1. Introduction
Venous thromboembolism (VTE) is the third most common cause of death globally, with its incidence varying by country. In Western countries, it occurs at a rate of 1-2 cases per 1000 person-years, whereas in Eastern countries, it is lower, with fewer than 1 case per 1000 person-years [1]. Approximately 400 million people worldwide live in regions with altitudes above 1500 meters, and hypoxia in the alveoli is the most significant feature of high-altitude environments, significantly affecting the cardiopulmonary system. Chronic hypoxia can lead to pulmonary vascular remodeling and pulmonary arterial hypertension, and chronic cardiopulmonary diseases, thrombotic or embolic diseases are also common among high-altitude residents [2].
Tibetan people have long inhabited the Qinghai-Tibet Plateau, where the high-altitude hypoxic environment affects the respiratory and circulatory systems of the population, making them prone to chronic pulmonary diseases and thrombotic disorders [3]. Chronic pulmonary diseases and their associated complications are the most common conditions encountered in high-altitude respiratory medicine. Therefore, respiratory physicians in the Qinghai-Tibet Plateau need to be vigilant about the occurrence of VTE [4]. Once VTE occurs, detached blood clots can cause acute pulmonary embolism, leading to sudden death. Additionally, it can lead to post-thrombotic syndrome, which can have long-lasting effects on a patient’s physical and mental health [5, 6].
Currently, there is a view that individuals at high risk of VTE should receive early pharmacological intervention. However, a study involving 18,890 patients suggests that routine VTE prevention in high-risk thrombosis patients may increase the risk of bleeding and may not have significant clinical benefits [7]. Therefore, it is crucial to find a predictive method for VTE to guide stratified treatment [8]. The Khorana Score is a scoring system used to predict prognosis in cancer patients based on factors such as cancer site, white blood cell count, hemoglobin levels, platelet count, and body mass index. While it has been used for VTE prediction in recent years, there is currently controversy between the conclusions of several clinical studies [9, 10]. Tibetan patients primarily visit the respiratory department due to respiratory and circulatory system diseases, making the Khorana risk scoreless suitable for this population.
The Caprini Score, introduced in 1991, has undergone extensive clinical validation and is currently used in a new version that includes 10 categories of clinical conditions and more than 40 items for scoring. However, it requires substantial effort and is dependent on close patient cooperation [11]. Therefore, there is a need to find a new, simple, and practical prediction method to accommodate the realities of respiratory intensive care units in Tibetan regions. D-dimer-to-platelet ratio (D-Dime to Platelet Ratio, D-DI/PLT) is an emerging clinical test ratio that is simple and easy to perform and reflects the body’s inflammatory and coagulation status. It has shown effectiveness in predicting various diseases [12]. Therefore, we will analyze the relevant clinical data of Tibetan patients treated in our respiratory and critical care medicine department, incorporating relevant scores and emerging clinical test ratios. We will use statistical methods to identify early indicators for predicting VTE occurrence, which can be used to guide clinical treatment.
2. Research Subjects and Methods:
2.1. Research Subjects and Grouping
Tibetan patients hospitalized in the Department of Respiratory and Critical Care Medicine at People’s Hospital of Lhasa City from September 2021 to August 2023 with diagnoses of acute or chronic high-altitude illness, pulmonary infections, chronic obstructive pulmonary disease, and pulmonary heart disease were included in the study. Exclusion criteria were: 1. Age less than 18 years; 2. Patients with cancer; 3. Failure to complete routine examinations and tests within 24 hours of admission; 4. Failure to complete a 28-day follow-up; 5. Use of anticoagulant medications before admission. Based on whether VTE occurred during hospitalization, patients were divided into the non-VTE group and VTE group.
2.2. Research Methods
Baseline data (gender, age, body mass index, respiration, pulse, blood pressure), routine laboratory results within 24 hours of admission (complete blood count, liver and kidney function, comprehensive coagulation profile, lipid profile), Caprini score, and D-DI/PLT were compared between the two groups. Indicators that showed differences between the groups were identified, and their relationship with the occurrence of VTE was determined through logistic regression analysis. The indicators associated with VTE occurrence were then subjected to COX regression analysis to identify predictors of VTE. Correlation analysis among indicators was conducted to explore their relationships.
2.3. Statistical Methods
Statistical analysis was performed using SPSS 23.0 software. Continuous variables were assessed for normality using the Kolmogorov-Smirnov test. Normally distributed metric data were presented as mean ± standard deviation (x̅±s), and categorical data were presented as percentages (%). Logistic regression was used for the analysis of factors influencing outcomes. ROC curves and the Area under the ROC Curve (AUC) were generated to compare the effectiveness of different indicators in predicting VTE. Pearson correlation analysis was used to assess correlations among indicators, with statistical significance defined as P < 0.05.
3. Results
3.1. Enrollment and Grouping
This study recruited a total of 1002 Tibetan patients who sought medical care at the Department of Respiratory and Critical Care Medicine at People’s Hospital of Lhasa City from September 2021 to August 2023. Following the established inclusion and exclusion criteria, 285 cases that did not meet the criteria were excluded, leaving a final cohort of 717 cases with complete data for inclusion in the study, and they were followed up for 28 days. Based on the occurrence of VTE, the participants were divided into the non-VTE group (582 cases) and the VTE group (135 cases), resulting in a VTE incidence rate of 18.83% (Figure 1).
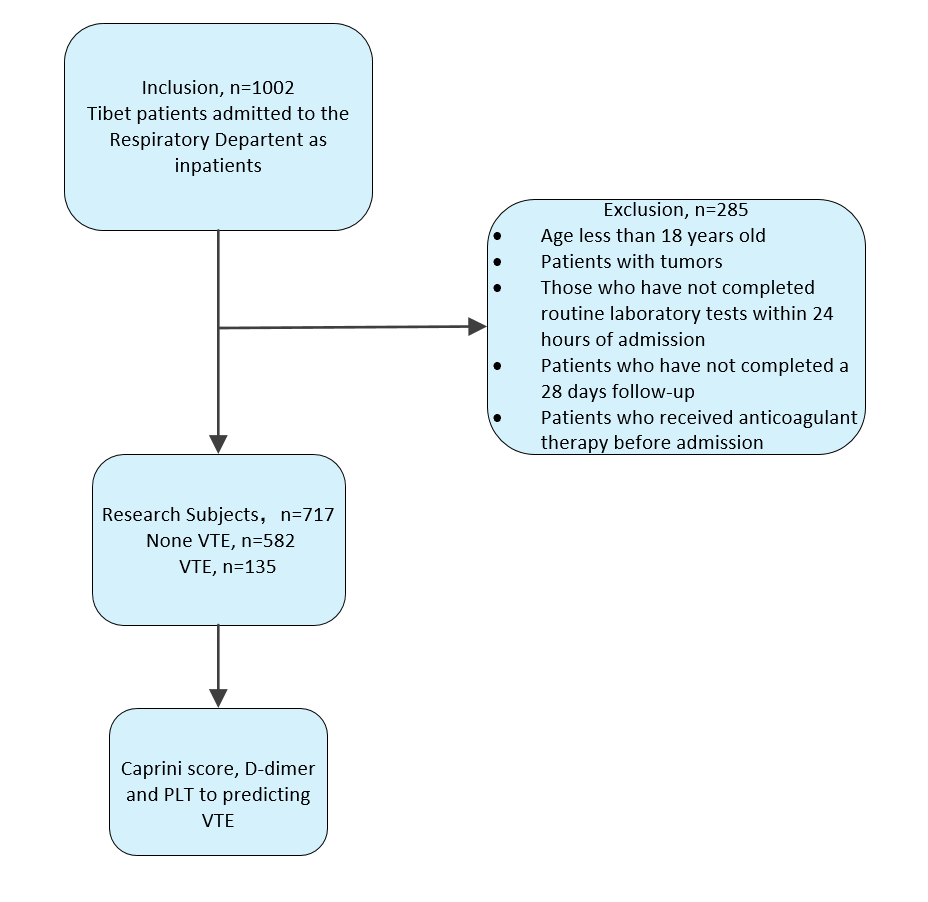
Figure 1. Flowchart of Inclusion and Exclusion.
3.2. Analysis of Baseline Data
Examination within 24 Hours of Admission, and Differences in Other Indicators between the Two Groups Baseline data including gender, age, body mass index, pulse, respiration, and mean arterial pressure were compared between the two groups. It was found that there were significant differences in age and pulse between the VTE group and the non-VTE group (p < 0.05) (Table 1).
Table 1. Analysis of Baseline Data between Two Groups.
Variables | Non-VTE | VTE | t/c2 | p-value |
Male/Female | 309/273 | 68/67 | 0.38 | 0.556 |
Age (years) | 54.27 ± 0.91 | 78.58 ± 1.23 | 6.032 | < 0.001* |
MBI(kg/m2) | 21.62 ± 0.25 | 24. 83± 0.67 | 0.714 | 0.501 |
Pulse Rate (beats/min) | 80.25 ± 0.80 | 87.94 ± 2.01 | 3.078 | 0.002* |
Mean Arterial Pressure(mmHg) | 94.84 ± 0.97 | 98.05 ±1.69 | 1.134 | 0.282 |
The results of comparing the complete blood count, coagulation profile, liver and kidney function, lipid profile, Caprini score, and D-DI/PLT within 24 hours of admission between the two groups revealed significant differences in white blood cell count, hematocrit, platelet count, prothrombin time, D-dimer, total bilirubin, blood urea nitrogen, uric acid, Caprini score, and D-DI/PLT (p < 0.05) (Table 2).
Table 2. Comparison of Examination and Other Indicators within 24 Hours of Admission between the Two Groups.
Variables | Non-VTE | VTE | t | p-value |
WBC(x109/ L) | 6.25±0.23 | 7.89±0.60 | 3.470 | 0.013* |
RBC(x1012/ L) | 5.08±0.15 | 5.30±0.15 | 0.724 | 0.479 |
HGB(g/L) | 153.16±1.62 | 157.05±3.10 | 1.146 | 0.258 |
HTC(%) | 46.63±0.52 | 51.04±3.33 | 2.684 | 0.008* |
PLT(x109/ L) | 229.18±4.80 | 173.38±8.00 | 5.458 | < 0.001* |
PT(s) | 13.12±0.09 | 13.84±0.29 | 3.043 | 0.003* |
APTT(s) | 43.37±1.58 | 40.11±1.21 | 1.032 | 0.309 |
INR | 1.27±0.27 | 1.14±0.03 | 0.274 | 0.81 |
FIB(g/l) | 4.10±0.09 | 4.01±0.17 | 0.446 | 0.097 |
D-DI | 1.06±0.20 | 3.99±0.44 | 5.937 | < 0.001* |
ALT (IU / L) | 35.79±2.37 | 29.96±4.64 | 1.143 | 0.271 |
AST (IU / L) | 29.19±1.56 | 27.93±1.71 | 0.443 | 0.69 |
TBIL(umol / L) | 16.76±0.69 | 22.79±2.06 | 3.365 | < 0.001* |
Cr(umol / L) | 67.12±2.12 | 67.60±2.58 | 0.184 | 0.914 |
BUN(mmol / L) | 4.58±0.18 | 5.78±0.36 | 3.136 | 0.003* |
UA(umol / L) | 323.76±5.89 | 358.56±13.33 | 2.735 | 0.011* |
TC(mmol / L) | 3.87±0.12 | 4.15±0.54 | 0.662 | 0.526 |
TG(mmol / L) | 1.00±0.02 | 0.89±0.04 | 1.962 | 0.057 |
Caprini score | 2.94 ±0.12 | 5.87 ± 0.36 | 11.896 | < 0.001* |
D-DI/PLT | 0.01±0.00 | 0.03±0.00 | 8.223 | < 0.001* |
Note: WBC: White Blood Cell Count, RBC: Red Blood Cell Count, HGB: Hemoglobin, HTC: Hematocrit, PLT: Platelet Count, PT: Prothrombin Time, APTT: Activated Partial Thromboplastin Time, INR: International Normalized Ratio, FIB: Fibrinogen, D-DI: D-Dimer, ALT: Alanine Aminotransferase, AST: Aspartate Aminotransferase, TBIL: Total Bilirubin, Cr: Creatinine, BUN: Blood Urea Nitrogen, UA: Uric Acid, TC: Total Cholesterol, TG: Triglycerides. *p < 0.05.
3.3. Binary Logistic Regression Analysis of Inter-Group Differences
The binary logistic regression analysis included the indicators that showed differences between the two groups, which were age, pulse rate, respiratory rate, white blood cell count, hematocrit, platelet count, prothrombin time, D-dimer, total bilirubin, blood urea nitrogen, uric acid, Caprini score, and D-DI/PLT. The results indicated a significant correlation between white blood cell count, hematocrit, prothrombin time, Caprini score, and D-dimer/PLT and the occurrence of VTE (p < 0.05) (Table 3).
Table 3. Binary Logistic Regression Analysis of Inter-Group Differences.
Variables | B | Standard Error | Wald Coefficient | Significance | OR Value |
Age | -0.025 | 0.014 | 2.805 | 0.088 | 0.973 |
P | -0.011 | 0.009 | 1.482 | 0.266 | 0.990 |
R | -0.050 | 0.029 | 2.904 | 0.090 | 0.962 |
Caprini score | -0.542 | 0.092 | 34.442 | 0.000* | 0.579 |
WBC | -0.116 | 0.050 | 5.517 | 0.020* | 0.889 |
HTC | -0.021 | 0.01 | 4.096 | 0.042* | 0.984 |
PLT | 0 | 0.002 | 0.041 | 0.85 | 1.002 |
PT | 0.214 | 0.078 | 7.509 | 0.007* | 1.264 |
D-dimer | 0.07 | 0.068 | 1.081 | 0.288 | 1.098 |
TBIL | -0.003 | 0.009 | 0.083 | 0.773 | 0.956 |
BUN | -0.039 | 0.041 | 0.902 | 0.353 | 0.946 |
UA | 0.001 | 0.001 | 0.175 | 0.662 | 1.065 |
D-DI/PLT | -36.707 | 14.005 | 6.87 | 0.010* | 0 |
Note: *p< 0.05.
3.4. ROC Curve Analysis for VTE Prediction
The efficacy of white blood cell count, hematocrit, prothrombin time, Caprini score, and D-DI/PLT in predicting VTE was assessed using ROC curve analysis. The results indicated that the areas under the ROC curves for D-DI/PLT and Caprini score were the largest, with D-DI/PLT at 81% and a cutoff value of 0.005, and Caprini score at 83% with a cutoff value of 3.5 (Figure 2A, Table 4).
To verify whether there was a correlation between D-DI/PLT and Caprini score, a Pearson correlation test was conducted, revealing a Pearson coefficient of 0.137, with a 95% confidence interval of -0.001797 to 0.2706, and a p-value of 0.053. This indicates no significant correlation (Figure 2B).
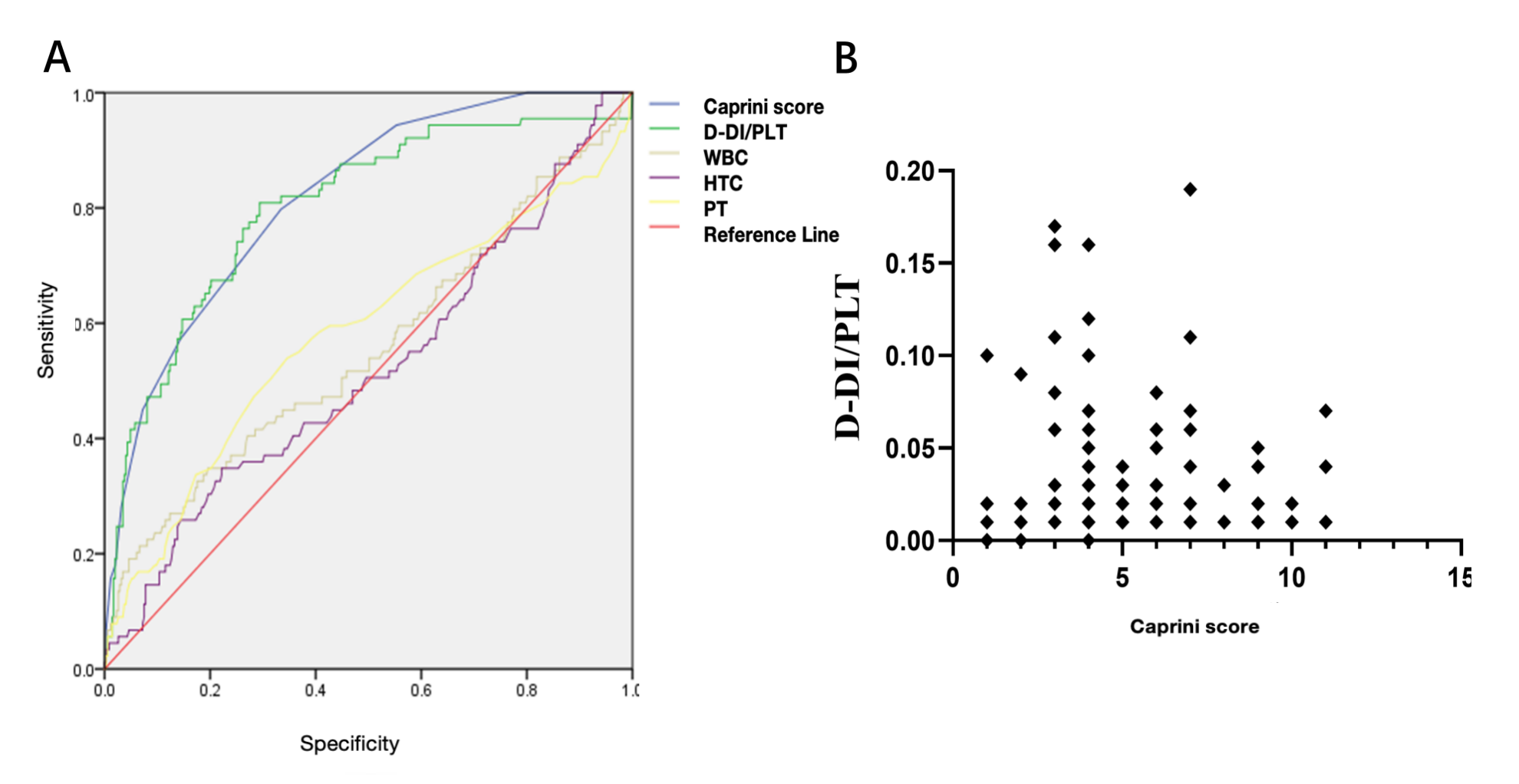
Figure 2. ROC Curve and Correlation Analysis. A: ROC curve for WBC, HCT, PT, Caprini score, and D-DI/PLT in predicting VET. B: Correlation analysis between D-DI/PLT and Caprini score.
Table 4. ROC Curve Analysis Results.
Variables | Area under the curve | Cut-off value | Youden index | p-value | 95% CI |
D-DI/PLT | 0.81 | 0.005 | 45.85 | < 0.001 | 0.771~0.864 |
Caprini score | 0.83 | 3.500 | 43.15 | < 0.001 | 0.744~0.855 |
WBC | 0.56 | 7.730 | 15.19 | 0.102 | 0.483~0.629 |
HTC | 0.52 | 52.450 | 12.59 | 0.562 | 0.449~0.591 |
PT | 0.58 | 13.450 | 19.86 | 0.019 | 0.506~0.654 |
4. Discussion
VTE is a multifactorial disease involving various genetic and acquired risk factors [13]. People of Tibetan ethnicity residing on the Qinghai-Tibet Plateau are affected by high-altitude hypoxia, which disrupts the expression of molecules related to vascular integrity, leading to the occurrence of chronic high-altitude sickness and VTE [14]. The incidence of VTE in individuals residing in high-altitude areas is approximately 6%, significantly higher than in low-altitude regions [15]. The incidence of VTE in low-altitude intensive care units is around 10% [16]. However, our study found that the incidence of VTE in Tibetan patients treated in the respiratory ICU was 18.83%, significantly higher than that in low-altitude ICU patients. Therefore, determining the population at high risk of VTE and providing precise stratified treatment is a challenging issue for respiratory physicians in the Tibetan region.
By analyzing baseline data of 717 Tibetan patients treated in our department and routine examination indicators, including complete blood counts, coagulation profiles, liver and kidney function, and lipid profiles, taken within 24 hours of admission, we identified significant differences in 12 indicators between the non-VTE and VTE groups. Among these, the VTE group was characterized by older age, higher respiratory rate, faster pulse rate, higher white blood cell count, significantly abnormal platelet count, coagulation function, and poorer liver and kidney function. These features suggest that patients in the VTE group may have more severe conditions. Studies have shown that 37.2% of critically ill septic shock patients admitted to the ICU eventually develop VTE [17]. Another survey of severely traumatized patients in the ICU revealed that approximately 27% of patients may develop VTE [18], indicating a relationship between the incidence of VTE and the severity of the condition. We further conducted logistic regression analysis of the intergroup differences and identified 5 indicators, WBC, HTC, PT, D-DI/PLT, and Caprini score, that were significantly correlated with VTE occurrence. ROC analysis confirmed that D-DI/PLT and Caprini score could predict the risk of VTE in Tibetan ICU patients.
D-DI/PLT consists of two clinical parameters, D-DI and PLT, both of which can be rapidly obtained through routine blood tests. The latest evidence suggests that VTE is related to venous endothelial damage caused by local/systemic inflammation and hypoxemia [14]. D-DI, as a good marker of intravascular coagulation and fibrinolysis, can reflect changes in the body’s coagulation status. It has been widely used to assess the overall mortality of inflammatory vascular conditions, thrombotic events, and guidance for the treatment of coagulation-related diseases [19-21]. Platelets can interact with immune cells by secreting and releasing pro-inflammatory factors and immune adhesion mediators, exacerbating the inflammatory response and forming inflammatory thrombi [22, 23]. High altitudes have a significant impact on platelet function [24]. Therefore, it is reasonable to use D-DI/PLT, composed of D-DI and PLT, as an indicator to predict the occurrence of VTE in Tibetan critically ill patients. D-DI/PLT is a relatively new ratio that, based on changes in both D-DI and PLT, can initially be used to differentiate the coagulation system status in pregnant women. D-DI/PLT can serve as an indicator for predicting whether a hypercoagulable reaction will occur [11], while VTE is associated with the activation of the coagulation system by systemic inflammatory reactions [25]. Changes in D-DI/PLT may reflect the inflammatory and coagulation changes during the formation of VTE. Our study, for the first time, considers D-DI/PLT as a predictor of VTE risk. In our study, through multivariate Cox regression analysis, we found that the ROC curve results indicated that D-DI/PLT had higher specificity and more accurate efficacy in predicting outcomes compared to other indicators. Additionally, the area under the Caprini thrombosis risk score curve was similar to that of D-DI/PLT. Still, through correlation analysis, we found no significant correlation between the two. We speculate that the Caprini score primarily evaluates more than 40 indicators related to the patient’s disease status [10], while D-DI/PLT may reflect the body’s inflammatory/coagulation status. Therefore, there is no correlation between the two. In this study, the optimal cutoff value for the Caprini score was 3.5, which is inconsistent with the conclusion that a score of 10 or higher may indicate a risk of VTE as reported in other important studies [10]. Therefore, we believe that D-DI/PLT is a simple and easy-to-use indicator for rapidly assessing the risk of VTE in critically ill patients, especially in Tibetan populations. However, due to the requirements of the research project, our study only involved Tibetan patients treated at our center. There is a lack of research on Han patients from multiple centers and those residing in high-altitude areas for an extended period, which requires further expansion of research centers and inclusion of more ethnic groups for in-depth research.
5. Conclusion
In summary, this study highlights the substantial prevalence of venous thromboembolism (VTE) among Tibetan patients in high-altitude areas, particularly those in the respiratory ICU, contrasting sharply with lower rates in low-altitude regions. These findings underscore the need for precise risk assessment and stratified treatment for VTE in this population. The analysis of 717 Tibetan patients revealed significant differences in 12 indicators between VTE and non-VTE groups. VTE patients exhibited characteristics of older age, elevated respiratory and pulse rates, increased white blood cell counts, abnormal platelet counts, coagulation dysfunction, and impaired liver and kidney function, suggesting more severe conditions. This corresponds with other studies linking VTE incidence to condition severity.
Furthermore, the study identified five key indicators—WBC, HTC, PT, D-DI/PLT, and Caprini score—significantly correlated with VTE. D-DI/PLT, a novel predictor, emerged as a simple and accessible indicator reflecting coagulation and inflammatory status, with high predictive accuracy. Despite its strengths, this single-center study calls for further validation through multicenter research involving diverse ethnic groups to consolidate its conclusions. Nonetheless, D-DI/PLT holds promise as an effective tool for assessing VTE risk in critically ill Tibetan patients, particularly those in high-altitude ICUs.
References
[1]. Pastori D, Cormaci VM, Marucci S, et al. A Comprehensive Review of Risk Factors for Venous Thromboembolism: From Epidemiology to Pathophysiology[J]. Int J Mol Sci, 2023 ,24(4):3169.
[2]. Sydykov A, Mamazhakypov A, Maripov A, et al. Pulmonary Hypertension in Acute and Chronic High Altitude Maladaptation Disorders[J]. Int J Environ Res Public Health,2021,18(4):1692.
[3]. Nizhu, He Hangyong, Zhang Yuntao. Analysis of Risk Factors for Venous Thromboembolism in Inpatients with High-Altitude Internal Medicine and the Predictive Value of Caprini Risk Score. Tibet Science and Technology Journal. 2022; (10): 34-37.
[4]. Qin Yi. Analysis of Influencing Factors of Major Diseases on the Qinghai-Tibet Plateau and Health Risk Assessment of Human Body [Doctoral Dissertation]. Northwest Normal University, 2021.
[5]. Phillippe HM. Overview of venous thromboembolism[J]. Am J Manag Care,2017,(20 Suppl):S376-S382.
[6]. Chen Donghai, Chen Xinyao, Cai Yan, et al. Clinical Characteristics Analysis of Patients with Pulmonary Embolism Complicated by Deep Venous Thrombosis in Lower Extremities. Journal of Clinical Emergency Medicine. 2022; Volume 23, Issue 5: 305-309.
[7]. Gafter-Gvili A, Drozdinsky G, Zusman O, et al. Venous Thromboembolism Prophylaxis in Acute Medically Ill Patients: A Retrospective Cohort Study[J]. Am J Med, 2020 ,133(12):1444-1452.e3.
[8]. Stevens H, Peter K, Tran H, et al. Predicting the Risk of Recurrent Venous Thromboembolism: Current Challenges and Future Opportunities[J]. J Clin Med,2020,9(5):1582.
[9]. Nishimura A, Ikeda Y. Predicting the Incidence of Venous Thromboembolism Using the Khorana Score: A Literature Review[J]. Yakugaku Zasshi,2021,141(4):611-622.
[10]. Wang Y, Attar BM, Fuentes HE, et al. Performance of Khorana Risk Score for Prediction of Venous Thromboembolism in Patients With Hepatocellular Carcinoma[J]. Clin Appl Thromb Hemost, 2018,24(3):471-476.
[11]. Cronin M, Dengler N, Krauss ES, et al. Completion of the Updated Caprini Risk Assessment Model (2013 Version) [J]. Clin Appl Thromb Hemost,2019,1076029619838052.
[12]. Limonta G, Intra J, Brambilla P. The clinical utility of D-dimer/platelet count ratio in pregnant women[J]. J Matern Fetal Neonatal Med, 2022,35(18):3602-11.
[13]. Srivastava S, Kumari B, Garg I, et al. Targeted gene expression study using TaqMan low density array to gain insights into venous thrombo-embolism (VTE) pathogenesis at high altitude[J]. Blood Cells Mol Dis, 2020,102421.
[14]. Prabhakar A, Chatterjee T, Bajaj N, et al. Venous thrombosis at altitude presents with distinct biochemical profiles: a comparative study from the Himalayas to the plains[J]. Blood Adv, 2019,3(22):3713-3723.
[15]. Algahtani FH, AlQahtany FS, Al-Shehri A, et al. Features and incidence of thromboembolic disease: A comparative study between high and low altitude dwellers in Saudi Arabia[J]. Saudi J Biol Sci, 2020,27(6):1632-1636.
[16]. Gao X, Zeng L, Wang H, et al. Prevalence of Venous Thromboembolism in Intensive Care Units: A Meta-Analysis[J]. J Clin Med,2022,11(22):6691.
[17]. Kaplan D, Casper TC, Elliott CG, et al. VTE Incidence and Risk Factors in Patients With Severe Sepsis and Septic Shock[J]. Chest, 2015,148(5):1224-1230.
[18]. Torres C, Haut ER. Prevention, diagnosis, and management of venous thromboembolism in the critically ill surgical and trauma patient[J]. Curr Opin Crit Care,2020 ,26(6):640-647.
[19]. Zhang X, Wang S, Sun L, et al. Prognostic value of D-dimer in acute myocardial infarction complicated by heart failure with preserved ejection fraction[J]. ESC Heart Fail, 2020,7(6):4118-25.
[20]. Lyngholm LE, Nickel CH, Kellett J, et al, Brabrand M. A negative D-dimer identifies patients at low risk of death within 30 days: a prospective observational emergency department cohort study[J]. QJM,2019,112(9):675-80.
[21]. Zhang Tao, Wan Yanan, Wang Yiping, et al. Construction of a DIC Early Warning System and Clinical Research in Patients with Sepsis. Journal of Clinical Emergency Medicine. 2021; Volume 22, Issue 8: 513-520.
[22]. de Bont CM, Boelens WC, Pruijn GJM. NETosis, complement, and coagulation: a triangular relationship[J]. Cell Mol Immunol, 2019,16(1):19-27.
[23]. Uzun G, Pelzl L, Singh A, et al. Immune-Mediated Platelet Activation in COVID-19 and Vaccine-Induced Immune Thrombotic Thrombocytopenia[J]. Front Immunol, 2022,13: 837629.
[24]. Wang Y, Huang X, Yang W, Zeng Q. Platelets and High-Altitude Exposure: A Meta-Analysis[J]. High Alt Med Biol, 2022 ,23(1):43-56.
[25]. Pham K, Parikh K, Heinrich EC. Hypoxia and Inflammation: Insights From High-Altitude Physiology[J]. Front Physiol,2021,12:676782.
[26]. Cronin M, Dengler N, Krauss ES, et al. Completion of the Updated Caprini Risk Assessment Model (2013 Version) [J]. Clin Appl Thromb Hemost,2019,1076029619838052.
Cite this article
Shi,X.;Zhang,Y.;Ni,Z. (2023). Predictive value of Caprini score, D-dimer, and PLT for venous thromboembolism in high-altitude. Theoretical and Natural Science,16,79-86.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 2nd International Conference on Modern Medicine and Global Health
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Pastori D, Cormaci VM, Marucci S, et al. A Comprehensive Review of Risk Factors for Venous Thromboembolism: From Epidemiology to Pathophysiology[J]. Int J Mol Sci, 2023 ,24(4):3169.
[2]. Sydykov A, Mamazhakypov A, Maripov A, et al. Pulmonary Hypertension in Acute and Chronic High Altitude Maladaptation Disorders[J]. Int J Environ Res Public Health,2021,18(4):1692.
[3]. Nizhu, He Hangyong, Zhang Yuntao. Analysis of Risk Factors for Venous Thromboembolism in Inpatients with High-Altitude Internal Medicine and the Predictive Value of Caprini Risk Score. Tibet Science and Technology Journal. 2022; (10): 34-37.
[4]. Qin Yi. Analysis of Influencing Factors of Major Diseases on the Qinghai-Tibet Plateau and Health Risk Assessment of Human Body [Doctoral Dissertation]. Northwest Normal University, 2021.
[5]. Phillippe HM. Overview of venous thromboembolism[J]. Am J Manag Care,2017,(20 Suppl):S376-S382.
[6]. Chen Donghai, Chen Xinyao, Cai Yan, et al. Clinical Characteristics Analysis of Patients with Pulmonary Embolism Complicated by Deep Venous Thrombosis in Lower Extremities. Journal of Clinical Emergency Medicine. 2022; Volume 23, Issue 5: 305-309.
[7]. Gafter-Gvili A, Drozdinsky G, Zusman O, et al. Venous Thromboembolism Prophylaxis in Acute Medically Ill Patients: A Retrospective Cohort Study[J]. Am J Med, 2020 ,133(12):1444-1452.e3.
[8]. Stevens H, Peter K, Tran H, et al. Predicting the Risk of Recurrent Venous Thromboembolism: Current Challenges and Future Opportunities[J]. J Clin Med,2020,9(5):1582.
[9]. Nishimura A, Ikeda Y. Predicting the Incidence of Venous Thromboembolism Using the Khorana Score: A Literature Review[J]. Yakugaku Zasshi,2021,141(4):611-622.
[10]. Wang Y, Attar BM, Fuentes HE, et al. Performance of Khorana Risk Score for Prediction of Venous Thromboembolism in Patients With Hepatocellular Carcinoma[J]. Clin Appl Thromb Hemost, 2018,24(3):471-476.
[11]. Cronin M, Dengler N, Krauss ES, et al. Completion of the Updated Caprini Risk Assessment Model (2013 Version) [J]. Clin Appl Thromb Hemost,2019,1076029619838052.
[12]. Limonta G, Intra J, Brambilla P. The clinical utility of D-dimer/platelet count ratio in pregnant women[J]. J Matern Fetal Neonatal Med, 2022,35(18):3602-11.
[13]. Srivastava S, Kumari B, Garg I, et al. Targeted gene expression study using TaqMan low density array to gain insights into venous thrombo-embolism (VTE) pathogenesis at high altitude[J]. Blood Cells Mol Dis, 2020,102421.
[14]. Prabhakar A, Chatterjee T, Bajaj N, et al. Venous thrombosis at altitude presents with distinct biochemical profiles: a comparative study from the Himalayas to the plains[J]. Blood Adv, 2019,3(22):3713-3723.
[15]. Algahtani FH, AlQahtany FS, Al-Shehri A, et al. Features and incidence of thromboembolic disease: A comparative study between high and low altitude dwellers in Saudi Arabia[J]. Saudi J Biol Sci, 2020,27(6):1632-1636.
[16]. Gao X, Zeng L, Wang H, et al. Prevalence of Venous Thromboembolism in Intensive Care Units: A Meta-Analysis[J]. J Clin Med,2022,11(22):6691.
[17]. Kaplan D, Casper TC, Elliott CG, et al. VTE Incidence and Risk Factors in Patients With Severe Sepsis and Septic Shock[J]. Chest, 2015,148(5):1224-1230.
[18]. Torres C, Haut ER. Prevention, diagnosis, and management of venous thromboembolism in the critically ill surgical and trauma patient[J]. Curr Opin Crit Care,2020 ,26(6):640-647.
[19]. Zhang X, Wang S, Sun L, et al. Prognostic value of D-dimer in acute myocardial infarction complicated by heart failure with preserved ejection fraction[J]. ESC Heart Fail, 2020,7(6):4118-25.
[20]. Lyngholm LE, Nickel CH, Kellett J, et al, Brabrand M. A negative D-dimer identifies patients at low risk of death within 30 days: a prospective observational emergency department cohort study[J]. QJM,2019,112(9):675-80.
[21]. Zhang Tao, Wan Yanan, Wang Yiping, et al. Construction of a DIC Early Warning System and Clinical Research in Patients with Sepsis. Journal of Clinical Emergency Medicine. 2021; Volume 22, Issue 8: 513-520.
[22]. de Bont CM, Boelens WC, Pruijn GJM. NETosis, complement, and coagulation: a triangular relationship[J]. Cell Mol Immunol, 2019,16(1):19-27.
[23]. Uzun G, Pelzl L, Singh A, et al. Immune-Mediated Platelet Activation in COVID-19 and Vaccine-Induced Immune Thrombotic Thrombocytopenia[J]. Front Immunol, 2022,13: 837629.
[24]. Wang Y, Huang X, Yang W, Zeng Q. Platelets and High-Altitude Exposure: A Meta-Analysis[J]. High Alt Med Biol, 2022 ,23(1):43-56.
[25]. Pham K, Parikh K, Heinrich EC. Hypoxia and Inflammation: Insights From High-Altitude Physiology[J]. Front Physiol,2021,12:676782.
[26]. Cronin M, Dengler N, Krauss ES, et al. Completion of the Updated Caprini Risk Assessment Model (2013 Version) [J]. Clin Appl Thromb Hemost,2019,1076029619838052.