1. Introduction
1.1. Introduction to the nasal cavity
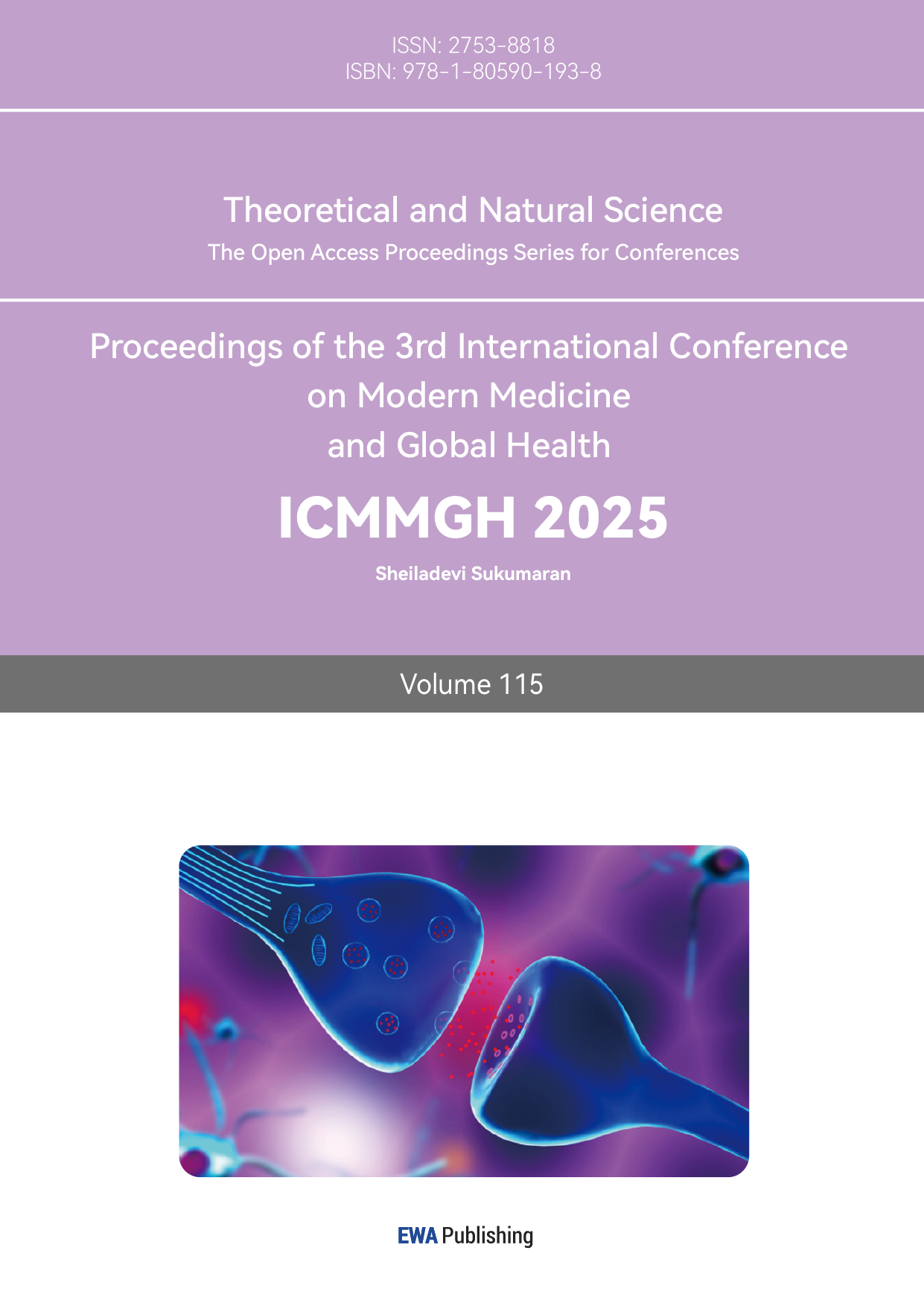
Nasal cavity is a very important part of the respiratory system, it functions to filter, warm, and humidify the air that people breath in.
In the nasal vestibule, there is a type of hair known as nose hair that can filter the air. They can filter most of the dust, bacteria, and other particles that have a radius bigger than 50μm.
The nasal mucosa is almost everywhere in the nasal cavity; it contains a lot of capillary vessels that will warm the air inhaled and glands that can humidify and help to purify the air inhaled by secreting nasal mucus [1]. It also has immunocyte-like mast cells that will secrete inflammatory mediators like histamine to cause symptoms of rhinitis. This is also the part where allergy happens. Figure 1 is a structure of the nasal cavity.
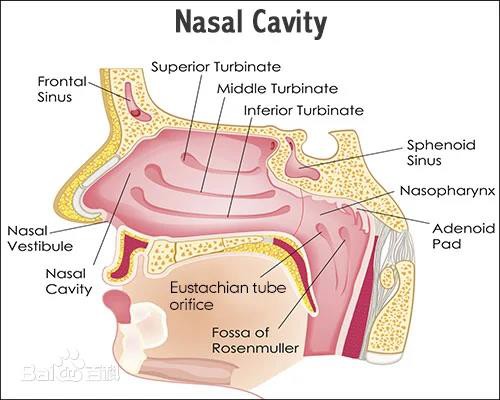
Figure 1: Structure of nasal cavity
1.2. Introduction to allergy
1.2.1. Basic information
Allergy is kind of hypersensitive reaction that the immune system takes against allergen, usually harmless substance including specific foods like nuts or glutens, pollen, animal furs, mites, and chemical substances. Serious allergy can be lethal [2].
The occur of this kind of hypersensitive reaction is because the immune system is producing too much IgE antibodies when exposed to allergen [3].
1.2.2. IgE antibodies
IgE is one of the five main types of Immunoglobulin (Ig). It mainly regulates allergic reactions.
After it’s produced by the immune system, the Fc region of the IgE antibodies (showed in figure 2) will bind to the FcRI receptors on the membrane of mast cells and instigate the production of soluble inflammatory mediators like histamines, which leads to allergic and inflammatory symptoms. Figure 2 is the structure of IgE antibodies [4]
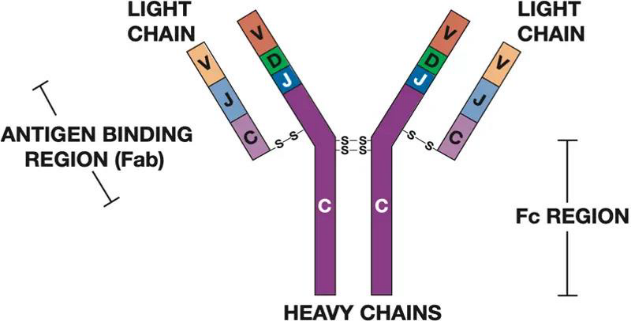
Figure 2: The structure of IgE antibodies
1.2.3. Histamine
Histamine is a kind of crucial biogenic amines produced by mast cells. It is a kind of inflammatory mediators that is responsible for most allergic symptoms.
Histamines are generated with other inflammatory mediators when IgE antibodies bind to mast cells in the process of allergy in allergic rhinitis [5].
When histamine binds to H1 amine receptors, it will cause various kinds of allergic reactions.
Inflammatory mediators like histamine can also stimulate nerve endings on the nasal mucosa, especially branches of the trigeminal nerve. When these nerve endings are stimulated, they send signals to the brain. After receiving these signals, the brain will issue commands and trigger a series of muscle movements through neural reflex mechanisms, including closing the glottis and quickly opening it to produce a strong airflow, which is called sneezing. Figure 3 is the structure of histamine [6].
Figure 3: Structure of histamine
1.2.4. H1 histamine receptor
H1 histamine receptor is a kind of protein that will bind with histamine and send signals to instigate inflammatory symptoms. The receptors in nasal cavity are mainly separated in vascular endothelial cells, smooth muscle cells, and submucosal glands [7].
When histamine binds to H1 histamine receptors on the vessel, it can cause vasodilation and increase vascular permeability, leading to congestion and edema of the nasal mucosa, as well as symptoms such as nasal congestion and runny nose [8].
H1 histamine receptors can also stimulate glandular secretion in the nasal mucosa, increasing the production of nasal mucus. This effect can lead to an increase in nasal mucus, resulting in symptoms of runny nose.
When binding to histamine, H1 histamine receptors distributed on the smooth muscles of the nasal cavity can cause smooth muscle contraction, further exacerbating the symptoms of nasal congestion [9].
Furthermore, the activation of H1 histamine receptor may instigate the biosynthesis of soluble inflammatory mediators such as histamine and therefore extravagate the allergic symptoms.
2. Allergic rhinitis and its therapeutic drugs
2.1. Introduction to allergic rhinitis
Allergic rhinitis is a kind of allergy caused by allergens in inhaled air and usually causes symptoms like sneezing, nasal discharge, nasal congestion, and optic symptoms.
Allergic rhinitis can mainly be divided into two kinds: perennial allergic rhinitis and seasonal allergic rhinitis.
Seasonal allergic rhinitis is mainly stimulated by pollens or other substances produced by plants, so patients with seasonal allergic rhinitis only have symptoms during the flowering season of the specific kinds of plants that they are allergic to.
On the other hand, perennial allergic rhinitis is mostly stimulated by other common allergens like dust mites. Since their allergens are commonly existing in the environment, patients who have perennial allergic rhinitis may suffer from allergic rhinitis all year.
Allergic rhinitis has always been a disease that bothers an extraordinary amount of population around the world. This disease's resistance to treatment, long-lasting seasonal recurrent flare-ups, and horrible feelings make it torture for patients. Allergic rhinitis is also known for its prevalence; according to research conducted during 2018-2019 with 184,326 participants aged ≥18 years old all over China, the weighted prevalence of allergic rhinitis in China is around 8.1%(±0.6%) [9]. The prevalence becomes more significant in cities with humid environments. For example, a survey conducted in Wu Han in 2011 that includes 2000 participants who have children aged between 1-8 years old points out that 48.7% of the participants’ children have had symptoms of allergic rhinitis during the past 12 months, 35% of those who had symptoms are officially diagnosed as allergic rhinitis by doctors [10].
Due to its prevalence, it’s important to know prevention and possible treatments for this disease. Although it’s extremely hard to cure allergic rhinitis completely, there are still multiple ways to inhibit its symptoms or stop it from flaring- up.
2.1.1. Main allergens
The main allergens of allergic rhinitis can be divided in to seasonal allergen and perennial allergen. Seasonal allergens are mainly pollen. Perennial allergens mainly contain dust mites, cigarette smoke, animal fur, and fungi [11].
2.1.2. Other possible factors
Allergic rhinitis can all so be instigated by other factors.
1) Environmental factors
Allergic rhinitis can be stimulated or deteriorated by air pollution.
2) Family factor
Families with allergic rhinitis or asthma may increase the possibility of allergic rhinitis.
3) Weather
Change in temperature and humidity may stimulate allergic rhinitis
4) Infection
Infections in the nasal cavity or organs near it may cause allergic rhinitis.
5) Medicines
Medicines like aspirin or NSAIDs may cause allergic rhinitis in hypersensitive populations.
2.1.3. Main medicine
1) Antihistamines
Drugs that inhibit the H1 histamine receptors are used to control the symptoms of multiple allergies. Taking pills that contain antihistamines, including levocetirizine, desloratadine, and others, can reduce allergic symptoms.
2) Corticosteroid
Drugs that inhibit the expression of inflammatory mediators, such as histamine, in order to inhibit various kinds of allergies. Nasal injection of mometasone furoate, a kind of corticosteroid, can be used to inhibit early and late-phase symptoms of both seasonal allergic rhinitis and perennial allergic rhinitis.
3) Cromolyn Sodium
A type of medicine that also inhibits the release of histamine to alleviate the symptoms of allergy. Cromolyn sodium can be made into nasal sprays in order to treat allergic rhinitis, and it can also be used to treat optic allergy in the form of gutta.
2.2. Introduction to mometasone furoate
2.2.1. Basic information
Mometasone furoate is a type of medicine that is widely used in the treatment of various kinds of allergies, including skin allergy and allergic rhinitis. Developed by Schering-Plough, an American company, in 1987.
Mometasone furoate is a kind of highly effective intranasal corticosteroid that can be used to treat or prevent nasal symptoms of seasonal allergic rhinitis and perennial allergic rhinitis. When used as a treatment of allergic rhinitis, mometasone furoate is usually made into a kind of nasal spray. Mometasone furoate can also be made into creams when it is used to treat skin allergies [12].
Experience in clinical trials proves the efficiency and good tolerability of mometasone furoate nasal spray in children and adults who have perennial rhinitis or seasonal allergic rhinitis are firmly stable. Therefore, intranasal injection of mometasone furoate is a useful first-line option for the treatment and prevention of both seasonal and perennial allergic rhinitis [13]. Figure 4 shows the structure and chemical formula of mometasone furoate.
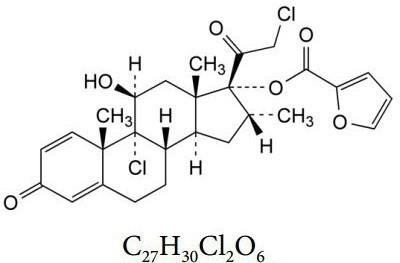
Figure 4: Structure and chemical formula of mometasone furoate
2.2.2. Mechanism
Corticosteroids such as mometasone furoate will bind to and activate glucocorticosteroid receptors in mast cells, it will then produce and send a special kind of complex into the cell’s nucleus, which regulates multiple pro-inflammatory and anti-inflammatory gene expression and inhibit the expression of inflammatory mediators like histamine by reducing the number of inflammatory mediators produced [14].
By inhibiting the expression of inflammatory mediators, mometasone furoate gets to stop symptoms like nasal discharge, nasal congestion and sneezing.
2.2.3. Side effects
1) Local side effects
When using mometasone furoate nasal spray, common local side effects include headache, nosebleeds (including bloody mucus and blood spots), pharyngitis, nasal irritation or burning sensation, nasal ulcers, etc. These side effects are usually more pronounced in the early stages of use, but over time, patients may gradually tolerate them, and symptoms may disappear on their own [15].
2) Allergic reactions
Although rare, some patients may have allergy toward mometasone furoate nasal spray, manifested as increased irritation of the nasal mucosa and even vascular edema.
3) Smell and taste interference
In rare cases, patients using mometasone furoate nasal spray have reported olfactory or taste interference.
4) Long-term side effects
For mometasone nasal sprays, long-term use may increase the risk of hormone-related adverse reactions.
2.3. Introduction to levocetirizine
2.3.1. Background information
Levocetirizine is a commonly used anti-allergic drug and belongs to the third generation of antihistamines. It is the levorotatory isomer of cetirizine, with high histamine H1 receptor antagonist activity.
Levocetirizine can be used to treat different kinds of allergy, including both seasonal allergic rhinitis and perennial allergic rhinitis, chronic idiopathic urticaria allergic skin diseases such as urticaria, allergic dermatitis, and eczema.
Based on the fact that levocetirizine has good oral absorption and high binding rate with plasma proteins, levocetirizine is usually made into oral pills. Figure 5 shows the structure of levocetirizine.
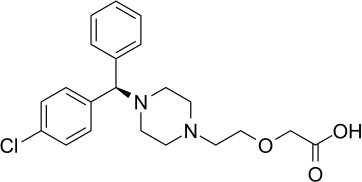
Figure 5: structure of levocetirizine
2.3.2. Mechanism
After absorbed by the body, antihistamine drugs like levocetirizine will bind to the amino acid residues group on the H1 histamine receptor that functions to bind with histamine and compete with histamine in order to achieve the goal of inhibiting allergic symptoms [16].
Although this mechanism is very effective for various kinds of allergies, H1 histamine receptors also exist and have important functions in the brain, so most antihistamine has an impact on the nerve centre and cause symptoms like drowsiness. However, since levocetirizine doesn’t have these kinds of side effects.
2.3.3. Side effects
Levocetirizine is the levorotatory configuration of cetirizine, a commonly used second-generation antihistamine medicine. However, levocetirizine doesn’t cause as much as cetirizine, including its impact on the nervous system and liver.
The penetrability of levocetirizine toward the central nervous system is relatively low,so compared to cetirizine and other antihistamine drugs, levocetirizine has a lower probability of causing central nervous system side effects such as drowsiness. Moreover, levocetirizine is more selective toward the H1 histamine receptor, and it has less reliance on the cytochrome P450 enzyme system, especially the CYP3A4 enzyme, which reduces interactions with other drugs or endogenous substances. These kinds of traits lower the risk of liver injury compared to cetirizine.
Besides, unlike cetirizine, levocetirizine has no or an extremely small amount of the dextrorotary configuration of cetirizine in it, which will cause most of the side effects that cetirizine may cause. This also helps levocetirizine to lower its side effects compared to cetirizine.
However, Levocetirizine may still cause some adverse reactions, such as headache, drowsiness, dry mouth, fatigue, weakness, or abdominal pain [17].
3. Comparison
3.1. Safety
For being both effective and producible, both levocetirizine pills and mometasone furoate nasal spray have been used as reliable clinical treatment for both seasonal allergic rhinitis and perennial allergic rhinitis for a very long period. With abundant clinical experience gained from this kind of wide usage of levocetirizine pills and mometasone furoate nasal spray, these two drugs both did not express very significant side effects or toxic.
Although there are also several different side effects may occur when taking these two kinds of medicine that are listed above, mometasone furoate nasal spray and levocetirizine pills don’t have significant difference in the rate of the appearance of those side effect, so neither of them exemplify important advantage in safety.
3.2. Cost
This study collects and compiles the prices of mometasone furoate nasal spray and levocetirizine pills from three random brands each on the internet, then transfers them into RMB per day(¥/day) and calculates the average and lowest price. These data are shown in Figure 6.
Based on the data shown below, the average price of mometasone furoate nasal spray is 2.023¥/day higher than the average price of levocetirizine pills, and the lowest price of mometasone furoate nasal spray is 1.56¥/day higher than the lowest price of levocetirizine pills.
Based on such a great difference between the cost of mometasone furoate and levocetirizine, it’s clear that the cost of taking levocetirizine pills is significantly higher than the cost of taking mometasone furoate nasal spray in a great difference, so taking levocetirizine pills, it’s a more economic friendly choice than the mometasone nasal spray.
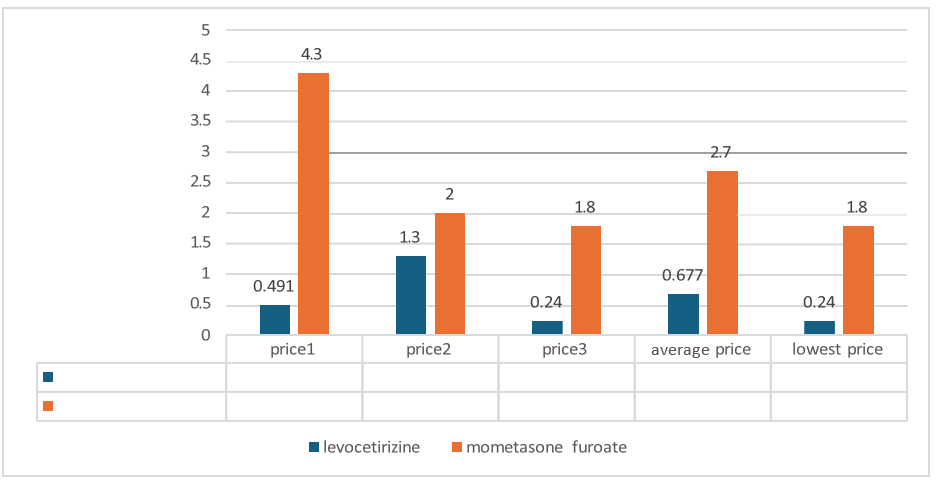
Figure 6: Cost of two drugs
4. Conclusion
Allergic rhinitis expressed a significantly high prevalence among China, so it’s important for government agency and civilian to pay attention to this disease’s prevention and possible treatments. Based on the fact that it’s hard to cure allergic rhinitis completely now, future study may focus on developing ways to cure or inhibit the symptoms of allergic rhinitis completely.
Levocetirizine pills and mometasone furoate nasal spray are proven to be two kinds of effective, safe, and possible treatments for both seasonal allergic rhinitis and perennial allergic rhinitis by a large number of scientific research and ample clinical experience gained from years of clinical usage as treatments for allergic rhinitis. However, there are still possible side effects when taking these two kinds of medicines, so the method to reduce it’s toxic or new drugs that have fewer side effects but similar effects may be potential topics for future studies.
Throughout the comparison between levocetirizine and mometasone furoate, it’s clear that these two kinds of drugs have similar effectiveness and safeness, but levocetirizine pills have a significantly lower price compared to mometasone furoate nasal spray. So, taking levocetirizine may be a more economically friendly choice. New ways to produce these two drugs at a lower cost are also a potential topic for future studies.
References
[1]. Arias-Montaño, J., & Young, J. (1993). Characteristics of histamine H1 receptors on HeLa cells. European Journal of Pharmacology Molecular Pharmacology, 245(3), 291–295. https://doi.org/10.1016/0922-4106(93)90110-u
[2]. Anolik, R. (2008). Clinical benefits of combination treatment with mometasone furoate nasal spray and loratadine vs monotherapy with mometasone furoate in the treatment of seasonal allergic rhinitis. Annals of Allergy Asthma & Immunology, 100(3), 264–271. https://doi.org/10.1016/s1081-1206(10)60452-8
[3]. Br. J. Pharmacol. ileal smooth muscle by 1,4-dithiothreitol., 87, 191–199
[4]. Blokdijk, G. (2018). Mometasone Furoate; a complete guide.
[5]. Berlucchi, M., & Pedruzzi, B. (2010). Intranasal mometasone furoate for treatment of allergic rhinitis. Clinical Medicine Insight
[6]. Cl, W. (1992). Allergic rhinitis: a review. PubMed, 18(3), 11–13. https://pubmed.ncbi.nlm.nih.gov/1572144
[7]. Donaldson, J., Hill, S.J., 1986. Selective enhancement of histamine H1-receptor responses in guinea-pig
[8]. Frieri, M., Therattil, J., Chavarria, V., Cosachov, J., Kumar, N. S., Wang, S. F., Sansone, G., Etzel, J., Dellevecchia, D., Zitt, M., Mesarina-Wicki, B., & Nolop, K. B. (1998). Effect of Mometasone Furoate on Early and Late Phase Inflammation in Patients with Seasonal Allergic Rhinitis. Annals of Allergy, Asthma, & Immunology, 81(5), 431–437. https://doi.org/10.1016/s1081- 1206(10)63141-9s. Therapeutics, 2, CMT.S4767. https://doi.org/10.4137/cmt.s4767
[9]. Gillard, M., Van Der Perren, C., Moguilevsky, N., Massingham, R., & Chatelain, P. (2002). Binding characteristics of cetirizine and levocetirizine to human H1Histamine receptors: contribution of LYS191 and THR194. Molecular Pharmacology, 61(2), 391–399. https://doi.org/10.1124/mol.61.2.391
[10]. Gametchu, B. (1995). Glucocorticoid receptor structure and leukemic cell responses. Springer.
[11]. Holgate, S. T., Church, M., & Lichtenstein, L. M. (2001). Allergy.
[12]. Lafaille, J. J., & De Lafaille, M. a. C. (2015). IGE antibodies: generation and function. Springer.
[13]. Meltzer, E., Bachert, C., & Staudinger, H. (2005). Treating acute rhinosinusitis: Comparing efficacy and safety of mometasone furoate nasal spray, amoxicillin, and placebo. Journal of Allergy and Clinical Immunology, 116(6), 1289–1295. https://doi.org/10.1016/j.jaci.2005.08.044
[14]. Parsons, M. E., & Ganellin, C. R. (2006). Histamine and its receptors. British Journal of Pharmacology, 147(S1). https://doi.org/10.1038/sj.bjp.0706440
[15]. Sundell, J., Zhou E, Sun Yue, Yang Xu, Zhang Ming& Ye Xin (2013). The relationship between indoor environmental quality and the incidence of childhood asthma and allergic rhinitis in Wuhan area Chinese Science Bulletin (Chinese Version), 58(25), 2548–2553. https://doi.org/10.1360/csb2013-58-25-2548
[16]. Shimamura, T., Shiroishi, M., Weyand, S., Tsujimoto, H., Winter, G., Katritch, V., Abagyan, R., Cherezov, V., Liu, W., Han, G. W., Kobayashi, T., Stevens, R. C., & Iwata, S. (2011). Structure of the human histamine H1 receptor complex with doxepin. Nature, 475(7354), 65–70. https://doi.org/10.1038/nature10236
[17]. Yonekura, S., Okamoto, Y., Sakurai, D., Iinuma, T., Sakurai, T., Yoneda, R., Kurita, J., Hanazawa, T., & Kawasaki, Y. (2019). Efficacy of Desloratadine and Levocetirizine in Patients with Cedar Pollen-Induced Allergic Rhinitis: A Randomized, Double-Blind Study. International Archives of Allergy and Immunology, 180(4), 274–283. https://doi.org/10.1159/000503065
Cite this article
Chen,P. (2025). An Introduction to Allergic Rhinitis & An Introduction and A Comparison Between Levocetirizine and Mometasone Furoate. Theoretical and Natural Science,115,47-54.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 3rd International Conference on Modern Medicine and Global Health
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Arias-Montaño, J., & Young, J. (1993). Characteristics of histamine H1 receptors on HeLa cells. European Journal of Pharmacology Molecular Pharmacology, 245(3), 291–295. https://doi.org/10.1016/0922-4106(93)90110-u
[2]. Anolik, R. (2008). Clinical benefits of combination treatment with mometasone furoate nasal spray and loratadine vs monotherapy with mometasone furoate in the treatment of seasonal allergic rhinitis. Annals of Allergy Asthma & Immunology, 100(3), 264–271. https://doi.org/10.1016/s1081-1206(10)60452-8
[3]. Br. J. Pharmacol. ileal smooth muscle by 1,4-dithiothreitol., 87, 191–199
[4]. Blokdijk, G. (2018). Mometasone Furoate; a complete guide.
[5]. Berlucchi, M., & Pedruzzi, B. (2010). Intranasal mometasone furoate for treatment of allergic rhinitis. Clinical Medicine Insight
[6]. Cl, W. (1992). Allergic rhinitis: a review. PubMed, 18(3), 11–13. https://pubmed.ncbi.nlm.nih.gov/1572144
[7]. Donaldson, J., Hill, S.J., 1986. Selective enhancement of histamine H1-receptor responses in guinea-pig
[8]. Frieri, M., Therattil, J., Chavarria, V., Cosachov, J., Kumar, N. S., Wang, S. F., Sansone, G., Etzel, J., Dellevecchia, D., Zitt, M., Mesarina-Wicki, B., & Nolop, K. B. (1998). Effect of Mometasone Furoate on Early and Late Phase Inflammation in Patients with Seasonal Allergic Rhinitis. Annals of Allergy, Asthma, & Immunology, 81(5), 431–437. https://doi.org/10.1016/s1081- 1206(10)63141-9s. Therapeutics, 2, CMT.S4767. https://doi.org/10.4137/cmt.s4767
[9]. Gillard, M., Van Der Perren, C., Moguilevsky, N., Massingham, R., & Chatelain, P. (2002). Binding characteristics of cetirizine and levocetirizine to human H1Histamine receptors: contribution of LYS191 and THR194. Molecular Pharmacology, 61(2), 391–399. https://doi.org/10.1124/mol.61.2.391
[10]. Gametchu, B. (1995). Glucocorticoid receptor structure and leukemic cell responses. Springer.
[11]. Holgate, S. T., Church, M., & Lichtenstein, L. M. (2001). Allergy.
[12]. Lafaille, J. J., & De Lafaille, M. a. C. (2015). IGE antibodies: generation and function. Springer.
[13]. Meltzer, E., Bachert, C., & Staudinger, H. (2005). Treating acute rhinosinusitis: Comparing efficacy and safety of mometasone furoate nasal spray, amoxicillin, and placebo. Journal of Allergy and Clinical Immunology, 116(6), 1289–1295. https://doi.org/10.1016/j.jaci.2005.08.044
[14]. Parsons, M. E., & Ganellin, C. R. (2006). Histamine and its receptors. British Journal of Pharmacology, 147(S1). https://doi.org/10.1038/sj.bjp.0706440
[15]. Sundell, J., Zhou E, Sun Yue, Yang Xu, Zhang Ming& Ye Xin (2013). The relationship between indoor environmental quality and the incidence of childhood asthma and allergic rhinitis in Wuhan area Chinese Science Bulletin (Chinese Version), 58(25), 2548–2553. https://doi.org/10.1360/csb2013-58-25-2548
[16]. Shimamura, T., Shiroishi, M., Weyand, S., Tsujimoto, H., Winter, G., Katritch, V., Abagyan, R., Cherezov, V., Liu, W., Han, G. W., Kobayashi, T., Stevens, R. C., & Iwata, S. (2011). Structure of the human histamine H1 receptor complex with doxepin. Nature, 475(7354), 65–70. https://doi.org/10.1038/nature10236
[17]. Yonekura, S., Okamoto, Y., Sakurai, D., Iinuma, T., Sakurai, T., Yoneda, R., Kurita, J., Hanazawa, T., & Kawasaki, Y. (2019). Efficacy of Desloratadine and Levocetirizine in Patients with Cedar Pollen-Induced Allergic Rhinitis: A Randomized, Double-Blind Study. International Archives of Allergy and Immunology, 180(4), 274–283. https://doi.org/10.1159/000503065