1.Introduction
Tuberculosis (TB) is a highly transmissible disease which is induced by the bacillus Mycobacterium tuberculosis that significantly contributes to the global burden of poor health, especially in low-income or in middle-income countries. Before the onset of COVID-19 (coronavirus) pandemic, TB occupied the position of being the leading cause of mortality from single infectious agent, surpassing even the long-term prevalence of HIV/AIDS worldwide [1]. Individuals with weakened immune system are more susceptible to tuberculosis infection compared to individuals with intact immune system [2].
Due to the accessibility of potent anti-tuberculous medications, it becomes feasible to implement controlling interventions in regions with a significant burden of TB disease. The conventional intervention mode mainly focused on the medical treatment for those with active tuberculosis. However, it is important to note that drug treatment alone does not provide a comprehensive solution to the prevention of new TB infections. Furthermore, the potential consequence following an improperly or incompletely utilization of drug treatment is the development and proliferation of drug-resistant variants, which could potentially give rise to an additional emerging issue in disease control [3]. According to the analysis, current available intervention would not effectively expedite the reduction in TB cases to the desired extent. Consequently, there is a need of developing novel and enhanced intervention in order to expedite the decline in disease incidence and alleviate the global burden of this illness. Relying upon the successful study conducted in India, it is obvious that nutritional support has the potential to serve as a viable strategy in the control of TB on a broader scale.
This paper aims to demonstrate the effectiveness of nutritional support in TB controlling procedure in China following India’s successful experience as a model.
2.Two phases in TB disease progression
There are two distinct conditions associated with TB: latent TB infection (LTBI) and TB disease. LTBI refers to a state in which the bacteria can persist within the body without causing any symptoms. In most case of TB infection, the immune system of the individual is able to stop the bacteria’s proliferation. As a result, individuals are not capable of transmitting their infection to others. The subsequent stage of TB disease occurs when the bacteria become active, get rid of the control from immune system and start the multiplication within an infected individual. In this period, individuals show syndromes and potentially serve as carriers for spreading the replicated bacteria. Not every individual progresses from LTBI to the TB disease, and the duration of this evolution varies significantly among different individuals. The use of flexible and adaptable treatment strategies could prevent the progression from LTBI to TB disease [4].
3.Global burden of tuberculosis
The current estimation of global prevalence of LTBI is approximately as 25% of the global population. Approximately 10% of these persons have risk of developing TB over their lifetime [5]. In 2020, the prevalence of LTBI on a global scale was estimated to 23.0%, amounting to approximately 1.7 billion infected individuals. Assuming the current LTBI status is maintained, by the years 2030 and 2050, it is projected that the group of LTBI individuals will give rise to 16.3 and 8.3 active TB patients per 100,000 population respectively [6]. The objective for TB elimination is to achieve a annual reduction less than one case per million population by 2050. Achieving that goal necessitates a decrease in incidence by a factor of 1,000 during a timeframe about 35 years [7]. Since the majority of newly reported TB cases arise from the reactivation of LTBI rather than recent transmission, there is a recognized need to enhance treatment approaches for the former. This is considered a vital element in the efforts to control or eliminate TB in areas with a high incidence of the disease [5]. In 2019, it was projected that around 10.0 million individuals worldwide contracted TB disease. Adults comprised 88% of the total number of deaths. Most individual developed to TB disease were in South-East Asia (44% of total infection cases, WHO regions).
There exist also wide variations in the prevalence of LTBI across regions. Approximately 66% of the global new infection cases was attributed to eight nations, where India accounting for 26% and China accounting for 8.4% [6]. Despite the downward trend in TB incidence in these two countries, as indicated by epidemiological statistical data, it remains a significant issue [8]. Both of them are still listed as high burden of TB and other related disease countries for 2022 in WHO TB global report [1].
4.“Vicious circle” between TB and malnutritio, and drug-resistance problem in TB prevelence
TB is associated with numerous negative impacts on health status, including the decrease of appetite, nutrient absorption and metabolism capacity, resulting in wasting and a decline in the general state of nutrition [9]. A “vicious circle” could be observed between TB and malnutrition. Existing of TB would contribute to malnutritional status by causing deficits in both protein-energy and micronutrient way. Consequently, this malnutrition further enhances the susceptibility of the host to TB infection. Research has indicated that lack of nourishment could affect both innate then adaptive immune responses that is required in controlling TB infection and may also impact response to live vaccinations for example BCG. As an example, malnourished mice received BCG vaccination had a higher level of mycobacterial dissemination to the lymph nodes and thymus compared to well-fed ones. This finding has raised concerns over the potential negative impacts of vaccination in malnutrional status [10]. TB patients with malnutrition experience a prolonged recovery period and elevated mortality rates in comparison to patients who are appropriately nourished [11]. In TB pandemic countries, undernutrition act as a virtual driver in increased TB incidence or prevalence, as well as in the poor outcomes of therapy [110].
The potential severity of the prevailing malnutrition issue may surpass public’s initial perceptions. Globally, the number of individuals suffering from chronic undernourishment is estimated to be around 800 million. 98% of these individuals reside in low-income and middle-income countries where TB also in endemic [10]. For example, in India, TB and undernutrition coexist as syndemics [12].
The use of drug treatment alone as a conventional control method itself is insufficient in preventing the reactivation of TB within the extensive population of LTBI individuals. Furthermore, improperly or incompletely usage of this approach may potentially contribute to the issue of drug resistance [3]. Recently, an increasing focus on nutritional support has been presented within the field of TB disease control. A cluster-randomized controlled trial was conducted in four districts of Jharkhand in India to investigate the effectiveness of a field-based, open-label intervention. The experiment involved household contacts of 2800 patients who had microbiologically confirmed TB infection. These previous studies have demonstrated that implementing a dietary intervention in only 6 months resulted in 39%-48% over a span of two years as a significant decrease of TB incidence within the household [12]. In conclusion this successful trail illustrates that the use of nutritional supplementation could potentially be a beneficial strategy in the management and control of tuberculosis.
5.A succeeded study application in India [12]
Previous trials have demonstrated that nutritional support as a “biosocial intervention” can effectively facilitate the reduction of TB incidence in TB and undernutrition syndemic countries. During the period from 1918 to 1943, partial area in UK faced the challenge of TB without the availability of chemotherapy or the BCG vaccine.The enhancement of living conditions, which subsequently led to improved nutrition, resulted in a significant reduction of TB incidence by a factor of six.
A clinical trial was conducted in India from 2019 to 2022, applying a total of 10,345 home contacts as experimental samples. 3543 (34%) of the entire experimental population experienced the condition of undernutrition. The total number of cases was randomly and equally allocated to either the control group or the intervention group. The distribution process was consistent to an average household size of one index case, along with four contacts in each group. In both 2 groups, TB patients were provided with a monthly food supplement containing 1200 kcal and 52 grams of protein per day, as well as daily pills delivering the required dietary amount of micronutrients. The intervention group’s family contacts were provided with an extra food supply containing 750 kcal energie suplly with 23 grams of protein per day and per person, as well as a recommended dietary allowance of micronutrient pills. An extensive list of participants’ basic information, categorized by groups, as well as their average values in aggregate, is provided in Table 1.
Table 1. Basic information of participants of household contact trial in two groups. (Not original, data from [12])
|
Groups and respective participants number |
Intervention group (n = 5621) |
Control group (n = 4724) |
Total (n = 10 345) |
|
Cases of TB incidence |
96 (1.7%) |
122 (2.6%) |
218 (2.1%) |
|
Contacts / index case (1400 index patients in each study group) |
4.0 |
3.4 |
3.7 |
|
Presence of BCG scar Total |
3426 (61.0%) |
2557 (54.1%) |
5983 (57.8%) |
|
Asset cost Cost of 23 household assets (American dollar on actual exchange rate in 2023) |
16 500 Indian Rupees Approximately 198 $ |
15 000 Indian Rupees Approximately 180 $ |
A decrease observed in the tracked total population each group as a result of the COVID-19 outbreak. The primary outcome assessment was completed by 5328 (94.8%) cases in the intervention group and 4283 (90.7%) cases in the control group, as a result of practical limitations. In this study, investigators have observed that the cumulative incidence of tuberculosis increases in each of the two groups as time progresses. The detailed results of accumulated incidence in two groups respectively could be found in figure 1 and table 2.
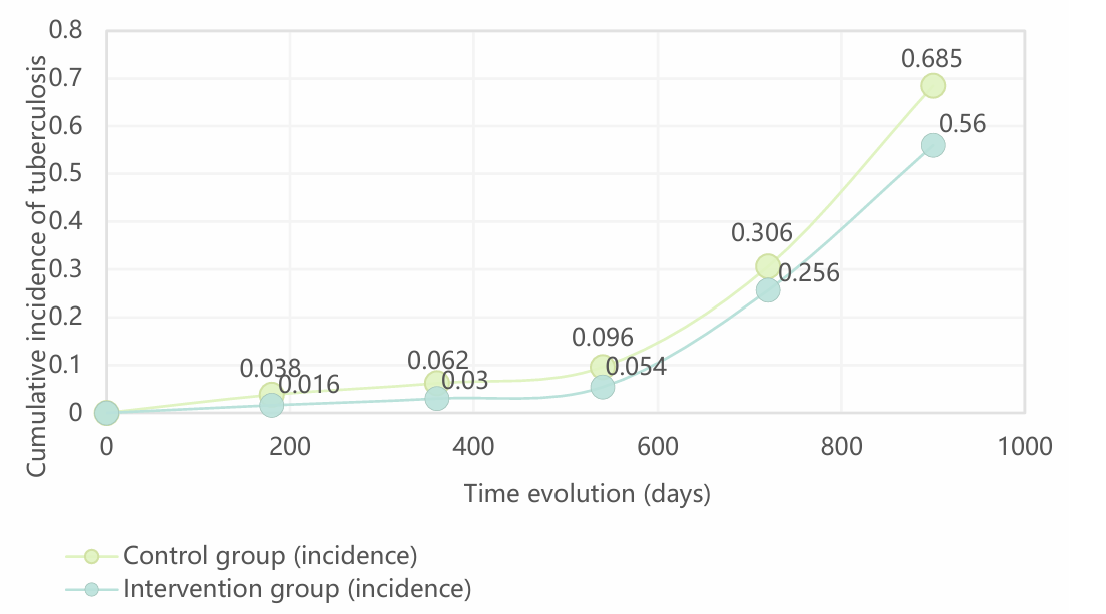
Figure 1. The cumulative incidence of TB disease within the trial group over the duration of the follow-up period, visualized by a scatter plot. (Not original, data from [13])
Table 2. Basic information of participants of household contact trial in two groups. (Not original, data from [12])
|
Group |
Number (decrease progressively over time) |
|||||
|
Control group (total number) |
4631 |
4619 |
4592 |
4562 |
4539 |
4526 |
|
Intervention group (total number) |
5542 |
5538 |
5512 |
5495 |
5476 |
5463 |
|
Control group (incidence) |
0 (0%) |
174 (3.8%) |
283 (6.2%) |
437 (9.6%) |
1387 (30.6%) |
3100 (68.5%) |
|
Intervention group (incidence) |
0 (0%) |
88 (1.6%) |
167 (3.0%) |
296 (5.4%) |
1400 (25.6%) |
3058 (56.0%) |
In beginning data, it is evident that among the undernutrition population, the initial occurrence rate of TB surpasses that of the general population (where nutritional status is determined by individual weight as shown by body mass index, or BMI). The variation between the data obtained is about a twofold difference. This randomized controlled trial demonstrates the effectiveness of nutritional support in significantly reducing 39% of the TB incidence rate across every form of the disease. Additionally, the intervention group exhibited a notable 48% decrease in the incidence rate of microbiologically confirmed pulmonary tuberculosis as the principal infection mode, compared to the reduction in control group. In summary, the nutritional support has been demonstrated to be a cost-effective, efficient, and accessible method in controlling TB, as evidenced by empirical research conducted in India. The final comprehensive outcome data is accessed in Table 3.
Table 3. The conclusive data provided within two trial groups. (Not original, data from [12])
|
Incidence per 100 person per year (caculated in %) |
||
|
Group |
Control group |
Intervention group |
|
Nutrition status at baseline Underweight (BMI < 18.5 kg/m²) |
1.94 (1.48–2.54) |
0.75 (0.51–1.12) |
|
Nutrition status at baseline Normal or above (BMI ≥ 18.5 kg/m²) |
0.93 (0.66–1.31) |
0.33 (0.17–0.65) |
|
Overall |
1.27 (1.00–1.61) |
0.78 (0.64–0.96) |
6.Current situation of tuberculosis and related controlling intervention in China
6.1.The actual burden of TB disease in China
As previously mentioned, although there has an obvious decrease in the tendency during the past few years, China continues to face a significant burden of TB disease. China accounts for 8.4% of the global new incidence cases, indicating that it ranks third among countries with the largest burden of tuberculosis worldwide [1]. Another issue that has arisen since the onset of the COVID-19 outbreak in 2019 is the diversion of primal healthcare resources and accompanying infrastructure away from other problematic diseases, such as TB. Based on predictions provided up by relevant researchers, it is anticipated that the COVID-19 pandemic will result in a 20% rise in tuberculosis mortality worldwide within the upcoming five-year period [11].
6.2.Mainstream disease control interventions in China
The dominant strategy for TB control in China continues to be the utilization of traditional methods. This involves providing vaccinations prior to potential exposure, followed by medical treatment after affirmative infection. In China, children under the age of one are eligible to receive free TB vaccine (BCG), in order to reduce the risk of future infection. Furthermore, individuals diagnosed with TB receive a fundamental set of free testing and medications. The expenses associated with additional services are borne by publicly-funded medical insurance programs. According to a study involving a total of 3,286 respondents diagnosed TB, the median costs associated with TB care per patient were found to be 1041.3 USD, 12.7 USD, and 1185.5 USD for direct, indirect, and total costs, respectively. The proportion of direct expenditures in relation to overall costs was found to be 88.0%, whereas direct medical costs constituted 69% of the total costs. One notable inference that can be drawn from the context of Chinese public health practice is the substantial financial burden faced by both the government and individual TB sufferers. The existing tuberculosis (TB) care strategies and packages are inadequate in effectively addressing this matter [13].
Another global issue that significantly impacts TB therapy in China is drug resistance. China is currently dealing with a significant burden of drug-resistant TB and multidrug-resistant tuberculosis (MDR-TB), which has resulted in it having the second highest caseload worldwide. MDR-TB exhibits a disproportionate impact on impoverished rural communities, with the highest prevalence observed in less developed locations. This resistance can be attributed mostly to the interruption and/or inappropriate implementation of TB treatment protocols. As previously indicated, a significant financial burden is experienced by the majority of households affected by the condition, primarily due to the cumulative expenses associated with treatment and other related expenditures. As a result of this factor, the application of TB treatment was restricted, leading to inadequate implementation or premature discontinuation [14].
7.Deduction: Why the application of nutritional support will be feasible in China?
In the aforementioned trial conducted in India, it has been demonstrated that nutritional support is a viable, efficient, and cost-effective intervention in the TB control or treatment. As an alternative of medical supplies, the cost of food supply would be considerably less. The potential benefit includes not only the economic advantage, but also a potent countermeasure towards medication resistance.
The management of TB in India is confronted with three major challenges. Firstly, disordered private healthcare sector, which is often characterized by a lack of organization, but serves as the initial point of care for a majority of patients. Consequently, patients may not always have access to adaptable and appropriate diagnosis or therapy following TB exposure. The absence of coordination and information sharing between departments restricts effective collaboration and communication, resulting in limited dissemination of information to public health authorities. Due to a lack of information pertaining to the present state of the disease, the government encounters challenges in formulating pertinent control policy for TB control. Lastly, the current economic load poses complications for the government in allocating funds towards nutritional support initiatives [15].
On the contrary, the Chinese government’s demonstrated execution ability in combating the initial outbreak of COVID-19 in 2019, coupled with its remarkable efficiency in epidemic control, indicate that the medical system in China possesses the capacity and potential to achieve comparable results in managing other diseases.
When comparing the two countries, it can be observed that China possesses a marginally higher Gross National Income (GNI) in contrast to India [16,17]. As previously said, it is important to note that the Chinese government is currently assuming partial financial responsibility for the diagnosis and treatment of tuberculosis patients. This implies that the government possesses the capability to assume the estimated cost of nutritional support as an intervention, which is far lower than the former amount.
In conclusion, it is recommended that the Chinese government explore the practical application of nutritional support as a simple, practicable, successful, and low-cost innovative approach to control tuberculosis.
8.Conclusion
Tuberculosis (TB) is an important topic in infectious disease context, having imposed a substantial burden on a global scale for an extended period of time. Present measures for controlling TB have been found to be unsuitable for the current circumstances and are unable to meet the public’s demand for combating the prevalence of TB. The implementation of nutritional support offers a novel approach that can provide patients with the essential nutritional requirements. This intervention has the potential to contribute to disease prevention, delay disease development, and give therapeutic advantages in the context of tuberculosis control. Based on the findings of a practical study conducted in India, it has been suggested that nutritional support could potentially serve as a novel and cost-effective intervention in China, potentially leading to superior outcomes compared to those observed in India. However, the practicality and availability of implementing this proposed intervention are still being assessed through a series of studies in order to get formal approval.
References
[1]. Global tuberculosis report 2022. https://www.who.int/publications/i/item/9789240061729
[2]. Mayo Clinic Press Tuberculosis Disease & Condition, 2023. https://www.mayoclinic. org/diseases-conditions/tuberculosis/symptoms-causes/syc-20351250
[3]. Shaji B, Arun Thomas ET, Sasidharan PK. Tuberculosis control in India: Refocus on nutrition. Indian J Tuberc. 2019 Jan;66(1):26-29. doi: 10.1016/j.ijtb.2018.10.001. https://pubmed.ncbi. nlm.nih.gov/30797277/
[4]. CDC Latent TB Infection and TB Disease, 2020. https://www.cdc.gov/tb/topic/basics/ tbinfectiondisease.htm
[5]. Huaman MA, Sterling TR. Treatment of Latent Tuberculosis Infection-An Update. Clin Chest Med. 2019 Dec;40(4):839-848. doi: 10.1016/j.ccm.2019.07.008. PMID: 31731988; PMCID: PMC7043866. https://www.sciencedirect.com/science/article/abs/pii/S0272523119300619? via%3Dihub
[6]. Chakaya J, Khan M, Ntoumi F, Aklillu E, Fatima R, Mwaba P, Kapata N, Mfinanga S, Hasnain SE, Katoto PDMC, Bulabula ANH, Sam-Agudu NA, Nachega JB, Tiberi S, McHugh TD, Abubakar I, Zumla A. Global Tuberculosis Report 2020 - Reflections on the Global TB burden, treatment and prevention efforts. Int J Infect Dis. 2021 Dec;113 Suppl 1(Suppl 1):S7-S12. doi: 10.1016/j.ijid.2021.02.107. Epub 2021 Mar 11. PMID: 33716195; PMCID: PMC8433257. https://www.ijidonline.com/article/S1201-9712(21)00193-4/fulltext
[7]. Dye C, Glaziou P, Floyd K, Raviglione M. Prospects for tuberculosis elimination. Annu Rev Public Health. 2013;34:271-86. doi: 10.1146/annurev-publhealth-031912-114431. Epub 2012 Dec 14. PMID: 23244049. https://pubmed.ncbi.nlm.nih.gov/23244049/
[8]. Incidence of tuberculosis in India and China, 2000-2020 https://ourworldindata.org/ grapher/estimated-tuberculosis-incidence-rates?tab=chart&country=CHN~IND
[9]. Kant S, Gupta H, Ahluwalia S. Significance of nutrition in pulmonary tuberculosis. Crit Rev Food Sci Nutr. 2015;55(7):955-63. doi: 10.1080/10408398.2012.679500. https://pubmed.ncbi.nlm. nih.gov/24915351/
[10]. Sinha P, Davis J, Saag L, Wanke C, Salgame P, Mesick J, Horsburgh CR, Hochberg NS. Undernutrition and Tuberculosis: Public Health Implications. J Infect Dis. 2019 Apr 16;219(9):1356-1363. doi: 10.1093/infdis/jiy675. https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC6941617/
[11]. Zhang Q, Song W, Liu S, An Q, Tao N, Zhu X, Yang D, Wan D, Li Y, Li H. An Ecological Study of Tuberculosis Incidence in China, From 2002 to 2018. Front Public Health. 2022 Jan 18;9:766362. doi: 10.3389/fpubh.2021.766362. PMID: 35118041; PMCID: PMC8804159. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8804159/
[12]. Bhargava A, Bhargava M, Meher A, Benedetti A, Velayutham B, Sai Teja G, Watson B, Barik G, Pathak RR, Prasad R, Dayal R, Madhukeshwar AK, Chadha V, Pai M, Joshi R, Menzies D, Swaminathan S. Nutritional supplementation to prevent tuberculosis incidence in household contacts of patients with pulmonary tuberculosis in India (RATIONS): a field-based, open-label, cluster-randomised, controlled trial. Lancet. 2023 Aug 19;402(10402):627-640. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(23)01231-X/fulltext
[13]. Xu C, Xia Y, Hu D, Zhang X, Zhao Y. Financial Burden of Tuberculosis Patients - China, 2020. China CDC Wkly. 2023 Mar 24;5(12):266-270. doi: 10.46234/ccdcw2023.048. PMID: 37138892; PMCID: PMC10150749. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC 10150749/
[14]. Long Q, Qu Y, Lucas H. Drug-resistant tuberculosis control in China: progress and challenges. Infect Dis Poverty. 2016 Jan 29;5:9. doi: 10.1186/s40249-016-0103-3. PMID: 26822738; PMCID: PMC4731907. https://pubmed.ncbi.nlm.nih.gov/26822738/
[15]. Arinaminpathy N, Nandi A, Vijayan S, Jha N, Nair SA, Kumta S, Dewan P, Rade K, Vadera B, Rao R, Sachdeva KS. Engaging with the private healthcare sector for the control of tuberculosis in India: cost and cost-effectiveness. BMJ Glob Health. 2021 Oct;6(10):e006114. doi: 10.1136/bmjgh-2021-006114. PMID: 34610905; PMCID: PMC8493898. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8493898/
[16]. Gross National Income (GNI) for India, 2022 https://fred.stlouisfed.org/series/ MKTGNIINA646NWDB
[17]. Gross National Income (GNI) for China, 2022 https://fred.stlouisfed.org/series/ MKTGNICNA646NWDB
Cite this article
Qiao,X. (2023). Nutritional supply: The potential simplest vaccine and therapy as tuberculosis control intervention in China. Theoretical and Natural Science,27,167-173.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 2nd International Conference on Modern Medicine and Global Health
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Global tuberculosis report 2022. https://www.who.int/publications/i/item/9789240061729
[2]. Mayo Clinic Press Tuberculosis Disease & Condition, 2023. https://www.mayoclinic. org/diseases-conditions/tuberculosis/symptoms-causes/syc-20351250
[3]. Shaji B, Arun Thomas ET, Sasidharan PK. Tuberculosis control in India: Refocus on nutrition. Indian J Tuberc. 2019 Jan;66(1):26-29. doi: 10.1016/j.ijtb.2018.10.001. https://pubmed.ncbi. nlm.nih.gov/30797277/
[4]. CDC Latent TB Infection and TB Disease, 2020. https://www.cdc.gov/tb/topic/basics/ tbinfectiondisease.htm
[5]. Huaman MA, Sterling TR. Treatment of Latent Tuberculosis Infection-An Update. Clin Chest Med. 2019 Dec;40(4):839-848. doi: 10.1016/j.ccm.2019.07.008. PMID: 31731988; PMCID: PMC7043866. https://www.sciencedirect.com/science/article/abs/pii/S0272523119300619? via%3Dihub
[6]. Chakaya J, Khan M, Ntoumi F, Aklillu E, Fatima R, Mwaba P, Kapata N, Mfinanga S, Hasnain SE, Katoto PDMC, Bulabula ANH, Sam-Agudu NA, Nachega JB, Tiberi S, McHugh TD, Abubakar I, Zumla A. Global Tuberculosis Report 2020 - Reflections on the Global TB burden, treatment and prevention efforts. Int J Infect Dis. 2021 Dec;113 Suppl 1(Suppl 1):S7-S12. doi: 10.1016/j.ijid.2021.02.107. Epub 2021 Mar 11. PMID: 33716195; PMCID: PMC8433257. https://www.ijidonline.com/article/S1201-9712(21)00193-4/fulltext
[7]. Dye C, Glaziou P, Floyd K, Raviglione M. Prospects for tuberculosis elimination. Annu Rev Public Health. 2013;34:271-86. doi: 10.1146/annurev-publhealth-031912-114431. Epub 2012 Dec 14. PMID: 23244049. https://pubmed.ncbi.nlm.nih.gov/23244049/
[8]. Incidence of tuberculosis in India and China, 2000-2020 https://ourworldindata.org/ grapher/estimated-tuberculosis-incidence-rates?tab=chart&country=CHN~IND
[9]. Kant S, Gupta H, Ahluwalia S. Significance of nutrition in pulmonary tuberculosis. Crit Rev Food Sci Nutr. 2015;55(7):955-63. doi: 10.1080/10408398.2012.679500. https://pubmed.ncbi.nlm. nih.gov/24915351/
[10]. Sinha P, Davis J, Saag L, Wanke C, Salgame P, Mesick J, Horsburgh CR, Hochberg NS. Undernutrition and Tuberculosis: Public Health Implications. J Infect Dis. 2019 Apr 16;219(9):1356-1363. doi: 10.1093/infdis/jiy675. https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC6941617/
[11]. Zhang Q, Song W, Liu S, An Q, Tao N, Zhu X, Yang D, Wan D, Li Y, Li H. An Ecological Study of Tuberculosis Incidence in China, From 2002 to 2018. Front Public Health. 2022 Jan 18;9:766362. doi: 10.3389/fpubh.2021.766362. PMID: 35118041; PMCID: PMC8804159. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8804159/
[12]. Bhargava A, Bhargava M, Meher A, Benedetti A, Velayutham B, Sai Teja G, Watson B, Barik G, Pathak RR, Prasad R, Dayal R, Madhukeshwar AK, Chadha V, Pai M, Joshi R, Menzies D, Swaminathan S. Nutritional supplementation to prevent tuberculosis incidence in household contacts of patients with pulmonary tuberculosis in India (RATIONS): a field-based, open-label, cluster-randomised, controlled trial. Lancet. 2023 Aug 19;402(10402):627-640. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(23)01231-X/fulltext
[13]. Xu C, Xia Y, Hu D, Zhang X, Zhao Y. Financial Burden of Tuberculosis Patients - China, 2020. China CDC Wkly. 2023 Mar 24;5(12):266-270. doi: 10.46234/ccdcw2023.048. PMID: 37138892; PMCID: PMC10150749. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC 10150749/
[14]. Long Q, Qu Y, Lucas H. Drug-resistant tuberculosis control in China: progress and challenges. Infect Dis Poverty. 2016 Jan 29;5:9. doi: 10.1186/s40249-016-0103-3. PMID: 26822738; PMCID: PMC4731907. https://pubmed.ncbi.nlm.nih.gov/26822738/
[15]. Arinaminpathy N, Nandi A, Vijayan S, Jha N, Nair SA, Kumta S, Dewan P, Rade K, Vadera B, Rao R, Sachdeva KS. Engaging with the private healthcare sector for the control of tuberculosis in India: cost and cost-effectiveness. BMJ Glob Health. 2021 Oct;6(10):e006114. doi: 10.1136/bmjgh-2021-006114. PMID: 34610905; PMCID: PMC8493898. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8493898/
[16]. Gross National Income (GNI) for India, 2022 https://fred.stlouisfed.org/series/ MKTGNIINA646NWDB
[17]. Gross National Income (GNI) for China, 2022 https://fred.stlouisfed.org/series/ MKTGNICNA646NWDB