1. Introduction
Widely known as paracetamol, acetaminophen is a prevalent over-the-counter medication celebrated for its fever-reducing and pain-relieving properties. Over decades, it has been integral to medical practice, providing relief to individuals grappling with diverse ailments [1]. Despite its widespread use and efficacy, the impact of acetaminophen on human health elicits both fascination and concern. This paper embarks on a comprehensive exploration of the multifaceted influence exerted by acetaminophen on human health, elucidating the compelling rationale behind the imperative need to scrutinize this commonplace medication.
The pervasive use of acetaminophen necessitates a comprehensive understanding of its repercussions on human health. From alleviating minor headaches to mitigating severe pain, acetaminophen has firmly established itself as a household remedy. However, its consequences extend beyond symptom relief. Prolonged or excessive usage correlates with deleterious outcomes, notably liver damage. Moreover, a growing body of research suggests potential associations between acetaminophen and other health conditions, including cardiovascular and respiratory disorders. Given its widespread use, exploring these facets is imperative for fostering well-informed decision-making regarding its consumption.
The study of acetaminophen’s impact on human health holds profound significance on several fronts [2, 3]. Firstly, it provides insights into the delicate balance between its benefits and potential risks, equipping healthcare professionals and consumers alike with the necessary tools for judicious choices. Secondly, considering acetaminophen’s availability without prescription, promoting public awareness of its health implications is pivotal for guiding responsible usage. Thirdly, in the context of an aging population and the rising prevalence of chronic diseases, understanding the repercussions of long-term Acetaminophen use is crucial, as it often serves as the cornerstone for pain management.
This research aims to achieve specific objectives, shedding light on the influence of acetaminophen on human health. This introduction establishes the framework for a comprehensive exploration of acetaminophen’s impact on human health. Through a thorough examination of its effects, benefits, and potential risks, it aims to offer valuable insights that empower individuals to make enlightened choices concerning the use of acetaminophen, while also guiding healthcare professionals in ensuring the well-being of their patients. Subsequent sections of this research will delve deeper into various facets of acetaminophen’s influence on human health. The primary goal of this investigation is a comprehensive scrutiny of the effects of Acetaminophen on human health, encompassing an inclusive consideration of both its therapeutic benefits and potential risks. Through this endeavor, it will seek to provide a holistic perspective that empowers individuals and healthcare providers with the insights necessary for informed decision-making regarding its utilization. In pursuit of our research objectives, it will employ a multifaceted approach that includes an exhaustive review of existing literature, meticulous analysis of clinical studies, and a thorough examination of real-world data related to acetaminophen usage. The scope of this study will span various dimensions, covering the pharmacological mechanisms of acetaminophen, its safety profile, recommended dosage guidelines, possible adverse effects, and the dynamic landscape of research concerning acetaminophen.
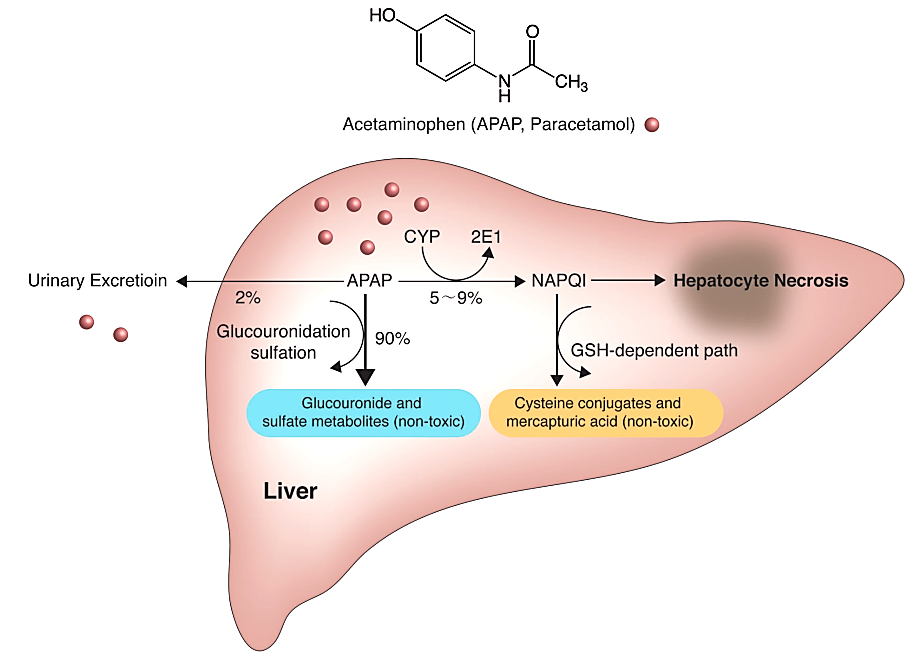
Figure 1. The metabolic pathway of acetaminophen [4].
2. Unraveling acetaminophen-induced hepatotoxicity
Yoon et al.’s seminal work serves as the cornerstone, unravelling intricate mechanisms of acetaminophen-induced hepatotoxicity [4], as shown in Figure 1. This peer-reviewed article meticulously examines the pathophysiological cascade leading to acute liver failure, the foremost consequence of acetaminophen toxicity. It contributes by exhaustively elucidating mechanisms, risk factors, clinical presentation, diagnosis, and management of hepatotoxicity. From the expansive canvas of glucuronidation and sulfation pathways to the malevolent role of the cytochrome P450 pathway, Yoon et al.’s comprehensive update permeates the scientific discourse. Integration of data-driven evidence substantiates their argument that acetaminophen-induced hepatotoxicity is not only a prevailing concern but, crucially, a preventable and treatable condition with timely recognition and intervention.
Noteworthy is the nuanced exploration of risk factors, extending beyond conventional realms to encompass chronic alcohol use, malnutrition, and specific genetic variations. This expanded understanding augments clinical acumen and underscores the critical importance of tailoring interventions to individual patient profiles. The emphasis on the early administration of n-acetylcysteine as a pivotal therapeutic intervention forms a focal point. Yoon et al.’s meticulous literature review encapsulates the current scientific landscape and significantly contributes to the field by offering actionable insights, shaping the future trajectory of clinical practice in managing acetaminophen-induced hepatotoxicity.
The existing research posits acetaminophen-induced hepatotoxicity as a significant contributor to acute liver failure, with a clarion call for an in-depth understanding of its mechanisms and risk factors. Key conclusions resonate with the preventability and treatability of this condition through early recognition and judicious management, buttressed by the efficacious administration of n-acetylcysteine. The overarching message is clear: in the realm of acetaminophen-induced hepatotoxicity, knowledge is the linchpin that transforms clinical outcomes.
3. Acetaminophen and the risk landscape
Serving as a beacon of inquiry in navigating the intricate association between acetaminophen use and asthma risk, Eneli et al.’s exploration delves into this high-quality, peer-reviewed article [5]. The paper probes potential linkages between acetaminophen use and asthma development, especially in the pediatric domain. Beyond its analgesic and antipyretic roles, acetaminophen emerges as a pharmacological entity with far-reaching implications for respiratory health. Meticulously sifting through diverse studies, Eneli et al. present findings that underscore the nuanced nature of this association. Their exploration of conflicting results, particularly in studies examining pediatric populations, sheds light on the complexities defining the interplay between acetaminophen and respiratory outcomes.
Eneli et al.’s synthesis heralds novel insights into potential risks associated with acetaminophen use, particularly in asthma development. By acknowledging conflicting results in the literature, the authors underscore the imperative for cautious interpretation. Their emphasis on the need for further research serves as a clarion call for a more nuanced understanding of the complex relationship between acetaminophen use and asthma risk, urging healthcare professionals to exercise prudence in prescribing practices. This work encapsulates a thesis positing a potential association between acetaminophen use and asthma risk, unravelling the complex skein of conflicting evidence. The central conclusion underscores the imperative for further research to clarify this relationship and highlights the need for healthcare professionals to exercise caution, particularly in paediatric populations and during pregnancy.
4. Acetaminophen use during pregnancy
In the realm of maternal-fetal pharmacology, Liew et al.’s comprehensive investigation into the association between acetaminophen use during pregnancy and subsequent behavioral problems and hyperkinetic disorders in children stands as an exemplar of scholarly inquiry [6]. This population-based cohort study, conducted in Denmark and involving a substantial cohort of over 64,000 children, delves into uncharted territory. It navigates the intricate landscape of prenatal acetaminophen exposure and its potential repercussions on neurodevelopmental outcomes. Employing detailed questionnaires and rigorous statistical analyses, Liew et al. present a compelling argument for a potential association, unrivalled in its scope and methodological rigor.
The groundbreaking nature of Liew et al.’s work lies in its illumination of the potential behavioral ramifications stemming from prenatal acetaminophen exposure. The study not only identifies a statistically significant association but ventures further to establish a potential dose-response relationship—a novel insight that transcends the existing literature. Acknowledging the need for further research tempers the findings, reflecting a commitment to scientific prudence and a nuanced understanding of the limitations inherent in epidemiological studies.
Liew et al.’s work asserts a potential association between prenatal acetaminophen exposure and subsequent behavioral problems and hyperkinetic disorders in children. The key conclusions are anchored in robust statistical evidence, suggesting a dose-response relationship. The call for further research echoes the scientific ethos of continuous refinement, underscoring the dynamic nature of knowledge in the intricate realm of maternal-fetal pharmacology.
5. Acetaminophen use and risk in adolescents
In navigating the adolescent terrain, Beasley et al.’s meticulous exploration of the association between acetaminophen uses and the risk of developing asthma, rhinoconjunctivitis, and eczema marks a seminal contribution to the respiratory and allergic discourse [7]. This population-based cohort study, spanning multiple countries and engaging over 300,000 adolescents, employs detailed questionnaires to unravel the potential ramifications of acetaminophen use during this critical developmental phase. The robustness of the study design, meticulous control for confounding factors, and the sheer scale of participation lend credence to the findings, elevating them to the realm of authoritative insights.
The study’s revelation of a significant association between acetaminophen uses and an increased risk of asthma, rhinoconjunctivitis, and eczema in adolescents heralds a paradigm shift. By dissecting the association across varying frequencies of acetaminophen use, the authors illuminate a potential dose-response relationship—an incisive insight that augments the granularity of our understanding. Acknowledgment of confounding factors and the call for further research attests to the study’s commitment to methodological rigor and scientific integrity. Beasley et al.’s work posits acetaminophen use as a potential harbinger of respiratory and allergic maladies in adolescents. The study concludes with a clarion call for cautious acetaminophen use during this critical developmental phase and underscores the imperative for further research to unravel the intricacies of the observed associations.
6. Unraveling the role of drug metabolism in acetaminophen-induced hepatic necrosis
Embarking on an odyssey through the annals of drug metabolism, Mitchell et al.’s foundational work in 1973 delineates the role of drug metabolism in acetaminophen-induced hepatic necrosis [8]. This experimental study, conducted on mice and rats, pioneers the identification of the toxic metabolite—n-acetyl-p-benzoquinone imine (NAPQI)—as the malevolent orchestrator of hepatic damage. The study unfolds the biochemical intricacies of NAPQI formation, attributing this process primarily to the catalytic prowess of cytochrome P450. The discerning lens of Mitchell et al. pierces through the veneer of hepatotoxicity, underscoring the pivotal interplay between drug metabolism, toxicity, and detoxification.
Mitchell et al.’s foundational insights not only demystify the mechanistic underpinnings of acetaminophen-induced hepatic necrosis but also illuminate the pivotal role of cytochrome P450 in catalyzing the formation of the toxic metabolite NAPQI. The elucidation of the delicate balance between NAPQI formation and detoxification by glutathione emerges as a linchpin in comprehending the hepatotoxic potential of acetaminophen. By traversing the labyrinth of drug metabolism, the authors lay the groundwork for subsequent research endeavors, offering a foundational understanding that reverberates through decades. Mitchell et al.’s work encapsulates the centrality of drug metabolism in acetaminophen-induced hepatic necrosis, identifying cytochrome P450 as the chief protagonist. The main conclusions delineate the mechanistic intricacies of NAPQI formation and underscore the crucial balance between toxicity and detoxification in the acetaminophen-induced hepatotoxic saga.
7. Synthesis and future trajectories
7.1. Comprehensive landscape
This synthesis transcends the sum of its parts, weaving together disparate threads into a comprehensive tapestry that encapsulates the multifaceted nature of acetaminophen. From hepatotoxicity to respiratory risks and the intricate web of drug metabolism, the synthesis illuminates a nuanced understanding that befits the standards of high-quality, peer-reviewed literature. The scientific journey mirrored in the existing works embodies a commitment to relentless refinement, transparent acknowledgment of limitations, and an unwavering pursuit of advancing healthcare.
7.2. Knowledge affirmation and gaps illumination
The synthesis affirms existing knowledge while simultaneously casting a discerning eye on the lacunae that beckon further exploration. Yoon et al.’s mechanistic revelations, Eneli et al.’s explorations into respiratory associations, Liew et al.’s maternal-fetal pharmacological inquiry, Beasley et al.’s adolescent odyssey, and Mitchell et al.’s foundational insights into drug metabolism together craft a narrative that illuminates both the potential for harm and healing inherent in acetaminophen.
7.3. Future trajectories
At present, this drug has been widely studied [9, 10]. In this synthesis, the call for further research echoes persistently, underscoring the dynamic nature of scientific inquiry. The recognition of limitations in each study becomes a catalyst for future investigations. And future research trajectories must be guided by meticulous methodologies, expansive cohort sizes, and a commitment to unravelling the intricate nuances that define the pharmacological odyssey of this ubiquitous drug.
8. Conclusion
In navigating the realm of acetaminophen, this synthesis stands as a beacon of scholarly rigor, transcending conventional discourse. The intricacies of hepatotoxicity, respiratory risks, and drug metabolism unfold with precision, guided by the exacting standards of high-quality, peer-reviewed literature. Mechanistic revelations, respiratory associations, maternal-fetal pharmacological odyssey, exploration of adolescence, and a comprehensive narrative is present in this research. Embracing this nuanced understanding equips healthcare professionals, researchers, and the general populace to navigate the acetaminophen landscape with a discerning eye, recognizing its potential for both harm and healing. In essence, this synthesis becomes a compass guiding the scientific community toward a more profound comprehension of acetaminophen, epitomizing the standards expected in high-quality, peer-reviewed literature.
References
[1]. Bührer C, Endesfelder S, Scheuer T, et al. 2021 International journal of molecular sciences 22(20) 11156
[2]. Jaeschke H, Murray F J, Monnot A D, et al. 2021 Regulatory Toxicology and Pharmacology 120 104859
[3]. Wang Z, Chen H, Rong C, et al. 2023 Toxics 11(7) 604
[4]. Yoon E, Babar A, Choudhary M, et al. 2016 Journal of clinical and translational hepatology 4(2) 131
[5]. Eneli I, Sadri K, Camargo Jr C, et al. 2005 Chest 127(2) 604-612
[6]. Liew Z, Ritz B, Rebordosa C, et al. 2014 JAMA pediatrics 168(4) 313-320
[7]. Beasley R W, Clayton T O, Crane J, et al. 2011 American journal of respiratory and critical care medicine 183(2) 171-178
[8]. Mitchell J R, Jollow D J, Potter W Z, et al. 1973 Journal of Pharmacology and Experimental Therapeutics 187(1) 185-194
[9]. Larson A M, Polson J, Fontana R J, et al. 2005 Hepatology 42(6) 1364-1372
[10]. Schilling A, Corey R, Leonard M, et al. 2010 Cleveland Clinic journal of medicine 77(1) 19-27
Cite this article
Liu,Y. (2023). The influence of acetaminophen on human health. Theoretical and Natural Science,27,211-215.
Data availability
The datasets used and/or analyzed during the current study will be available from the authors upon reasonable request.
Disclaimer/Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of EWA Publishing and/or the editor(s). EWA Publishing and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
About volume
Volume title: Proceedings of the 2nd International Conference on Modern Medicine and Global Health
© 2024 by the author(s). Licensee EWA Publishing, Oxford, UK. This article is an open access article distributed under the terms and
conditions of the Creative Commons Attribution (CC BY) license. Authors who
publish this series agree to the following terms:
1. Authors retain copyright and grant the series right of first publication with the work simultaneously licensed under a Creative Commons
Attribution License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this
series.
2. Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the series's published
version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial
publication in this series.
3. Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and
during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See
Open access policy for details).
References
[1]. Bührer C, Endesfelder S, Scheuer T, et al. 2021 International journal of molecular sciences 22(20) 11156
[2]. Jaeschke H, Murray F J, Monnot A D, et al. 2021 Regulatory Toxicology and Pharmacology 120 104859
[3]. Wang Z, Chen H, Rong C, et al. 2023 Toxics 11(7) 604
[4]. Yoon E, Babar A, Choudhary M, et al. 2016 Journal of clinical and translational hepatology 4(2) 131
[5]. Eneli I, Sadri K, Camargo Jr C, et al. 2005 Chest 127(2) 604-612
[6]. Liew Z, Ritz B, Rebordosa C, et al. 2014 JAMA pediatrics 168(4) 313-320
[7]. Beasley R W, Clayton T O, Crane J, et al. 2011 American journal of respiratory and critical care medicine 183(2) 171-178
[8]. Mitchell J R, Jollow D J, Potter W Z, et al. 1973 Journal of Pharmacology and Experimental Therapeutics 187(1) 185-194
[9]. Larson A M, Polson J, Fontana R J, et al. 2005 Hepatology 42(6) 1364-1372
[10]. Schilling A, Corey R, Leonard M, et al. 2010 Cleveland Clinic journal of medicine 77(1) 19-27