1. Introduction
The pulse oximeter, as a developing wearable medical device, emits photons from the light emitting diode inside the device on a non-invasive basis, passing through different parts of the human skin surface, and then the light signal is converted into an electrical signal by the photodiode. Using PPG technology, which also has broad application prospects in the field of medical equipment, a signal graph is obtained, and physiological parameter information such as heart rate and blood oxygen saturation is calculated based on the results. However, in practical applications, pulse oximeters have some shortcomings, such as being affected by external environmental interference, the motion state of the measured body, and some flaws in the algorithm itself. Therefore, further improving the accuracy and real-time monitoring capability of pulse oximeters, enhancing their performance and reliability, has become the future development trend. This article will propose some specific suggestions for this development trend, such as optimization, deep learning algorithms, artificial intelligence technology, the optimization of product structure, the addition and integration of more sensors, and the reduction of external interference to achieve more stable, accurate, and comprehensive health analysis, and even to achieve non-invasive monitoring of more physiological parameters in the future. It can be foreseen that pulse oximeters will be more closely integrated into people's daily lives and become an indispensable part of monitoring human health.
2. Types and composition structure of pulse oximeters
As shown in Figure 1, in common practical applications, optical capacitive pulse wave sensors can be roughly divided into two basic types: transmission type and reflection type. Transmitting optical sensors place light-emitting diodes and photodiodes on both sides of the skin. Due to the external electric field inside the light-emitting diode, the electrons inside are excited, transitioning from the Ev valence to the Ec conduction, recombining with holes in an excited state, releasing energy and photons, and the electrons transition from the excited state to the ground state, thus achieving electroluminescence. After passing through the test object, photons are absorbed by photodiodes, producing photoelectric effects. With the energy of photons, electrons are excited to transition from Ev valence to Ec conduction, forming electron hole pairs inside the diode. Under the electric field of the internal PN junction, charge carriers are separated to form current. Traditional pulse oximeters, such as those produced by Masimo and Nonin, mostly use transmissive optical sensors to monitor physiological parameters by clamping them onto the user’s fingertips or earlobes. These devices are widely used in medical and home health monitoring. On the other hand, reflective optical sensors place light-emitting diodes and photodiodes on the same side of the skin, but also emit photons from the light-emitting diodes, which are reflected by the skin and then captured by the photodiodes. This layout makes reflective optical sensors particularly suitable for monitoring areas such as the wrist, forearm, or earlobe. For example, the Apple Watch introduced to the market in 2015 uses reflective optical sensors to monitor users' heart rate, helping them monitor exercise intensity and overall heart health [1].
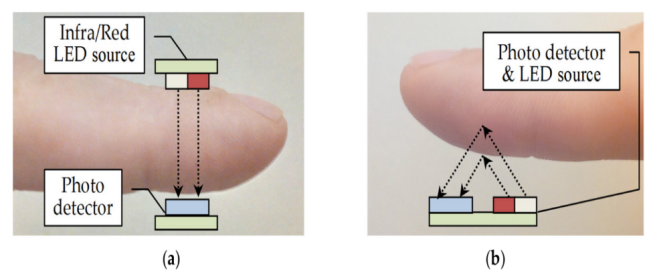
Figure 1. A basic principle of PPG sensors working in: (a) transmission, (b) reflection modes.
3. The working principle of A pulse oximeter
3.1. The formation of photoplethysmography signal graph
During the contraction and relaxation of the heart, the blood volume in the arteries also changes. When the heart contracts, the blood volume of the arteries increases, the blood content increases, the amount of photons absorbed by the blood as the test body increases, the amount of photons captured by the photodiode decreases, and the signal weakens. On the contrary, the heart relaxes, blood volume decreases, and signals become stronger. Therefore, the flow characteristics of blood can be represented by changes in light intensity, and photoplethysmography (PPG) signal maps can be obtained through temporal and amplitude changes (Figure 2).
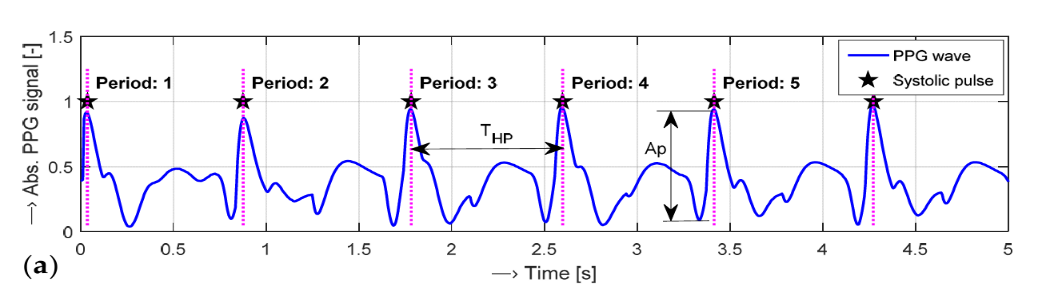
Figure 2. An example of the PPG signal analysis
3.2. Methods for calculating heart rate and blood oxygen saturation
Observing the PPG signal graph, the signal is strong during cardiac diastole, and recording a peak; When the heart contracts, the signal is weak and a trough is recorded. The adjacent peaks are recorded as one cycle, and by combining the time characteristics of the horizontal axis with the amplitude changes of the vertical axis, the heart rate index can be calculated. On the other hand, blood oxygen saturation needs to be combined with two formulas, namely The Beer Lambert Law and the definition formula for blood oxygen saturation. The following formula is the definition of blood oxygen saturation [2].
\( {SpO_{2}}=\frac{[{HbO_{2}}]}{[{HbO_{2}}]+[Hb]}×100\%=\frac{{C_{{HbO_{2}}}}}{{C_{{HbO_{2}}}}+{C_{Hb}}}×100\%\ \ \ (1) \)
The Beer Lambert Law is “A=lg (1/T)=Kbc.” Among them, A represents absorbance, T represents transmittance, that is, the outgoing light intensity (I) is greater than the incident light intensity (I0), K is the molar extinction coefficient, which is related to the properties of the absorbing material and the wavelength λ of the incident light, c is the molar concentration of the absorbing material, and b is the thickness of the absorbing layer. Referring to The Beer Lambert Law, it is easy to obtain the calculation formulas for the valley and peak values of the PPG signal graph. The following formulas are the calculation formula for the valley value of PPG signal graph and the calculation formula for the peak value of PPG signal graph.
\( {I_{V}}={I_{o}}{e^{-{ε_{t}}{C_{t}}{l_{t}}-[{ε_{Hb}}{C_{Hb}}+{ε_{{HbO_{2}}}}{C_{{HbO_{2}}}}]{l_{b}}}}\ \ \ (2) \)
\( {I_{p}}={I_{o}}{e^{-{ε_{t}}{C_{t}}{l_{t}}-[{ε_{Hb}}{C_{Hb}}+{ε_{{HbO_{2}}}}{C_{{HbO_{2}}}}]〖{(l〗_{b}}+∆l)}}\ \ \ (3) \)
Among them, Iv and Ip represent the outgoing light intensity of the PPG signal valley and peak, respectively. I0 is the incident light intensity, ε (λ) is the molar extinction coefficient, C is the molar concentration of the absorbing substance (blood), and lb is the thickness of the absorption layer. And ∆ l represents the diameter change of the path through the arterial blood when the artery dilates, and the parameters related to other light-absorbing substances with t subscripts. After applying The Beer Lambert Law, it is necessary to use a series of mathematical deductions to associate the two calculation formulas with the definition formula, and finally obtain the empirical formula: Sp𝑶𝟐=− 𝟒𝟓. 𝟎𝟔𝟐+𝟑𝟎. 𝟎𝟓𝑹+𝟗𝟒.𝟖𝟒(%). At this point, the calculation of heart rate and blood oxygen saturation has been completed, and these physiological parameters have been obtained.
4. Further improvement of the performance and reliability of pulse oximeters
4.1. Several problems during the utilization
In practical applications, pulse oximeters capture light signals reflected or transmitted through the blood through photodiodes, and then use PPG technology to monitor blood dynamics based on its absorption and scattering characteristics, analyze changes in light signals, demonstrate blood flow characteristics, and finally obtain a PPG signal graph. However, as shown in Figure 6, the actual signal graph obtained will not be similar to the ideal state in Figure 2. The time characteristics and amplitude changes of the waveform are stable and exhibit periodic characteristics, with peaks and valleys stable at the same horizontal line. As shown in Figure 6, the true amplitude variation is not stable, and peaks and valleys also exhibit a fluctuating pattern. The reasons for this inaccuracy can be divided into three aspects [3].
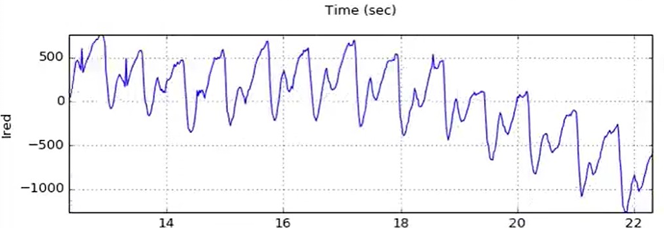
Figure 3. Example of PPG signal analysis in practical applications
The external environment has two main impacts on the PPG signal graph. Firstly, the light signal received by the photodiode does not exclude the interference of external complex light sources, such as sunlight, fluorescent lamps, LEDs, and similar light sources, which can cause the photodiode to capture excess photons and generate errors. On the other hand, there is partial interference from radio frequency pulses at the receiving end. Therefore, it is necessary to establish a safe and normal receiving environment with weak light signals and low magnetic fields to further weaken the influence of external environment on photodiodes. For example, a cover using non-ferromagnetic materials (such as Al) can be designed for the emitting area of the light-emitting diode and the receiving part of the photodiode to isolate external complex optical and magnetic signals, while also considering comfort and not being too tightly sealed [4].
The measured body is also divided into two aspects, namely the external state and the internal state. Firstly, whether the tested object is in a stationary state during monitoring has a significant impact on the accuracy of the PPG signal map. If the subject is in a state of vigorous exercise during monitoring, the PPG signal will be subject to baseline drift caused by breathing, electromyographic interference caused by muscle contraction jitter, and more severe motion artifacts [5]. Because wearing a pulse oximeter requires consideration of comfort, the measured body and the oximeter will not be in a tightly integrated state, and there may be some gaps [6]. So during the process of movement, the distance between the gaps will constantly change, resulting in irregular light leakage phenomena, which will form motion artifacts reflected in the PPG signal, thereby causing the PPG signal in the time domain to completely lose its periodicity. On the other hand, in the frequency domain, the frequency of motion artifacts is similar to the frequency of real heart rate and cannot be removed by simple filtering methods. This is the impact of external states on the PPG signal graph. The internal state is mainly composed of two aspects: the molar extinction coefficient and the light absorption caused by other substances. The internal state of the tested body, such as skin tissue, muscle tissue, skeleton, etc., will produce a relatively different result for each person based on various factors such as skin color, age, gender, etc. Both the molar extinction coefficient and the light absorption caused by other substances will adopt the same constant due to algorithmic reasons, which undoubtedly leads to a certain degree of error. [7].
4.2. Targeted suggestions
The optimization algorithm refers to improving the algorithm to eliminate errors caused by usage issues when calculating heart rate and blood oxygen saturation [8]. And among them, the first thing to solve is to remove the motion artifacts of PPG signals. There are mainly two methods. One is to change the acquisition position of PPG signals, selecting positions such as earlobes and fingertips to collect PPG signals. Another approach is to use algorithms to eliminate motion artifacts. The main requirements include Independent Component Analysis, ICA, Wavelet Transform, WT, Empirical Mode Decomposition, EMD, Singular Value Decomposition, SVD, Adaptive filters, etc. The most suitable research method is to use a joint algorithm based on cascaded RLS CEMDAN to remove motion artifacts. Using cascaded RLS adaptive filtering to use three-axis acceleration signals as Recursive Least Squares, the reference signal of the RLS adaptive filter is improved to overcome the shortcomings of single-stage adaptive filter denoising, thereby filtering out most of the motion artifacts in the PPG signal. Then, using the Complete Ensemble Empirical Mode Decomposition With Adaptive Noise (CEEMDAN), the PPG signal is decomposed, denoised, and reconstructed to remove residual motion artifacts and ultimately obtain a clean PPG signal. In the next stage, an improved spectral peak tracking method based on Grey Wolf Optimization, GWO Support Vector Machine, and SVM is proposed for heart rate estimation algorithms. This method extracts the characteristic values of PPG signals and three-axis acceleration signals in both time and frequency domains, and inputs them into the classification model to automatically classify the spectral peaks under different motion states, locate the correct spectral peaks corresponding to the true heart rate values, and further improve the accuracy of heart rate estimation. Finally, the time-varying autoregressive model method based on multi wavelet basis function expansion, fast Fourier transform, FFT spectrum analysis method, and acceleration signal are combined to preprocess the photoplethysmographic pulse wave signal using a bandpass filter and a sliding average filter. The interfered PPG signal is segmented using the time-varying autoregressive model method based on multi wavelet basis function expansion. Fast Fourier transform spectrum analysis is performed on each segment of the signal to search for spectral peaks and determine all possible heart rate values. The acceleration signal is used to make the optimal selection from all possible heart rate values, and the heart rate is finally determined [9]. A PPG signal graph with relatively reduced error is confirmed. On this basis, it is also possible to increase the number of LED lights to increase the corresponding wavelength and molar extinction coefficient in practical calculations. Reduce errors by comparing multiple sets of calculations and data. Finally, big data can be utilized to organize and summarize factors such as gender, age, and race that affect the properties of absorbed substances and integrate a more accurate sample data of the molar extinction coefficient to achieve targeted treatment.
As mentioned earlier, interference is mainly divided into two parts, namely external environmental interference and internal motion state interference. In terms of the external environment, the product style can be optimized, such as by designing it as two bottle caps. The bottom part of the bottle cap is composed of light-emitting diodes and photodiodes, while the surrounding parts are isolated from complex light sources and RF pulse interference. On the other hand, the internal state can be achieved by integrating more sensors, such as accelerometers, gyroscopes, and other tools, to further accurately correct the interference caused by the internal motion state and improve the accuracy and stability of monitoring data [10].
5. Conclusion
Pulse oximeters have shown tremendous potential for development with the rapid development of wearable medical devices and the increasing importance individuals place on health monitoring. It obtains signals from different parts of the human skin surface on a non-invasive basis and calculates physiological parameter information such as heart rate and blood oxygen saturation based on the obtained PPG signal graph. There are certain shortcomings in the discussion of this aspect in this article, that is; it does not combine actual data and cases to demonstrate, but only simply explains the working principle of the pulse oximeter. The method has singularity, and there are relatively few references in the literature, which can lead to a decrease in persuasiveness. Therefore, introducing some practical cases and combining them with specific data, calculating according to existing algorithms and improved algorithms, and then comparing and analyzing the differences between the two algorithms and which one is more suitable for practical applications, would be a better improvement method. In the future, with the advancement of deep learning algorithms and artificial intelligence technology, improving product structure, integrating more sensors, optimizing related algorithms, and even achieving non-invasive monitoring of more physiological parameters for more accurate health analysis will become the focus of future research. At the same time, it cannot be ignored that portability, efficiency, and production costs will become various issues in actual industrial production. In short, pulse oximeters will be more closely integrated into people's daily lives and become an indispensable part of monitoring human health.
References
[1]. Jiří Přibil, Anna Přibilová and Ivan Frollo. Comparative Measurement of the PPG Signal on Different Human Body Positions by Sensors Working in Reflection and Transmission Modes. The 7th International Electronic Conference on Sensors and Applications. 14 November 2020. 2, 6.
[2]. LIU Jun-wei,PANG Chun-ying,XU Bo-luan. Design and Implementation of photoelectric pulse oximetry. LASER & INFRARED. January, 2014. Vol.44, No.1, 50-51.
[3]. Xu Chengxi, Li Zhiwei, Yao Jiafeng. Applications and future developments of photoplethysmography technology in wearable medical devices. Modern Instruments & Medical Treatment. 2024. Vol.30, No.3, 58-59.
[4]. Min Li. Research on Motion-resistant Heart Rate and Oxygen Saturation Extracting Algorithm Based on Photoplethysmography. Beijing Institute of Technology. January, 2016. 35-40.
[5]. HU Linqi, ZHANG Yulin, CHOU Yongxin, YANG Haiping, HE Xiao. Real-time Detection Method for Motion Artifact of Photoplethysmography Signals Based on Decision Trees. Chinese Journal of Medical Instrumentation. 2024. Vol.48, No.3, 288-290.
[6]. Yang Yanhong, Li Xian. Error Analysis and Countermeasures of Pulse Oximeter Monitoring Results. Journal of China-Japan Friendship Hospital. Dec, 2007. Vol.21, No.6, 376.
[7]. CHANG Bing. Research on the Calibration Method of Pulse Oximeters. BRAND & STANDARDIZATION. February, 2024. Phase II 254-256.
[8]. DENG Zhenjin, HUANG Haiping, WU Bitao, LIU Xiangrong, XIE Lifeng, LIU Pengju, CHEN Xinping, ZHOU Yang, LIU Yang. Study on Accuracy Test Method of Blood Oxygen Saturation and Pulse Rate of Pulse Oximeter. China Medical Equipment. 2023. Vol.38, No.9, 46-48.
[9]. Zhang xiangfeng. Research on heart rate estimation algorithm of PPG signal under human exercise condition. Anhui University of Science and Technology. 3 June 2023. 6-18.
[10]. WANG Gao-jian, CHEN Yi-jiao, LIN Jiao-jiao, WANG Fang-xu, ZHOU Ke, ZHU Ji-hong, QIU Yan, ZHOU Da-chun. Invasive Controlled Desaturation Study of Accuracy of the Cofoe Pulse Oximeter. Clinical Application. May, 2023. 126-127.
Cite this article
An,Q. (2024). The application and future development of pulse oximeters in monitoring human health. Theoretical and Natural Science,62,148-153.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 4th International Conference on Biological Engineering and Medical Science
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Jiří Přibil, Anna Přibilová and Ivan Frollo. Comparative Measurement of the PPG Signal on Different Human Body Positions by Sensors Working in Reflection and Transmission Modes. The 7th International Electronic Conference on Sensors and Applications. 14 November 2020. 2, 6.
[2]. LIU Jun-wei,PANG Chun-ying,XU Bo-luan. Design and Implementation of photoelectric pulse oximetry. LASER & INFRARED. January, 2014. Vol.44, No.1, 50-51.
[3]. Xu Chengxi, Li Zhiwei, Yao Jiafeng. Applications and future developments of photoplethysmography technology in wearable medical devices. Modern Instruments & Medical Treatment. 2024. Vol.30, No.3, 58-59.
[4]. Min Li. Research on Motion-resistant Heart Rate and Oxygen Saturation Extracting Algorithm Based on Photoplethysmography. Beijing Institute of Technology. January, 2016. 35-40.
[5]. HU Linqi, ZHANG Yulin, CHOU Yongxin, YANG Haiping, HE Xiao. Real-time Detection Method for Motion Artifact of Photoplethysmography Signals Based on Decision Trees. Chinese Journal of Medical Instrumentation. 2024. Vol.48, No.3, 288-290.
[6]. Yang Yanhong, Li Xian. Error Analysis and Countermeasures of Pulse Oximeter Monitoring Results. Journal of China-Japan Friendship Hospital. Dec, 2007. Vol.21, No.6, 376.
[7]. CHANG Bing. Research on the Calibration Method of Pulse Oximeters. BRAND & STANDARDIZATION. February, 2024. Phase II 254-256.
[8]. DENG Zhenjin, HUANG Haiping, WU Bitao, LIU Xiangrong, XIE Lifeng, LIU Pengju, CHEN Xinping, ZHOU Yang, LIU Yang. Study on Accuracy Test Method of Blood Oxygen Saturation and Pulse Rate of Pulse Oximeter. China Medical Equipment. 2023. Vol.38, No.9, 46-48.
[9]. Zhang xiangfeng. Research on heart rate estimation algorithm of PPG signal under human exercise condition. Anhui University of Science and Technology. 3 June 2023. 6-18.
[10]. WANG Gao-jian, CHEN Yi-jiao, LIN Jiao-jiao, WANG Fang-xu, ZHOU Ke, ZHU Ji-hong, QIU Yan, ZHOU Da-chun. Invasive Controlled Desaturation Study of Accuracy of the Cofoe Pulse Oximeter. Clinical Application. May, 2023. 126-127.