1. Introduction
The primary cause of dementia in late adulthood and one of the most diverse neurodegenerative disorders, Alzheimer's disease gets worse over time [1]. Clinical signs of AD include a steady decline in executive reasoning, memory, learning ability, and cognition [2]. While there are medications and surgical options for relieving symptoms, there is not any treatment that can stop or slow the advancement of the disease yet. One of the main causes of impairment is AD, which places a heavy burden on public health and care systems, as well as patients and their families [3-4]. For doctors and policymakers directing health and care services, it is crucial to comprehend the distribution and size of AD due to their severity and substantial loads, as previously indicated [5].
2. Epidemiology of AD in the U.S.
2.1. Overview
The prevalence of Alzheimer's disease refers to the quantity and percentage of individuals who presently have the disease in a population. The term incidence describes the number and percentage of new instances each year [6].
Alzheimer's diagnosis rates per 100,000 persons seem to be dropping. Risk factors for Alzheimer's disease have changed over the 20th century, such as high blood pressure and illiteracy. The incidence rate may decline due to the growing population of persons 65 and older, who are at higher risk of developing Alzheimer's, but more people are anticipated to develop the disease [6].
The most recent information from the Chicago Health and Aging Study and U.S. Census Bureau's 2022 projections was combined into a new analysis (CHAP). In 2022, Alzheimer's dementia is anticipated to affect 6.5 million Americans aged 65 and over. 73% of people are 75 or older [7]. Projections from the Aging, Demographics, and Memory Study (ADAMS) indicate that 11% of Americans 65 and older have dementia [8], with some variations. Alzheimer's dementia affects roughly 1 in 9 Americans (or 10.7% of the entire population) who are 65 or older. Alzheimer's dementia is more common as people get older, and this correlation is significant. 5.0% of the population is 65 to 74 years old, 13.1% is 75 to 84 years old, and 33.2% is beyond 85 years old [7].
Those younger than 65 can also develop Alzheimer's disease. A estimated estimate of 200,000 Americans, or 110 out of every 100,000 people, are thought to have younger-onset dementia, according to specialists, despite the fact that there are few research on the frequency of younger-onset Alzheimer's disease in the United States [9].
2.2. Difference between symptom-based data and biomarker-based data
Compared to symptoms, Alzheimer's-related brain abnormalities may estimate a lower prevalence than 6.5 million. Biomarker-based research found that 15% to 30% of persons with clinical symptoms of Alzheimer's disease did not have Alzheimer's-related brain abnormalities, suggesting that their dementia is caused by something else. Hence, prevalence estimates based on biomarkers may be 30% lower than those based on symptoms of Alzheimer's dementia. MCI caused by Alzheimer's disease will increase illness prevalence. The number of Americans 65 and older—the demographic most at risk—will grow, which will increase both symptom-based and biomarker-based prevalence estimates of Alzheimer's disease [10-11].
2.3. The forecasted increase on prevalence between 2020-2025 in the states
The predictions in Table 1 show that between 2020 and 2025, there will have been an increase in the number of people with Alzheimer's in every state nationwide of at least 6.7%. The Western and Southeastern regions are anticipated to experience the largest percentage increases in the number of Alzheimer's patients throughout this time. These hikes will have a substantial effect on the state-run healthcare systems [12].
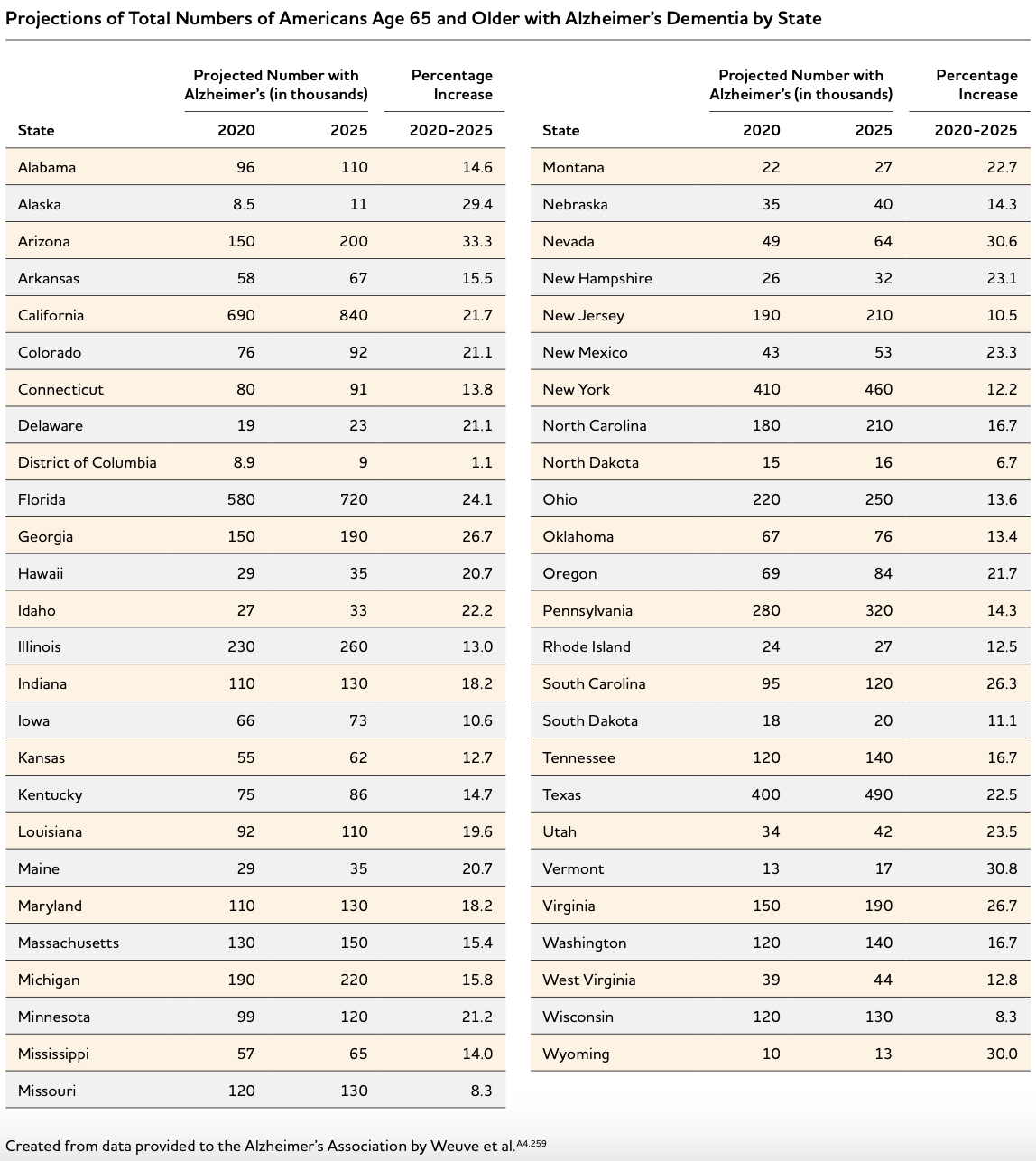
Figure 1. Projections of the Overall Number of People 65 and Older Suffering from Alzheimer's Disease by State [6].
2.4. Incidence
Recent diagnoses of Alzheimer's disease in individuals 65 and older are referred to as "incidence". It offers a prediction of the likelihood that the illness will appear. Estimates based on information from the CHAP study and the U.S. Census Bureau suggest that in 2011, around 910,000 People aged 65 and over had Alzheimer's dementia. If forecasts from the CHAP research were available for 2022, it is anticipated that this sum will rise far higher. With advancing age, the prevalence of Alzheimer's disease drastically rises. The average annual incidence in 2011 was predicted by CHAP [13] to be 0.4% for individuals 65 to 74, 3.2% for people 75 to 84, and 7.6% for people 85 and above.
2.5. Race
According to a large California health plan research, Black American older persons had the greatest dementia rate, followed by Hispanic, Pacific, American Indian or Native Alaskan, White, and Asian American older adults. In a subsequent study using the same population, there was variation within Asian-American categories, but their dementia incidence was lower in all categories than in the White population [14-15].
3. Epidemiology of AD in China
3.1. Overview
A paper from China Public Health used demographic statistics along with data on the incidence, mortality, YLL, YLD, and DALY of Alzheimer's disease in China from 1990 to 2019 to anticipate the disease's incidence over the following 30 years. The standard mortality rate of Alzheimer's disease in China showed a decreasing trend from 1990 to 2019, although the incidence showed a rising trend. The overall incidence increased from 1990 to 2019, rising from 43.32 per 100,000 people in 1990 to 126.57 per 100,000 people in 2019, with a greater incidence in females than in males. In contrast to girls, who saw a rise from 56.95 per 100,000 in 1990 to 160.70 per 100,000 in 2019, males saw an increase from 30.52 per 100,000 to 93.73 per 100,000 in 2019. The declining trend in mortality shows that Alzheimer's disease drug therapy in China is steadily improving, but the rising trend in incidence shows that Alzheimer's disease prevention in China still has to be reinforced.It is suggested that we enhance the health literacy of senior women over 75 and old men over 79 in order to reduce the occurrence of Alzheimer's disease in the future. They should be inspired to develop wholesome attitudes and behaviors [16].
The age-standardized prevalence rate of AD in the Chinese population over 60 years old was 3.20%, which was nearly equal to the population-standardized prevalence rate for the region (2.90%). These numbers are comparable to the 3.21 percent previously reported AD prevalence in China [17].
AD prevalence in China was found in 1985–2018 database searches. Rates grew considerably with each 10-year age increase. AD prevalence was anticipated to climb from 3.81% to 6.17% in five years [5]. China's AD male-to-female ratio is 0.57 according to Cui [5]. AD prevalence increased 11.7 times in 60-69 to over 80-year-olds [18]. Since aging is the biggest risk factor for AD, this age scale shows a significant incidence in China [19]. Clinicians and politicians that oversee health care must understand AD's prevalence and distribution because it's burdensome. An aging population, lack of disease prevention, detection, and treatment, and Alzheimer's disease are straining China's healthcare system [20]. North China, East China, Northwest China, Northeast China, Central China, South Central China, and Southwest China were the study's geographic locations. Figure 2 demonstrates China's varied pooled prevalence rates. AD was lowest in South China and greatest in Northwest China [5]
.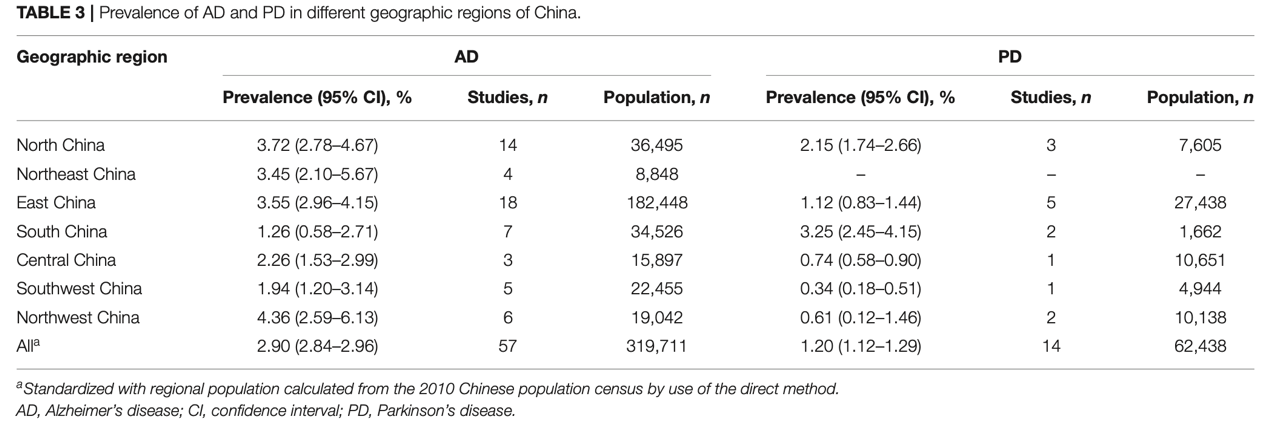
Figure 2. Prevalence of AD in different geographic regions of China.
3.2. Regional researches
Regional researches in China on the epidemiology of Alzheimer’s disease also have great significance. These regional studies provide references in different aspects, which are more detailed, closer to people's livelihood and more comprehensive than the national data. This research enables scientists and governments to use these data to see the burden condition, adjust local policies, and be aware of providing real help and welfare to local patients.
The current situation and influencing factors of Alzheimer's disease in the elderly population aged 65 and above in Henan Province were studied, and the prevalence rate was 6.05% [21].
The investigation in Beijing analyzed the knowledge and cognition of healthcare workers on Alzheimer's disease in Beijing. Among the 7 dimensions, the correct rate of treatment management and course of the disease was the highest, which were 67.89% and 66.14% respectively, but the correct rate of care dimension was only 37.23%. It is concluded that medical workers in Beijing have little knowledge about Alzheimer's disease, and relevant knowledge training should be strengthened to improve the service quality of medical workers for patients with Alzheimer's disease [22].
In Taiyuan, Shanxi, aged adults with mild cognitive impairment (MCI) and those with full cognitive function were compared for Alzheimer's disease risk. Researchers came to the conclusion that the risk of AD was 5.27 times higher in old people with mild cognitive impairment than in the general population from a random sample of 6192 elderlies aged 65 and over. Risk factors for MCI developing into AD include hypertension, hyperlipidemia, diabetes, anxiety, fear, and introversion. High educational level, mental work, frequent reading, and frequent participation in activities were protective factors for MCI conversion to AD. The AD prevalence rate is 4.86%. Early detection and therapy should be pursued through long-term surveillance. Elderly individuals with mild cognitive impairment ought to be urged to engage in more recreational activities in their local communities and increase their physical activity levels. In order to secure their mental and physical pleasure, mindset, and relief from anxiety, elderly individuals with hypertension or other disorders should have active treatment. This can significantly reduce the likelihood of Alzheimer's disease. Taiyuan's older population has an Alzheimer's disease prevalence that is comparable to northern Chinese cities, greater than southern cities, but lower than that of foreign countries [23].
A research in Yunnan, China conducted a survey on Alzheimer’s disease using samples from Yuxi region. The sample size is 4000, and they used a questionnaire and some Alzheimer’s disease scales to evaluate the situation in this region. People tested are all aged 60-93. The marital status was mainly married (77.95%); Education is mainly illiteracy and primary school education(88.81%), and only 11.19% were in junior high school or above. Most of the respondents often communicate with neighbors (82.42%), do physical exercise (87.73%), and do not often participate in social activities (27.74%). The result comes out that the prevalence in Yuxi is 2.34%, the difference between two different community’s data and data from different sex has statistical significance [24].s
4. Conclusion
We can notice various differences, benefits, and drawbacks between China and the United States through the aforementioned examination of the epidemiological data on Alzheimer's disease in the United States and Alzheimer's disease in China.
First, the prevalence of Alzheimer's disease in China is generally lower than that in the United States. The reason may be that Asians generally have lower rates of Alzheimer's than Caucasians, due to some ethnic and genetic differences. It may also be social and cultural factors. For example, China pays more attention to mathematics education than the United States. However, the sheer size of China's population makes the number of Alzheimer's patients very large. So the burden on health care is still too great to ignore.
Second, China's Alzheimer's disease death rate has dropped, proving that its medical skills have improved and its intervention is correct. Yet, China and the US must be mindful that as the world's population ages, the number of senior people and Alzheimer's illness will rise. Although short-term mortality declines, disease rates are rising, thus community health care, welfare, and medical research must be prepared.
Third, both China and the United States agree on some features of Alzheimer's, such as the fact that more women have the disease than men, which has complicated reasons. In addition, the differences between local regions and different races are jointly determined by social factors, genetic factors, and many other aspects. Social factors include education level, extroversion level, social circle range, and so on.
Fourth, this article analyzed the statistics of incidence, prevalence, and mortality in several small regions in China and the statistics of every state in the United States. Combined with the overall data in China and in the world, it is suggested that the government of every small city or region in China should make precise regulations to policies and implement plans based on specific differences in the region, to provide benefits and assistance to the elderly in the area who already have Alzheimer's disease, and to do preventive work for the elderly who are still healthy.
Fifthly, through specific studies in small areas of China, we can see some entry points, such as the stimulation of Alzheimer's disease by mild cognitive impairment and the knowledge level of local medical staff on Alzheimer’s. These are things that can peripherally help with Alzheimer's prevention and treatment.
Finally, China should understand that the current situation of Alzheimer's disease in China is clearly not worse than that in the United States, so China should have enough confidence. We should continue to implement and improve existing interventions in China, and at the same time learn from the most cutting-edge research on biomarkers in the US in the Alzheimer’s disease field, in order to improve our scientific strength simultaneously.
References
[1]. A. Kumar et al. (2015). A review on Alzheimer’s disease pathophysiology and its management: an update. Pharmacological Reports, 67, 195–203
[2]. Jiang, T., Sun, Q., and Chen, S. (2016). Oxidative stress: A major pathogenesis and potential therapeutic target of antioxidative agents in Parkinson’s disease and Alzheimer’s disease. Prog. Neurobiol. 147, 1–19.
[3]. Rajiah, K., Maharajan, M. K., Yeen, S. J., and Lew, S. (2017). Quality of life and caregivers’ burden of Parkinson’s disease. Neuroepidemiology 48, 131–137.
[4]. Henderson, C., Knapp, M., Nelis, S. M., Quinn, C., Martyr, A., Wu, Y. T., et al. (2019). Use and costs of services and unpaid care for people with mild-to-moderate dementia: baseline results from the IDEAL cohort study. Alzheimer’s Dement. 5, 685–696.
[5]. Cui L, Hou N-N, Wu H-M, Zuo X, Lian Y-Z, Zhang C-N, Wang Z-F, Zhang X and Zhu J-H. (2020).Prevalence of Alzheimer’s Disease and Parkinson’s Disease in China: An Updated Systematical Analysis. Front. Aging Neurosci. 12:603854.
[6]. Alzheimer’s Association. (2022). 2022 Alzheimer’s Disease Facts and Figures. Alzheimer’s Dement 2022;18.
[7]. Weuve J, Rajan KB, Barnes LL, Wilson RS, Evans DA. (2018). Secular trends in cognitive performance in older black and white U.S. adults, 1993-2012: Findings from the Chicago Health and Aging Project. J Gerontol B Psychol Sci Soc Sci 2018;73.
[8]. Hudomiet P, Hurd MD, Rohwedder S. (2019). The relationship between lifetime out-of-pocket medical expenditures, dementia and socioeconomic status in the U.S. J Econ Ageing 2019;14: 100181.
[9]. Hendriks S, Peetoom K, Bakker C, van der Flier WM, Papma JM, Koopmans R, et al. (2021). Global prevalence of young-onset dementia: A systematic review and meta-analysis. JAMA Neurol 2021;78(9):1080-90.
[10]. Kapasi A, DeCarli C, Schneider JA. (2017). Impact of multiple pathologies on the threshold for clinically overt dementia. Acta Neuropathol 2017;134(2):171-86.
[11]. Barnes LL, Leurgans S, Aggarwal NT, Shah RC, Arvanitakis Z, James BD, et al. (2019). Mixed pathology is more likely in black than white decedents with Alzheimer’s dementia. Neurology 2015;85:528-34.
[12]. Weuve J, Hebert LE, Scherr PA, Evans DA. Prevalence of Alzheimer’s disease in U.S. states. Epidemiology 2015;26(1): E4-6.
[13]. Rajan KB, Weuve J, Barnes LL, Wilson RS, Evans DA. (2019). Prevalence and incidence of clinically diagnosed Alzheimer's disease dementia from 1994 to 2012 in a population study. Alzheimer’s Dement 2019;15(1):1-7.
[14]. Mayeda ER, Glymour MM, Quesenberry CP, Whitmer RA. (2016). Inequalities in dementia incidence between six racial and ethnic groups over 14 years. Alzheimer’s Dement 2016;12(3):216-24.
[15]. Mayeda ER, Glymour MM, Quesenberry CP, Jr., Whitmer RA. (2017). Heterogeneity in 14-year dementia incidence between Asian American subgroups. Alzheimer Dis Assoc Disord 2017;31(3):181-6.
[16]. ZHANG Jing-ya*, LU Yong-bo, LI Hao-ran, et al. (2022). Disease burden of Alzheimer’s disease and other dementias in Chinese residents between 1990 and 2019: an age-period-cohort analysis and prediction. Chin J Public Health, 38(5), 523-528.
[17]. Jia, J., Wang, F., Wei, C., Zhou, A., Jia, X., Li, F., et al. (2014). The prevalence of dementia in urban and rural areas of China. Alzheimers Dement. 10, 1–9.
[18]. Gao, S., Hendrie, H. C., Hall, K. S., and Hui, S. (1998). The relationships between age, sex, and the incidence of dementia and Alzheimer disease: a meta-analysis. Arch. Gen. Psychiatry 55, 809–815.
[19]. Wyss-Coray, T. (2016). Ageing, neurodegeneration and brain rejuvenation. Nature 539, 180–186.
[20]. Dubois, B., Hampel, H., Feldman, H. H., Scheltens, P., Aisen, P., Andrieu, S., et al. (2016). Preclinical Alzheimer’s disease: definition, natural history, and diagnostic criteria. Alzheimer’s Dement. 12, 292–323.
[21]. WANG Hai-ling, et al. (2022). Current situation and influencing factors of Alzheimer’s disease in the elderly aged 65 and above in Henan Province. Modern Preventive Medicine, 49(8), 1356-1360.
[22]. MA Yan-ru, Xu Yang, et al. (2022). Investigation on knowledge and cognition of Alzheimer's disease among 580 medical workers in Beijing. South China J Prev Med, 48(1), 125-127.
[23]. WANG Yan-ping, ZHAI Jing-bo, ZHU Fang, et al. (2011). Analysis of Alzheimer's disease and its influencing factors among elderly people in the community. Shanxi Medical University.
[24]. LIU Bo-yuan. (2018). Prevalence of Alzheimer's disease in areas of Yunnan Province. Kunming Medical University.
Cite this article
Cheng,J. (2023). Epidemiology comparison and analysis of Alzheimer's disease in China and the United States. Theoretical and Natural Science,20,57-63.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 3rd International Conference on Biological Engineering and Medical Science
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. A. Kumar et al. (2015). A review on Alzheimer’s disease pathophysiology and its management: an update. Pharmacological Reports, 67, 195–203
[2]. Jiang, T., Sun, Q., and Chen, S. (2016). Oxidative stress: A major pathogenesis and potential therapeutic target of antioxidative agents in Parkinson’s disease and Alzheimer’s disease. Prog. Neurobiol. 147, 1–19.
[3]. Rajiah, K., Maharajan, M. K., Yeen, S. J., and Lew, S. (2017). Quality of life and caregivers’ burden of Parkinson’s disease. Neuroepidemiology 48, 131–137.
[4]. Henderson, C., Knapp, M., Nelis, S. M., Quinn, C., Martyr, A., Wu, Y. T., et al. (2019). Use and costs of services and unpaid care for people with mild-to-moderate dementia: baseline results from the IDEAL cohort study. Alzheimer’s Dement. 5, 685–696.
[5]. Cui L, Hou N-N, Wu H-M, Zuo X, Lian Y-Z, Zhang C-N, Wang Z-F, Zhang X and Zhu J-H. (2020).Prevalence of Alzheimer’s Disease and Parkinson’s Disease in China: An Updated Systematical Analysis. Front. Aging Neurosci. 12:603854.
[6]. Alzheimer’s Association. (2022). 2022 Alzheimer’s Disease Facts and Figures. Alzheimer’s Dement 2022;18.
[7]. Weuve J, Rajan KB, Barnes LL, Wilson RS, Evans DA. (2018). Secular trends in cognitive performance in older black and white U.S. adults, 1993-2012: Findings from the Chicago Health and Aging Project. J Gerontol B Psychol Sci Soc Sci 2018;73.
[8]. Hudomiet P, Hurd MD, Rohwedder S. (2019). The relationship between lifetime out-of-pocket medical expenditures, dementia and socioeconomic status in the U.S. J Econ Ageing 2019;14: 100181.
[9]. Hendriks S, Peetoom K, Bakker C, van der Flier WM, Papma JM, Koopmans R, et al. (2021). Global prevalence of young-onset dementia: A systematic review and meta-analysis. JAMA Neurol 2021;78(9):1080-90.
[10]. Kapasi A, DeCarli C, Schneider JA. (2017). Impact of multiple pathologies on the threshold for clinically overt dementia. Acta Neuropathol 2017;134(2):171-86.
[11]. Barnes LL, Leurgans S, Aggarwal NT, Shah RC, Arvanitakis Z, James BD, et al. (2019). Mixed pathology is more likely in black than white decedents with Alzheimer’s dementia. Neurology 2015;85:528-34.
[12]. Weuve J, Hebert LE, Scherr PA, Evans DA. Prevalence of Alzheimer’s disease in U.S. states. Epidemiology 2015;26(1): E4-6.
[13]. Rajan KB, Weuve J, Barnes LL, Wilson RS, Evans DA. (2019). Prevalence and incidence of clinically diagnosed Alzheimer's disease dementia from 1994 to 2012 in a population study. Alzheimer’s Dement 2019;15(1):1-7.
[14]. Mayeda ER, Glymour MM, Quesenberry CP, Whitmer RA. (2016). Inequalities in dementia incidence between six racial and ethnic groups over 14 years. Alzheimer’s Dement 2016;12(3):216-24.
[15]. Mayeda ER, Glymour MM, Quesenberry CP, Jr., Whitmer RA. (2017). Heterogeneity in 14-year dementia incidence between Asian American subgroups. Alzheimer Dis Assoc Disord 2017;31(3):181-6.
[16]. ZHANG Jing-ya*, LU Yong-bo, LI Hao-ran, et al. (2022). Disease burden of Alzheimer’s disease and other dementias in Chinese residents between 1990 and 2019: an age-period-cohort analysis and prediction. Chin J Public Health, 38(5), 523-528.
[17]. Jia, J., Wang, F., Wei, C., Zhou, A., Jia, X., Li, F., et al. (2014). The prevalence of dementia in urban and rural areas of China. Alzheimers Dement. 10, 1–9.
[18]. Gao, S., Hendrie, H. C., Hall, K. S., and Hui, S. (1998). The relationships between age, sex, and the incidence of dementia and Alzheimer disease: a meta-analysis. Arch. Gen. Psychiatry 55, 809–815.
[19]. Wyss-Coray, T. (2016). Ageing, neurodegeneration and brain rejuvenation. Nature 539, 180–186.
[20]. Dubois, B., Hampel, H., Feldman, H. H., Scheltens, P., Aisen, P., Andrieu, S., et al. (2016). Preclinical Alzheimer’s disease: definition, natural history, and diagnostic criteria. Alzheimer’s Dement. 12, 292–323.
[21]. WANG Hai-ling, et al. (2022). Current situation and influencing factors of Alzheimer’s disease in the elderly aged 65 and above in Henan Province. Modern Preventive Medicine, 49(8), 1356-1360.
[22]. MA Yan-ru, Xu Yang, et al. (2022). Investigation on knowledge and cognition of Alzheimer's disease among 580 medical workers in Beijing. South China J Prev Med, 48(1), 125-127.
[23]. WANG Yan-ping, ZHAI Jing-bo, ZHU Fang, et al. (2011). Analysis of Alzheimer's disease and its influencing factors among elderly people in the community. Shanxi Medical University.
[24]. LIU Bo-yuan. (2018). Prevalence of Alzheimer's disease in areas of Yunnan Province. Kunming Medical University.