestyle Interventions in the Prevention and Treatment of Gestational Diabetes Mellitus, Oct 01, 2024
[11]. World Health Organization. (2021). Global Diabetes Compact. Geneva: World Health Organization. Retrieved from https://www.who.int/news-room/fact-sheets/detail/diabetes
Cite this article
Yu,X. (2025). Gestational Diabetes Mellitus Pathogenesis and Comprehensive Management Strategies. Theoretical and Natural Science,96,1-6.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 5th International Conference on Biological Engineering and Medical Science
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Sweeting, A., Wong, J., Murphy, H. R., & Ross, G. P. (2022). A clinical update on gestational diabetes mellitus. Endocrine Reviews, 43(5), 763–793. https://doi.org/10.1210/endrev/bnac003
[2]. Lo, J. C., Feigenbaum, S. L., Escobar, G. J., Yang, J., Crites, Y. M., & Ferrara, A. (2006). Increased prevalence of gestational diabetes mellitus among women with diagnosed polycystic ovary syndrome: A population-based study. Diabetes Care, 29(8), 1915–1917. https://doi.org/10.2337/dc06-0877
[3]. Hu, J., et al. (2021). Association of maternal lipid profile and gestational diabetes mellitus: A systematic review and meta-analysis of 292 studies and 97,880 women. eClinicalMedicine, 34, 100830.
[4]. Contreras-Duarte, S., Carvajal, L., Fuenzalida, B., Cantin, C., Sobrevia, L., & Leiva, A. (2019). Maternal dyslipidaemia in pregnancy with gestational diabetes mellitus: Possible impact on foetoplacental vascular function and lipoproteins in the neonatal circulation. Current Vascular Pharmacology, 17(1), 52–71. https://doi.org/10.2174/1570161115666171116154247
[5]. Su, S., Zhang, E., Gao, S., et al. (2024). Associations of remnant cholesterol in early pregnancy with gestational diabetes mellitus risk: A prospective birth cohort study. Lipids in Health and Disease, 23, 243. https://doi.org/10.1186/s12944-024-02230-w
[6]. Zhu, Z., Wang, K., Hao, X., Chen, L., Liu, Z., & Wang, C. (2022). Causal graph among serum lipids and glycemic traits: A Mendelian randomization study. Diabetes, 71(8), 1818–1826. https://doi.org/10.2337/db21-0734
[7]. Cleary-Goldman, J., Malone, F. D., Vidaver, J., Ball, R. H., Nyberg, D. A., Comstock, C. H., Saade, G. R., Eddleman, K. A., Klugman, S., Dugoff, L., Timor-Tritsch, I. E., Craigo, S. D., Carr, S. R., Wolfe, H. M., Bianchi, D. W., & D'Alton, M. (2005). Impact of maternal age on obstetric outcome. Obstetrics & Gynecology, 105(5 Part 1), 983–990. https://doi.org/10.1097/01.AOG.0000158118.75532.51
[8]. Yamamoto, J. M., Kellett, J. E., Balsells, M., Garcia-Patterson, A., Hadar, E., Sola, I., & Corcoy, R. (2018). Gestational diabetes mellitus and diet: A systematic review and meta-analysis of randomized controlled trials examining the impact of modified dietary interventions on maternal glucose control and neonatal birth weight. Diabetes Care, 41(7), 1346–1361. https://doi.org/10.2337/dc18-0191
[9]. Persson, M., Norman, M., & Hanson, U. (2009). Obstetric and perinatal outcomes in Type 1 diabetic pregnancies: A large, population-based study. Diabetes Care, 32(11), 2005–2009. https://doi.org/10.2337/dc09-0656
[10]. Zakaria, H. The Role of Lifestyle Interventions in the Prevention and Treatment of Gestational Diabetes Mellitus, Oct 01, 2024
[11]. World Health Organization. (2021). Global Diabetes Compact. Geneva: World Health Organization. Retrieved from https://www.who.int/news-room/fact-sheets/detail/diabetes